Schizophrenia and Related Psychotic Disorders
Comprehensive Nursing Notes
Table of Contents
1. Introduction to Psychotic Disorders
Psychotic disorders are severe mental conditions characterized by abnormal thinking and perceptions that impair reality testing.
Psychotic disorders encompass a range of conditions that affect how a person’s brain processes information. These disorders involve disturbances in thinking, perception, emotions, language, sense of self, and behavior. The most prominent symptoms include hallucinations, delusions, and disorganized thinking, resulting in functional impairment and challenges in daily life activities.
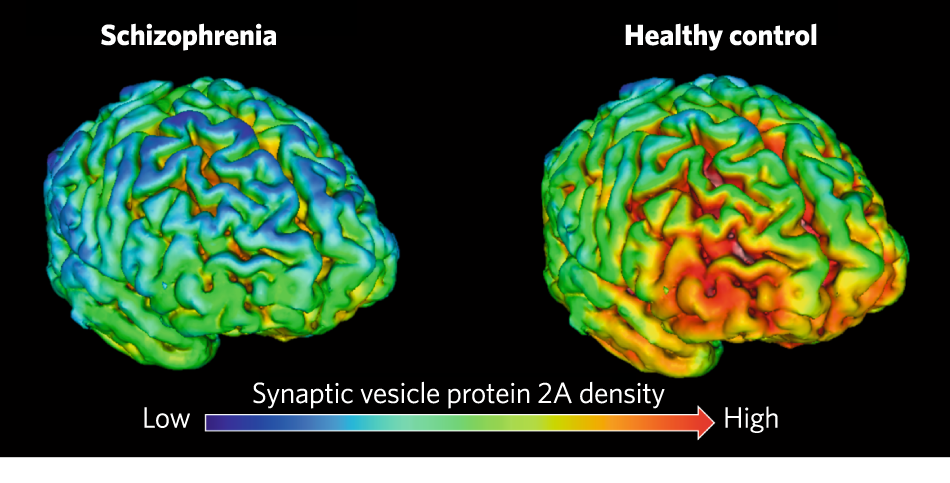
Fig 1. Neuroimaging comparing healthy brain structure to schizophrenia brain structure. Note the enlarged ventricles and reduced gray matter in key regions.
Schizophrenia is the prototypical psychotic disorder, but the spectrum includes several other conditions that share features of psychosis with varying severity, duration, and functional impact. Understanding this spectrum is crucial for nursing assessment, care planning, and intervention.
2. Prevalence and Incidence
Schizophrenia Prevalence
- Global prevalence: Affects approximately 24 million people worldwide (~1 in 300 people or 0.32%)
- Adult prevalence: ~1 in 222 people (0.45%) among adults
- United States: Approximately 1.1% of the population (~2.8 million adults)
- Lifetime prevalence: 0.3-0.7% of people will develop schizophrenia during their lifetime
Key Point: Schizophrenia ranks among the top 10 causes of global disability despite its relatively low prevalence.
Age of Onset
Males: Typically begin developing symptoms in late teens to early 20s
Females: Often show first signs in late 20s to early 30s
Early-onset: Can occur in childhood (rare, less than 1% of cases)
Late-onset: After age 45 (uncommon, often with higher proportion of positive symptoms)
Other Psychotic Disorders
| Disorder | Prevalence | Typical Age of Onset |
|---|---|---|
| Schizoaffective Disorder | 0.3-0.5% | Late adolescence to early adulthood |
| Brief Psychotic Disorder | 0.05-0.1% | Early adulthood (20s-30s) |
| Delusional Disorder | 0.03% | Middle to late adulthood (40s-50s) |
| Schizophreniform Disorder | 0.07% | Similar to schizophrenia |
Risk Patterns
- Higher incidence in urban environments compared to rural settings
- Higher rates in migrant populations
- Slightly higher prevalence in males (1.4:1 male-to-female ratio)
- Mortality: People with schizophrenia have 2-3 times higher mortality rate than general population
- Suicide risk: ~4.9% of people with schizophrenia die by suicide, with highest risk in early stages
3. Classification of Psychotic Disorders
According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), psychotic disorders are classified under “Schizophrenia Spectrum and Other Psychotic Disorders.” This categorization represents a shift from previous editions, emphasizing the spectrum nature of these conditions.
| Disorder | Key Features | Duration Requirement |
|---|---|---|
| Schizophrenia | Hallucinations, delusions, disorganized speech, negative symptoms, disorganized/catatonic behavior | At least 6 months (including 1 month of active symptoms) |
| Schizophreniform Disorder | Same symptoms as schizophrenia | 1-6 months |
| Schizoaffective Disorder | Features of schizophrenia plus mood episodes (depressive or manic) | Mood symptoms present for majority of illness duration |
| Delusional Disorder | Non-bizarre delusions without other psychotic features | At least 1 month |
| Brief Psychotic Disorder | Sudden onset of psychotic symptoms | 1 day to 1 month, with full return to functioning |
| Substance/Medication-Induced Psychotic Disorder | Psychotic symptoms directly attributable to substance use or medication | Develops during or shortly after substance use/withdrawal |
| Psychotic Disorder Due to Another Medical Condition | Psychotic symptoms directly resulting from physiological effects of medical condition | Evidence of causation through history, physical exam, or lab findings |
Subtypes of Schizophrenia
Note: The DSM-5 removed the traditional subtypes of schizophrenia (paranoid, disorganized, catatonic, undifferentiated, and residual) that were present in DSM-IV. The current approach focuses on symptom dimensions and severity rather than distinct subtypes.
Mnemonic: “PSYCHOTIC”
Psychosis due to medical conditions
Schizoaffective disorder
Years of symptoms indicate schizophrenia (6+ months)
Chemical causes (substance-induced)
Hallucinations & delusions (core features)
One to six months? Think schizophreniform
Temporary symptoms (1 day – 1 month) suggest brief psychotic disorder
Isolated delusions point to delusional disorder
Catatonia can occur across spectrum
4. Etiology and Risk Factors
The etiology of schizophrenia and related disorders is multifactorial, involving a complex interplay of genetic, neurobiological, environmental, and developmental factors. No single cause has been identified, but rather a combination of vulnerabilities and triggers contribute to the development of these conditions.
