Directing and Leading in Nursing Management
Comprehensive Educational Notes for Nursing Students
Table of Contents
Introduction
Directing and leading are critical functions in nursing management that drive healthcare organizations toward their goals by guiding, motivating, and coordinating the efforts of nursing personnel. Effective leadership within the directing function transforms plans into actions and ensures quality patient care outcomes.
Throughout these notes, we’ll explore the principles and elements of directing, the role of supervision and guidance, participatory management approaches, and the importance of interprofessional collaboration in nursing leadership.
Definition of Directing
Directing is the managerial function that involves guiding, leading, supervising, and motivating subordinates to accomplish organizational objectives effectively and efficiently.
In nursing management, directing involves:
- Providing clear instructions and guidance to nursing staff
- Ensuring appropriate implementation of nursing care plans
- Facilitating effective communication among team members
- Motivating staff to achieve optimal patient outcomes
- Supervising nursing activities to maintain quality standards

Figure 1: The basic functions of nursing management including planning, organizing, directing, and controlling
Principles of Directing
Effective directing in nursing management is guided by several key principles that ensure optimal outcomes when implemented correctly.
Harmony of Objectives
Aligning individual staff goals with the overall organizational objectives to create a unified purpose in care delivery.
Unity of Command
Each nurse should receive instructions from only one supervisor to avoid conflict and confusion in task execution.
Maximum Individual Contribution
Encouraging each team member to contribute their best by recognizing their unique skills and experience.
Effective Communication
Ensuring clear, concise, and complete information flow between nurse managers and staff members.
Direct Supervision
Regular face-to-face interaction between nurse leaders and staff to provide immediate guidance and feedback.
Follow-Through
Monitoring tasks from assignment to completion to ensure quality outcomes and address issues promptly.

Figure 2: Key principles of directing applicable to nursing management
Elements of Directing
Directing in nursing management comprises several essential elements that work together to ensure effective care delivery and staff performance.
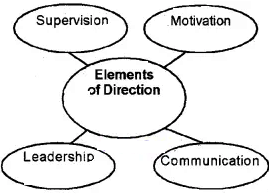
Communication
The process of exchanging information, ideas, and feedback between nurse managers and staff members. Effective communication ensures clarity in instructions, promotes understanding, and fosters a collaborative work environment.
Communication best practices in nursing:
- Use clear, concise language appropriate to the recipient
- Implement standardized handoff protocols (SBAR, I-PASS)
- Provide regular updates on organizational changes
- Encourage open dialogue and active listening
Leadership
The ability to influence and guide nursing staff toward achieving organizational goals. Effective leadership inspires confidence, promotes professional growth, and creates a positive work culture.
Leadership styles in nursing:
- Transformational: Inspires change and innovation
- Democratic: Involves staff in decision-making
- Situational: Adapts style based on circumstances
- Servant: Prioritizes needs of staff and patients
Motivation
The process of stimulating nurses to perform their duties willingly and effectively. Motivation enhances job satisfaction, reduces turnover, and improves overall patient care quality.
Motivational techniques in nursing management:
- Recognition programs for exceptional performance
- Professional development opportunities
- Shared governance and decision-making
- Creating a positive work environment
- Addressing workload concerns promptly
Supervision
The process of overseeing nursing staff performance to ensure quality care delivery and adherence to standards. Effective supervision includes monitoring, guiding, and providing constructive feedback.
Supervision components in nursing:
- Direct observation of practice
- Regular performance reviews
- Just-in-time teaching moments
- Competency assessments
- Documentation review
Supervision and Guidance
Supervision and guidance are critical aspects of the directing function in nursing management, ensuring staff development and quality patient care.
Types of Nursing Supervision
| Type | Description | Application |
|---|---|---|
| One-to-One Supervision | Direct interaction between supervisor and an individual nurse | New staff orientation, remediation, skill development |
| Peer-to-Peer Supervision | Nurses at similar levels supervising each other | Collaborative learning, skill reinforcement |
| Group Supervision | One supervisor guiding multiple nurses simultaneously | Team training, departmental updates, policy reviews |
| Clinical Supervision | Focused on clinical practice and patient care | Evidence-based practice implementation, care protocols |
Effective Guidance Techniques in Nursing
Demonstrating
Showing proper techniques and procedures to ensure correct understanding and application. This is particularly important for complex clinical skills or new equipment use.
Coaching
Providing ongoing support, encouragement, and feedback to help nurses develop their skills and confidence. Effective coaching focuses on strengths while addressing areas for improvement.
Mentoring
Establishing a professional relationship where experienced nurses guide less experienced staff in career development and professional growth beyond basic skills.
