Psychotherapy
Comprehensive Guide for Nursing Students
Introduction to Psychotherapy
Psychotherapy is a collaborative treatment based on the relationship between an individual and a psychotherapist. It provides a supportive environment that allows you to talk openly with someone who’s objective, neutral, and nonjudgmental.
Definition
Psychotherapy is a general term for treating mental health problems by talking with a psychiatrist, psychologist, or other mental health provider. It involves examining your thoughts, feelings, behaviors, and relationships to improve your wellbeing.

Figure 1: Overview of the Psychotherapy Process
Core Elements of Psychotherapy
- Therapeutic Relationship: The foundation of effective therapy, based on trust, empathy, and collaboration
- Theoretical Orientation: The framework or approach that guides the therapist’s understanding and interventions
- Evidence-Based Practice: Use of techniques and approaches supported by research
- Tailored Approach: Customization to meet individual needs, cultural backgrounds, and goals
- Regular Sessions: Consistent meetings to develop understanding, skills, and implement changes
Mnemonic: “CARES”
Remember the essential components of effective psychotherapy:
- C – Confidentiality and trust
- A – Active listening and empathy
- R – Respect for client’s autonomy
- E – Evidence-based approaches
- S – Structured goal setting
Types of Psychotherapy
There are several approaches to psychotherapy, each with its own theoretical framework, techniques, and applications. The following are the major types commonly used in clinical practice:
Cognitive Behavioral Therapy (CBT)
Figure 2: The CBT Model showing the relationship between thoughts, feelings, and behaviors
CBT focuses on identifying, challenging, and changing unhelpful thoughts (cognitive distortions) and behavior patterns. It is based on the concept that thoughts, feelings, and behaviors are interconnected.
Key Principles of CBT
- Psychological problems are partly based on faulty or unhelpful ways of thinking
- Psychological problems are partly based on learned patterns of unhelpful behavior
- People can learn better ways of coping with difficulties, relieving symptoms
- Focuses on the present rather than the past
- Structured and problem-oriented approach
Common CBT Techniques
- Cognitive Restructuring: Identifying and challenging negative thought patterns
- Behavioral Activation: Increasing positive behaviors and engagement in rewarding activities
- Exposure Therapy: Gradual exposure to feared situations to reduce anxiety
- Skills Training: Learning specific skills like assertiveness, problem-solving, or relaxation
- Homework: Practicing new skills between sessions
CBT has strong empirical support for treating depression, anxiety disorders, PTSD, OCD, substance use disorders, and eating disorders. Meta-analyses show CBT is as effective as medication for many conditions, with lower relapse rates.
When teaching CBT principles to patients, using the “Thought Record” technique can help them identify and challenge cognitive distortions. Guide patients to document the situation, automatic thoughts, emotions, evidence for and against the thought, and alternative perspectives.
Psychodynamic Therapy
Psychodynamic therapy focuses on unconscious processes as they manifest in a person’s present behavior. The goals are to increase self-awareness and understanding of how past experiences influence current behaviors.
Key Principles of Psychodynamic Therapy
- Emphasis on unconscious mental processes
- Focus on past experiences and their influence on present behavior
- Attention to transference (how feelings toward significant figures are projected onto the therapist)
- Exploration of defense mechanisms
- Recognition of resistance to treatment
Common Psychodynamic Techniques
- Free Association: Spontaneously expressing thoughts and feelings
- Dream Analysis: Exploring the unconscious through dream interpretation
- Transference Analysis: Examining how feelings toward others are transferred to the therapist
- Interpretation: Providing insights about unconscious patterns
- Working Through: Processing insights repeatedly until they lead to change
Mnemonic: “DRIFT”
Core elements of psychodynamic therapy:
- D – Defense mechanisms
- R – Resistance exploration
- I – Interpretation of unconscious material
- F – Free association
- T – Transference analysis
Research supports psychodynamic therapy’s effectiveness for depression, anxiety, somatic symptoms, and personality disorders. Meta-analyses show that benefits often continue to increase after therapy ends, unlike with CBT where gains tend to remain stable.