Genetic Factors
- Heritability estimated at 60-80%
- 10% risk if first-degree relative has schizophrenia
- 40-50% concordance rate in monozygotic twins
- Multiple genes involved rather than a single gene
- Risk genes include DISC1, DTNBP1, NRG1, and COMT
Neurobiological Factors
- Dopamine dysregulation: Hyperactivity in mesolimbic pathway, hypoactivity in mesocortical pathway
- Glutamate abnormalities (NMDA receptor dysfunction)
- Serotonin system alterations
- Reduced brain volume in frontal and temporal regions
- Enlarged ventricles
- Reduced synaptic density
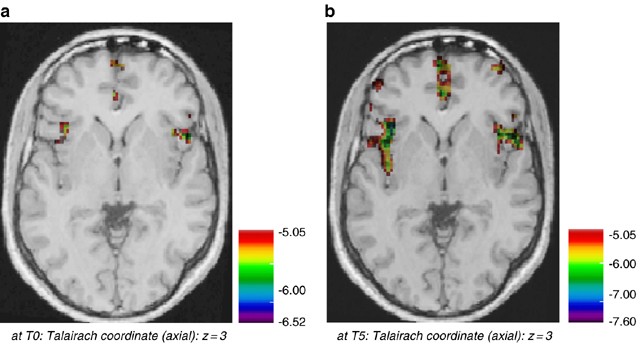
Fig 2. Focal gray matter changes in schizophrenia. Note the progressive loss of gray matter over time, particularly in frontal and temporal regions.
Developmental Factors
- Prenatal exposure to infections (influenza, Toxoplasma gondii)
- Pregnancy and birth complications
- Maternal malnutrition during pregnancy
- Advanced paternal age
- Neurodevelopmental abnormalities
Environmental Factors
- Urban upbringing (1.5-2.5x increased risk)
- Migration and minority status
- Childhood trauma and adversity
- Cannabis use (especially in adolescence)
- Psychosocial stressors
The Stress-Vulnerability Model
The stress-vulnerability model proposes that individuals inherit a predisposition (vulnerability) to developing schizophrenia, which may be triggered by environmental stressors when the threshold is exceeded.
The “Two-Hit” Hypothesis:
This model suggests that schizophrenia develops from:
1. First hit: Early neurodevelopmental disruption (genetic or prenatal factors)
2. Second hit: Neurobiological changes during adolescence or early adulthood, triggered by stress, substance use, or other environmental factors
Mnemonic: “GENETICS”
Genes (multiple risk genes)
Environment (urban living, migration)
Neurotransmitter dysregulation (dopamine, glutamate)
Early life events (birth complications)
Toxins and substances (cannabis use)
Infections (prenatal exposure)
Cerebral abnormalities (structural changes)
Stress as a trigger
5. Psychodynamics
While biological models are now dominant in explaining schizophrenia, psychodynamic perspectives offer insights into the subjective experience and psychological mechanisms that may be involved in psychotic processes.
Freudian Perspective
In classical psychoanalytic theory, Freud viewed schizophrenia as a regression to a primary narcissistic state due to ego weakness. He proposed that:
- Psychosis results from the disintegration of the ego
- The ego fails to mediate between the id, superego, and reality
- Withdrawal of cathexis (emotional investment) from objects in the external world
- Regression to primitive defense mechanisms
Modern Psychodynamic Understanding
Contemporary psychodynamic perspectives view psychotic symptoms as meaningful expressions of the patient’s inner psychological world rather than random phenomena:
| Psychodynamic Process | Expression in Psychosis |
|---|---|
| Concretization | Abstract psychological conflicts are experienced as concrete external realities |
| Perceptualization | Internal thoughts and feelings are projected and experienced as perceptions from the external world |
| Projection | Unacceptable internal impulses are attributed to external sources |
| Splitting | Inability to integrate positive and negative aspects of self and others |
| Symbolization | Delusions and hallucinations represent symbolic expressions of psychological material |
Key Concept: Psychotic symptoms as defensive operations
Psychotic symptoms may serve a defensive function, protecting the individual from overwhelming anxiety, trauma, or intolerable emotional states. Hallucinations and delusions can be understood as attempts to make sense of confusing experiences or to restore a sense of meaning and control.
Clinical Implications of Psychodynamic Understanding
- Symptoms have personal meaning and symbolic significance
- Content of delusions and hallucinations often relates to personal history and conflicts
- Understanding the meaning behind symptoms can guide therapeutic approaches
- Psychotherapy can help patients make sense of their experiences
- Therapeutic relationship provides a safe container for disorganized psychological processes
Integrated Perspective:
Modern approaches integrate psychodynamic understanding with neurobiological models, recognizing that:
- Biological factors create vulnerability to psychosis
- Psychological factors shape the content and expression of symptoms
- Social factors influence triggers, course, and outcomes
6. Clinical Manifestations
The clinical presentation of schizophrenia and related psychotic disorders is heterogeneous, with symptoms typically categorized into positive, negative, and cognitive domains. Understanding these distinct symptom domains is essential for comprehensive assessment and targeted interventions.
:max_bytes(150000):strip_icc()/schizophrenia-sign-symptoms-5095511_final-57a52853a10c4edcb4bd6a3b31f041ea.jpg)
Fig 3. Overview of positive, negative, and cognitive symptoms in schizophrenia.
Positive Symptoms
Excess or distortion of normal functions
- Hallucinations – Most commonly auditory (voices), but can be visual, tactile, olfactory, or gustatory
- Delusions – Fixed false beliefs (persecutory, referential, grandiose, somatic, or bizarre)
- Disorganized thinking – Tangential speech, loose associations, word salad
- Disorganized behavior – Unpredictable agitation, inappropriate behavior, bizarre posturing
Negative Symptoms
Diminution or loss of normal functions
- Affective flattening – Reduced emotional expression, monotone voice
- Alogia – Poverty of speech, reduced content of speech
- Avolition – Lack of motivation and goal-directed behavior
- Anhedonia – Inability to experience pleasure
- Social withdrawal – Reduced interest in social interactions
Cognitive Symptoms
Deficits in cognitive function
- Attention deficits – Difficulty focusing and maintaining attention
- Working memory impairment – Problems holding and manipulating information
- Executive dysfunction – Difficulties with planning, decision-making, problem-solving
- Processing speed deficits – Slowed information processing
- Impaired social cognition – Difficulty interpreting social cues and others’ intentions
Mnemonic: “NURSE PAINS” for Negative Symptoms
No emotion (flat affect)
Uninterested in pleasurable activities (anhedonia)
Reduced speech (alogia)
Social withdrawal
Energy lacking (avolition)
Poor self-care
Apathetic presentation
Inattention to surroundings
Neglect of responsibilities
Spontaneity reduced
Phases of Schizophrenia
| Phase | Clinical Features | Duration |
|---|---|---|
| Prodromal Phase |
|
Months to years before full psychosis |
| Acute Phase |
|
Weeks to months if untreated |
| Stabilization Phase |
|
3-6 months after acute episode |
| Maintenance Phase |
|
Long-term |
Clinical Features of Other Psychotic Disorders
Schizoaffective Disorder
- Features of schizophrenia plus mood disorder
- Major depressive or manic episodes concurrent with psychotic symptoms
- Psychotic symptoms present during periods of normal mood
Delusional Disorder
- Non-bizarre delusions (could occur in real life)
- Relatively preserved functioning outside delusional domain
- Absence of prominent hallucinations
- Common types: persecutory, jealous, somatic, erotomanic
Brief Psychotic Disorder
- Sudden onset of psychotic symptoms
- Duration: 1 day to 1 month
- Complete return to premorbid functioning
- Often triggered by severe stress
Schizophreniform Disorder
- Identical to schizophrenia in presentation
- Duration: 1-6 months
- Better prognosis than schizophrenia
- Diagnosis may change to schizophrenia if symptoms persist beyond 6 months
7. Diagnostic Criteria
Accurate diagnosis of schizophrenia and related psychotic disorders requires careful clinical assessment based on established diagnostic criteria. The DSM-5 provides standardized criteria for diagnosis, allowing clinicians to reliably identify and differentiate between psychotic conditions.