Reflecting
Encouraging nurses to analyze their practice, evaluate outcomes, and consider alternative approaches. Reflective practice promotes critical thinking and continuous improvement.
Barriers to Effective Supervision
- Time constraints and high workload
- Inadequate supervisor training
- Resistance from experienced staff
- Lack of organizational support
- Poor communication channels
- Unclear expectations and standards
- Insufficient documentation systems
- Generational differences in work styles
Participatory Management
Participatory management is an approach where nurse managers involve staff in decision-making processes, problem-solving, and planning activities, recognizing their expertise and valuing their input.
Participatory management represents a significant shift from traditional top-down management styles, embracing collaborative leadership and shared governance models that empower nurses at all levels.
Benefits of Participatory Management in Nursing
For Staff Nurses
- Increased job satisfaction and engagement
- Enhanced sense of ownership and autonomy
- Improved professional growth opportunities
- Greater workplace morale and team cohesion
- Reduced moral distress and burnout
For Organizations
- Higher staff retention rates
- Improved quality of patient care
- More innovative solutions to problems
- Enhanced communication across departments
- Stronger organizational culture
Implementation Strategies for Participatory Management
Shared Governance Councils
Establishing formal structures where staff nurses participate in decision-making regarding clinical practice, quality improvement, professional development, and policy formation.
Unit-Based Committees
Creating unit-specific teams to address local issues, implement changes, and evaluate outcomes with the direct involvement of frontline staff.
Open Forum Discussions
Conducting regular meetings where all staff can voice concerns, suggest improvements, and participate in brainstorming solutions.
Participatory Problem-Solving
Using structured approaches like PDSA (Plan-Do-Study-Act) cycles with multidisciplinary teams to address operational challenges.
Challenges in Implementing Participatory Management
Common Barriers
- Traditional hierarchical culture
- Time constraints and staffing issues
- Resistance to change from both managers and staff
- Inadequate communication infrastructure
Mitigation Strategies
- Gradual implementation with pilot projects
- Comprehensive education on shared governance
- Recognition systems for participation
- Clear role definitions and expectations
Interprofessional Collaboration
Interprofessional collaboration in nursing refers to the practice where personnel from different healthcare disciplines work together with patients, families, and communities to deliver comprehensive, high-quality care.
Effective leadership in nursing management facilitates interprofessional collaboration by breaking down silos between disciplines and creating environments where diverse expertise is valued and integrated.
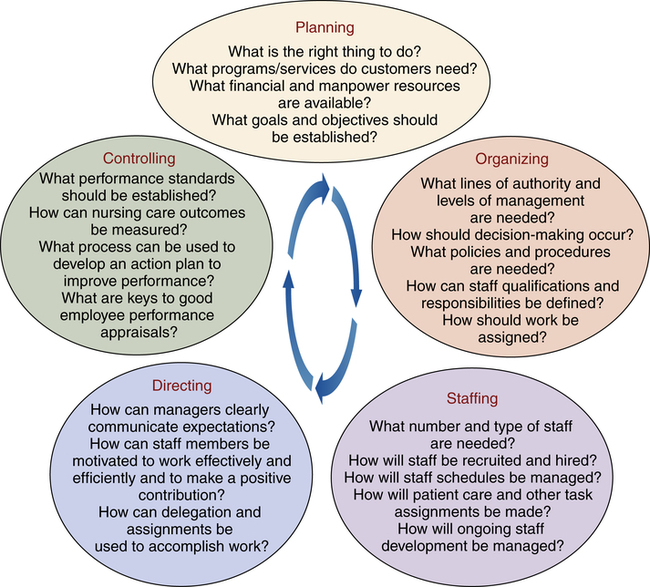
Figure 3: A model of interprofessional collaboration in healthcare settings
Core Components of Interprofessional Collaboration
Communication
Clear, respectful exchange of information using standardized formats and tools
Role Clarity
Understanding and respecting each discipline’s unique scope, expertise, and contributions
Shared Goals
Establishing common patient-centered objectives that integrate all disciplinary perspectives
Benefits of Interprofessional Collaboration
Patient Outcomes
- Reduced adverse drug reactions and medical errors
- Decreased hospital readmission rates
- Improved pain management and symptom control
- Enhanced patient satisfaction and experience
- More comprehensive care planning
Healthcare Provider Benefits
- Greater job satisfaction and reduced burnout
- Enhanced knowledge and skill development
- Improved understanding of other disciplines
- More efficient resource utilization
- Increased workplace safety and team cohesion
Nurse Leader’s Role in Facilitating Collaboration
Creating collaborative environments: Establishing physical and psychological spaces that encourage cross-disciplinary interaction
Modeling collaborative behaviors: Demonstrating respect, active listening, and valuing diverse perspectives
Resolving interprofessional conflicts: Mediating disagreements with a focus on patient-centered outcomes
Promoting shared decision-making: Implementing processes that incorporate input from all relevant disciplines
Supporting interprofessional education: Facilitating opportunities for cross-disciplinary learning and development
Helpful Mnemonics for Directing and Leading
These mnemonics will help nursing students remember key concepts related to directing and leading in nursing management.
