Critical Path Analysis in Nursing Management
Comprehensive guide for nursing students and healthcare professionals
Table of Contents
- Introduction to Critical Path Analysis
- Key Concepts and Terminology
- Step-by-Step Guide to Critical Path Analysis
- Critical Path Calculation Techniques
- Float Calculation and Its Significance
- Applications in Healthcare and Nursing
- Case Studies and Examples
- Mnemonics for Critical Path Analysis
- Summary and Key Takeaways
- References
Introduction to Critical Path Analysis
Critical Path Analysis (CPA), also known as the Critical Path Method (CPM), is a powerful project management technique used to plan, schedule, and control complex projects. In nursing and healthcare settings, the critical pathway approach helps coordinate care delivery, optimize resource allocation, and improve patient outcomes.
The concept of critical pathway was first developed in the 1950s by the DuPont company and later refined by other organizations. Today, it has become an essential tool in healthcare management, allowing nursing professionals to visualize project timelines, identify dependencies between tasks, and determine the minimum time required to complete a project.
Why Critical Path Analysis Matters in Nursing
- Helps in efficiently planning and managing nursing workflows
- Improves resource allocation and staff scheduling
- Identifies potential bottlenecks in care delivery pathways
- Enhances patient care by optimizing treatment protocols
- Supports evidence-based practice through systematic planning
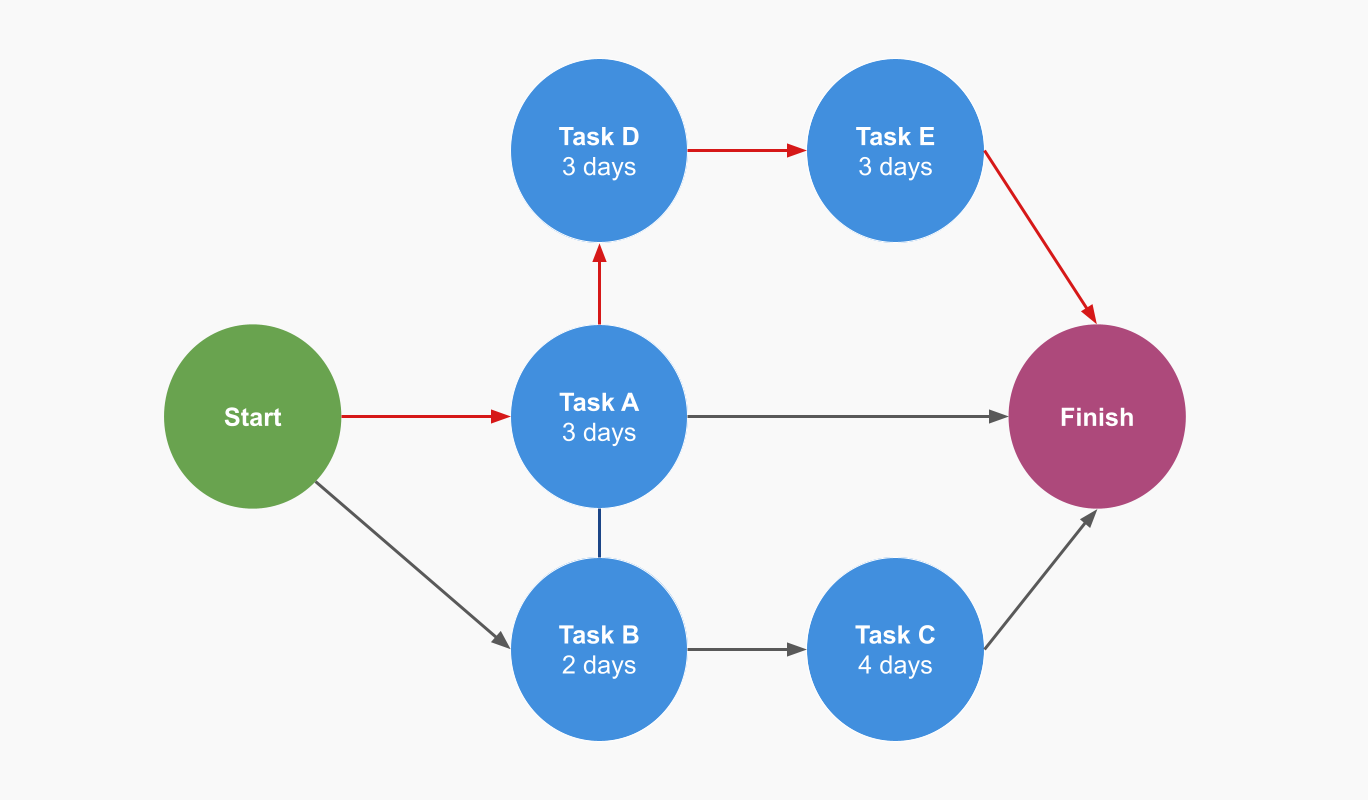
Figure 1: Visual representation of a critical path in project management
Key Concepts and Terminology
Understanding the fundamental concepts of Critical Path Analysis is essential for effectively implementing this technique in nursing management. Let’s explore the key terminology that forms the foundation of critical pathway analysis.