DSM-5 Criteria for Schizophrenia
A. Two (or more) of the following, present for a significant portion of time during a 1-month period (or less if successfully treated). At least one of these must be (1), (2), or (3):
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior
- Negative symptoms (i.e., diminished emotional expression or avolition)
B. For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas (work, interpersonal relations, or self-care) is markedly below the level achieved prior to the onset.
C. Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A and may include periods of prodromal or residual symptoms.
D. Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out.
E. The disturbance is not attributable to the physiological effects of a substance or another medical condition.
F. If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to the other required symptoms of schizophrenia, are also present for at least 1 month (or less if successfully treated).
Mnemonic: “A DEFECT” for Schizophrenia Diagnostic Criteria
A – At least two symptoms (delusions, hallucinations, disorganization, negative symptoms, abnormal behavior)
D – Dysfunction in major life areas
E – Enduring for at least 6 months (with 1 month of active symptoms)
F – Filtered out other disorders (not schizoaffective or mood disorder)
E – Exclude substance or medical causes
C – Consider developmental disorders in context
T – Treatment may shorten required symptom duration
Differential Diagnosis
| Condition | Key Distinguishing Features |
|---|---|
| Major Depressive Disorder with Psychotic Features | Psychotic symptoms only during mood episodes; depression precedes psychosis |
| Bipolar Disorder with Psychotic Features | Psychotic symptoms only during mood episodes; clear manic or hypomanic episodes |
| Substance-Induced Psychotic Disorder | Temporal relationship to substance use; resolves with abstinence |
| Delirium | Fluctuating consciousness, attention deficits, direct medical cause |
| Personality Disorders (e.g., Schizotypal, Borderline) | Less severe, non-psychotic perceptual disturbances; long-standing patterns |
| Autism Spectrum Disorder | Early onset; social communication deficits; restricted interests and behaviors |
| Post-Traumatic Stress Disorder | Trauma history; flashbacks rather than true hallucinations; hypervigilance |
Diagnostic Assessment
Comprehensive assessment for psychotic disorders should include:
Clinical Evaluation
- Thorough psychiatric history and mental status examination
- Collateral information from family/caregivers
- Developmental and premorbid functioning history
- Substance use assessment
- Physical examination
Laboratory and Diagnostic Tests
- Complete blood count
- Comprehensive metabolic panel
- Thyroid function tests
- Toxicology screen
- Brain imaging (CT or MRI) if indicated
- EEG if seizure disorder suspected
Important Nursing Consideration:
Accurate diagnosis requires ruling out medical causes of psychosis. Nurses should be vigilant for signs and symptoms of underlying medical conditions that can present with psychotic features, including:
- Delirium
- Metabolic disorders
- Neurological conditions (e.g., seizures, tumors, dementia)
- Autoimmune disorders
- Infectious processes
- Medication side effects
8. Treatment Approaches
Effective management of schizophrenia and related psychotic disorders requires a comprehensive, multidisciplinary approach that addresses biological, psychological, and social dimensions of the illness. Treatment is typically lifelong, with goals of symptom reduction, relapse prevention, and optimizing functional recovery.
-1024x576.jpg)
Fig 4. Overview of integrated treatment approaches for schizophrenia.
Pharmacological Interventions
First-Generation Antipsychotics (FGAs)
- Also called “typical” antipsychotics
- Mechanism: D2 dopamine receptor antagonism
- Examples: Haloperidol, Chlorpromazine, Fluphenazine
- More effective for positive symptoms
- Higher risk of extrapyramidal side effects (EPS) and tardive dyskinesia
Second-Generation Antipsychotics (SGAs)
- Also called “atypical” antipsychotics
- Mechanism: 5-HT2A/D2 receptor antagonism
- Examples: Risperidone, Olanzapine, Quetiapine, Aripiprazole
- Effective for both positive and (somewhat) negative symptoms
- Lower risk of EPS, higher risk of metabolic side effects
Clozapine: The Gold Standard for Treatment-Resistant Schizophrenia
Clozapine is considered the most effective antipsychotic, particularly for treatment-resistant cases (failure to respond to at least two adequate trials of different antipsychotics). However, due to the risk of agranulocytosis, it requires regular blood monitoring through the Clozapine REMS program.
Common Side Effects of Antipsychotics
| Category | Side Effects | Monitoring/Management |
|---|---|---|
| Extrapyramidal Symptoms (EPS) | Acute dystonia, akathisia, parkinsonism, tardive dyskinesia | AIMS assessment, anticholinergic medications (benztropine, trihexyphenidyl) |
| Metabolic Effects | Weight gain, diabetes, dyslipidemia, metabolic syndrome | Regular weight, glucose, and lipid monitoring; lifestyle interventions |
| Cardiovascular Effects | Orthostatic hypotension, QTc prolongation, tachycardia | ECG monitoring, vital signs, dose adjustments |
| Anticholinergic Effects | Dry mouth, constipation, urinary retention, blurred vision | Symptom management, adequate hydration |
| Other | Sedation, hyperprolactinemia, sexual dysfunction, neuroleptic malignant syndrome | Timing adjustments, dose reduction, medication changes |
Mnemonic: “ANTIPSYCHOTICS” for Side Effect Monitoring
Akathisia (restlessness) and other EPS
NMS (neuroleptic malignant syndrome) – rare but serious
Tardive dyskinesia (monitor with AIMS)
Increased weight and metabolic changes
Prolactin elevation (galactorrhea, sexual dysfunction)
Sedation (especially with certain SGAs)
Yielding to orthostatic hypotension
Cardiac effects (QTc prolongation)
Hyperglycemia risk
Ocular changes (blurred vision)
Temperature dysregulation
Intestinal issues (constipation)
Cholinergic blockade effects
Salivation changes (drooling with clozapine or dry mouth)
Psychosocial Interventions
Cognitive Behavioral Therapy for Psychosis (CBTp)
- Helps patients identify and challenge delusional beliefs
- Develops coping strategies for hallucinations
- Addresses negative thinking patterns
- Enhances problem-solving skills
Family Interventions
- Psychoeducation about illness and treatment
- Communication and problem-solving skills training
- Reducing high expressed emotion in family environment
- Relapse prevention planning
Social Skills Training
- Interpersonal skills development
- Role-playing social scenarios
- Community integration skills
- Managing social anxiety
Vocational Rehabilitation
- Supported employment programs
- Job coaching and skills training
- Educational support
- Workplace accommodations
Additional Evidence-Based Interventions
- Assertive Community Treatment (ACT): Intensive case management with multidisciplinary team
- Cognitive Remediation: Targeted exercises to improve cognitive functioning
- Peer Support: Connection with others who have lived experience of psychosis
- Illness Management and Recovery (IMR): Self-management skills development
Treatment Phases and Approach

Fig 5. Clinical pathway for antipsychotic selection and management in schizophrenia.
