These notes provide essential knowledge about two common respiratory conditions in pediatric patients. They are designed for nursing students to understand pathophysiology, clinical presentation, diagnostics, and management strategies, including nursing interventions and patient education.
Childhood Pneumonia
Definition & Significance
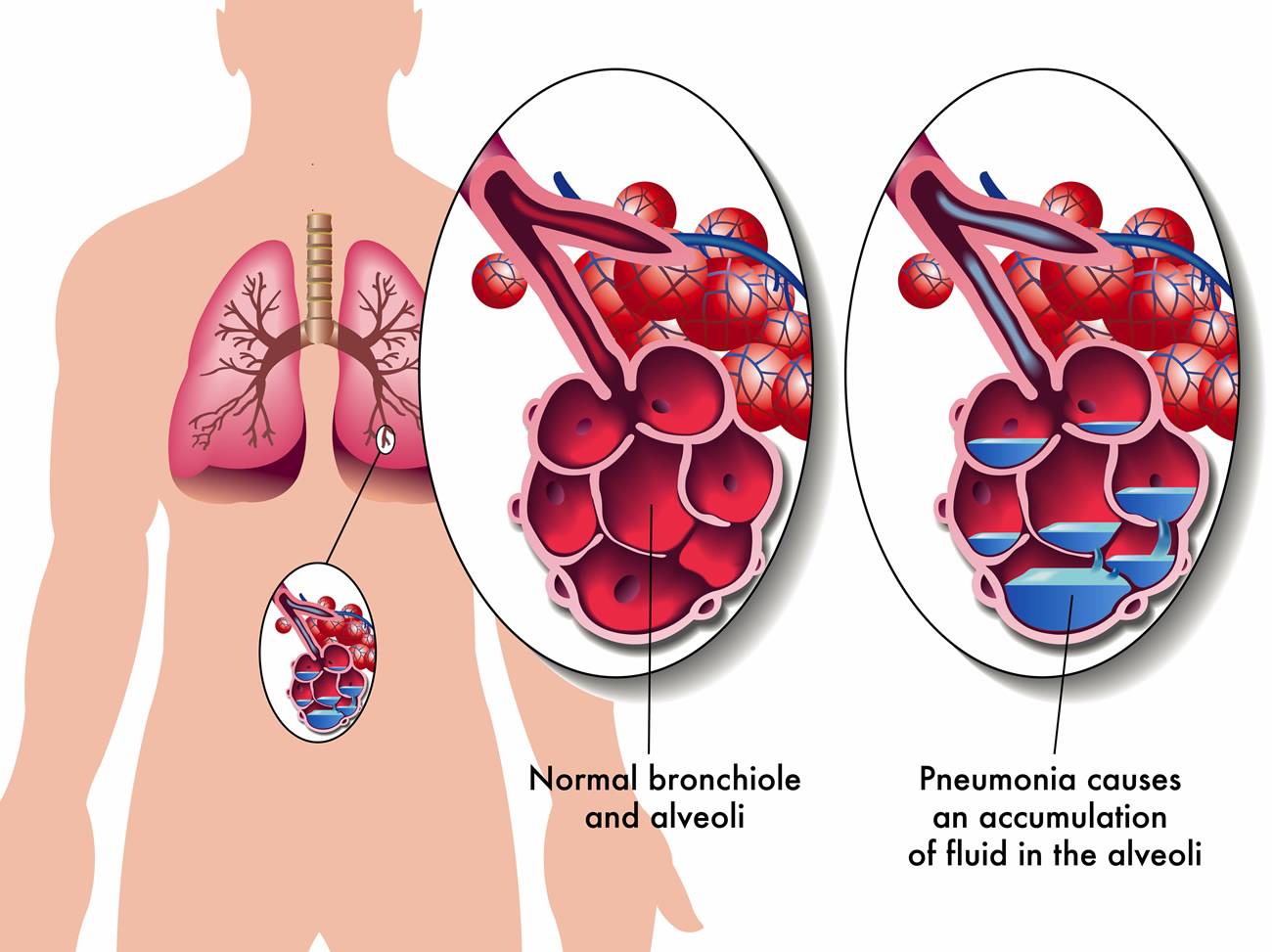
Pneumonia is an infection of the lung parenchyma characterized by inflammation of the alveoli and abnormal alveolar filling with fluid. It is a leading cause of morbidity and mortality in children under 5 years worldwide, especially in developing countries.
