Pediatric Rheumatic Fever & Rheumatic Heart Disease
Comprehensive Nursing Notes
Introduction
Rheumatic Fever (RF) is a multisystem inflammatory disease that occurs as a delayed consequence of untreated group A streptococcal (GAS) pharyngeal infection. It primarily affects children between 5-15 years of age and can lead to significant cardiac complications.
Rheumatic Heart Disease (RHD) represents the cardiac manifestation of RF, characterized by permanent damage to heart valves that develops after repeated episodes of acute rheumatic fever or following a severe initial episode.
Key Insight
While RF is acute and usually self-limiting, RHD is a chronic condition that can cause lifelong cardiac complications. Proper nursing management is critical in both immediate care and long-term prevention of recurrent episodes and complications.
Rheumatic Fever
- Acute, inflammatory, autoimmune response
- Follows untreated group A streptococcal throat infection
- Usually affects children 5-15 years old
- Self-limiting but can recur
- Diagnosed using Jones Criteria
Rheumatic Heart Disease
- Chronic sequela of rheumatic fever
- Progressive valvular damage (primarily mitral and aortic)
- Can lead to heart failure
- Preventable with proper antibiotic prophylaxis
- May require surgical intervention
Pathophysiology
Pathogenesis of Rheumatic Fever
Initial GAS Infection
Pharyngeal infection with group A β-hemolytic streptococcus (Streptococcus pyogenes).
Latent Period (2-3 weeks)
Asymptomatic period between the streptococcal infection and the onset of rheumatic fever symptoms.
Molecular Mimicry
Antibodies produced against GAS antigens cross-react with human tissues due to structural similarities (molecular mimicry).
Autoimmune Response
The immune system attacks the body’s own tissues, particularly affecting the heart, joints, skin, and brain.
Tissue Inflammation
Inflammation of affected tissues leads to the clinical manifestations of RF, including carditis, arthritis, and other symptoms.
Clinical Insight
The pathophysiology of RF involves type II hypersensitivity reactions (antibody-mediated) targeting heart valves, particularly the mitral valve, leading to valvulitis and eventual valve scarring if recurrent episodes occur.
Molecular Mimicry in Rheumatic Fever

Figure 1: Pathogenesis of Acute Rheumatic Fever showing molecular mimicry between streptococcal M protein and human cardiac tissue
Progression to Rheumatic Heart Disease
Rheumatic heart disease develops as a consequence of valvular damage caused during the acute phase of rheumatic fever. The progression typically follows this pattern:
Valvulitis
Initial inflammation of heart valves during acute RF, primarily affecting the mitral valve, followed by the aortic valve.
Anitschkow Bodies (Anitschow Nodules)
Characteristic histological finding in RF – fibrinoid degeneration with granulomatous lesions called Anitschkow bodies in the myocardium.
Valve Leaflet Changes
Thickening of valve leaflets with fusion of the commissures and shortening of chordae tendineae leading to valve stenosis and/or regurgitation.
Progressive Valve Damage
Recurrent episodes of RF cause cumulative damage, leading to chronic rheumatic heart disease with permanent valve deformity.
Complications
Progression to heart failure, atrial fibrillation, thromboembolic events, and infective endocarditis may occur in severe cases.