Interpersonal Therapy (IPT)

Figure 3: Interpersonal Therapy Formulation
Interpersonal Therapy (IPT) is a time-limited (typically 12-16 sessions) structured approach that focuses on improving interpersonal relationships and social functioning to help reduce distress.
Four Primary Problem Areas in IPT
- Grief: Complicated bereavement after the death of a loved one
- Role Disputes: Conflicts with significant others
- Role Transitions: Life changes that require adapting to new circumstances
- Interpersonal Deficits: Persistent problems forming and maintaining relationships
IPT Process
Initial Phase (Sessions 1-3)
Conduct interpersonal inventory, identify problem areas, create a treatment contract
Middle Phase (Sessions 4-9)
Implement strategies specific to identified problem areas (grief, disputes, transitions, deficits)
Termination Phase (Sessions 10-12)
Review progress, reinforce gains, develop strategies for maintaining improvements
IPT has strong empirical support for treating depression, particularly maternal depression, and has demonstrated effectiveness for eating disorders and bipolar disorder. It is recognized as an evidence-based treatment by multiple organizations including the APA and WHO.
When implementing IPT with patients experiencing depression related to role transitions (e.g., retirement, divorce), focus on helping them mourn the loss of the old role, develop new skills for the new role, and build a support system to assist in mastering the transition.
Dialectical Behavior Therapy (DBT)
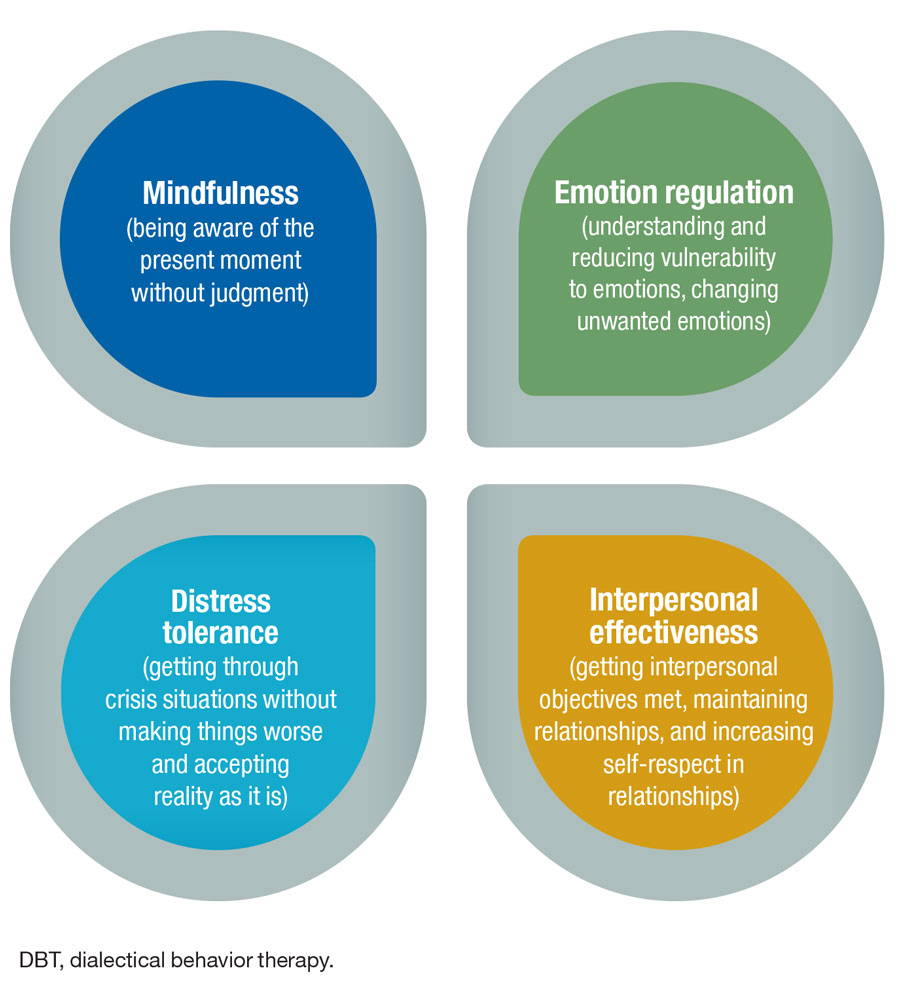
Figure 4: DBT Core Skills
Dialectical Behavior Therapy (DBT) integrates cognitive-behavioral techniques with mindfulness practices. It was originally developed to treat borderline personality disorder but has been adapted for various conditions involving emotional dysregulation.
