Bronchial Asthma Nursing Care Plan
Comprehensive Guide for Nursing Students
Table of Contents
Introduction to Bronchial Asthma
Bronchial asthma is a chronic inflammatory disease of the airways characterized by hyperresponsiveness, mucosal edema, and excessive mucus production. This inflammation leads to recurrent episodes of coughing, chest tightness, wheezing, and dyspnea.
Asthma affects approximately 26 million people in the United States and is the most common chronic disease in childhood. The bronchial asthma nursing care plan is essential for effective management of this condition across all healthcare settings.
Key Statistics
- Affects ~26 million Americans
- Most common chronic disease in childhood
- 5-10% of hospital admissions for asthma require ICU care
- Approximately 20-40% of patients have increased sputum volume and mucus hypersecretion
Risk Factors for Bronchial Asthma
- Family history of asthma or allergies
- Allergies to airborne substances
- Chronic exposure to air pollutants
- Respiratory infections in childhood
- Obesity (4-6× higher hospitalization risk)
- Occupational exposures
- Smoking or exposure to secondhand smoke
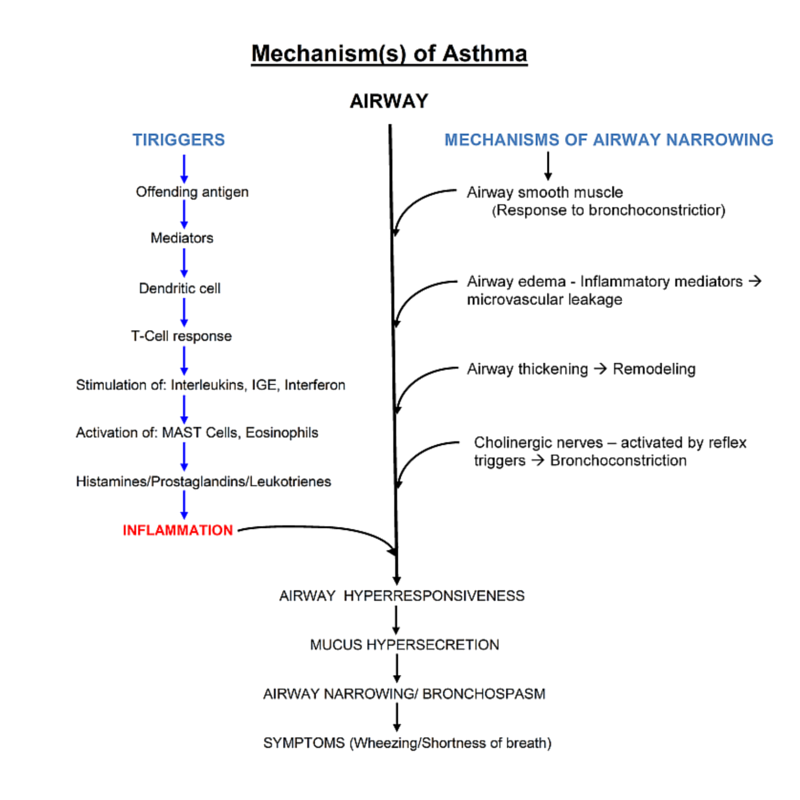
Pathophysiology of Bronchial Asthma
Understanding Asthma Pathophysiology
The pathological process of asthma begins with the inhalation of an irritant or allergen, which triggers an inflammatory cascade in the airways. This cascade includes:
- Airway Inflammation: Release of inflammatory mediators like histamine, leukotrienes, and cytokines
- Bronchial Hyperreactivity: Increased sensitivity to various stimuli
- Bronchospasm: Contraction of bronchial smooth muscle
- Mucosal Edema: Swelling of the airway lining
- Mucus Hypersecretion: Increased production of thick mucus
These changes ultimately lead to airway narrowing, increased airway resistance, and the classic symptoms of asthma. If not corrected rapidly, mucus production can prevent inhaled medications from reaching the mucosa, making the condition more difficult to treat.

Normal vs. Asthmatic Airways
Normal Airway
- Relaxed bronchial smooth muscle
- Normal epithelial lining
- Minimal mucus production
- No inflammatory cell infiltration
- Adequate airflow during respiration
Asthmatic Airway
- Contracted bronchial smooth muscle
- Thickened, damaged epithelium
- Excessive, thick mucus production
- Inflammatory cell infiltration (eosinophils, mast cells)
- Impaired airflow, especially during expiration
Ventilation-Perfusion Mismatch in Asthma
During asthma exacerbations, narrowed airways create areas that are ventilated but poorly perfused. This V/Q mismatch results in:
- Early hypoxemia without CO₂ retention
- Respiratory alkalosis (early stage)
- Respiratory acidosis (later stage as exhaustion sets in)
- Increased work of breathing and oxygen consumption
Clinical Note: This understanding is crucial for developing an effective bronchial asthma nursing care plan focused on improving gas exchange.