Rheumatic Heart Disease – Valve Pathology
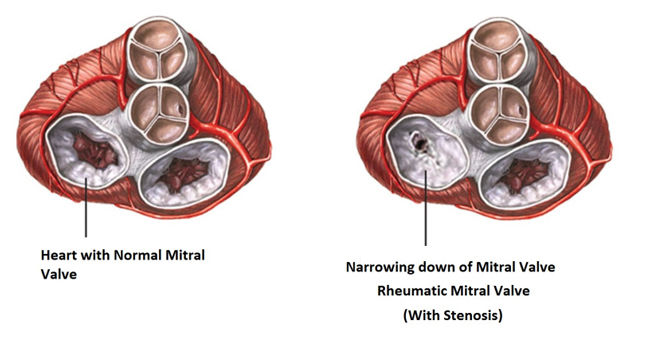
Figure 2: Comparison of normal heart valve and valve damaged by rheumatic heart disease
Epidemiology and Risk Factors
Epidemiology
- Primarily affects children aged 5-15 years
- More common in developing countries and resource-limited settings
- Global burden: 33 million cases of RHD worldwide
- Annual incidence of acute RF: 300,000-500,000 cases globally
- More prevalent in areas with overcrowding and limited access to healthcare
- Declining incidence in developed countries due to improved living conditions and antibiotic availability
Risk Factors
Non-modifiable Risk Factors
- Genetic predisposition
- Age (5-15 years)
- History of previous rheumatic fever
Modifiable Risk Factors
- Untreated group A streptococcal pharyngitis
- Overcrowded living conditions
- Poor access to healthcare
- Low socioeconomic status
- Poor hygiene practices
- Inadequate or incomplete antibiotic treatment
Clinical Alert
Children who have had a previous episode of rheumatic fever have a significantly increased risk (up to 50%) of developing recurrent episodes if exposed to group A streptococcal infection, highlighting the critical importance of secondary prophylaxis.
Clinical Manifestations
The clinical presentation of rheumatic fever is diverse and involves multiple organ systems. The major manifestations are summed up in the Jones criteria, but the full spectrum of signs and symptoms is broader.
| Manifestation | Clinical Features | Nursing Assessment Findings |
|---|---|---|
| Carditis |
|
|
| Polyarthritis |
|
|
| Sydenham’s Chorea |
|
|
| Erythema Marginatum |
|
|
| Subcutaneous Nodules |
|
|
Minor Manifestations and General Symptoms
Fever
Temperature ≥38.5°C (101.3°F) in low-risk populations or ≥38°C (100.4°F) in moderate/high-risk populations.
Arthralgia
Joint pain without objective evidence of inflammation. Often affects large joints and may be migratory.
Elevated Acute Phase Reactants
Elevated ESR (≥60 mm/h) and/or CRP (≥3.0 mg/dL) in low-risk or ESR ≥30 mm/h in higher-risk populations.
Prolonged PR Interval
Electrocardiographic finding of first-degree heart block (after accounting for age variability).
Fatigue and Malaise
General feeling of unwellness and low energy, often preceding more specific manifestations.
Abdominal Pain
May be present, especially in children, and can sometimes mimic acute abdomen.
Progression to Rheumatic Heart Disease
RHD develops in approximately 60-80% of patients with carditis during acute RF, particularly after recurrent episodes. The most common valve lesions in pediatric RHD include:
Mitral Valve Involvement
- Most common valve affected (>70% of cases)
- Initially presents as mitral regurgitation
- May progress to mitral stenosis after repeated episodes
- Clinical findings: apical holosystolic murmur, left atrial enlargement
Aortic Valve Involvement
- Second most commonly affected valve