Four Core Skill Modules in DBT
- Mindfulness: Being present and aware without judgment
- Distress Tolerance: Surviving crisis situations without making them worse
- Emotion Regulation: Understanding, recognizing, and managing emotions
- Interpersonal Effectiveness: Maintaining relationships while respecting yourself
Components of Comprehensive DBT
- Individual Therapy: Weekly one-on-one sessions focusing on motivation and behavioral change
- Group Skills Training: Weekly sessions teaching the four core skills
- Phone Coaching: Between-session support for applying skills in real life
- Therapist Consultation Team: Support for therapists to enhance effectiveness
Mnemonic: “CALM MIND”
For remembering key DBT distress tolerance skills:
- C – Crisis survival strategies
- A – Accept reality (radical acceptance)
- L – Living in the moment
- M – Managing triggers
- M – Mindful breathing
- I – Improving the moment
- N – Note pros and cons
- D – Distraction techniques
DBT has strong evidence for treating borderline personality disorder, reducing self-harm behaviors, suicidal ideation, and hospitalizations. It has also shown effectiveness for substance use disorders, eating disorders, PTSD, and depression with suicidality.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is an integrative psychotherapy approach designed to treat trauma and other distressing life experiences. It uses bilateral stimulation (usually eye movements) while the client focuses on traumatic memories.
Eight-Phase EMDR Protocol
- History Taking: Gathering information and identifying targets
- Preparation: Establishing trust and teaching self-regulation techniques
- Assessment: Identifying target memory components (image, belief, emotion, sensation)
- Desensitization: Processing the memory with bilateral stimulation
- Installation: Strengthening positive cognition
- Body Scan: Identifying and resolving remaining physical tension
- Closure: Returning to emotional equilibrium
- Reevaluation: Assessing progress and determining next steps
Mnemonic: “PEACE DRC”
To remember the 8 phases of EMDR:
- P – Patient history and planning
- E – Establishing safety (preparation)
- A – Assessment of target
- C – Clearing with bilateral stimulation (desensitization)
- E – Embedding positive cognition (installation)
- D – Doing body scan
- R – Reestablishing calm (closure)
- C – Checking progress (reevaluation)
EMDR is recognized as an effective treatment for PTSD by the World Health Organization, American Psychiatric Association, and Department of Veterans Affairs. Research shows it can achieve results in fewer sessions compared to some other trauma therapies.
When describing EMDR to patients, emphasize that they will maintain control throughout the process. Explain that they don’t need to share detailed trauma narratives, which can be particularly helpful for patients who find it difficult to verbalize their traumatic experiences.
Group Therapy
Group therapy involves one or more therapists working with several people at once. It allows members to share experiences, provide support, offer perspectives, and learn from each other.