Critical Path
The sequence of dependent tasks that determines the minimum time needed to complete the entire project. This pathway cannot be delayed without delaying the overall project.
Activity
A specific task that consumes time and resources. In healthcare, activities might include patient assessment, medication administration, or discharge planning.
Dependencies
Relationships between activities that determine their sequence. For example, medication administration (dependent activity) cannot start before physician’s order (predecessor activity).
Float (or Slack)
The amount of time an activity can be delayed without affecting the overall project duration. Activities on the critical pathway have zero float.
Network Diagram
A graphical representation of project activities and their dependencies, showing the flow of work through the project timeline.
Duration
The estimated time required to complete an activity. In healthcare, durations may vary based on patient condition and available resources.
| Term | Definition | Nursing Example |
|---|---|---|
| Earliest Start Time (ES) | The earliest time an activity can begin, based on the completion of predecessor activities | Blood draw can start at 7:00 AM after patient admission |
| Earliest Finish Time (EF) | The earliest time an activity can be completed (ES + Duration) | Blood draw completes at 7:15 AM (ES 7:00 + 15 minutes) |
| Latest Start Time (LS) | The latest time an activity can begin without delaying the project | Blood draw must start by 7:30 AM to avoid delaying lab results |
| Latest Finish Time (LF) | The latest time an activity can be completed without delaying the project | Blood draw must complete by 7:45 AM |
| Total Float | The amount of time an activity can be delayed without affecting the project completion time (LS – ES or LF – EF) | Blood draw has 30 minutes float if it can be done anytime between 7:00-7:30 AM |
| Free Float | The amount of time an activity can be delayed without affecting the early start of successor activities | 15 minutes free float if delaying blood draw doesn’t delay medication administration |
Important Distinction
In healthcare, the term “Critical Pathway” sometimes refers to standardized care plans or clinical pathways. While related, this is different from the project management concept of Critical Path Analysis. Clinical pathways focus on standardizing care processes, while Critical Path Analysis is a project management technique for planning and scheduling.
Step-by-Step Guide to Critical Path Analysis
Implementing Critical Path Analysis in nursing management involves a systematic approach. Follow these steps to effectively analyze and optimize your healthcare projects and workflows.
Step 1: Define the Project Scope and Objectives
Clearly define what needs to be accomplished and the desired outcomes. In nursing, this might involve:
- Implementing a new nursing protocol
- Improving patient discharge process
- Reorganizing a clinical unit workflow
Example: Reducing average Emergency Department (ED) wait times from 4 hours to 2.5 hours.
Step 2: Identify All Required Activities
Break down the project into specific tasks or activities that need to be completed. Be comprehensive but avoid excessive detail.
Example for ED Improvement:
- Patient registration
- Initial triage assessment
- Physician evaluation
- Diagnostic testing (labs, imaging)
- Treatment administration
- Discharge or admission process
Step 3: Determine Activity Sequence and Dependencies
Establish the logical relationships between activities. Identify which tasks must be completed before others can begin.