- Usually presents as aortic regurgitation
- Often occurs concurrently with mitral valve disease
- Clinical findings: early diastolic decrescendo murmur, widened pulse pressure
Rheumatic Heart Disease – Valvular Damage
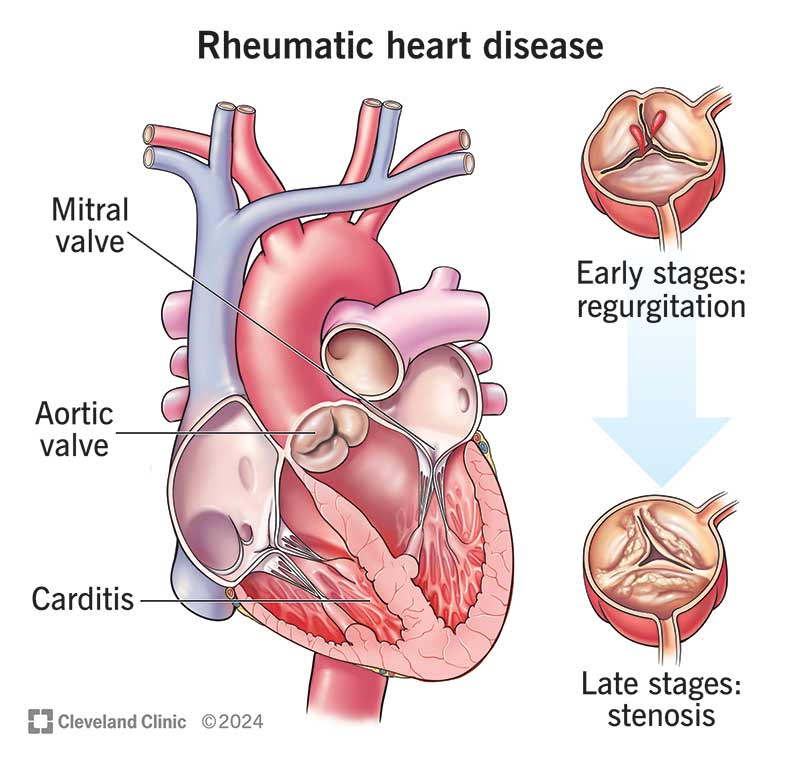
Figure 3: Illustration of heart valve damage in rheumatic heart disease
Diagnosis: The Jones Criteria
The diagnosis of acute rheumatic fever is based on the revised Jones criteria (2015), which categorize patients based on risk stratification and provide specific diagnostic parameters.
Clinical Importance
Evidence of preceding group A streptococcal infection is required for the diagnosis of rheumatic fever, regardless of which diagnostic criteria are met. This can be established through positive throat culture, rapid strep test, or elevated or rising antistreptococcal antibody titers.
| Revised Jones Criteria (2015) | |
|---|---|
| Diagnostic Requirements (with evidence of preceding GAS infection) | |
| Initial RF | 2 Major manifestations OR 1 Major + 2 Minor manifestations |
| Recurrent RF | 2 Major OR 1 Major + 2 Minor OR 3 Minor manifestations |
| Major Criteria | |
| Low-risk populations | Moderate/High-risk populations |
| Carditis (clinical and/or subclinical) | Carditis (clinical and/or subclinical) |
| Polyarthritis only | Monoarthritis or polyarthritis or polyarthralgia |
| Chorea | Chorea |
| Erythema marginatum | Erythema marginatum |
| Subcutaneous nodules | Subcutaneous nodules |
| Minor Criteria | |
| Low-risk populations | Moderate/High-risk populations |
| Polyarthralgia | Monoarthralgia |
| Fever (≥38.5°C) | Fever (≥38°C) |
| ESR ≥60 mm/h and/or CRP ≥3.0 mg/dL | ESR ≥30 mm/h and/or CRP ≥3.0 mg/dL |
| Prolonged PR interval (after accounting for age) | Prolonged PR interval (after accounting for age) |
JONES Mnemonic for Major Criteria
Joints
(Polyarthritis)
Oh, my heart!
(Carditis)
Nodules
(Subcutaneous)
Erythema
marginatum
Sydenham’s
chorea
Diagnostic Tests for Rheumatic Fever and RHD
Laboratory Tests
- Streptococcal Antibody Tests: ASO (anti-streptolysin O), anti-DNase B
- Acute Phase Reactants: ESR, CRP
- Complete Blood Count: Leukocytosis, normocytic anemia
- Throat Culture: May be positive for group A streptococcus
- Rapid Strep Test: May confirm recent GAS infection
Imaging and Other Tests
- Echocardiography: Gold standard for detecting subclinical carditis and valvular lesions
- Electrocardiogram: May show prolonged PR interval, other conduction abnormalities
- Chest X-ray: May show cardiomegaly in patients with significant carditis
- Joint X-rays: Usually normal despite symptoms (helps differentiate from other arthritides)
Nursing Assessment
A comprehensive nursing assessment is essential for patients with suspected or confirmed rheumatic fever or rheumatic heart disease. The assessment should focus on identifying key clinical manifestations and monitoring for complications.