Types of Group Therapy
- Psychoeducational Groups: Focus on education about specific conditions or issues
- Skills Development Groups: Teach specific skills (e.g., social skills, coping strategies)
- Support Groups: Provide mutual support for people with shared experiences
- Cognitive-Behavioral Groups: Apply CBT principles in a group format
- Psychodynamic Groups: Explore unconscious patterns in a group setting
Therapeutic Factors in Group Therapy
- Universality: Realizing you’re not alone
- Altruism: Helping others and feeling valuable
- Hope: Seeing others’ progress
- Guidance: Receiving advice and information
- Imparting Information: Learning from therapist and members
- Interpersonal Learning: Gaining insights about relationships
- Cohesiveness: Feeling accepted and belonging
- Catharsis: Emotional release
- Imitative Behavior: Modeling after others
- Corrective Recapitulation: Reworking family dynamics
Stages of Group Development
- Forming: Initial orientation, testing boundaries, dependency
- Storming: Conflict, resistance, emotional responses to demands
- Norming: Development of group cohesion and establishment of roles
- Performing: Functional role relatedness, problem-solving
- Adjourning: Termination, addressing separation issues
Group therapy has demonstrated effectiveness for depression, anxiety disorders, PTSD, substance use disorders, and eating disorders. For some conditions, group formats can be as effective as individual therapy while being more cost-effective.
Comparison of Psychotherapy Approaches
| Therapy Type | Focus | Timeframe | Best For | Nursing Considerations |
|---|---|---|---|---|
| CBT | Thoughts, behaviors, and their relationship to emotions | Short-term (12-20 sessions) | Depression, anxiety, PTSD, OCD, phobias | Can incorporate elements into daily nursing care; teach thought records and behavioral experiments |
| Psychodynamic | Unconscious processes, past experiences | Long-term (months to years) | Complex psychological issues, personality disorders | Awareness of transference/countertransference in nurse-patient relationship |
| Interpersonal (IPT) | Current relationships and social roles | Short-term (12-16 sessions) | Depression, relationship difficulties | Help patients identify relationship patterns; encourage social support systems |
| DBT | Emotional regulation, distress tolerance | Medium to long-term (6+ months) | Borderline personality disorder, self-harm, suicidality | Teach mindfulness and distress tolerance skills; validate emotions while encouraging change |
| EMDR | Processing traumatic memories | Variable (often 8-12 sessions) | PTSD, trauma, anxiety | Provide calm environment; teach grounding techniques; monitor for emotional distress |
| Group Therapy | Interpersonal learning, mutual support | Variable (weeks to ongoing) | Wide range of conditions; isolation; need for peer support | Can facilitate psychoeducation groups; observe group dynamics; encourage participation |
Nursing Considerations in Psychotherapy
Nurses play an essential role in the psychotherapeutic process, whether delivering interventions directly or supporting patients who are engaged in therapy with other providers.
Nursing Role in Psychotherapy
- Assessment: Conducting mental health assessments, identifying therapeutic needs
- Planning: Developing care plans that incorporate psychotherapeutic principles
- Implementation: Applying therapeutic techniques within scope of practice
- Evaluation: Monitoring progress and response to interventions
- Coordination: Facilitating multidisciplinary care and referrals
- Education: Teaching patients about their conditions and treatment
- Support: Providing emotional support and reinforcing coping skills
Therapeutic Communication Techniques
- Active Listening: Focusing completely on the patient
- Open-Ended Questions: Encouraging elaboration
- Reflection: Mirroring thoughts and feelings
- Clarification: Checking understanding
- Validation: Acknowledging feelings and experiences
- Silence: Allowing space for processing
- Focusing: Directing attention to important areas
- Summarizing: Reviewing key points
Mnemonic: “THERAPIST”
Key nursing skills for supporting psychotherapy:
- T – Trust-building consistently
- H – Holding hope and promoting recovery
- E – Empathic responding
- R – Reinforcing coping skills
- A – Assessing mental status regularly
- P – Providing psychoeducation
- I – Identifying warning signs
- S – Supporting treatment adherence
- T – Teaching self-management techniques
Nursing Interventions Across the Psychotherapy Continuum
Before Therapy Begins
- Conduct comprehensive mental health assessment
- Provide education about psychotherapy process and expectations