DIRECT: Elements of Effective Directing
Delegation
Assigning appropriate tasks to qualified staff members based on their skills and experience
Instruction
Providing clear guidance and expectations for task completion and standards
Responsibility
Establishing accountability for actions and outcomes at all levels
Empowerment
Enabling staff to make decisions and take ownership of their work
Communication
Ensuring clear, two-way information exchange between all team members
Teamwork
Fostering collaboration and mutual support among nursing staff
LEADS: Nursing Leadership Principles
Listen
Active listening to understand staff concerns, ideas, and feedback
Empower
Providing autonomy and authority to make decisions at appropriate levels
Acknowledge
Recognizing achievements and providing constructive feedback
Develop
Investing in ongoing professional growth and skill enhancement
Support
Providing resources, guidance, and advocacy for staff needs
TEAMS: Interprofessional Collaboration Framework
Trust
Building mutual confidence in each team member’s competence and reliability
Expertise
Recognizing and utilizing each discipline’s unique knowledge and skills
Accountability
Taking responsibility for one’s role in patient outcomes and team performance
Mutual Respect
Valuing all team members’ contributions and perspectives
Shared Goals
Working together toward common patient-centered outcomes
Practical Applications
Applying the concepts of directing and leading in real nursing scenarios is essential for developing effective management skills. Here are practical examples and case studies:
Case Study: Implementing a New Care Protocol
Scenario: A nurse manager needs to implement a new evidence-based pressure ulcer prevention protocol in a busy medical-surgical unit.
Directing Approach:
- Clearly communicate the rationale and expected outcomes of the new protocol
- Provide comprehensive training through demonstrations and simulations
- Assign champions for each shift to guide implementation
- Supervise initial implementation with constructive feedback
- Monitor compliance and outcomes, adjusting the approach as needed
Participatory Elements:
- Involve staff in adapting the protocol to unit workflow
- Create a feedback mechanism for implementation challenges
- Establish interprofessional teams to evaluate effectiveness
- Celebrate successes and recognize contributions
Application: Leading Through Change
Effective Strategies
- Vision Communication: Clearly articulate the purpose and benefits of change
- Stakeholder Engagement: Involve key personnel in planning and implementation
- Resource Allocation: Ensure adequate support for transition activities
- Milestone Celebration: Acknowledge progress and early wins
Common Pitfalls
- Insufficient Communication: Creating uncertainty and resistance
- Overlooking Resistance: Failing to address underlying concerns
- Inadequate Training: Expecting proficiency without proper preparation
- Change Fatigue: Implementing too many initiatives simultaneously
Practical Tool: Leadership Style Assessment
Understanding your natural leadership style helps in developing a more flexible and effective approach to directing nursing teams.
| Leadership Style | Characteristics | Best Used When |
|---|---|---|
| Transformational | Inspirational, visionary, empowering | Major changes, innovation needed |
| Transactional | Clear expectations, reward-based | Standardized procedures, clear outputs |
| Democratic | Collaborative, inclusive decision-making | Complex issues, high staff expertise |
| Servant | Supportive, focuses on staff growth | Team development, high stress environments |
| Situational | Adaptable, context-specific | Mixed staff experience, varied tasks |
Reflection Questions: Consider which style you most naturally gravitate toward. When has this style been effective? When have you needed to adopt a different approach? How can you develop greater flexibility in your directing and leading techniques?
Summary
Key Concepts in Directing and Leading
- Directing is the managerial function of guiding, supervising, and motivating staff toward organizational goals
- Effective directing follows principles such as harmony of objectives, unity of command, and direct supervision
- The four key elements of directing are communication, leadership, motivation, and supervision
- Supervision and guidance ensure quality care through monitoring, coaching, and reflective practice
- Participatory management empowers nurses through involvement in decision-making and shared governance
- Interprofessional collaboration enhances patient outcomes through coordinated care across disciplines
Essential Skills for Nurse Leaders
- Clear, effective communication
- Delegation and task management
- Conflict resolution and mediation
- Team building and motivation
- Adaptable leadership styles
- Performance evaluation
- Change management
- Collaborative problem-solving
Practical Application Tips
- Assess your natural leadership style and develop flexibility
- Practice clear communication with standardized tools and techniques
- Build collaborative relationships across disciplines
- Implement shared decision-making in your unit or team
- Develop mentoring relationships to enhance supervisory skills
- Use reflective practice to continuously improve your directing approach
References
American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). ANA.