Health History
- Recent Illness: History of sore throat or scarlet fever within past 2-4 weeks
- Previous Episodes: Any prior diagnosis of RF or RHD
- Family History: RF/RHD in family members
- Living Conditions: Crowding, socioeconomic status
- Medication History: Current medications, antibiotic use
- Symptom Assessment:
- Joint pain, swelling, redness
- Fever pattern and duration
- Any involuntary movements
- Rash or skin nodules
- Chest pain, palpitations, shortness of breath
- Fatigue or exercise intolerance
Physical Assessment
- Vital Signs:
- Temperature (fever ≥38°C)
- Heart rate (tachycardia)
- Respiratory rate (tachypnea)
- Blood pressure (hypotension in severe carditis)
- Cardiovascular Assessment:
- Heart sounds and murmurs
- Presence of friction rub
- Signs of heart failure (JVD, hepatomegaly, edema)
- Musculoskeletal Assessment:
- Joint examination (swelling, warmth, redness, ROM)
- Subcutaneous nodules over bony prominences
- Skin Assessment:
- Erythema marginatum (transient, non-pruritic rash)
- Neurological Assessment:
- Involuntary movements (chorea)
- Coordination and muscle strength
- Emotional lability
Nursing Assessment Tip
The migratory nature of joint pain is a distinctive feature of RF. During assessment, document which joints have been affected, when symptoms began in each joint, and whether symptoms have resolved in previously affected joints.
Focused RHD Assessment
For patients with established RHD, additional assessment parameters include:
Functional Capacity
Assess using New York Heart Association (NYHA) classification:
- Class I: No limitation of activity
- Class II: Slight limitation of activity
- Class III: Marked limitation of activity
- Class IV: Unable to carry out any physical activity without discomfort
Compliance Assessment
- Adherence to antibiotic prophylaxis
- Regular follow-up attendance
- Dental hygiene practices
- Understanding of endocarditis prophylaxis
- Medication adherence (diuretics, etc.)
Complications Monitoring
- Signs of heart failure progression
- Arrhythmias (especially atrial fibrillation)
- Embolic events
- Infective endocarditis
- Pulmonary hypertension
- Growth and development in children
Nursing Diagnosis
Based on comprehensive assessment findings, several nursing diagnoses may be appropriate for patients with rheumatic fever and rheumatic heart disease. Priority nursing diagnoses include:
Acute Pain
Related to: Joint inflammation, carditis, arthritis
Evidenced by: Verbal reports of pain, guarding behavior, facial expressions of pain, changes in vital signs
Goal: Patient will verbalize decreased pain intensity (pain score ≤3/10) and demonstrate increased comfort.
Decreased Cardiac Output
Related to: Valvular dysfunction, myocardial inflammation, altered heart rhythm
Evidenced by: Tachycardia, dyspnea, fatigue, edema, abnormal heart sounds, arrhythmias
Goal: Patient will maintain adequate cardiac output as evidenced by stable vital signs, absence of dysrhythmias, and improved activity tolerance.
Hyperthermia
Related to: Inflammatory process, immune response to streptococcal infection
Evidenced by: Elevated body temperature, warm skin, tachycardia, flushed appearance
Goal: Patient will maintain normal body temperature between 36.5°C and 37.5°C.
Activity Intolerance
Related to: Decreased cardiac output, joint pain, generalized weakness, carditis
Evidenced by: Fatigue, dyspnea on exertion, abnormal heart rate or blood pressure response to activity
Goal: Patient will demonstrate increased activity tolerance and participate in activities appropriate to cardiac status.