| Treatment Phase | Goals | Key Interventions |
|---|---|---|
| Acute Phase |
|
|
| Stabilization Phase |
|
|
| Maintenance Phase |
|
|
Treatment-Resistant Schizophrenia (TRS)
Approximately 30% of individuals with schizophrenia have treatment-resistant illness, defined as failure to respond adequately to at least two different antipsychotics (one of which is an SGA) at appropriate doses for 6-8 weeks.
Management approach for TRS:
- Trial of clozapine (the only FDA-approved medication for TRS)
- Augmentation strategies (adding another antipsychotic or mood stabilizer)
- Electroconvulsive therapy (ECT) consideration
- Intensive psychosocial interventions
9. Nursing Care and Interventions
Nurses play a crucial role in the comprehensive care of individuals with schizophrenia and related psychotic disorders across all treatment settings. The nursing process provides an organized framework for assessment, diagnosis, planning, implementation, and evaluation of care.
Nursing Assessment
Mental Status Assessment
- Appearance and behavior
- Thought content and processes (delusions, thought disorders)
- Perceptual disturbances (hallucinations)
- Mood and affect
- Cognitive functioning
- Insight and judgment
Safety Assessment
- Suicidal ideation and risk
- Homicidal ideation
- Self-care abilities
- Command hallucinations
- Impulsivity and agitation
Functional Assessment
- Activities of daily living
- Social functioning
- Occupational/educational performance
- Support system
- Living situation
Physical Assessment
- Vital signs
- Nutritional status
- Medication side effects (EPS, metabolic changes)
- Sleep patterns
- Comorbid physical conditions
Common Nursing Diagnoses
| Nursing Diagnosis | Related Factors | Key Interventions |
|---|---|---|
| Disturbed Thought Processes | Delusions, hallucinations, disorganized thinking |
|
| Risk for Self-Directed or Other-Directed Violence | Command hallucinations, paranoid delusions, impulsivity |
|
| Self-Care Deficit | Negative symptoms, cognitive impairment, lack of motivation |
|
| Social Isolation | Paranoia, social skill deficits, stigma, negative symptoms |
|
| Ineffective Coping | Stress vulnerability, limited coping skills, emotional dysregulation |
|
| Noncompliance (Medication/Treatment) | Poor insight, side effects, complex regimen, lack of support |
|
Therapeutic Communication Techniques
Mnemonic: “PSYCHOTIC” for Communication with Psychotic Patients
Present reality without arguing about delusions
Simple, clear, and concrete language
Yield to patient’s need for personal space
Calm, consistent approach
Honest and transparent interactions
One topic at a time; avoid overwhelming
Time for processing; patient appropriate pace
Identify and address the feeling behind delusional content
Confirm understanding through feedback
Do’s
- Establish trust and rapport
- Use clear, concrete language
- Focus on reality and the present
- Acknowledge feelings behind delusions
- Set consistent limits on inappropriate behavior
- Allow adequate response time
- Provide a calm, low-stimulation environment
Don’ts
- Argue with or challenge delusions directly
- Use abstract language or idioms
- Whisper or talk about patient in their presence
- Touch without permission (especially with paranoia)
- Reinforce or validate hallucinations
- Make promises you cannot keep
- Show fear or frustration in interactions
Medication Management
Nurses play a critical role in medication management for patients with psychotic disorders:
- Administration: Ensure proper administration and documentation
- Monitoring: Assess effectiveness and side effects
- Education: Teach patients and families about medications
- Adherence: Implement strategies to improve medication adherence
- Side effect management: Identify and address adverse effects
Long-Acting Injectable (LAI) Antipsychotics
LAIs can improve adherence and reduce relapse rates in schizophrenia. Nursing considerations for LAIs include:
- Proper administration technique (Z-track method for many LAIs)
- Rotation of injection sites
- Monitoring for post-injection syndrome (with olanzapine LAI)
- Ensuring timely administration according to schedule
- Patient education about the benefits of consistent medication levels
Patient and Family Education
Education is a cornerstone of nursing care for patients with psychotic disorders and their families. Key educational topics include:
Disease Education
- Nature of schizophrenia as a biological brain disorder
- Common symptoms and their management
- Course of illness and prognosis
- Importance of early intervention
Relapse Prevention
- Identifying early warning signs
- Creating a relapse prevention plan
- Stress management techniques
- When and how to seek help
Medication Education
- Medication names, doses, and schedules
- Expected benefits and timeframe
- Potential side effects and management
- Importance of adherence
- Consequences of discontinuation
Healthy Lifestyle
- Nutrition and weight management
- Physical activity recommendations
- Sleep hygiene
- Substance use avoidance
- Stress reduction techniques
Recovery-Oriented Nursing Care
The recovery model emphasizes hope, personal responsibility, empowerment, and meaningful life beyond illness. Nurses can support recovery by:
- Focusing on strengths and abilities, not just symptoms and deficits
- Promoting autonomy and shared decision-making
- Supporting personal goals beyond symptom management
- Combating stigma through education and advocacy
- Connecting patients with peer support and recovery communities
- Maintaining hope and positive expectations
10. References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- World Health Organization. (2023). Schizophrenia fact sheet. https://www.who.int/news-room/fact-sheets/detail/schizophrenia
- National Institute of Mental Health. (2022). Schizophrenia. https://www.nimh.nih.gov/health/topics/schizophrenia
- Leucht, S., Leucht, C., Huhn, M., Chaimani, A., Mavridis, D., Helfer, B., et al. (2017). Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: Systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. American Journal of Psychiatry, 174(10), 927-942.
- Correll, C. U., & Schooler, N. R. (2020). Negative symptoms in schizophrenia: A review and clinical guide for recognition, assessment, and treatment. Neuropsychiatric Disease and Treatment, 16, 519-534.
- Jääskeläinen, E., Juola, P., Hirvonen, N., McGrath, J. J., Saha, S., Isohanni, M., et al. (2013). A systematic review and meta-analysis of recovery in schizophrenia. Schizophrenia Bulletin, 39(6), 1296-1306.