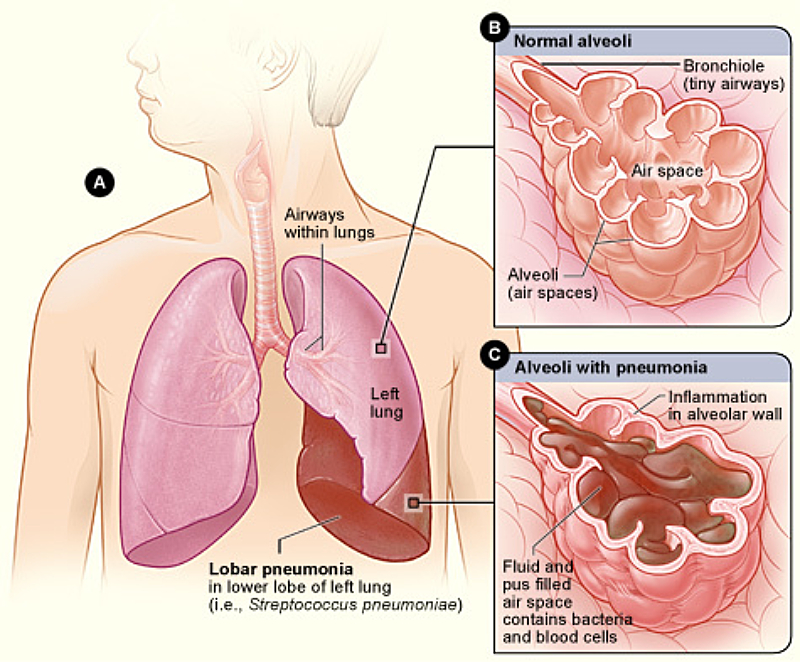
Lobar pneumonia affecting different lobes of the lung, showing areas of consolidation
Epidemiology
- Globally, 120 million cases of pneumonia annually with 1.3 million deaths
- Children under age 2 account for 80% of pneumonia-related deaths in developing countries
- Approximately 2.5 million cases yearly in developed countries
- One-third to half of cases require hospitalization
- Introduction of pneumococcal vaccine has significantly reduced incidence in the United States
Etiology
Pneumonia can be classified by age-specific versus pathogen-specific organisms:
| Age Group | Common Pathogens |
|---|---|
| Neonates (0-30 days) | Group B streptococci, Klebsiella, Escherichia coli, Listeria monocytogenes, Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus aureus |
| Infants/Toddlers (30 days-2 years) | Primarily viruses (RSV, influenza, parainfluenza, human metapneumovirus), Streptococcus pneumoniae |
| Young Children (2-5 years) | Respiratory viruses, S. pneumoniae, H. influenzae type B |
| School-age Children (5-13 years) | Mycoplasma pneumoniae, S. pneumoniae, Chlamydia pneumoniae |
| Adolescents | Similar to adults: S. pneumoniae, M. pneumoniae, C. pneumoniae |
Clinical Pearl
Consider tuberculosis (TB) in immigrant children from high-prevalence areas and children with known TB exposures. Children with chronic diseases are at risk for specific pathogens: S. aureus and Pseudomonas aeruginosa in cystic fibrosis, encapsulated organisms in sickle cell disease, and opportunistic pathogens in immunocompromised patients.
Pathophysiology
Pneumonia develops when pathogens invade the lower respiratory tract through:
- Inhalation of airborne pathogens
- Aspiration of oropharyngeal contents
- Direct invasion of respiratory epithelium
- Hematogenous spread from distant sites
Mnemonic: The 4 Stages of Lobar Pneumonia
CRGS: Congestion → Red → Gray → Solution
- Congestion (0-24 hours): Alveolar edema, vascular congestion, bacteria and neutrophils present
- Red hepatization (2-4 days): Neutrophils, red blood cells, desquamated epithelial cells, fibrin deposits (liver-like consistency)
- Gray hepatization (4-8 days): Dark brown appearance, hemosiderin accumulation, hemolysis of red cells
- Resolution (8+ days): Cellular infiltrates resorbed, pulmonary architecture restored (may lead to parapneumonic effusions if healing is suboptimal)
Clinical Manifestations
Signs and Symptoms of Pediatric Pneumonia
General Symptoms:
- Fever (usually high in bacterial pneumonia)
- Cough (may be productive or nonproductive)
- Tachypnea (key indicator in young children)
- Difficulty breathing
- Decreased appetite
- Irritability and lethargy
- Abdominal pain (may be the presenting complaint)
Physical Examination Findings:
- Nasal flaring
- Retractions (intercostal, subcostal, supraclavicular)
- Decreased breath sounds over affected area
- Crackles (rales) on auscultation
- Dullness to percussion
- Increased tactile fremitus
- Grunting (in severe cases)
- Hypoxemia (low oxygen saturation)
Clinical Pearl
The absence of fever does not rule out pneumonia, especially in infants and immunocompromised children. Additionally, a child who initially exhibits significant respiratory distress but subsequently “tires out,” appears to breathe at a normal rate, becomes lethargic, or no longer exhibits wheezing may be at risk of impending respiratory failure.