Risk for Infection
Related to: Vulnerability to recurrent streptococcal infection, risk of endocarditis in RHD
Risk factors: History of RF/RHD, valvular damage, inadequate prophylaxis
Goal: Patient will remain free from infection as evidenced by normal temperature, absence of symptoms of infection, and normal WBC count.
Deficient Knowledge
Related to: Lack of exposure to information, unfamiliarity with disease process and management
Evidenced by: Questions, statements of misconception, inaccurate follow-through of instructions
Goal: Patient/family will verbalize understanding of RF/RHD, treatment regimen, and importance of prophylaxis.
Additional Nursing Diagnoses for RHD
Ineffective Tissue Perfusion
Related to impaired cardiac function and decreased cardiac output secondary to valvular disease.
Risk for Impaired Gas Exchange
Related to pulmonary congestion secondary to heart failure in severe RHD.
Disturbed Body Image
Related to physical limitations, surgical scars (if valve surgery is performed), and chronic illness.
Interrupted Family Processes
Related to child’s illness, hospitalization, and changes in family roles and functioning.
Risk for Ineffective Therapeutic Regimen Management
Related to complexity of prophylactic regimen, medication side effects, and long-term nature of treatment.
Anxiety
Related to uncertain prognosis, potential for complications, and impact on future lifestyle.
Nursing Management
Acute Phase Management
1. Pain Management
- Administer prescribed anti-inflammatory medications such as aspirin or NSAIDs
- Position affected joints for comfort and proper alignment
- Apply warm compresses to painful joints
- Implement gentle range-of-motion exercises when appropriate
- Assess pain regularly using age-appropriate pain scales
- Provide diversional activities to distract from pain
Note: The dose of aspirin for anti-inflammatory effects in RF is higher than for analgesia. Monitor for signs of salicylate toxicity such as tinnitus, hyperventilation, and GI distress.
2. Promoting Rest and Limited Activity
- Enforce bed rest during the acute febrile phase, especially with carditis
- Implement gradual activity progression based on clinical improvement
- Monitor vital signs before, during, and after activity
- Schedule nursing care to allow for adequate rest periods
- Assist with activities of daily living as needed
- Educate family about importance of activity restrictions
Tip: Create a daily schedule that balances rest and progressive activity to prevent deconditioning while protecting the heart.
3. Antibiotic Administration
- Administer antibiotics as prescribed to eradicate streptococcal infection:
- Penicillin V 250 mg orally twice daily for 10 days, or
- Benzathine penicillin G single IM injection
- For penicillin allergic patients: erythromycin or azithromycin
- Monitor for allergic reactions to antibiotics
- Ensure complete course of antibiotic treatment
- Teach family about importance of completing full antibiotic course
4. Cardiac Monitoring
- Assess heart rate, rhythm, and heart sounds every 4 hours
- Monitor for signs of heart failure (tachycardia, dyspnea, crackles, JVD)
- Monitor ECG for prolonged PR interval and arrhythmias
- Implement cardiac precautions
- Position patient for optimal cardiac function (semi-Fowler’s position)
- Monitor for chest pain and shortness of breath
5. Temperature Management
- Monitor temperature every 4 hours during acute phase
- Administer antipyretics as prescribed
- Provide tepid sponge baths for high fevers
- Ensure adequate hydration
- Maintain comfortable environmental temperature
- Document fever pattern
6. Management of Chorea
- Provide a safe environment to prevent injury from involuntary movements
- Implement fall precautions
- Pad bed rails if necessary
- Assist with feeding and self-care activities
- Administer sedatives or antiepileptic medications if prescribed
- Provide emotional support and reassurance
- Educate family that chorea is self-limiting (typically resolves in 2-3 months)
Long-term Management and RHD Care
1. Secondary Prophylaxis
- Administer long-term prophylactic antibiotics:
- Benzathine penicillin G 1.2 million units IM every 3-4 weeks, or
- Penicillin V 250 mg orally twice daily, or
- Sulfadiazine or erythromycin for penicillin-allergic patients
- Educate about importance of adherence to prophylaxis regimen
- Discuss duration of prophylaxis (5+ years, possibly lifelong with severe RHD)
- Teach injection techniques if home administration is planned
- Coordinate with primary care for regular follow-up
Important: Secondary prophylaxis is the most effective strategy for preventing recurrent RF episodes and progression of RHD.