- Address misconceptions and fears about therapy
- Assist with practical barriers (transportation, scheduling)
- Coordinate referrals to appropriate therapists or programs
During Ongoing Therapy
- Monitor for therapeutic response and adverse effects
- Reinforce skills taught in therapy sessions
- Provide support during difficult phases of therapy
- Collaborate with therapists and treatment team
- Document observations and patient progress
- Encourage treatment adherence
After Therapy Completion
- Support maintenance of therapeutic gains
- Monitor for signs of relapse
- Facilitate connection to support groups or community resources
- Encourage continued use of learned coping strategies
- Provide guidance for handling setbacks
Important Considerations
- Scope of Practice: Ensure interventions are within nursing scope and competency
- Supervision: Seek appropriate supervision when implementing psychotherapeutic techniques
- Boundaries: Maintain clear professional boundaries while being therapeutic
- Self-Awareness: Monitor personal reactions and countertransference
- Cultural Sensitivity: Consider cultural factors affecting therapy perception and engagement
- Documentation: Maintain thorough, objective documentation of interventions and responses
When supporting patients engaged in trauma-focused therapies like EMDR or trauma-focused CBT, be prepared for temporary increases in distress. This “emotional processing” is a normal part of therapy but may require additional nursing support. Teach patients that this “getting worse before getting better” phenomenon is expected and usually temporary.
Evidence-Based Applications
Understanding the evidence base for different psychotherapeutic approaches is essential for providing informed nursing care and education to patients.
Evidence-Based Applications by Condition
| Condition | First-Line Therapy | Alternative Options | Level of Evidence | Key Nursing Considerations |
|---|---|---|---|---|
| Major Depression | CBT, IPT | Psychodynamic, behavioral activation | Strong – Multiple RCTs and meta-analyses | Monitor for suicidality; encourage activity scheduling; assess medication interactions |
| Generalized Anxiety | CBT | ACT, mindfulness-based interventions | Strong – Multiple RCTs | Teach relaxation techniques; monitor physical symptoms; reinforce exposure exercises |
| PTSD | Trauma-focused CBT, EMDR | CPT, prolonged exposure | Strong – Multiple RCTs and guidelines | Provide safe environment; teach grounding skills; be aware of potential for increased distress during processing |
| Borderline Personality Disorder | DBT | Mentalization-based therapy, schema therapy | Strong – Multiple RCTs and longitudinal studies | Maintain consistent boundaries; validate emotions while encouraging responsibility; monitor for self-harm |
| Substance Use Disorders | CBT, motivational interviewing | Contingency management, 12-step facilitation | Moderate to Strong – Multiple RCTs | Assess readiness to change; support through withdrawal; address comorbid conditions |
| Eating Disorders | CBT-E (enhanced), FBT (for youth) | IPT, DBT | Moderate to Strong – Multiple RCTs | Monitor physical health parameters; avoid focusing on weight/food during non-meal times; support nutritional rehabilitation |
| Bipolar Disorder | Interpersonal and social rhythm therapy | CBT for bipolar, family-focused therapy | Moderate – Several RCTs | Emphasize sleep hygiene and routine; monitor for mood shifts; coordinate with medication management |
| OCD | Exposure and response prevention | CBT, ACT | Strong – Multiple RCTs | Support during exposure exercises; avoid participating in compulsions; educate about anxiety habituation |
Research Insights for Nursing Practice
- Therapeutic Alliance: Research consistently shows the quality of the therapeutic relationship is one of the strongest predictors of outcomes across all therapy types
- Dose-Response: Studies indicate 12-20 sessions are typically needed for 50-75% of patients to show clinically significant improvement
- Combination Treatments: For many conditions, combining psychotherapy with appropriate medication yields better outcomes than either alone
- Early Response: Improvement in the first few sessions predicts overall therapy success
- Maintenance: Continued “booster sessions” after acute treatment help maintain gains and prevent relapse
When educating patients about psychotherapy options, explain that while certain approaches have stronger evidence for specific conditions, factors like therapist expertise, patient preference, and treatment accessibility are also important considerations in treatment selection. The “best” therapy is one that the patient will engage with and complete.