Diagnostic Evaluation
Laboratory Tests
- Complete blood count (CBC)
- Blood cultures (for severely ill patients)
- Nasopharyngeal swabs for viral testing
- Sputum gram stain and culture (often difficult to obtain in children)
- Electrolytes and renal function (for hospitalized patients)
- PCR testing for atypical pathogens
Imaging Studies
- Chest X-ray: Not routinely recommended but helpful in:
- Severe illness or toxic appearance
- Suspected complications
- Failure to respond to initial therapy
- Infants 0-3 months with fever
- Suspected foreign body or congenital abnormality
- Chest ultrasound: To evaluate for pleural effusion
- Chest CT: Rarely indicated, used for complications
Chest X-ray showing right lower lobe pneumonia in a child
Treatment and Management
Mnemonic: BREATHE for Pneumonia Management
- Bronchodilators (if wheezing present)
- Respiratory support (oxygen as needed)
- Empirically treat with antibiotics based on age/severity
- Antipyretics for fever
- Thorough hydration
- Hospitalization criteria assessment
- Education about prevention and follow-up
Pharmacological Management by Age Group
| Age Group | Empiric Antibiotic Therapy |
|---|---|
| Neonates (0-30 days) | Ampicillin + aminoglycoside OR ampicillin + third-generation cephalosporin (not ceftriaxone in infants <1 month due to risk of kernicterus) |
| Infants (1-3 months) | Ampicillin + third-generation cephalosporin; consider adding erythromycin or clarithromycin for atypical coverage |
| Infants & Children (>3 months), Outpatient | Amoxicillin 90 mg/kg/day divided BID as first-line for typical pneumonia; azithromycin for suspected atypical pneumonia |
| Infants & Children (>3 months), Inpatient | Ampicillin or penicillin G; add macrolide if atypical pneumonia suspected; consider ceftriaxone/cefotaxime for severe cases |
| Special Considerations |
– Sickle cell disease: Cefotaxime, macrolide, ± vancomycin – Cystic fibrosis: Piperacillin/tazobactam or ceftazidime + tobramycin – Suspected MRSA: Add clindamycin or vancomycin |
Supportive Care
- Oxygen therapy to maintain SpO2 ≥92%
- Appropriate fluid management
- Antipyretics for fever (acetaminophen or ibuprofen)
- Chest physiotherapy (controversial, may be beneficial in specific cases)
- Nutritional support
- Monitor for clinical improvement or deterioration
Indications for Hospitalization
- Age younger than 3-6 months
- Moderate to severe respiratory distress
- Oxygen saturation <92% on room air
- Dehydration or inability to maintain oral intake
- Failed outpatient therapy
- Complications (pleural effusion, empyema, lung abscess)
- Immunocompromised status
- Underlying chronic conditions
- Unreliable caregivers or poor social situation
Nursing Management
Assessment
Nursing Diagnosis
Planning
Implementation
Evaluation
Assessment Focus Areas
- Respiratory status (rate, depth, effort, breath sounds)
- Vital signs including temperature
- Oxygen saturation
- Hydration status
- Nutritional intake
- Level of comfort/pain
- Response to medications
Common Nursing Diagnoses
- Ineffective breathing pattern
- Impaired gas exchange
- Ineffective airway clearance
- Hyperthermia
- Risk for dehydration
- Imbalanced nutrition: less than body requirements
- Activity intolerance
- Anxiety (child and/or parents)
Nursing Interventions
- Respiratory support:
- Position for optimal lung expansion (elevate head of bed 30-45°)
- Administer oxygen therapy as prescribed
- Monitor respiratory status and oxygen saturation
- Suction as needed to clear secretions
- Medication administration:
- Administer antibiotics on schedule
- Provide antipyretics for fever
- Administer bronchodilators if ordered
- Monitor for medication effectiveness and adverse effects
- Fluid and nutritional management:
- Encourage oral fluids if tolerated
- Administer IV fluids if ordered
- Monitor intake and output
- Provide small, frequent, nutritious meals
- Comfort measures:
- Provide pain relief as needed
- Ensure adequate rest periods
- Maintain comfortable room temperature
- Provide emotional support to child and family
Patient & Family Education
- Explanation of pneumonia and its treatment
- Importance of completing the full course of antibiotics
- Signs and symptoms that require medical attention
- Proper hand hygiene and cough etiquette
- Importance of adequate rest and hydration
- Avoidance of smoke exposure
- Value of pneumococcal and influenza vaccinations
Clinical Pearl
For children sent home on oral antibiotics, stress the importance of completing the full course even if symptoms improve. Schedule a follow-up appointment to evaluate response to treatment. Children who fail to show improvement within 48-72 hours of antibiotic therapy should be reassessed for possible complications or incorrect diagnosis.