2. Heart Failure Management
- Administer medications as prescribed:
- Diuretics for fluid overload
- ACE inhibitors to reduce afterload
- Digoxin for inotropic support
- Monitor fluid status and daily weights
- Implement sodium and fluid restriction as prescribed
- Position for optimal respiratory function
- Monitor for signs of worsening heart failure
- Assess for medication side effects
3. Endocarditis Prevention
- Educate about need for antibiotic prophylaxis before dental procedures
- Promote good oral hygiene
- Teach signs and symptoms of endocarditis
- Emphasize importance of prompt treatment of infections
- Provide endocarditis prophylaxis wallet card
4. Activity and Exercise Guidelines
- Develop individualized activity plan based on severity of cardiac involvement
- Implement progressive return to activities after acute phase
- Collaborate with physical therapy for exercise prescription
- Guide parents regarding school attendance and physical education participation
- Teach recognition of activity intolerance symptoms
- Recommend appropriate sports and activities based on cardiac status
5. Preoperative and Postoperative Care for Valve Surgery
For patients with severe RHD who require valve repair or replacement:
Preoperative Care:
- Provide age-appropriate preoperative teaching
- Ensure antibiotic prophylaxis as ordered
- Complete preoperative assessments
- Prepare family for ICU environment
- Address anxiety and fears
Postoperative Care:
- Monitor hemodynamic status closely
- Assess for bleeding and infection
- Provide pain management
- Implement cardiac rehabilitation protocol
- Teach anticoagulation management (for mechanical valves)
- Prepare for discharge and home care
Patient and Family Education
Disease Information
- Pathophysiology of RF and RHD
- Relationship between strep throat and RF
- Long-term implications and complications
- Importance of early treatment of strep infections
Medication Management
- Antibiotic prophylaxis schedule
- Importance of adherence
- Potential side effects
- What to do if a dose is missed
- Medication interactions
Prevention Strategies
- Prompt treatment of sore throats
- Good hand hygiene
- Avoiding crowded conditions when possible
- Dental hygiene and prophylaxis
- Prompt reporting of fever or other symptoms
Follow-up Care
- Importance of regular medical follow-up
- Schedule for echocardiograms and other tests
- When to seek immediate medical attention
- Coordination between specialists (cardiology, rheumatology)
- Need for dental follow-up and prophylaxis
Lifestyle Adaptations
- Activity recommendations and restrictions
- School accommodations if needed
- Nutritional guidance (especially with heart failure)
- Emotional support resources
- Community resources and support groups
- Future planning (career, pregnancy considerations for adolescents)
Prevention and Prophylaxis
Primary Prevention
Primary prevention focuses on preventing the initial attack of RF by promptly treating streptococcal pharyngitis.
Recommended Antibiotic Regimens for Strep Throat
- First Line: Penicillin V 250mg (children) or 500mg (adolescents) orally 2-3 times daily for 10 days
- Alternative: Benzathine penicillin G single IM injection:
- 600,000 units for children <27kg
- 1.2 million units for children ≥27kg and adults
- For Penicillin Allergy:
- Erythromycin 20-40 mg/kg/day in 2-4 divided doses for 10 days
- Azithromycin 12 mg/kg once daily (max 500 mg) for 5 days
- Clarithromycin 15 mg/kg/day in two divided doses for 10 days
Primary Prevention Tip
Educate families that all sore throats warrant medical attention, especially in children with a history of RF. Early diagnosis and treatment of strep throat can prevent RF in 90% of cases.
Secondary Prevention
Secondary prevention focuses on preventing recurrent attacks of RF in patients who have already had RF or have RHD.