Types of Dependencies in Healthcare:
- Finish-to-Start (FS): Lab results must be received before treatment decisions (most common)
- Start-to-Start (SS): Patient education can begin once medication administration starts
- Finish-to-Finish (FF): Documentation must be completed before shift handover is complete
- Start-to-Finish (SF): New nurse shift must start before previous nurse can finish (rare)
Step 4: Estimate Activity Durations
Assign realistic time estimates to each activity. In healthcare, consider:
- Historical data from similar activities
- Standard operating procedures
- Staff expertise and availability
- Patient acuity and variability
Example: Triage assessment – 10 minutes, Lab collection – 5 minutes, Lab processing – 30 minutes
Step 5: Create the Network Diagram
Draw a diagram that visually represents all activities and their relationships. Two common formats are:
- Activity-on-Node (AON): Activities are represented as nodes (boxes) connected by arrows showing dependencies
- Activity-on-Arrow (AOA): Activities are represented as arrows between nodes (less common today)
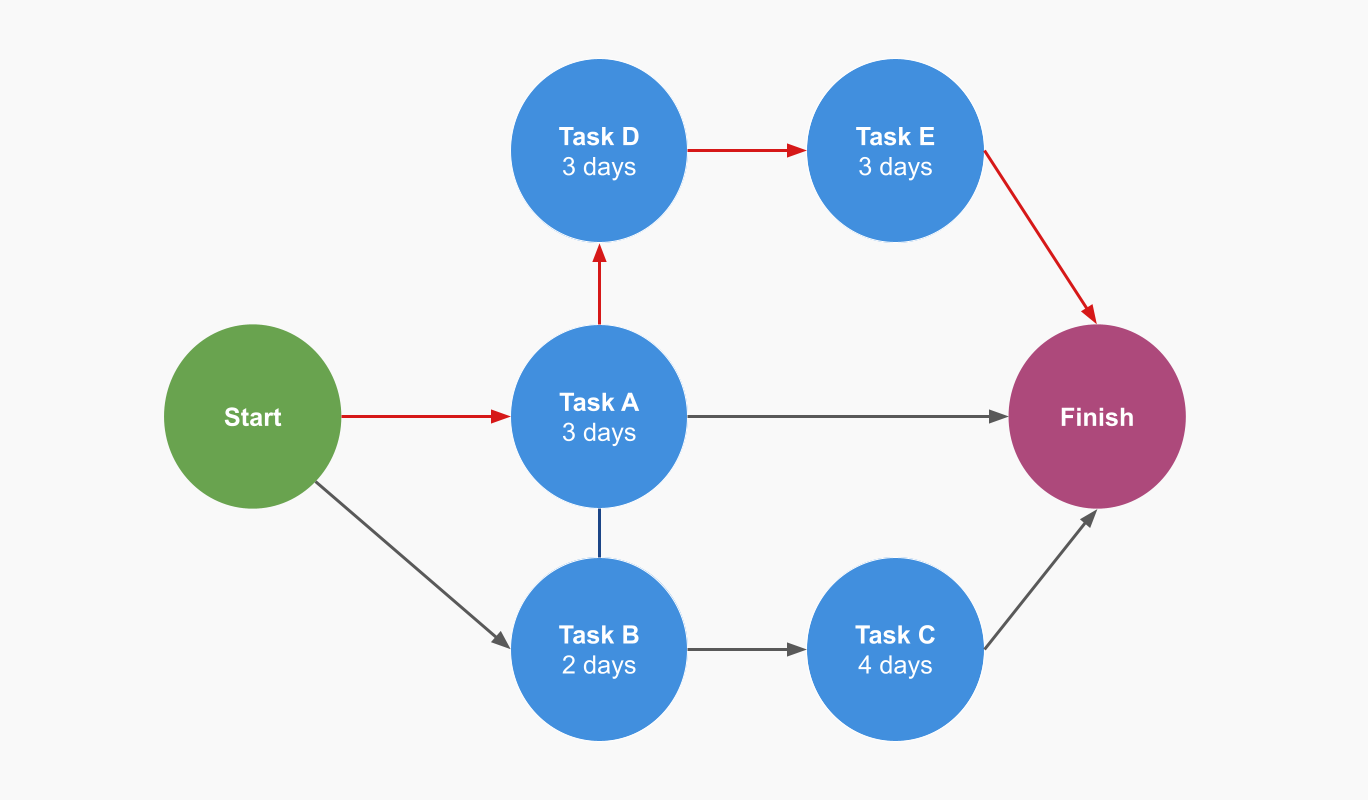
Figure 2: Activity-on-Node network diagram example
Step 6: Perform Critical Path Calculations
Calculate the earliest and latest start and finish times for each activity through forward and backward pass calculations.