Complications
- Pleural effusion/empyema: Collection of fluid or pus in the pleural space
- Pneumothorax: Air in the pleural space
- Lung abscess: Localized collection of pus within the lung parenchyma
- Necrotizing pneumonia: Destruction of lung tissue
- Respiratory failure: Inadequate gas exchange requiring mechanical ventilation
- Sepsis: Systemic inflammatory response to infection
- Long-term sequelae: Bronchiectasis, restrictive lung disease (rare)
Prevention
- Immunizations: Pneumococcal conjugate vaccine (PCV13), Haemophilus influenzae type b (Hib), annual influenza vaccine
- Hand hygiene: Regular handwashing
- Avoid exposure: Limit contact with sick individuals
- Avoid smoke exposure: Tobacco smoke increases risk
- Breastfeeding: Provides passive immunity to infants
- Adequate nutrition: Maintains immune function
Clinical Pearl
The introduction of pneumococcal conjugate vaccine (PCV) has dramatically reduced the incidence of invasive pneumococcal disease, including pneumonia, in children. Ensure all children receive age-appropriate vaccinations according to the recommended schedule.
Childhood Asthma
Definition & Significance
Asthma is a chronic inflammatory disorder of the airways characterized by variable expiratory airflow limitation, bronchial hyperresponsiveness, and underlying inflammation. It is one of the most common chronic diseases in childhood and a leading cause of school absences, emergency department visits, and hospitalizations.
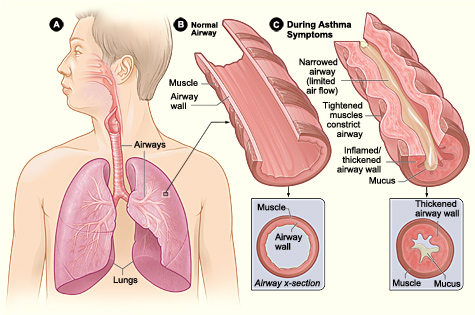
Comparison of normal airway and airway during asthma attack, showing bronchial constriction, inflammation, and excess mucus production
Epidemiology
- Over 6 million (6.5%) children in the United States have asthma
- Prevalence increases with age: 1.9% in ages 0-4 to 7.7% in ages 5-14
- Higher prevalence in boys than girls before age 20
- Approximately 20% of infants experience wheezing with respiratory infections, but 60% outgrow it by age 6
- Higher prevalence (10.1%) in Black children compared to White children (8.1%)
- Highest morbidity and mortality among underrepresented minorities and those living below the poverty line
Risk Factors & Etiology
Genetic Factors
- Family history of asthma or atopy
- Specific genetic markers (ORMDL3, GSDMB, IL33, TSLP genes)
- Epigenetic changes due to environmental exposures
- Atopy (genetic predisposition to produce IgE antibodies)
Environmental Factors
- Prenatal/Perinatal: Maternal smoking, prematurity, maternal age
- Allergen exposure: Dust mites, pet dander, cockroaches, molds, pollens
- Infections: Respiratory syncytial virus (RSV), human rhinovirus
- Irritants: Tobacco smoke, air pollution, strong odors
- Other: Obesity, early puberty, vitamin D deficiency
Mnemonic: ASTHMA Triggers