Secondary Prophylaxis Regimens
- Preferred: Benzathine penicillin G IM injection:
- 1.2 million units every 4 weeks (every 3 weeks in high-risk areas)
- For weight <30kg: 600,000 units every 4 weeks
- Alternative: Penicillin V 250 mg orally twice daily
- For Penicillin Allergy:
- Sulfadiazine 500 mg once daily (weight <27kg) or 1g once daily (≥27kg)
- Erythromycin 250 mg twice daily
Duration of Secondary Prophylaxis
| Category | Duration |
|---|---|
| RF with carditis and residual heart disease (persistent valvular disease) | 10 years since last episode and at least until age 40 (lifelong may be considered) |
| RF with carditis but no residual heart disease | 10 years or until age 21, whichever is longer |
| RF without carditis | 5 years or until age 21, whichever is longer |
Endocarditis Prophylaxis in RHD
Patients with RHD are at increased risk for infective endocarditis and require prophylaxis before certain procedures.
Procedures Requiring Prophylaxis
- All dental procedures that involve manipulation of gingival tissue or perforation of oral mucosa
- Invasive procedures involving respiratory tract
- Procedures involving infected skin, skin structures, or musculoskeletal tissue
- Certain GI or GU procedures in the presence of infection
Endocarditis Prophylaxis Regimens
- Standard Prophylaxis (Oral): Amoxicillin 50 mg/kg (max 2g) 1 hour before procedure
- Unable to Take Oral Medication: Ampicillin 50 mg/kg (max 2g) IM/IV or Cefazolin/Ceftriaxone 50 mg/kg (max 1g) IM/IV within 30 minutes of procedure
- Penicillin Allergy (Oral): Clindamycin 20 mg/kg (max 600mg) or Azithromycin 15 mg/kg (max 500mg) 1 hour before procedure
- Penicillin Allergy (IV/IM): Clindamycin 20 mg/kg (max 600mg) IV within 30 minutes of procedure
Mnemonics for Clinical Practice
JONES: Major Criteria for RF Diagnosis
Joints (Polyarthritis)
Oh my heart! (Carditis)
Nodules (Subcutaneous)
Erythema marginatum
Sydenham’s chorea
FEVER: Minor Criteria for RF Diagnosis
Fever
ESR/CRP elevation
Values of PR interval (prolonged)
Extra heart ache (arthralgia)
Recent strep infection
HEART: Complications of RHD
- Heart failure
- Endocarditis (infective)
- Atrial fibrillation
- Regurgitation and stenosis (valve lesions)
- Thromboembolism
ABCDE: Secondary Prophylaxis Teaching
- Antibiotic regimen: explain type, dose, frequency
- Be consistent: emphasize importance of adherence
- Calendar marking: track injections/doses
- Duration: explain how long prophylaxis will continue
- Educate about when to seek medical help
Comprehensive Mind Map
Pathophysiology
- Group A streptococcal infection
- Molecular mimicry
- Autoimmune response
- Inflammation of target tissues
- Valvular damage in RHD
Clinical Manifestations
Major
- Carditis
- Polyarthritis
- Chorea
- Erythema marginatum
- Subcutaneous nodules
Minor
- Fever
- Arthralgia
- Elevated ESR/CRP
- Prolonged PR interval
Diagnosis
- Jones Criteria
- Evidence of GAS infection
- Acute phase reactants
- Echocardiography
- ECG
Nursing Assessment
- Vital signs
- Cardiovascular assessment
- Joint examination
- Neurological status
- Skin assessment
- Functional capacity
Nursing Interventions
Acute Phase
- Pain management
- Rest promotion
- Antibiotic administration
- Fever management
Long-term
- Secondary prophylaxis
- Education
- HF management
- Activity guidance
Prevention
Primary
- Prompt treatment of strep throat
- Penicillin therapy
- Complete antibiotic course
Secondary
- Long-term prophylaxis
- Regular follow-up
- Endocarditis prophylaxis
RHD Complications
- Mitral valve disease
- Aortic valve disease
- Heart failure