- Bighelli, I., Rodolico, A., García-Mieres, H., Pitschel-Walz, G., Hansen, W. P., Schneider-Thoma, J., et al. (2022). Psychosocial interventions for positive and negative symptoms in schizophrenia: Network meta-analysis. The Lancet Psychiatry, 9(8), 640-651.
- Fortinash, K. M., & Holoday Worret, P. A. (2012). Psychiatric mental health nursing (5th ed.). St. Louis, MO: Elsevier Mosby.
- Videbeck, S. L. (2017). Psychiatric-mental health nursing (7th ed.). Philadelphia, PA: Wolters Kluwer.
- Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of care in evidence-based practice (9th ed.). Philadelphia, PA: F.A. Davis.
Geriatric Considerations and Special Populations in Schizophrenia
Follow-up Care and Rehabilitation Nursing Notes
Introduction
Schizophrenia is a complex psychiatric disorder that affects approximately 1% of the global population. While standard treatment approaches exist, special populations require unique considerations for optimal care and outcomes. This guide focuses on evidence-based approaches for nursing care in geriatric patients, adolescents, substance abusers, and treatment-resistant cases, along with follow-up care and rehabilitation strategies.
Special Populations in Schizophrenia
- Geriatric patients (>65 years)
- Adolescents (onset before 18 years)
- Substance abusers (dual diagnosis)
- Treatment-resistant cases (inadequate response to standard therapy)
These populations present unique challenges that require specialized nursing approaches and treatment considerations to optimize outcomes and quality of life.
Geriatric Considerations in Schizophrenia
Schizophrenia in the elderly can be either chronic (carrying over from younger age) or late-onset (developing after age 40). The epidemiological data shows a 6-month prevalence rate of 0.2% to 0.9% in the elderly population. Other illnesses with psychotic symptoms are more common in this age group, including psychotic depression (0.1-1.6%) and organic psychosis (16.8-23%).
Mnemonic: “ELDER” – Key Considerations in Geriatric Schizophrenia
- E – Exquisite sensitivity to medication side effects
- L – Lower doses required (25-50% of adult dosing)
- D – Drug interactions due to polypharmacy
- E – Extended monitoring for adverse effects
- R – Reduced metabolism and clearance of medications
Clinical Presentation in Elderly
Older adults with schizophrenia often show a different clinical picture compared to younger patients:
Positive Symptoms
- Often less severe with aging
- May include paranoia, often focused on caregivers
- Visual hallucinations more common than in younger patients
- Delusions may be less complex and more focused on immediate environment
Negative Symptoms & Functioning
- Can improve with age in some patients
- Better psychosocial functioning compared to earlier life
- Reduced substance use
- Improved mental health-related quality of life
- Lower risk of psychiatric hospitalization
Medication Management
Pharmacokinetic and pharmacodynamic changes in the elderly require special attention when prescribing antipsychotics:
| Age-Related Changes | Clinical Implications | Nursing Considerations |
|---|---|---|
| ↑ Volume of distribution and elimination half-life | Medications stay in system longer | Monitor for cumulative effects; longer intervals between dose adjustments |
| ↑ Free drug fraction in blood | Higher biologically active drug levels | Start at lower doses; monitor for increased side effects |
| ↓ Dopamine neurons and D2 receptors | Higher sensitivity to antipsychotics | Watch for EPS at lower doses than in younger adults |
| ↓ Blood-brain barrier permeability | Increased CNS drug availability | Monitor for increased sedation and cognitive effects |
| ↓ Hepatic/renal function | Decreased drug clearance | Monitor blood levels when available; adjust doses based on renal/hepatic function |
Second-Generation Antipsychotics in the Elderly
| Medication | Dosing in Elderly | Advantages | Key Concerns |
|---|---|---|---|
| Risperidone | 0.25-0.5 mg initially; target 0.5-3 mg/day | Effective for positive and negative symptoms; low anticholinergic effects | Orthostatic hypotension; EPS at higher doses; hyperprolactinemia |
| Olanzapine | 2.5 mg initially; target 5-15 mg/day | Good efficacy; fewer EPS | Sedation; anticholinergic effects; metabolic effects; worsens parkinsonism |
| Quetiapine | 12.5-25 mg initially; target 100-300 mg/day | First-line for psychosis with Parkinson’s; low EPS risk | Sedation; orthostatic hypotension; anticholinergic effects |
| Clozapine | 12.5-25 mg initially; titrate slowly to 50-300 mg/day | Effective in treatment-resistant cases; low EPS | Increased agranulocytosis risk (4% in elderly); seizure risk; sedation; orthostasis |
Important Safety Considerations in Elderly
- Extrapyramidal symptoms (EPS): Occur in >50% of elderly patients on conventional antipsychotics
- Tardive dyskinesia (TD): Annual incidence >25% in elderly; less likely to reverse with age
- Orthostatic hypotension: Occurs in 5-30% of geriatric patients; major risk factor for falls
- Anticholinergic effects: Increased sensitivity; can cause constipation, urinary retention, confusion, cognitive impairment
- Falls risk: Higher likelihood of serious consequences (fractures, head injuries)
- Cognitive decline: Antipsychotics may accelerate cognitive impairment in elderly patients
Nursing Assessment Tips
Physical Assessment
- Monitor vital signs, especially orthostatic changes
- Regular weight checks for metabolic changes
- EPS assessments including AIMS (Abnormal Involuntary Movement Scale)
- Hydration and nutritional status
Functional Assessment
- Activities of daily living (ADLs)
- Cognitive function (orientation, memory)
- Fall risk assessment
- Medication self-management capability
Adolescent Schizophrenia
Approximately 10-30% of patients with schizophrenia develop their first psychotic symptoms before age 18. Early-onset schizophrenia (onset between puberty and 18 years) and very-early-onset schizophrenia (onset before puberty) present unique diagnostic and treatment challenges.