- Allergens (dust mites, pet dander, pollens, molds)
- Smoke (tobacco, wood, incense)
- Temperature changes (cold air)
- Hormonal changes (puberty)
- Medications (NSAIDs, beta-blockers)
- Activity (exercise, crying, laughing)
Pathophysiology
Asthma involves complex interactions between inflammatory cells, mediators, and the airway epithelium, leading to three main characteristics:
Airway Inflammation
- Activated mast cells release inflammatory mediators
- T-helper 2 (Th2) lymphocytes produce cytokines (IL-4, IL-5, IL-13)
- IgE antibodies bind to mast cells and basophils
- Allergen exposure causes degranulation and release of histamine, leukotrienes
- Influx of inflammatory cells (eosinophils, neutrophils, monocytes)
Airflow Obstruction
- Acute bronchoconstriction from smooth muscle contraction
- Airway edema due to increased vascular permeability
- Mucus hypersecretion causing airway plugging
- Airway remodeling from chronic inflammation
- Restriction of airflow, especially during exhalation
Bronchial Hyperresponsiveness
- Exaggerated bronchoconstrictor response to stimuli
- Altered breathing patterns
- Excessive smooth muscle contraction
- Enhanced sensitivity of neural pathways
- Structural changes from remodeling
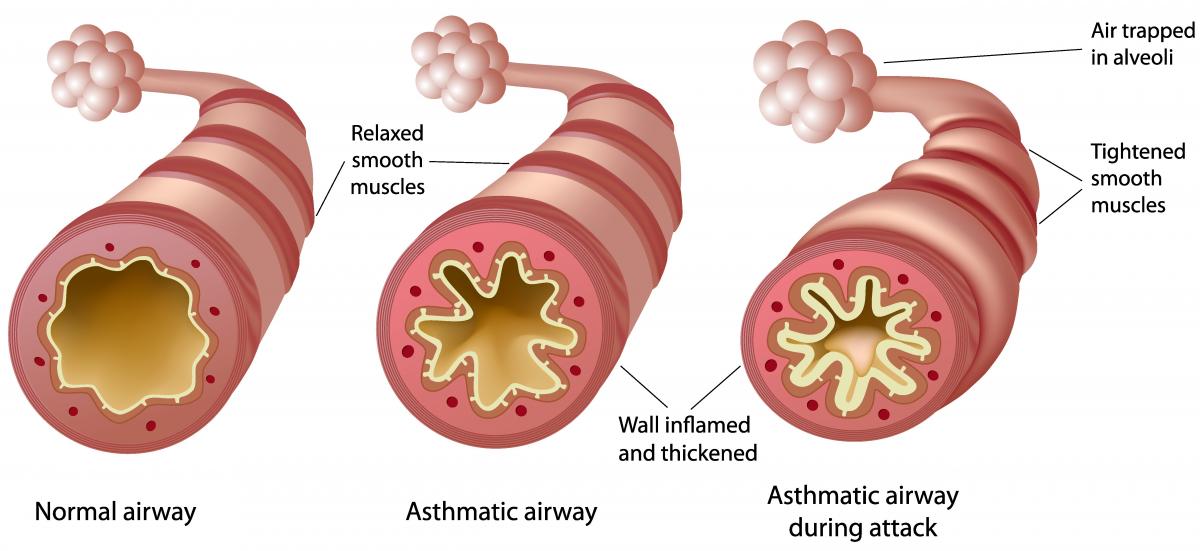
Pathological changes in asthmatic airways, showing inflammation, muscle hypertrophy, and mucus hypersecretion
Clinical Pearl
Airway remodeling may begin early in childhood asthma, even before symptoms become apparent. This process includes thickening of the basement membrane, collagen deposition, and shedding of epithelial cells, potentially leading to irreversible changes in the airways and accelerated decline in lung function, especially in children with severe and early-onset asthma.
Clinical Manifestations
Signs and Symptoms of Childhood Asthma
Chronic/Recurring Symptoms:
- Recurrent cough (may be only symptom)
- Wheezing, especially with exhalation
- Shortness of breath with activity
- Chest tightness or pain (in older children)
- Nighttime awakening with symptoms
- Symptoms that worsen with triggers
- Decreased exercise tolerance
- Frequent respiratory infections
Acute Exacerbation Findings:
- Tachypnea
- Audible wheezing
- Prolonged expiratory phase
- Use of accessory muscles
- Nasal flaring
- Retractions (intercostal, subcostal, supraclavicular)
- Inability to speak in complete sentences
- Tripod positioning
- Decreased air entry
- Hypoxemia
Clinical Pearl
Warning signs of severe or life-threatening asthma include altered mental status, lethargy, cyanosis, “silent chest” (absence of wheezing due to severe obstruction), and poor respiratory effort after initial distress. These signs indicate impending respiratory failure and require immediate intervention.