World Health Organization. (2010). Framework for action on interprofessional education and collaborative practice. WHO.
Nurseslabs. (2024). Nursing Management: Guide to Organizing, Staffing, Scheduling, Directing and Delegating. https://nurseslabs.com/nursing-management-guide-to-organizing-staffing-scheduling-directing-delegation/
Nurses Revision Uganda. (2023). Directing in Management. https://nursesrevisionuganda.com/directing-in-management/
Maryville University. (2023). Interprofessional Collaboration in Nursing: Examples and Benefits. https://nursing.maryville.edu/blog/interprofessional-collaboration-in-nursing.html
Journal of Nursing Administration. (2021). Participatory management effects on nurses’ organizational support and moral distress in pediatric nurses. https://pubmed.ncbi.nlm.nih.gov/37357944/
American Association of Colleges of Nursing. (2021). Domain 6: Interprofessional Partnerships. https://www.aacnnursing.org/essentials/tool-kit/domains-concepts/interprofessional-partnerships
Management by Objectives in Nursing Leadership
A Comprehensive Guide for Nursing Students
Table of Contents
1. Introduction to Management by Objectives
Management by Objectives (MBO) is a strategic management approach that emphasizes setting clear, specific objectives collaboratively and using these defined goals to guide and evaluate organizational performance. This systematic approach, pioneered by Peter Drucker in 1954, has become a cornerstone of modern management practices, including in healthcare settings.
Definition and Purpose
Management by Objectives is a dynamic system where managers and employees work together to identify common objectives, define individual responsibilities, and measure outcomes against these specific goals. In nursing management, MBO serves as both a planning and evaluation tool that aligns individual nursing staff goals with broader healthcare organizational objectives.
For nursing leaders, understanding and implementing MBO provides a structured framework for guiding teams, improving patient care outcomes, and developing staff competencies while ensuring alignment with hospital-wide strategic goals. This approach is particularly valuable in the complex, rapidly evolving healthcare environment where clear direction and measurable outcomes are essential.
The MBO Cycle in Nursing Management
1. Set Organizational Goals
Define hospital/unit objectives aligned with mission
2. Translate to Department Objectives
Nursing units define specific departmental objectives
3. Set Individual Staff Objectives
Nurses and leaders establish personal performance goals
4. Monitor Progress
Regular check-ins and performance tracking
5. Evaluate Performance
Measure achievements against established objectives
6. Provide Feedback & Reset
Review, recognize, and establish new objectives
2. Core Principles of MBO
Management by Objectives is built upon several foundational principles that guide its implementation. Understanding these core concepts is essential for nursing leaders seeking to effectively apply MBO in healthcare settings.
Specific, Measurable Objectives
All objectives should follow the SMART criteria: Specific, Measurable, Achievable, Relevant, and Time-bound. In nursing, this might translate to “Reduce patient falls by 25% in the next quarter” rather than “Improve patient safety.”
Participative Decision Making
MBO emphasizes collaborative goal-setting rather than top-down directives. Nursing staff should actively participate in defining their objectives, increasing buy-in and commitment.
Defined Time Period
Each set of objectives has a specific timeframe (quarterly, annually) with regular review periods for monitoring progress and making adjustments.
Performance Evaluation
Achievements are measured against pre-established objectives, creating a more objective evaluation system that focuses on outcomes rather than personalities.
MBO Principles Mnemonic: “SCOPE”
The SCOPE mnemonic provides an easy way to remember the essential elements that define effective Management by Objectives implementation. These principles create a structured framework for setting, monitoring, and achieving meaningful objectives in nursing management.
3. MBO in Nursing Practice
Implementing Management by Objectives in nursing environments requires adapting the general principles to address the unique challenges and requirements of healthcare settings. When properly applied, MBO can transform nursing departments by aligning individual performance with broader patient care objectives.