Assessment of Bronchial Asthma
A thorough assessment is the foundation of an effective bronchial asthma nursing care plan. Nurses should systematically evaluate the following areas:
Subjective Data
- Dyspnea: Shortness of breath, especially with exertion
- Chest tightness: Sensation of pressure or constriction
- Cough: Often nonproductive, worse at night
- Wheezing: Self-reported or noted during exhalation
- History: Frequency and severity of attacks
- Triggers: Environmental, emotional, or physical
- Sleep patterns: Nocturnal symptoms disrupting sleep
- Activity limitations: Restrictions due to symptoms
- Anxiety levels: Related to breathlessness
Objective Data
- Respiratory rate and pattern: Typically increased
- Adventitious breath sounds: Wheezes, rhonchi
- Use of accessory muscles: For breathing
- Nasal flaring: Especially in children
- Prolonged expiration: Compared to inspiration
- Vital signs: Tachycardia, potentially hypertension
- Oxygen saturation: May be decreased
- Peak expiratory flow rate: Typically reduced
- Arterial blood gases: May show hypoxemia
Diagnostic Criteria
| Assessment Parameter | Mild | Moderate | Severe | Life-Threatening |
|---|---|---|---|---|
| Breathlessness | Walking | Talking | At rest | Respiratory arrest imminent |
| Speech | Can complete sentences | Phrases only | Words only | Unable to speak |
| Alertness | Normal | May be agitated | Usually agitated | Confusion or drowsiness |
| Respiratory Rate | Increased | Increased | Often >30/min | Bradypnea or exhaustion |
| Wheeze | Moderate, end-expiratory | Loud throughout expiration | Loud, inspiratory and expiratory | Silent chest (severe limitation) |
| Pulse Rate | <100 bpm | 100-120 bpm | >120 bpm | Bradycardia |
| O₂ Saturation | >95% | 91-95% | <91% | <88% |
| PEF (% predicted) | >80% | 60-80% | <60% | <33% or unable to measure |
| Pulsus Paradoxus | Absent | May be present (10-15 mmHg) | Often present (15-40 mmHg) | May be absent (fatigue) |
Clinical Examinations
- Spirometry (FEV₁, FVC measurements)
- Peak flow measurements
- Bronchodilator reversibility testing
- Chest x-ray (complications/alternatives)
- Allergy testing (if indicated)
Laboratory Tests
- Complete blood count (eosinophilia)
- Arterial blood gases
- Serum IgE levels
- Sputum analysis
- Electrolyte monitoring (with β-agonist use)
Red Flag Findings
- Silent chest (severe obstruction)
- Cyanosis or SpO₂ <90%
- Inability to complete sentences
- Altered mental status
- Respiratory fatigue or acidosis
Assessment Tip:
Remember that absent wheezing in a severely dyspneic patient may indicate critical airway obstruction with insufficient airflow to generate wheezing sounds. This is a medical emergency requiring immediate intervention.
10 Nursing Diagnoses for Bronchial Asthma
The following nursing diagnoses form the foundation of a comprehensive bronchial asthma nursing care plan. Each diagnosis addresses specific aspects of patient care and management.
Ineffective Breathing Pattern
Related to bronchospasm, airway inflammation, mucosal edema, and increased work of breathing.
As evidenced by: Dyspnea, use of accessory muscles, altered chest excursion, tachypnea, prolonged expiratory phase, and abnormal blood gases.
Ineffective Airway Clearance
Related to bronchospasm, increased mucus production, thick secretions, and ineffective cough.
As evidenced by: Adventitious breath sounds (wheezes, crackles), ineffective cough, changes in respiratory rate, and difficulty expectorating secretions.
Impaired Gas Exchange
Related to ventilation-perfusion mismatch and alveolar-capillary membrane changes secondary to airway inflammation.
As evidenced by: Hypoxemia, hypercapnia, abnormal ABGs, dyspnea, and cyanosis.
Anxiety
Related to breathlessness, hypoxia, unfamiliar environment, and perceived threat to well-being.
As evidenced by: Expressed concerns, restlessness, increased heart rate, fear, and feeling of suffocation.