Diagnostic Evaluation
For Children 5 Years and Older
- Spirometry: Key diagnostic test showing obstructive pattern
- FEV1 less than 80% predicted
- FEV1/FVC ratio less than 0.85 or 85%
- Improvement in FEV1 of ≥12% (or ≥8% in children) after bronchodilator indicates significant reversibility
- Bronchoprovocation testing: For those with normal spirometry but suspected asthma
- Methacholine challenge
- Exercise challenge
- Cold air challenge
- Allergy testing: Skin testing or specific IgE blood testing to identify triggers
- Fractional exhaled nitric oxide (FeNO): Measures eosinophilic airway inflammation (elevated in some asthma patients)
- Peak flow measurements: Serial measurements to assess variability and response to treatment
For Children Under 5 Years
Diagnosis is more challenging and relies on:
- Pattern of symptoms (recurrent wheezing, cough, breathing difficulty)
- Symptom triggers and timing
- Family history of asthma or atopy
- Response to trial of asthma medication
- Exclusion of alternative diagnoses
Mnemonic: ASTHMA for Diagnosis in Young Children
- Atopic history (personal or family)
- Symptoms that recur and vary in intensity
- Triggers that consistently cause symptoms
- History of nighttime cough or symptoms
- Medication response (improvement with bronchodilator or ICS)
- Alternate diagnoses ruled out
Asthma Classification and Stepwise Management
Classification by Severity (Initial Assessment)
| Classification | Symptom Frequency | Nighttime Awakenings | SABA Use | Activity Limitation | Lung Function |
|---|---|---|---|---|---|
| Intermittent | ≤2 days/week | ≤2 times/month | ≤2 days/week | None | FEV1 >80% predicted Normal FEV1/FVC |
| Mild Persistent | >2 days/week but not daily | 3-4 times/month | >2 days/week but not daily | Minor limitation | FEV1 ≥80% predicted Normal FEV1/FVC |
| Moderate Persistent | Daily | >1 time/week but not nightly | Daily | Some limitation | FEV1 60-80% predicted Reduced FEV1/FVC |
| Severe Persistent | Throughout the day | Often 7 times/week | Several times per day | Extremely limited | FEV1 <60% predicted Reduced FEV1/FVC |
Stepwise Approach to Treatment (Children 5-11 Years)
| Step | Preferred Controller | Alternative Controller | Quick-Relief Medication |
|---|---|---|---|
| Step 1 (Intermittent) |
None | None | SABA as needed for symptoms Intensity of treatment depends on severity of symptoms |
| Step 2 (Mild Persistent) |
Low-dose ICS | Cromolyn, LTRA, Nedocromil, or Theophylline | |
| Step 3 (Moderate Persistent) |
Low-dose ICS + LABA OR Medium-dose ICS |
Low-dose ICS + LTRA, Theophylline, or Zileuton | |
| Step 4 | Medium-dose ICS + LABA | Medium-dose ICS + LTRA, Theophylline, or Zileuton | |
| Step 5 | High-dose ICS + LABA | High-dose ICS + LTRA, Theophylline, or Zileuton | |
| Step 6 (Severe Persistent) |
High-dose ICS + LABA + oral corticosteroids | Consider biologics (omalizumab for allergic asthma, mepolizumab for eosinophilic asthma) |
Abbreviations: ICS = inhaled corticosteroid; LABA = long-acting beta2-agonist; LTRA = leukotriene receptor antagonist; SABA = short-acting beta2-agonist
Clinical Pearl
The stepwise approach involves both “stepping up” (intensifying treatment until control is achieved) and “stepping down” (reducing treatment when control is maintained). Reassess control every 3-6 months, and if well controlled for at least 3 months, consider gradually stepping down therapy to identify the minimum effective treatment.