Adapting MBO for Healthcare
In nursing practice, objectives must balance quantitative metrics (patient satisfaction scores, infection rates) with qualitative aspects of care (compassion, patient education). This dual focus ensures that efficiency doesn’t come at the expense of quality patient care.
| Areas for Nursing MBO Implementation | Example Objectives | Measurement Methods |
|---|---|---|
| Patient Care Quality | Reduce pressure ulcer incidence by 15% within 6 months | Monthly prevalence studies, electronic health record data |
| Patient Satisfaction | Achieve HCAHPS nurse communication scores above 85th percentile | Patient satisfaction surveys, feedback forms |
| Staff Development | 100% of nursing staff to complete advanced certification within 18 months | Training records, certification tracking |
| Operational Efficiency | Reduce average patient discharge time by 30 minutes | Time studies, EHR timestamps |
| Safety Initiatives | Achieve 95% medication reconciliation completion within 24 hours of admission | Compliance audits, incident reports |
MBO Process in Nursing Units
-
Assessment: Conduct gap analysis of current performance vs. desired outcomes
-
Objective Setting: Collaborate with nursing staff to establish unit and individual objectives
-
Resource Allocation: Ensure staff have necessary tools and support to achieve objectives
-
Implementation: Integrate objectives into daily operations and workflows
-
Monitoring: Establish regular check-ins (daily huddles, weekly meetings) to track progress
-
Evaluation: Conduct formal reviews at predetermined intervals
-
Feedback & Adjustment: Provide constructive feedback and modify objectives as needed
4. Team Management Strategies
Effective team management is crucial for successful implementation of Management by Objectives in nursing settings. The collaborative nature of healthcare delivery requires nurse leaders to develop teams that can work cohesively toward shared objectives while maintaining individual accountability.
Team Formation Principles
- Skill Complementarity: Build nursing teams with diverse clinical specialties and experience levels to ensure comprehensive patient care coverage
- Workload Distribution: Assign responsibilities based on skills, experience, and availability to prevent burnout
- Role Clarity: Ensure each team member understands their specific responsibilities and how they contribute to team objectives
- Cross-Training: Develop versatile teams through education and rotation opportunities
Team Development Stages
Team Communication Framework
Effective communication is the foundation of successful team management in nursing. Implement the following structured communication approach to support objective achievement:
CLEAR Communication Model
Keep messages focused on relevant information
Relate discussions to team goals
Support points with data and best practices
Focus on solutions and next steps
Honor diverse perspectives and expertise
Implementing Team MBO
-
1.
Establish team-level objectives: Create shared goals that reflect unit priorities while supporting organizational direction
-
2.
Translate to individual contributions: Help each team member identify how their role supports team objectives
-
3.
Create accountability mechanisms: Implement tracking systems and regular check-ins to monitor progress
-
4.
Foster peer support: Encourage team members to assist each other in achieving individual and team objectives
-
5.
Celebrate achievements: Recognize both individual and collective progress toward objectives
5. Assignments and Rotations
Strategic staff assignments and rotation planning are critical components of Management by Objectives in nursing. Well-designed assignments ensure optimal patient care while supporting individual nurse development and unit objectives.
Assignment Principles
- Acuity-Based Staffing: Match nurse competency levels to patient care complexity, ensuring appropriate care delivery while supporting nurse development objectives
- Competency Alignment: Assign nurses to patient care situations that utilize their strengths while providing opportunities to develop in areas identified in their personal objectives
- Equitable Distribution: Ensure fairness in assignments while considering individual development goals and unit objectives
- Transparency: Communicate assignment rationale clearly to promote understanding and acceptance
Rotation Benefits
Strategic Rotation Planning Framework
| Rotation Type | Purpose | Duration | MBO Alignment |
|---|---|---|---|
| Clinical Cross-Training | Develop versatility across specialties | 2-4 weeks | Supports staff development and flexibility objectives |
| Leadership Shadow | Develop management skills | 1-2 weeks | Supports succession planning and leadership objectives |
| Specialty Immersion | Build expertise in a specific area | 4-12 weeks | Supports quality improvement and specialization objectives |
| Interdepartmental Exchange | Improve cross-departmental coordination | 1-2 weeks | Supports care continuity and collaboration objectives |
| Project-Based Assignment | Develop specific competencies | Variable | Supports innovation and quality improvement objectives |
Implementing MBO in Assignments
The following steps outline how to integrate MBO principles into nursing assignments and rotations:
-
1.
Map Unit Requirements: Identify patient care needs and required competencies
-
2.
Inventory Staff Skills: Document current competencies and development objectives
-
3.
Create Development Plans: Establish rotation schedules that support individual growth objectives
-
4.
Implement Assignment System: Create a transparent process that balances patient needs with staff development
-
5.
Evaluate Outcomes: Measure the impact of assignments on both patient care and staff development objectives
-
6.
Adjust and Refine: Modify the assignment approach based on evaluation findings
6. Maintenance of Discipline
Discipline in the context of nursing management refers to maintaining professional standards, adherence to policies, and fostering a culture of accountability. Within the Management by Objectives framework, discipline becomes a strategic element that supports the achievement of organizational and unit objectives.