Special Populations Considerations
Children and Adolescents
- Involve parents/caregivers appropriately
- Use developmentally appropriate techniques
- Consider school and peer contexts
- CBT and family therapy have strongest evidence
- Play therapy for younger children
Older Adults
- Adapt pace to cognitive abilities
- Address cohort-specific beliefs about mental health
- Consider sensory impairments
- Integrate life review and meaning-making
- Problem-solving therapy shown highly effective
Cultural Considerations
- Adapt therapy to cultural values and beliefs
- Consider collectivist vs. individualist perspectives
- Address cultural stigma around mental health
- Incorporate cultural healing practices when appropriate
- Ensure linguistic accessibility
Memory Aids and Study Tips
Quick Reference Guide to Psychotherapy Approaches
Mnemonic: “EPIC DIPG”
For remembering the major psychotherapy approaches:
- E – EMDR (Eye Movement Desensitization and Reprocessing)
- P – Psychodynamic Therapy
- I – Interpersonal Therapy
- C – Cognitive Behavioral Therapy
- D – Dialectical Behavior Therapy
- I – Integrative Approaches
- P – Person-Centered (Humanistic) Therapy
- G – Group Therapy
Mnemonic: “The 5 C’s of Therapeutic Communication”
- C – Clarity (use clear, simple language)
- C – Compassion (show empathy and understanding)
- C – Curiosity (ask thoughtful, open-ended questions)
- C – Control (help patients gain control over their situation)
- C – Collaboration (work together as partners in care)
CBT Cognitive Distortions “TEN FAULTS”
- T – Twenty-Twenty Hindsight (should statements)
- E – Emotional Reasoning
- N – Negative Filter (discounting the positive)
- F – Fortune Telling (prediction)
- A – All-or-Nothing Thinking
- U – Unfair Labeling
- L – Leaping to Conclusions (mind reading)
- T – Taking Things Personally
- S – Sizzling Magnification (catastrophizing)
DBT Skills “WISE MIND”
- W – Willingness over willfulness
- I – Interpersonal effectiveness
- S – Self-soothing techniques
- E – Emotional regulation
- M – Mindfulness practices
- I – Improve the moment
- N – Notice and name emotions
- D – Distress tolerance
Therapeutic Models Remember: “PACE”
Four major theoretical foundations:
- P – Psychodynamic (unconscious, past experiences)
- A – Attachment (relationship patterns)
- C – Cognitive-behavioral (thoughts, behaviors)
- E – Existential-humanistic (meaning, growth)
Critical Thinking Questions
- How would you determine which psychotherapy approach might be most appropriate for a patient with comorbid depression and anxiety?
- How can nurses integrate basic principles of CBT into their everyday interactions with patients?
- What are the ethical considerations when a patient is participating in psychotherapy while receiving inpatient care?
- How would you explain the difference between psychotherapy and psychiatric medication to a patient who is unfamiliar with mental health treatments?
- What nursing assessments are particularly important to conduct for patients engaged in trauma-focused therapies like EMDR?
Study Tips
For Visual Learners
- Create mind maps of different therapy approaches
- Use color-coding for different therapy categories
- Draw diagrams showing therapy processes
- Watch videos demonstrating therapy techniques
- Create flashcards with visual cues
For Auditory/Verbal Learners
- Record yourself explaining key concepts
- Participate in study groups to discuss concepts
- Teach concepts to peers or family members
- Create songs or rhymes for mnemonics
- Listen to podcasts about therapy approaches
© 2025 Psychotherapy Nursing Notes. Created by Soumya Ranjan Parida for educational purposes only.
These notes are meant to supplement, not replace, comprehensive nursing education on psychotherapy approaches.