This step identifies the critical pathway and determines float for each activity.
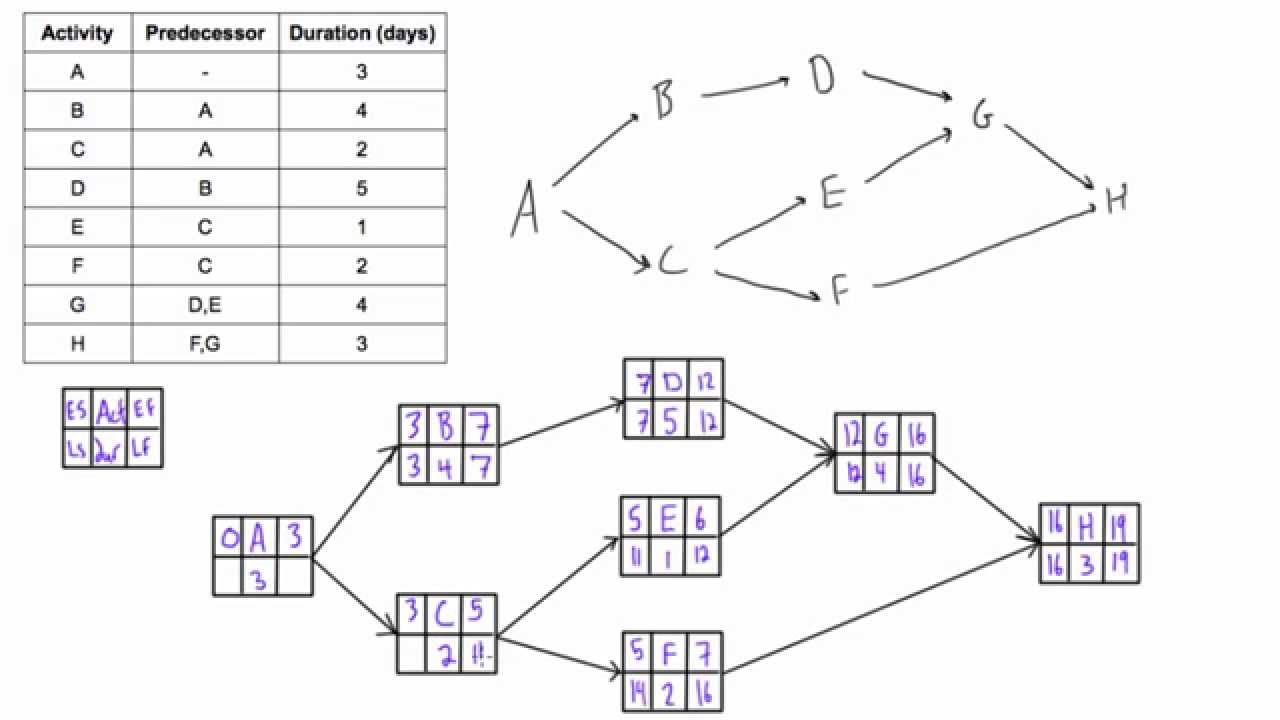
Figure 3: Forward and backward pass calculation example
Step 7: Identify the Critical Path
The critical pathway is the sequence of activities with zero float. Any delay in these activities will delay the entire project.
Healthcare Example: In the ED workflow, the critical pathway might include registration → triage → physician assessment → diagnostic testing → treatment → discharge planning.
Step 8: Analyze and Optimize
Examine the critical pathway and identify opportunities for improvement:
- Can any critical activities be shortened?
- Can any activities be performed in parallel?
- Are there resource constraints that could be addressed?
- Which activities have the most impact on total project duration?
Step 9: Implement and Monitor
Execute the project according to the plan and continuously track progress. In healthcare settings:
- Monitor actual vs. planned durations
- Address delays promptly, especially on the critical pathway
- Document lessons learned for future improvement
- Adjust the plan as needed based on real-world implementation
Critical Path Calculation Techniques
Calculating the critical pathway requires systematic forward and backward pass calculations. These calculations help determine the earliest and latest start and finish times for each activity, ultimately revealing which activities form the critical pathway.