Proactive Discipline Approach
Effective MBO implementation shifts the discipline paradigm from reactive punishment to proactive prevention through clear expectations aligned with measurable objectives. This approach emphasizes:
Explicit performance expectations tied to unit objectives
Ongoing communication about progress toward objectives
Resources to help staff meet performance expectations
Celebration of achievement and progress toward objectives
Discipline Framework Mnemonic: “ORDER”
Align discipline with performance goals
Maintain dignity in all interactions
Focus on growth not punishment
Apply consistently across team
Strengthen desired behaviors
Progressive Discipline in MBO Framework
When performance issues arise despite proactive measures, an MBO-aligned progressive discipline approach maintains focus on organizational objectives while supporting staff development:
| Stage | Approach | MBO Alignment |
|---|---|---|
| Verbal Coaching | Private discussion identifying gap between performance and expectations | Link performance issue to specific objectives and impact on team goals |
| Performance Improvement Plan | Documented plan with specific targets and timeline | Create measurable micro-objectives that support broader unit goals |
| Written Warning | Formal documentation of continued performance issues | Explicitly connect consequences of underperformance to unit objectives |
| Final Warning | Clear communication about employment jeopardy | Reassess fit between individual capabilities and position objectives |
| Termination/Reassignment | Separation or role change based on performance | Ensure alignment between staffing decisions and organizational objectives |
Best Practices for Discipline in MBO
Do’s
- Connect disciplinary discussions directly to relevant objectives
- Focus on behavioral patterns rather than isolated incidents
- Document performance discussions and agreements
- Involve HR early for guidance on complex issues
- Provide clear path to improvement with specific objectives
Don’ts
- Address performance issues in public settings
- Use vague language about expectations or objectives
- Delay addressing issues until they become severe
- Apply disciplinary measures inconsistently
- Focus exclusively on problems without offering solutions
7. Leadership in Nursing Management
Leadership is a critical component of successful MBO implementation in nursing settings. Effective nurse leaders create environments where teams can achieve their objectives while developing professionally and providing excellent patient care.
Leadership Styles in MBO
Transformational Leadership
Focus: Inspiring innovation and change to achieve ambitious objectives
MBO Application: Sets compelling vision and motivates staff to exceed basic objectives
Best for: Units undergoing significant change or improvement initiatives
Servant Leadership
Focus: Supporting team members’ growth and removing barriers to goal achievement
MBO Application: Provides resources and coaching to help staff meet objectives
Best for: Experienced teams with well-defined performance objectives
Situational Leadership
Focus: Adapting leadership approach based on team and situation needs
MBO Application: Varies support levels based on staff competency with specific objectives
Best for: Mixed-experience teams with diverse development needs
Core Leadership Competencies for MBO
LEADS Framework
Understand staff strengths, challenges, and aspirations to align individual and organizational objectives
Involve team members in setting objectives and developing action plans
Ensure individual and unit objectives support organizational priorities
Build team capacity through appropriate delegation and development opportunities
Provide ongoing feedback and resources to maintain momentum toward objectives
Leadership Responsibilities in MBO
| Phase | Leadership Actions | Skills Required |
|---|---|---|
| Objective Setting |
|
|
| Implementation |
|
|
| Monitoring |
|
|
| Evaluation |
|
|
Developing Leadership Capacity for MBO
Building leadership skills at all levels enhances MBO implementation through shared accountability for objectives:
Formal Leaders
- Advanced MBO training and certification
- Executive coaching for strategic alignment
- Change management education
Emerging Leaders
- Leadership shadowing opportunities
- Project leadership assignments
- Mentoring from senior leaders
All Staff
- Basic MBO principles education
- Goal-setting workshops
- Self-leadership development
8. Implementing MBO in Nursing Units
Successfully implementing Management by Objectives in nursing units requires a structured approach that considers healthcare’s unique challenges. This section outlines a practical implementation framework that nursing leaders can adapt to their specific contexts.