Epidemiology
- Male predominance (2:1) in very-early-onset
- Prevalence of childhood onset: 1/10,000
- 54-90% have premorbid abnormalities (withdrawal, odd traits, isolation)
- High rates of comorbid neurodevelopmental disorders
Clinical Presentation
- Auditory hallucinations in ~80% (command hallucinations most common)
- Delusions vary by age (younger children have less complex delusions)
- Often misdiagnosed as behavioral disorders
- High rates of comorbid conditions (ADHD, learning disorders)
Treatment Approach for Adolescents
An intensive, comprehensive approach is recommended for adolescents with schizophrenia:
Structured Environment
Special education & psychoeducation
Psychosocial Interventions
Family therapy, skills training
Pharmacologic Treatment
Second-generation antipsychotics preferred
Ongoing Assessment
Regular monitoring & adjustment
Medication Considerations in Adolescents
| Medication | Dosing in Adolescents | Efficacy | Special Considerations |
|---|---|---|---|
| Risperidone | 0.25-0.5 mg initially; target 0.5-4 mg/day | Effective for positive and negative symptoms | Weight gain (~8.7 kg/6 months); prolactin elevation (menstrual irregularities, galactorrhea); sedation |
| Olanzapine | 2.5-5 mg initially; target 5-20 mg/day | Effective for positive and negative symptoms | Significant weight gain (>8 kg/12 weeks); metabolic effects; sedation; sustained prolactin elevation |
| Quetiapine | 25-50 mg initially; target 200-800 mg/day | Improvement in positive and negative symptoms | Postural tachycardia; insomnia; limited research in adolescents |
| Clozapine | 12.5-25 mg initially; target up to 300 mg/day | Superior efficacy, especially for negative symptoms; last resort due to side effects | Somnolence; hypersalivation; significant weight gain; higher seizure risk than adults; enuresis |
Important Nursing Considerations for Adolescents
- Heightened side effect sensitivity: Adolescents experience more weight gain, prolactin effects, and EPS
- Informed consent and assent: Obtain from parents/guardians and adolescents
- Growth and development monitoring: Assess impact on height, weight, sexual development
- Educational impact: Coordinate with school for academic accommodations
- Family involvement: Essential for treatment adherence and support
Mnemonic: “TEENS” – Assessment Focus for Adolescent Schizophrenia
- T – Thought process (assess cognitive disorganization, delusions)
- E – Educational functioning (school performance, attendance)
- E – Emotional regulation (mood, anxiety, irritability)
- N – Negative symptoms (anhedonia, social withdrawal)
- S – Social connections (peer relationships, family dynamics)
Schizophrenia with Substance Abuse
Substance abuse is significantly more prevalent among people with schizophrenia than in the general population, with conservative estimates indicating that one-third to one-half of schizophrenia patients abuse alcohol and illicit drugs. This dual diagnosis presents unique challenges for treatment and nursing care.
Key Statistics
30-50%
Of people with schizophrenia have comorbid substance use disorders
3-4×
Higher rates of relapse and rehospitalization in dual diagnosis patients
↑ Risk
For medication side effects and treatment non-compliance
Clinical Implications of Dual Diagnosis
Challenges
- Higher rates of medication non-compliance
- Increased frequency of EPS and risk of TD
- Poorer response to conventional antipsychotics
- More florid psychotic symptoms
- Higher relapse rates
- Increased risk of homelessness and legal issues
- Greater burden on caregivers
Paradoxical Strengths
- Often have better premorbid functioning
- Less functional impairment than non-substance-abusing patients
- May represent a subgroup with better potential for recovery and reintegration
- Often more motivated to engage in treatment when properly approached
- Can benefit significantly from integrated treatment models
Treatment Approaches for Dual Diagnosis
Second-generation antipsychotics (SGAs) are generally preferred for schizophrenia patients with comorbid substance abuse:
| Medication | Evidence in Dual Diagnosis | Special Considerations |
|---|---|---|
| Clozapine | Growing evidence for reduced cravings and substance use; similar response rates in substance users and non-users | Only SGA shown to potentially reduce substance use; may diminish cocaine effects and related paranoia |
| Risperidone | Case reports of effectiveness in substance-induced psychosis; limited evidence for reducing substance use | Lower rates of rehospitalization; better compliance than conventional antipsychotics |
| Olanzapine | Similar response in substance-abusing and non-abusing populations; may improve cannabis-induced psychosis | Patients with history of substance abuse may have higher TD rates at baseline that improve with treatment |
| Quetiapine | Limited data for dual diagnosis patients | Potential for misuse due to sedative properties; monitor for diversion |
Mnemonic: “SUBSTANCE” – Nursing Approach for Dual Diagnosis
- S – Screen regularly for substance use
- U – Understand reasons for substance use (self-medication, social factors)
- B – Build therapeutic alliance without judgment
- S – Support harm reduction strategies
- T – Track medication effects and interactions
- A – Address both disorders simultaneously
- N – Navigate integrated treatment services
- C – Coordinate with addiction specialists
- E – Educate about interactions between substances and medications
Integrated Treatment Model
Integrated Assessment
Mental health + substance use
Motivational Interviewing
Enhance readiness to change
Dual Treatment
Both disorders simultaneously
Relapse Prevention
For both conditions
Critical Nursing Monitoring
- Drug interactions: Substances may interact with antipsychotics (e.g., alcohol enhances sedation)
- Medication adherence: Higher rates of non-compliance require creative approaches
- Heightened side effects: More frequent EPS and increased TD risk
- Metabolic monitoring: Substance use may exacerbate metabolic effects of SGAs
- Vital sign changes: Monitor for substance intoxication or withdrawal
Treatment-Resistant Schizophrenia
Approximately 20-30% of patients with schizophrenia do not respond adequately to standard antipsychotic treatments. These patients experience persistent symptoms, functional impairment, and often require extensive periods of hospitalization. Understanding treatment resistance is essential for appropriate nursing care.
Defining Treatment Resistance
Modified Kane Criteria for Treatment Resistance
- Persistent positive psychotic symptoms (hallucinations, delusions, thought disorder)
- Moderately severe illness as rated by standardized scales (BPRS score ≥45, CGI score ≥4)
- Persistence of illness with no period of good social/occupational functioning in past 5 years
- Inadequate response to at least two antipsychotic trials of sufficient dose and duration
What Constitutes an Adequate Trial?