Forward Pass Calculation
The forward pass moves from the start to the end of the project, calculating the earliest possible times each activity can start and finish.
Forward Pass Formulas:
- Earliest Start (ES) = Latest ES of all predecessor activities
- Earliest Finish (EF) = ES + Duration
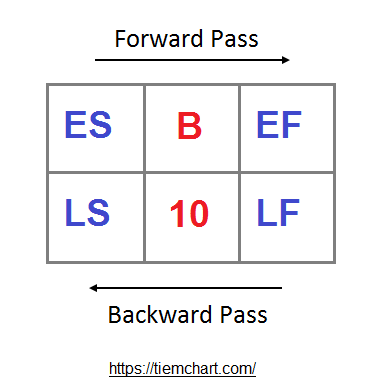
Figure 4: Forward pass calculation example
Forward Pass Example:
Consider a patient discharge process with the following activities:
- Activity A: Physician discharge order (Duration: 15 min)
- Activity B: Nurse discharge education (Duration: 30 min, depends on A)
- Activity C: Medication reconciliation (Duration: 20 min, depends on A)
- Activity D: Final paperwork (Duration: 15 min, depends on B and C)
Calculations:
- Activity A: ES = 0, EF = 0 + 15 = 15
- Activity B: ES = 15 (after A), EF = 15 + 30 = 45
- Activity C: ES = 15 (after A), EF = 15 + 20 = 35
- Activity D: ES = 45 (max of B and C’s EF), EF = 45 + 15 = 60
Backward Pass Calculation
The backward pass works in reverse, from the project end to the beginning, determining the latest possible start and finish times without delaying the project.
Backward Pass Formulas:
- Latest Finish (LF) = Earliest LS of all successor activities
- Latest Start (LS) = LF – Duration
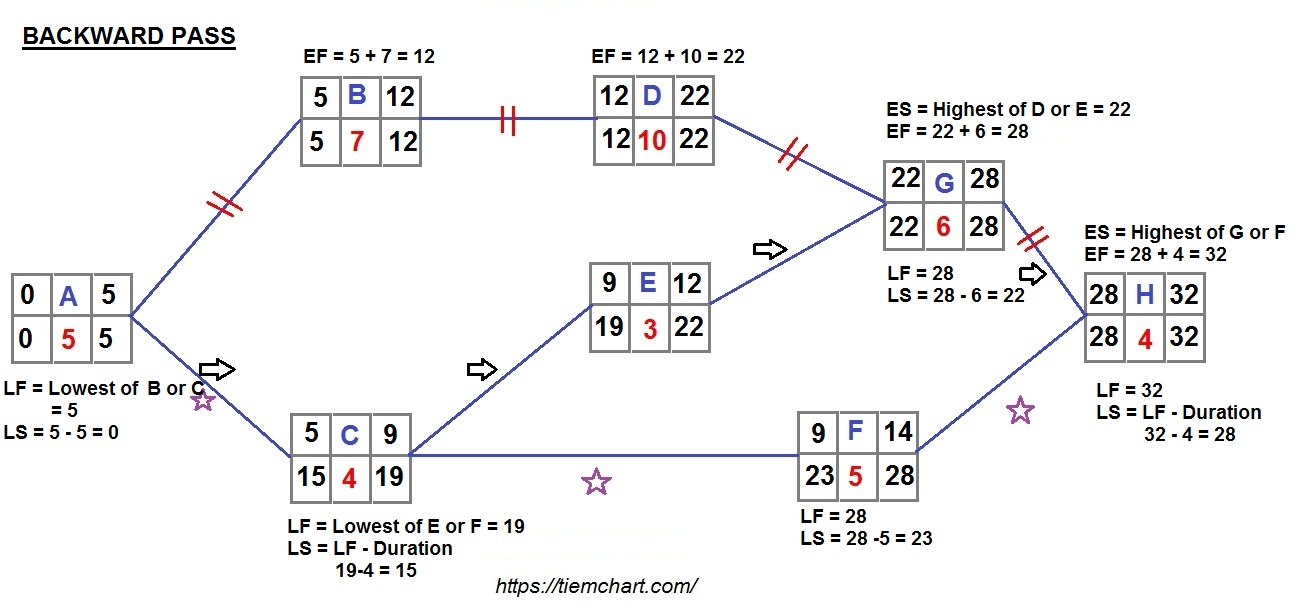
Figure 5: Backward pass calculation example
Backward Pass Example:
Continuing with our patient discharge example:
- Activity D: LF = 60 (project end), LS = 60 – 15 = 45
- Activity C: LF = 45 (D must start by 45), LS = 45 – 20 = 25
- Activity B: LF = 45 (D must start by 45), LS = 45 – 30 = 15
- Activity A: LF = 15 (earliest of B and C’s LS), LS = 15 – 15 = 0
Identifying the Critical Path
After completing both forward and backward passes, calculate the float for each activity. Activities with zero float form the critical pathway.