MBO Implementation Roadmap
Phase 1: Preparation
3-4 Weeks
- Assess unit readiness
- Train leadership team
- Align with organizational strategy
- Establish baseline metrics
Phase 2: Orientation
2-3 Weeks
- Educate all staff on MBO principles
- Clarify roles and expectations
- Introduce documentation tools
- Address questions and concerns
Phase 3: Goal Setting
2-4 Weeks
- Define unit-level objectives
- Facilitate team objectives development
- Support individual objectives creation
- Ensure alignment across levels
Phase 4: Implementation
Ongoing
- Launch tracking systems
- Begin regular review meetings
- Provide coaching and support
- Address barriers to goal achievement
Phase 5: Monitoring
Continual
- Conduct regular progress checks
- Document achievements and challenges
- Adjust objectives as needed
- Celebrate early wins
Phase 6: Evaluation
End of Cycle
- Assess achievement of all objectives
- Recognize accomplishments
- Analyze barriers and facilitators
- Prepare for next cycle
Critical Success Factors
Organizational Factors
- Executive Sponsorship: Visible support from senior leadership for MBO initiatives
- Resource Allocation: Dedicated time and tools for MBO implementation
- Integration: Alignment of MBO with existing systems (performance reviews, quality improvement)
- Recognition Systems: Formal acknowledgment of achievement toward objectives
Unit-Level Factors
- Leadership Competency: Nurse managers skilled in MBO principles and coaching
- Staff Engagement: Active participation in setting and tracking objectives
- Communication Systems: Regular forums to discuss progress toward objectives
- Data Accessibility: Easy access to metrics related to unit objectives
Implementation Mnemonic: “IMPACT”
Build infrastructure and support
Engage staff in the process
Set clear, aligned objectives
Execute with accountability
Monitor and provide feedback
Embed MBO into culture
9. Challenges and Solutions
Implementing Management by Objectives in nursing environments presents unique challenges. This section identifies common obstacles and provides practical strategies to overcome them, ensuring successful MBO implementation despite healthcare’s complexity.
| Challenge | Impact on MBO | Solution Strategies |
|---|---|---|
| High Workload Demands | Staff may view MBO as “one more thing” adding to already heavy workload |
|
| Rapidly Changing Environment | Established objectives may become irrelevant due to shifting priorities |
|
| Resistance to Measurement | Staff may fear judgment or punitive consequences from objective evaluation |
|
| Leadership Turnover | Changes in management can disrupt MBO continuity |
|
| Goal Displacement | Focus shifts to measured objectives at expense of unmeasured but important aspects |
|
| Data Limitations | Lack of timely, accessible metrics to track progress |
|
Overcoming Resistance to MBO
Resistance is natural when implementing new management approaches. Use these strategies to address specific concerns:
“This is just another management fad”
- Share evidence of MBO effectiveness in similar settings
- Connect MBO principles to existing successful practices
- Commit to long-term implementation with leadership stability
“We’re too busy for this”
- Demonstrate how MBO can streamline priorities and reduce wasted effort
- Start with just 2-3 high-impact objectives
- Provide administrative support for documentation and tracking
“Nursing care can’t be reduced to numbers”
- Include qualitative objectives that capture the art of nursing
- Involve nurses in defining meaningful measures
- Use patient stories alongside metrics to illustrate impact
“This will be used against us”
- Establish psychological safety through clear “learning not blaming” principles
- Focus initial evaluation on progress rather than absolute achievement
- Include contextual factors in all performance analyses
Adaptations for Different Nursing Contexts
Acute Care Settings
Focus on balancing efficiency objectives with quality metrics, using shorter review cycles to accommodate rapid patient turnover.
Long-Term Care
Emphasize resident-centered objectives with longer timeframes for progress evaluation, incorporating quality of life measures.
Ambulatory/Clinic Settings
Structure objectives around patient access, preventive care metrics, and chronic disease management outcomes.
Academic/Teaching Environments
Integrate educational objectives alongside clinical metrics, with specific attention to knowledge transfer and evidence-based practice.
10. Case Studies and Examples
Real-world applications of Management by Objectives in nursing settings demonstrate its practical value. These case studies provide concrete examples of successful MBO implementation across different healthcare contexts.
Reducing Patient Fall Rates
Initial Situation:
A 36-bed medical-surgical unit experienced fall rates exceeding the national benchmark by 25%, with significant staff turnover affecting consistent protocol implementation.
MBO Approach:
- Unit collaborative established SMART objective: “Reduce patient falls by 30% within 6 months”
- Team objectives developed for each shift to support main goal
- Individual nurse objectives included specific components (risk assessment, hourly rounding)
- Weekly data review with visual tracking board
- Monthly recognition for progress toward objectives
Outcomes:
- Fall rate reduced by 42% (exceeding objective) within 5 months
- Staff engagement scores improved by 15%
- Standardized processes implemented for risk assessment
- Approach expanded to other quality indicators
Key Lessons:
Staff ownership of objectives development led to higher engagement. Visual tracking tools supported sustained focus on goals.
Improving Patient Flow
Initial Situation:
Busy ED experiencing extended wait times and high left-without-being-seen rates. Staff frustration with process inefficiencies contributing to burnout.