- 4-6 weeks of treatment
- Adequate dosage (equivalent to 400-600 mg/day of chlorpromazine)
- Confirmed medication adherence
- Two separate trials (can be one retrospective and one prospective)
- Less than 7% chance of responding to a third conventional antipsychotic after failing two trials
Neurobiological Factors
- Increased cortical atrophy on MRI
- Lower catecholamine levels in cerebrospinal fluid
- Response to early treatment predictive of overall response
- Higher cognitive disorganization
- Low ratio of CSF homovanillic acid to 5-hydroxyindoleacetic acid associated with clozapine response
Treatment Approaches
A systematic approach is recommended for treatment-resistant schizophrenia:
Verify Treatment Resistance
Confirm diagnosis, adequate previous trials, medication adherence, rule out substance abuse or comorbidities
Trial of a Second-Generation Antipsychotic
If not already tried, assess response to risperidone, olanzapine, or other SGAs (except clozapine)
Clozapine Trial
Only medication with proven efficacy in treatment-resistant schizophrenia (30-50% response rate)
Clozapine Augmentation Strategies
For partial response to clozapine, consider augmentation with another antipsychotic or mood stabilizer
Alternative Strategies
ECT in combination with antipsychotics; other adjunctive therapies (e.g., lamotrigine)
Medication Approaches in Treatment Resistance
| Treatment | Evidence | Response Rate | Nursing Considerations |
|---|---|---|---|
| Clozapine | Only medication with proven efficacy in rigorous trials | 30-50% | Weekly blood monitoring; slow titration; monitor for agranulocytosis, seizures, myocarditis, metabolic effects |
| Risperidone | Higher response than haloperidol in treatment-resistant patients | ~24% | Monitor for EPS at higher doses; prolactin-related effects; metabolic effects |
| Olanzapine | Mixed results in well-characterized treatment-resistant patients | 7-36% | Monitor for significant weight gain; metabolic syndrome; sedation |
| Quetiapine | Limited data for treatment resistance | Not well established | Monitor for sedation; orthostatic hypotension; metabolic effects |
| Clozapine + Risperidone | Case reports suggest added benefit | Not well established | Monitor for additive side effects; combination may enhance D2 blockade |
| Antipsychotic + ECT | Favorable short-term response; limited long-term data | ~20% | Monitor cognitive effects; prepare patient for procedure; assess memory |
Clozapine Monitoring Requirements
- Absolute neutrophil count (ANC): Weekly for 6 months, then every 2 weeks for 6 months, then monthly
- Vital signs: Regular monitoring for tachycardia, fever, and orthostatic changes
- Seizure precautions: Risk increases with doses >600 mg/day; myoclonus may precede seizures
- Cardiovascular: ECG monitoring; echocardiogram if myocarditis suspected
- Metabolic parameters: Weight, glucose, lipids at baseline and regular intervals
- Bowel function: Constipation can be severe and even life-threatening
Mnemonic: “CLOZAPINE” – Key Nursing Considerations
- C – Complete blood count monitoring weekly
- L – Low starting dose with slow titration
- O – Orthostatic hypotension monitoring
- Z – Zero tolerance for missed monitoring
- A – Agranulocytosis risk (teach signs of infection)
- P – Prevent constipation (hydration, fiber)
- I – Increased salivation management
- N – Neurological side effects (seizures, myoclonus)
- E – Educate about metabolic monitoring
Follow-up and Home Care in Schizophrenia
Effective follow-up care is essential for long-term management of schizophrenia and prevention of relapse. Research indicates that adequate follow-up and home care can significantly reduce rehospitalization rates and improve quality of life for patients with schizophrenia.
Key Components of Follow-up Care
- Regular psychiatric assessment (at least every 1-3 months during stable periods)
- Medication management and monitoring
- Side effect assessment and management
- Psychosocial intervention continuation
- Family support and education
- Crisis management planning
- Physical health monitoring
Benefits of Structured Follow-up
- Reduces rehospitalization rates by up to 40%
- Improves medication adherence
- Earlier detection of relapse signs
- Increased continuity of care
- Better management of comorbid conditions
- Reduced burden on families
- Improved long-term functional outcomes
Post-Discharge Follow-up Timeline
Critical Period (1-7 days)
- First follow-up within 7 days of discharge (ideally within 48-72 hours)
- Medication review and adjustment
- Assessment of immediate needs
- Crisis plan review
Stabilization (1-3 months)
- Biweekly to monthly appointments
- Medication optimization
- Integration of psychosocial interventions
- Family education and support
Maintenance (Ongoing)
- Monthly to quarterly appointments
- Regular medication review
- Continued psychosocial support
- Focus on recovery and functioning
Medication Monitoring
| Parameter | Frequency | Nursing Considerations |
|---|---|---|
| Medication adherence | Every visit | Assess barriers; consider long-acting injectables for non-adherence; pill counts; family involvement |
| Side effect assessment | Every visit | Systematic use of rating scales (AIMS, Barnes Akathisia Scale); patient-reported side effects |
| Metabolic monitoring | Weight monthly; glucose and lipids quarterly to annually | Document BMI; provide lifestyle counseling; refer for abnormal values |
| Blood pressure | Every visit | Monitor for orthostatic changes, especially in elderly; track trends over time |
| Prolactin-related effects | Ask at every visit; test levels if symptomatic | Assess for gynecomastia, galactorrhea, sexual dysfunction, menstrual irregularities |
| Specific monitoring (e.g., clozapine) | Per medication protocol | Ensure no gaps in required monitoring; coordinate with pharmacy systems |
Home Care Strategies
Medication Management
- Pill organizers/reminder systems
- Simplified medication regimens
- Medication calendars or apps
- Family education on medication
- Long-acting injectable options
Daily Structure
- Consistent daily routines
- Regular sleep schedule
- Meal planning and nutrition
- Activity scheduling
- Time management skills
Early Warning Signs
- Personalized relapse signature
- Symptom tracking tools
- Family education on warning signs
- Action plan for emerging symptoms
- Emergency contact information
Mnemonic: “HOME CARE” – Essential Elements of Follow-up
- H – Health monitoring (physical and mental)
- O – Optimize medication regimen
- M – Monitor for early warning signs
- E – Educate patient and family
- C – Coordinate care among providers
- A – Address psychosocial needs
- R – Reassess treatment plan regularly
- E – Engage in rehabilitation activities
Family Support and Education
Family involvement is a critical component of successful follow-up care, with research showing family psychoeducation reduces relapse rates by up to 20%.
Family Psychoeducation Elements
Content Areas
- Nature, symptoms, and diagnosis of schizophrenia
- Treatment options and medication effects
- Early warning signs and relapse prevention
- Crisis management strategies
- Communication and problem-solving skills
Delivery Methods
- Multiple-family groups (most effective)
- Individual family sessions
- Combined patient-family sessions
- Peer-led support groups
- Online resources and virtual support
Critical Red Flags Requiring Immediate Attention
- Suicidal ideation or behavior (10% lifetime suicide risk in schizophrenia)
- Homicidal ideation or threat of violence
- Severe medication side effects (e.g., signs of agranulocytosis, NMS, severe EPS)
- Complete medication non-adherence
- Acute psychotic decompensation with inability to care for self
- Substance intoxication or severe withdrawal
Rehabilitation in Schizophrenia
Rehabilitation interventions are essential complements to medication management in schizophrenia. They target functional recovery, community integration, and quality of life. Only about 13.5% of individuals with schizophrenia meet criteria for recovery that remains stable over time, highlighting the need for comprehensive rehabilitation approaches.