Activity Intolerance
Related to imbalance between oxygen supply and demand, increased work of breathing, and fatigue.
As evidenced by: Dyspnea with activity, fatigue, weakness, and inability to perform usual activities.
Deficient Knowledge
Related to lack of information about asthma pathophysiology, treatment regimen, trigger management, and action plan.
As evidenced by: Questions about condition, misconceptions, inaccurate follow-through of instructions, and development of preventable complications.
Risk for Infection
Related to stasis of respiratory secretions, compromised immune function from corticosteroid therapy, and chronic disease.
As evidenced by: Potential for developing respiratory infections that can trigger asthma exacerbations.
Fatigue
Related to increased work of breathing, stress of illness, sleep deprivation from nocturnal symptoms, and hypoxemia.
As evidenced by: Verbalized exhaustion, inability to maintain normal routines, lethargy, and decreased performance.
Ineffective Coping
Related to situational crisis of acute exacerbation, chronic illness management demands, and inadequate support systems.
As evidenced by: Verbalized difficulty managing condition, non-adherence to treatment plan, and expressed feelings of powerlessness.
Risk for Aspiration
Related to increased respiratory secretions, impaired swallowing during severe respiratory distress, and potential for respiratory failure.
As evidenced by: Risk factors including severe dyspnea, altered level of consciousness during severe exacerbations, or GERD comorbidity.
Nursing Diagnosis Selection Tip:
When formulating a bronchial asthma nursing care plan, prioritize diagnoses based on Maslow’s hierarchy of needs. Address physiological needs first (breathing, oxygenation), followed by safety needs (prevention of complications), and then psychosocial needs (education, coping).
Mnemonics and Memory Aids
These mnemonics will help you remember key aspects of bronchial asthma nursing care plans and interventions.
ASTHMA Treatment Mnemonic
Adrenergics
Short-acting beta-agonists like albuterol for quick relief
Steroids
Inhaled or oral corticosteroids to reduce inflammation
Theophylline
Bronchodilator that relaxes smooth muscle
Hydration
Adequate fluid intake to thin secretions
Mast cell stabilizers
Medications like cromolyn sodium to prevent histamine release
Anticholinergics
Medications like ipratropium to reduce mucus secretion
WHEEZE Assessment Mnemonic
Work of breathing
Assess use of accessory muscles, retractions
Hypoxemia signs
Check for cyanosis, confusion, oxygen saturation
Expiratory phase
Note prolonged expiration, I:E ratio changes
Effort tolerance
Evaluate activity limitations, fatigue level
Zest for breathing
Assess anxiety, panic, perception of breathlessness
Educational needs
Identify knowledge gaps about asthma management
A CHEST Mnemonic for Life-Threatening Asthma
Altered consciousness
Confusion, drowsiness
Cyanosis
Central cyanosis indicates severe hypoxemia
Hypotension
Sign of respiratory failure and impending arrest
Exhaustion
Inability to continue effective breathing
Silent chest
Absence of wheezing due to severe airflow limitation
Tachycardia/bradycardia
Severe tachycardia or late bradycardia
BREATHE Patient Education Mnemonic
Bronchodilators
Proper use and timing of rescue medications
Recognize triggers
Identify and avoid personal asthma triggers
Environmental control
Home modifications to reduce allergens
Action plan
Written plan for daily management and exacerbations
Technique check
Regularly review inhaler technique
Health maintenance
Regular follow-up with healthcare providers
Exercise appropriately
Safe physical activity with proper precautions

Comprehensive Care Plans
Below are detailed nursing care plans for the top five priority diagnoses in bronchial asthma nursing care plan management.
Care Plan 1: Ineffective Breathing Pattern
| Assessment | Nursing Interventions | Rationale | Expected Outcomes |
|---|---|---|---|
|
|
|
|
Care Plan 2: Ineffective Airway Clearance
| Assessment | Nursing Interventions | Rationale | Expected Outcomes |
|---|---|---|---|
|
|
|
|
Care Plan 3: Impaired Gas Exchange
| Assessment | Nursing Interventions | Rationale | Expected Outcomes |
|---|---|---|---|
|
|
|
|
Care Plan 4: Anxiety
| Assessment | Nursing Interventions | Rationale | Expected Outcomes |
|---|---|---|---|
|
|
|
|
Care Plan 5: Deficient Knowledge
| Assessment | Nursing Interventions | Rationale | Expected Outcomes |
|---|---|---|---|
|
|
|
|
Care Plan Implementation Tip:
A successful bronchial asthma nursing care plan requires continuous assessment and adjustment. Regularly evaluate the patient’s response to interventions and modify the care plan accordingly. Document all assessments, interventions, and patient responses thoroughly to ensure continuity of care.