Pharmacological Management
Quick-Relief Medications
- Short-acting beta2-agonists (SABAs):
- Albuterol (most common)
- Levalbuterol
- Onset: 5-15 minutes, Duration: 4-6 hours
- Used for acute symptom relief and prevention of exercise-induced bronchoconstriction
- Anticholinergics:
- Ipratropium bromide
- Usually added to SABA in acute severe exacerbations
- Systemic corticosteroids:
- Prednisone, prednisolone, dexamethasone
- Used for moderate to severe exacerbations
- Short courses (3-5 days) usually sufficient
Controller Medications
- Inhaled corticosteroids (ICS):
- Fluticasone, budesonide, beclomethasone, mometasone
- First-line controller therapy
- Reduce airway inflammation
- Long-acting beta2-agonists (LABAs):
- Salmeterol, formoterol
- Always used with ICS, never as monotherapy
- Leukotriene modifiers:
- Montelukast, zafirlukast, zileuton
- Alternative or add-on therapy
- Particularly useful for allergic asthma, exercise-induced bronchoconstriction
- Biological agents (for severe asthma):
- Omalizumab (anti-IgE) for allergic asthma
- Mepolizumab, reslizumab (anti-IL-5) for eosinophilic asthma
- Dupilumab (anti-IL-4/IL-13) for Type 2 inflammation
Delivery Devices
Metered Dose Inhalers (MDIs)
- Pressurized canister with medication
- Always use with spacer/valved holding chamber in children
- Face mask for children under 4-5 years
- Requires coordination of actuation and inhalation
Dry Powder Inhalers (DPIs)
- Breath-activated (no propellant)
- Requires adequate inspiratory flow
- Generally for children 5-6 years and older
- No spacer needed
Nebulizers
- Converts liquid medication to mist
- Useful for infants, young children, or during severe exacerbations
- Minimal coordination required
- Time-consuming, less portable
Clinical Pearl
Proper inhaler technique is crucial for effective medication delivery. MDIs with valved holding chambers/spacers are as effective as nebulizers in most clinical situations. Regularly assess and reinforce proper inhaler technique at every visit. For most children, 5-10 normal breaths are needed to empty a spacer.
Management of Acute Asthma Exacerbations
Initial Assessment
Assess severity, vital signs, oxygen saturation, work of breathing
Initial Treatment
Oxygen (if SpO2 <92%), SABA (2-6 puffs or nebulized), consider oral corticosteroids
Reassessment (15-20 minutes)
Evaluate response to initial treatment
Good Response
Continue SABA every 4-6h
Consider discharge
Incomplete Response
Continue SABA + add ipratropium
Consider hospitalization
Poor Response
Add continuous SABA, IV magnesium
Consider ICU
Home Management of Mild Exacerbations
- Administer SABA (2-4 puffs via MDI with spacer or nebulized treatment)
- Repeat every 20 minutes for up to 3 doses if needed
- If good response, continue SABA every 4-6 hours as needed
- If incomplete response after 3 treatments, add oral corticosteroids and contact healthcare provider
- Seek emergency care for severe symptoms, significant distress, or lack of improvement
Emergency Department/Hospital Management
- Initial assessment and treatment:
- Oxygen to maintain SpO2 ≥92%
- SABA via MDI with spacer or nebulizer (up to 3 treatments in first hour)
- Ipratropium bromide for moderate-severe exacerbations
- Systemic corticosteroids for moderate-severe exacerbations
- For severe exacerbations or poor response:
- Continuous SABA nebulization
- IV magnesium sulfate (25-75 mg/kg, max 2g)
- Consider IV terbutaline for impending respiratory failure
- Consider non-invasive positive pressure ventilation
- Prepare for possible intubation if deteriorating
Clinical Pearl
Heliox (helium-oxygen mixture) may be beneficial in severe exacerbations not responding to standard therapy by reducing airflow resistance and work of breathing. Early administration of systemic corticosteroids reduces hospitalization rates and speeds recovery. Consider IV magnesium sulfate for children with FEV1 <60% predicted who fail to respond to initial treatment.
Nursing Management
Assessment
- Respiratory status (rate, depth, pattern, use of accessory muscles)
- Oxygen saturation and vital signs
- Breath sounds (presence and character of wheezing, air entry)
- Level of consciousness and activity
- Medication use and adherence
- Inhaler technique
- Trigger identification and exposure
- Impact on daily activities and quality of life
Common Nursing Diagnoses
- Ineffective breathing pattern
- Ineffective airway clearance
- Impaired gas exchange
- Activity intolerance
- Anxiety related to breathlessness
- Deficient knowledge regarding asthma management
- Risk for infection
- Sleep pattern disturbance
- Ineffective health maintenance
Nursing Interventions
- Acute care interventions:
- Position for optimal breathing (usually upright or leaning forward)
- Administer oxygen and medications as prescribed
- Monitor response to treatment
- Maintain calm environment to reduce anxiety
- Ensure adequate hydration
- Education and health promotion:
- Teach proper inhaler technique and medication administration
- Explain differences between controller and rescue medications
- Assist with developing an Asthma Action Plan
- Educate about symptom recognition and early intervention
- Teach peak flow monitoring if appropriate
- Provide guidance on trigger avoidance
- Psychosocial support:
- Address fears and concerns about asthma
- Provide age-appropriate education to child
- Involve child in self-management as appropriate for age
- Connect family with support resources
- Address potential barriers to adherence
Mnemonic: ASTHMA Nursing Care
- Assess respiratory status and response to therapy
- Spacers and proper inhaler technique teaching
- Trigger identification and avoidance strategies
- Help develop and review Asthma Action Plan
- Medication adherence promotion
- Anticipatory guidance for school, exercise, and lifestyle
Patient and Family Education
Asthma Education Components
Disease Understanding
- Basic pathophysiology of asthma
- Chronic nature of the condition
- Recognition of symptoms
- Importance of ongoing management
Medications
- Purpose of each medication
- Difference between controllers and relievers
- Proper administration technique
- Potential side effects and when to report
- Importance of adherence even when asymptomatic
Self-Monitoring
- Symptom recognition
- Peak flow monitoring if applicable
- Keeping an asthma diary
- Identifying patterns in symptoms
Asthma Action Plan
- Green zone: Maintenance care when well
- Yellow zone: Actions for mild symptoms
- Red zone: Emergency actions for severe symptoms
- When to seek medical help
- Emergency contact information
Trigger Management
- Identification of personal triggers
- Environmental control measures
- Allergen avoidance strategies
- Managing exercise-induced symptoms
- Infection prevention (handwashing, vaccinations)
School and Activity Management
- School asthma management plan
- Exercise modifications if needed
- Communication with teachers and coaches
- Planning for field trips and special events
Clinical Pearl
Asthma education should be continuous, reinforced at every visit, and adjusted based on the child’s developmental stage. Involving children in their asthma management from an early age helps them develop self-management skills as they grow. Use age-appropriate teaching methods, such as games, videos, and interactive demonstrations for young children, and more complex explanations and smartphone apps for adolescents.
Long-term Management and Follow-up
- Regular follow-up visits:
- Every 1-6 months depending on control
- Assess symptom control and lung function
- Review medication technique and adherence
- Adjust treatment as needed
- Monitoring tools:
- Symptom diaries
- Asthma Control Test (ACT) or Childhood Asthma Control Test (C-ACT)
- Peak flow monitoring for some children
- Periodic spirometry
- Preventive care:
- Annual influenza vaccination
- Pneumococcal vaccination for high-risk patients
- Regular dental check-ups
- Prompt treatment of respiratory infections
- Specialist referral indications:
- Diagnostic uncertainty
- Poor control despite appropriate therapy
- Severe or life-threatening exacerbations
- Need for additional diagnostic testing
- Consideration for biological therapy
- Significant comorbidities
Special Considerations
- Exercise-induced bronchoconstriction (EIB):
- Pre-treat with SABA 15-30 minutes before exercise
- Warm-up period before vigorous activity
- Consider daily controller therapy if frequent symptoms
- Indoor, warm environments may be better tolerated
- Asthma in adolescents:
- Address adherence challenges
- Screen for risk-taking behaviors (smoking, vaping)
- Support transition to self-management
- Consider impact on quality of life and peer relationships
- Comorbidities:
- Allergic rhinitis (often coexists, may worsen asthma)
- Gastroesophageal reflux disease (GERD)
- Obesity (associated with more difficult control)
- Obstructive sleep apnea
- Anxiety and depression
Clinical Pearl
Childhood asthma is often characterized by a variable course, with some children experiencing remission as they grow older. However, severe asthma, persistent symptoms in early life, and presence of atopy are associated with persistence into adulthood. Even during symptom-free periods, the potential for airway remodeling continues, highlighting the importance of maintaining appropriate controller therapy.
Summary and Key Points
Pneumonia
- Leading cause of morbidity and mortality in children under 5 years
- Etiology varies by age with viruses predominant in younger children
- Clinical presentation includes fever, cough, tachypnea, and respiratory distress
- Diagnosis based on clinical findings; chest X-ray not always necessary
- Treatment guided by age and likely pathogens
- Prevention includes vaccination and reducing risk factors
Asthma
- Chronic inflammatory airway disease with variable expiratory airflow limitation
- Results from complex interaction of genetic and environmental factors
- Characterized by recurrent episodes of wheezing, coughing, and breathing difficulty
- Stepwise approach to treatment based on severity and control
- Education and self-management are cornerstones of care
- Regular monitoring and follow-up essential for long-term control
Nursing Priorities for Both Conditions
- Careful respiratory assessment and monitoring
- Proper medication administration
- Comprehensive patient and family education
- Recognition of warning signs requiring urgent intervention
- Promotion of preventive measures
- Support for adherence to treatment plans
Created for nursing education purposes. Prepared by Soumya Ranjan Parida.