- Atrial fibrillation
- Infective endocarditis
- Thromboembolism
Patient Education
- Disease process
- Medication adherence
- Prophylaxis importance
- Activity guidelines
- Follow-up care
- Red flag symptoms
Special Considerations
- School accommodations
- Growth & development
- Psychosocial support
- Family education
- Transition to adult care
- Long-term follow-up
Key Takeaways
Understanding RF & RHD
- RF is an inflammatory response to group A streptococcal infection
- RF can lead to permanent heart valve damage (RHD)
- Children 5-15 years are most commonly affected
- Diagnosis is based on the revised Jones criteria
- Evidence of preceding streptococcal infection is required for diagnosis
Nursing Management
- Comprehensive assessment of all body systems
- Pain management for arthritis/arthralgia
- Promoting rest during acute phase
- Monitoring for cardiac complications
- Administration of antibiotic therapy
- Coordinating long-term prophylaxis
- Education for patient and family
Prevention Focus
- Primary prevention: prompt treatment of strep throat
- Secondary prevention: long-term antibiotic prophylaxis
- Endocarditis prophylaxis for invasive procedures
- Regular cardiac follow-up with echocardiography
- Recognition of early symptoms of recurrence
- Education about importance of medication adherence
Critical Nursing Responsibility
The nurse plays a pivotal role in the management of rheumatic fever and RHD by ensuring adherence to secondary prophylaxis, which is the most effective measure to prevent recurrent episodes and progression of valve damage. Patient and family education about the chronic nature of RHD and the importance of long-term follow-up is essential for optimal outcomes.
References
- World Health Organization. (2023). Rheumatic heart disease. https://www.who.int/news-room/fact-sheets/detail/rheumatic-heart-disease
- Gewitz, M. H., Baltimore, R. S., Tani, L. Y., Sable, C. A., Shulman, S. T., Carapetis, J., & et al. (2015). Revision of the Jones Criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: a scientific statement from the American Heart Association. Circulation, 131(20), 1806-1818.
- Kumar, R. K., & Tandon, R. (2013). Rheumatic fever & rheumatic heart disease: The last 50 years. Indian Journal of Medical Research, 137(4), 643-658.
- Carapetis, J. R., Beaton, A., Cunningham, M. W., Guilherme, L., Karthikeyan, G., Mayosi, B. M., & et al. (2016). Acute rheumatic fever and rheumatic heart disease. Nature Reviews Disease Primers, 2, 15084.
- Zühlke, L., Engel, M. E., Karthikeyan, G., Rangarajan, S., Mackie, P., Cupido, B., & et al. (2015). Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). European Heart Journal, 36(18), 1115-1122.
- Beaton, A., Okello, E., Lwabi, P., Mondo, C., McCarter, R., & Sable, C. (2012). Echocardiography screening for rheumatic heart disease in Ugandan schoolchildren. Circulation, 125(25), 3127-3132.
- Watkins, D. A., Johnson, C. O., Colquhoun, S. M., Karthikeyan, G., Beaton, A., Bukhman, G., & et al. (2017). Global, regional, and national burden of rheumatic heart disease, 1990-2015. New England Journal of Medicine, 377(8), 713-722.
- Heunis, N. A., Naicker, E., Tshifularo, V., & Watkins, D. A. (2021). Secondary Antibiotic Prophylaxis for Latent Rheumatic Heart Disease. New England Journal of Medicine, 384(20), 1883-1892.
- NursesLabs. (2024). Rheumatic Fever Nursing Care Management and Study Guide. https://nurseslabs.com/rheumatic-fever/
- NursesLabs. (2024). Acute Rheumatic Fever Nursing Care Plans. https://nurseslabs.com/acute-rheumatic-fever-nursing-care-plans/