Medication Management
Medication management is a critical component of bronchial asthma nursing care plans. Understanding the various medication categories, their actions, and nursing considerations is essential for effective patient care.
| Medication Category | Examples | Action | Nursing Considerations |
|---|---|---|---|
| Short-Acting Beta-Agonists (SABAs) |
|
Rapid bronchodilation by relaxing bronchial smooth muscle. Used for quick relief during acute symptoms. |
|
| Inhaled Corticosteroids (ICS) |
|
Reduce airway inflammation, hyperresponsiveness, and mucus production. Primary controller medication for persistent asthma. |
|
| Long-Acting Beta-Agonists (LABAs) |
|
Extended bronchodilation (12+ hours). Used as add-on therapy with ICS for persistent asthma. |
|
| Combination Inhalers |
|
Combines anti-inflammatory and bronchodilator effects. Improves compliance with dual therapy. |
|
| Anticholinergics |
|
Blocks acetylcholine receptors in bronchial smooth muscle causing bronchodilation. Often used as adjunct therapy. |
|
| Leukotriene Modifiers |
|
Block leukotriene pathway, reducing inflammation, mucus production, and bronchoconstriction. Oral tablets for daily use. |
|
| Systemic Corticosteroids |
|
Powerful anti-inflammatory drugs used for moderate to severe exacerbations. Available in oral and intravenous forms. |
|
| Biologic Therapies |
|
Target specific inflammatory pathways. Used for severe, refractory asthma with specific phenotypes (e.g., eosinophilic, allergic). |
|
Stepwise Approach to Medication
Asthma medications are adjusted based on control level and severity:
- Step 1: As-needed SABA (intermittent asthma)
- Step 2: Low-dose ICS + as-needed SABA
- Step 3: Medium-dose ICS or Low-dose ICS + LABA
- Step 4: Medium-dose ICS + LABA
- Step 5: High-dose ICS + LABA ± additional controller
- Step 6: High-dose ICS + LABA + oral corticosteroids ± biologics
Note: Step up when uncontrolled; step down when controlled for 3+ months
Inhaler Technique Teaching Points
Include these in your bronchial asthma nursing care plan:
- Remove cap and shake inhaler (if required)
- Breathe out completely away from inhaler
- Place mouthpiece in mouth or 1-2 inches from open mouth
- Begin slow, deep inhalation and press canister
- Continue inhaling slowly and deeply
- Hold breath for 10 seconds
- Wait 1 minute between puffs if multiple doses
- Rinse mouth after ICS use
- Clean device per manufacturer’s instructions

Asthma Action Plan
An asthma action plan is an essential component of a comprehensive bronchial asthma nursing care plan. It provides personalized written instructions for daily management and handling of asthma exacerbations.
Components of an Asthma Action Plan
-
Personal Information: Patient name, emergency contacts, healthcare provider information
-
Asthma Severity Classification: Intermittent, mild persistent, moderate persistent, or severe persistent
-
Known Triggers: List of patient-specific asthma triggers to avoid
-
Peak Flow Zones: Personal best and zone thresholds (green, yellow, red)
-
Daily Medications: Controller medications with dosages and schedules
-
Zone-Based Instructions: Actions for each control level
-
Emergency Instructions: When to call provider or seek emergency care
The Zone System
GREEN ZONE: Doing Well
Symptoms: No cough, wheeze, chest tightness, or shortness of breath
Peak Flow: 80-100% of personal best
Actions: Take controller medications as prescribed
YELLOW ZONE: Caution
Symptoms: Some symptoms, mild activity limitations, waking at night
Peak Flow: 50-80% of personal best
Actions: Continue controller medications plus rescue inhaler, monitor response
RED ZONE: Medical Alert
Symptoms: Severe shortness of breath, difficulty talking, blue lips/fingernails
Peak Flow: Below 50% of personal best
Actions: Use rescue medications immediately, call provider or 911
Nursing Role in Asthma Action Plan Development
| Role | Actions |
|---|---|
| Assessment |
|
| Plan Development |
|
| Education |
|
| Follow-up |
|
Clinical Tip:
When implementing an asthma action plan as part of a bronchial asthma nursing care plan, ensure the patient demonstrates their understanding by having them teach-back the essential components. Provide copies for home, work/school, and all caregivers. Consider using smartphone apps for digital versions that patients can access anywhere.