MBO Approach:
- Primary objective: “Reduce door-to-provider time by 20% within 90 days”
- Cross-functional team established with representation from all roles
- Triage team established specific sub-objectives for initial assessment
- Treatment team focused on objectives for rapid cycle testing of new workflows
- Daily huddles reviewed real-time performance data
Outcomes:
- Door-to-provider time reduced by 35% (exceeding objective)
- Left-without-being-seen rate decreased from 7% to 2%
- Staff satisfaction improved as measured by pulse surveys
- New standard workflows developed and documented
Key Lessons:
Breaking complex flow challenges into discrete team-level objectives made the improvement manageable. Daily data review maintained momentum.
Developing Future Leaders
Initial Situation:
Regional health system struggled with nursing manager vacancies and extended time-to-fill for leadership positions. Limited internal pipeline for leadership roles.
MBO Approach:
- System-wide objective: “Develop internal candidates for 80% of nurse manager openings within 18 months”
- Each nursing director set objectives for identifying potential leaders
- Aspiring leaders received individual development objectives
- Structured mentorship program with progress tracking
- Quarterly leadership immersion experiences with specific competency objectives
Outcomes:
- Leadership candidate pool increased from 12 to 47 nurses
- 85% of manager positions filled internally within 15 months
- Time-to-fill for leadership positions decreased by 65%
- New leader retention at 95% after one year
- Sustainable leadership development program established
Key Lessons:
The cascading objectives approach (system to director to individual) created accountability at all levels. Measurable leadership development objectives transformed an abstract goal into concrete action steps.
By focusing development efforts on specific competencies with clear objectives, the program prepared candidates more effectively than traditional approaches.
Common Success Patterns
Analysis of successful MBO implementations in nursing reveals these recurring elements:
-
Staff Co-Creation:
Units where staff actively participated in setting objectives showed significantly higher goal achievement and engagement.
-
Visual Management:
Teams using visual displays of objectives and progress maintained better focus and momentum toward goals.
-
Regular Review Cadence:
Structured, consistent progress reviews (often daily or weekly) correlated with higher achievement rates.
-
Balanced Objective Sets:
Units that included both quality and efficiency objectives avoided unintended consequences and achieved more sustainable outcomes.
-
Celebration of Progress:
Formal recognition of milestone achievement reinforced the value of the MBO approach and maintained motivation.
11. Conclusion
Management by Objectives offers a structured, collaborative approach to nursing leadership that aligns individual efforts with organizational goals. When implemented thoughtfully, MBO can transform nursing units by creating clarity of purpose, measurable outcomes, and shared accountability for results.
Key Takeaways
- Strategic Alignment: MBO creates a direct line of sight from organizational vision to daily nursing activities through cascading objectives.
- Collaborative Engagement: The participative nature of MBO increases nurse buy-in and commitment to achieving outcomes.
- Performance Clarity: SMART objectives provide clear expectations and measurement criteria for evaluation.
- Development Focus: MBO integrates professional development with operational performance through personalized objectives.
- Adaptable Framework: The MBO approach can be tailored to various nursing contexts while maintaining core principles.
Implementation Journey
Implementing MBO in nursing is best viewed as a progressive journey rather than a destination:
Focus on building understanding, establishing basic processes, and creating early wins through team objectives.
Expand to individual objectives, refine measurement systems, and connect MBO to other organizational processes.
Create advanced alignment across departments, develop predictive capabilities, and build systems for continuous improvement of objectives.
MBO becomes embedded in organizational culture, driving innovation and adaptability through shared objectives and collaborative achievement.
Future Directions
As healthcare continues to evolve, MBO in nursing will likely develop in these directions:
Technology Integration
Mobile apps and dashboards will make tracking objectives more accessible and dynamic, enabling real-time adjustments and feedback.
Patient-Centered Objectives
Greater involvement of patients in setting care objectives, creating truly collaborative goal establishment across the care continuum.
Predictive Analytics
Advanced data analysis will help nursing leaders set more precise objectives based on trend analysis and predictive modeling.
Final Reflection
Management by Objectives provides nursing leaders with a powerful framework for achieving excellence in patient care while developing staff potential. The collaborative nature of MBO aligns perfectly with nursing’s professional values of teamwork, evidence-based practice, and continuous improvement.
When implemented with attention to healthcare’s unique challenges and opportunities, MBO can transform nursing units into high-performing teams that consistently achieve or exceed their objectives. The key to success lies in maintaining the balance between measurable outcomes and the compassionate, patient-centered care that defines the nursing profession.
By mastering MBO principles and adapting them to your specific nursing context, you can create an environment where clear direction, meaningful feedback, and shared purpose drive exceptional results for patients, staff, and the organization.