Factors Affecting Functional Outcomes
Disease-Related
- Neurocognitive impairment
- Social cognition deficits
- Negative symptoms
- Functional capacity
Personal Resources
- Resilience
- Self-efficacy
- Motivation
- Engagement with services
Environmental
- Social support
- Internalized stigma
- Access to resources
- Community opportunities
Key Rehabilitation Approaches
Focus: Improving cognitive impairments (attention, memory, executive function)
Effectiveness:
- Moderate effect on cognitive performance (ES=0.45)
- Small-medium effect on social functioning (ES=0.36)
- Small effect on symptoms (ES=0.28)
- More effective when combined with other rehabilitation
Focus: Teaching interpersonal skills, problem-solving, conversation skills
Effectiveness:
- Strong effect on skills acquisition (ES=0.77)
- Moderate effect on social functioning (ES=0.52)
- Moderate effect on negative symptoms (ES=0.40)
- Moderate effect on reducing hospitalization (ES=0.48)
Focus: Modifying dysfunctional beliefs, coping with symptoms
Effectiveness:
- Moderate effect on positive symptoms (ES=0.37)
- Moderate effect on negative symptoms (ES=0.44)
- Moderate effect on social functioning (ES=0.38)
- Effective for reducing distress related to symptoms
Implementing Rehabilitation Interventions
Comprehensive Functional Assessment
Conduct a thorough assessment of cognitive function, social skills, daily living skills, vocational abilities, and symptom impact on functioning.
Tools: UCSD Performance-Based Skills Assessment (UPSA), Social Functioning Scale (SFS), cognitive assessments
Individualized Rehabilitation Plan
Develop a plan targeting specific functional domains based on assessment results and patient goals.
Example: For someone with social cognition deficits and employment goals, combine social cognition training with supported employment
Implementation of Targeted Interventions
Deliver evidence-based interventions focusing on areas of greatest need and potential impact.
Match intensity to patient capacity; ensure regular attendance and engagement
Skill Transfer to Real-World Settings
Incorporate strategies to promote generalization of skills to everyday environments.
Use homework assignments, in vivo practice, community outings, and family involvement
Regular Reassessment and Plan Adjustment
Systematically reassess progress and adjust interventions as needed.
Document functional improvements, not just symptom changes
Specific Rehabilitation Programs
| Program | Target Population | Components | Evidence Summary |
|---|---|---|---|
| Cognitive Behavioral Social Skills Training (CBSST) | Adults over 45 with schizophrenia | Combines CBT, social skills training, and problem-solving training | Improves insight, social activities, and overall functioning; benefits maintained 1 year after treatment |
| Functional Adaptation Skills Training (FAST) | Adults over 40 with schizophrenia | 24-week program targeting medication management, social skills, communication, organization, transportation, finances | Enhances everyday living skills and social skills; benefits maintained at 3-month follow-up |
| Helping Older People Experience Success (HOPES) | Older adults with serious mental illness | Social rehabilitation and integrated health care program | Improvements in social skills, psychosocial functioning, community functioning, negative symptoms, and self-efficacy |
| Integrated Psychological Therapy (IPT) | Adults with schizophrenia | Combines cognitive remediation and social skills training | More effective than standard care for cognition, psychosocial functioning, and negative symptoms |
| Supported Employment (SE) | Adults with schizophrenia seeking employment | Rapid job placement with ongoing support; competitive employment | Superior to traditional vocational rehabilitation; improved employment rates, hours worked, and wages earned |
Mnemonic: “RECOVER” – Key Rehabilitation Principles
- R – Restore cognitive and functional abilities
- E – Encourage skill practice in real-world settings
- C – Collaborate with patients on meaningful goals
- O – Optimize environmental supports
- V – Validate progress and strengths
- E – Engage family and support network
- R – Reinforce integration of multiple approaches
Addressing Barriers to Rehabilitation
- Negative symptoms: Use motivational interviewing, small achievable goals, rewards
- Cognitive impairment: Adapt pace, use repetition, written materials, memory aids
- Stigma: Address self-stigma, provide psychoeducation, peer support
- Access to services: Telehealth options, mobile interventions, transportation assistance
- Engagement: Build therapeutic alliance, align with personal goals, involve supports
Summary: Integrating Care Across Special Populations
Providing comprehensive care for special populations with schizophrenia requires integrating medication management, psychosocial approaches, and rehabilitation strategies tailored to each group’s unique needs.
| Population | Key Medication Considerations | Psychosocial Focus | Rehabilitation Emphasis |
|---|---|---|---|
| Geriatric Patients | Lower doses (25-50% of adult dose); start low, go slow; monitor for anticholinergic effects, EPS, TD, orthostasis | Maintaining independence; compensating for sensory/cognitive changes; fall prevention | Functional maintenance; social connection; caregiver support; physical health |
| Adolescents | Higher sensitivity to side effects; monitoring growth and development; more pronounced weight gain | Educational support; family involvement; developmental considerations; peer relationships | Age-appropriate skill development; normative experiences; identity formation |
| Substance Abusers | Consider clozapine for substance reduction; monitor for interactions; higher risk of non-adherence | Integrated dual diagnosis treatment; motivational interviewing; harm reduction | Substance-specific skills; relapse prevention for both conditions; healthy alternatives |
| Treatment-Resistant | Trial of clozapine; augmentation strategies; medication combinations; careful monitoring | Focus on residual symptoms; realistic goal-setting; acceptance of limitations | Compensatory strategies; maximizing strengths; environmental accommodations |
Key Principles Across Populations
Person-Centered Approach
- Focus on individual needs, preferences, and strengths
- Shared decision-making
- Recovery-oriented care
- Cultural competence
Integrated Care Model
- Coordination between providers
- Addressing physical and mental health
- Combining pharmacological and non-pharmacological approaches
- Continuity across services
Proactive Monitoring
- Regular assessment of symptoms and functioning
- Early intervention for emerging issues
- Systematic side effect monitoring
- Adjustment of interventions as needed
Final Nursing Considerations
- Document progress using standardized assessments when possible
- Maintain therapeutic optimism – recovery is possible at any stage
- Advocate for access to comprehensive services
- Support transitions between levels of care
- Educate about serious but rare side effects requiring immediate attention
- Balance independence with appropriate support
- Involve peer specialists when available
- Address comorbid physical health conditions
- Recognize and respect patient autonomy
- Maintain hope and focus on quality of life
References
- Jeste DV, Maglione JE. Treating older adults with schizophrenia: challenges and opportunities. Schizophr Bull. 2013;39(5):966-968.
- Morin L, Franck N. Rehabilitation interventions to promote recovery from schizophrenia: a systematic review. Front Psychiatry. 2017;8:100.
- Conley RR, Kelly DL. Treatment of the special patient with schizophrenia. Dialogues Clin Neurosci. 2001;3(2):123-135.
- Xia J, Merinder LB, Belgamwar MR. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. 2011;6:CD002831.
- Kurtz MM, Mueser KT. A meta-analysis of controlled research on social skills training for schizophrenia. J Consult Clin Psychol. 2008;76:491-504.
- Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168:472-485.
- McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164:1791-1802.
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models and methodological rigor. Schizophr Bull. 2008;34:523-537.
- Galderisi S, Rossi A, Rocca P, et al. The influence of illness-related variables, personal resources, and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13:275-287.
- Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39:1296-1306.