Patient Education
Patient education is a critical component of a bronchial asthma nursing care plan. Effective education empowers patients to manage their condition and prevent exacerbations.
Core Educational Topics
Disease Process
Explain asthma pathophysiology using simple language and visual aids. Help patients understand that asthma is a chronic inflammatory condition requiring ongoing management.
Medication Purpose and Use
Distinguish between controller and rescue medications. Explain why daily controller medications are necessary even when feeling well.
Inhaler Technique
Demonstrate and have patients return-demonstrate proper inhaler technique. Review technique at each visit as errors commonly develop over time.
Trigger Identification and Avoidance
Help patients identify personal triggers and develop practical strategies for avoiding or minimizing exposure.
Self-Monitoring
Teach symptom recognition and peak flow monitoring. Explain how to interpret results and respond appropriately.
Educational Strategies
Personalize Information
Tailor education to the patient’s specific asthma phenotype, triggers, lifestyle, and health literacy level.
Use Multiple Modalities
Incorporate verbal instruction, written materials, videos, apps, and hands-on demonstrations to accommodate different learning styles.
Teach-Back Method
Ask patients to explain concepts back in their own words to verify understanding.
Involve Support Persons
Include family members or caregivers in education sessions, especially for children and elderly patients.
Reinforce and Review
Provide ongoing education at each visit, reinforcing key concepts and addressing new questions.
Special Education Topics
| Topic | Key Points |
|---|---|
| Exercise-Induced Bronchoconstriction |
|
| Environmental Control Measures |
|
| Device Maintenance |
|
| Comorbidity Management |
|
Important Education Points:
When developing your bronchial asthma nursing care plan, be sure to include these critical patient education elements:
- Early warning signs of worsening asthma (increased nighttime awakenings, increased rescue inhaler use)
- When and how to seek emergency care (severe breathlessness, inability to speak in full sentences)
- The importance of carrying rescue medication at all times
- The need for annual influenza vaccination and appropriate pneumococcal vaccination
- Avoiding medications that may worsen asthma (certain NSAIDs, beta-blockers)
Complication Prevention
An effective bronchial asthma nursing care plan must address the prevention of both acute exacerbations and long-term complications.
Preventing Acute Exacerbations
Medication Adherence
Encourage strict adherence to controller medications even during symptom-free periods. Non-adherence is a leading cause of preventable exacerbations.
Trigger Avoidance
Help patients identify and develop strategies to avoid personal triggers, including allergens, irritants, exercise in extreme conditions, and respiratory infections.
Regular Monitoring
Encourage daily symptom monitoring and peak flow measurements to detect early signs of worsening control.
Follow-up Care
Ensure patients attend regular follow-up appointments for ongoing assessment and medication adjustment as needed.
Infection Prevention
Encourage annual influenza vaccination, appropriate pneumococcal vaccination, and good hand hygiene to prevent respiratory infections.
Preventing Long-term Complications
Airway Remodeling
Early and consistent use of anti-inflammatory medications helps prevent permanent structural changes in airways that can lead to fixed airflow obstruction.
Medication Side Effects
Monitor for and manage side effects of long-term medications, such as oral thrush from ICS or bone density issues with systemic steroids.
Psychosocial Impact
Address anxiety, depression, and social isolation that may develop with chronic asthma, especially in patients with severe disease.
Growth Effects in Children
Monitor growth in children on high-dose ICS and adjust therapy as needed to minimize growth effects while maintaining control.
Exercise Deconditioning
Encourage appropriate physical activity to prevent deconditioning, which can worsen asthma symptoms over time.
Nursing Interventions for Complication Prevention
| Complication | Nursing Interventions |
|---|---|
| Status Asthmaticus |
|
| Respiratory Failure |
|
| Pneumothorax |
|
| Medication Side Effects |
|
| Social and Psychological Impact |
|
Prevention Protocol Tip:
When implementing a bronchial asthma nursing care plan, use the “Teachable Moment” approach after an exacerbation. Patients are often more receptive to prevention education during recovery from an acute episode. Review what triggered the exacerbation, how it might have been prevented, and reinforce proper response for future episodes.
References
- Morris, M. J., & Mosenifar, Z. (2022). Asthma. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK568760/
- Hashmi, M. F., Tariq, M., & Cataletto, M. E. (2022). Asthma. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK568735/
- Nurseslabs. (2023). Asthma Nursing Care Plans. https://nurseslabs.com/asthma-nursing-care