Float Calculation:
Total Float = LS – ES (or LF – EF)
Critical Path Identification Example:
Calculating float for our patient discharge activities:
- Activity A: Float = 0 – 0 = 0 (critical)
- Activity B: Float = 15 – 15 = 0 (critical)
- Activity C: Float = 25 – 15 = 10 (not critical)
- Activity D: Float = 45 – 45 = 0 (critical)
Therefore, the critical pathway is A → B → D (activities with zero float).
Float Calculation and Its Significance
Float (or slack) is a crucial concept in Critical Path Analysis that indicates the flexibility available for scheduling activities. Understanding different types of float helps nursing managers optimize resource allocation and handle unexpected delays.
Total Float
The maximum amount of time an activity can be delayed without delaying the overall project completion.
Formula: Total Float = LS – ES or LF – EF
Nursing Example: If a patient education session can start anytime between 10:00 AM and 11:30 AM without delaying discharge, it has 90 minutes of total float.
Free Float
The amount of time an activity can be delayed without delaying the early start of any successor activity.
Formula: Free Float = (Earliest ES of successors) – EF
Nursing Example: If delaying medication reconciliation won’t delay the start of discharge paperwork, it has free float.
Strategic Importance of Float in Healthcare
Understanding float has several practical applications in nursing and healthcare management:
- Resource Allocation: Assign staff to critical pathway activities first, then utilize float time to optimize staffing for non-critical activities
- Risk Management: Activities with minimal float require closer monitoring as delays will impact the entire project
- Schedule Flexibility: Activities with substantial float can be rescheduled to accommodate emergencies or unexpected situations
- Process Improvement: Analyzing patterns of float can identify areas of inefficiency in clinical pathways
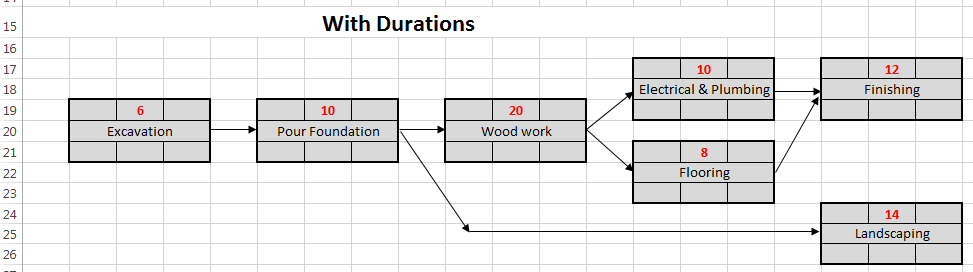
Figure 6: Network diagram showing activity durations and dependencies for float calculation
| Activity | Duration | ES | EF | LS | LF | Total Float | On Critical Path? |
|---|---|---|---|---|---|---|---|
| Patient Assessment | 30 min | 0 | 30 | 0 | 30 | 0 | Yes |
| Order Labs | 10 min | 30 | 40 | 30 | 40 | 0 | Yes |
| Obtain Medication History | 20 min | 30 | 50 | 50 | 70 | 20 | No |
| Lab Processing | 45 min | 40 | 85 | 40 | 85 | 0 | Yes |
| Physician Review | 15 min | 85 | 100 | 85 | 100 | 0 | Yes |
| Treatment Administration | 30 min | 100 | 130 | 100 | 130 | 0 | Yes |
Common Misconceptions About Float
- Misconception: Activities with float can be delayed indefinitely.
Reality: Delays beyond the available float will impact the project timeline. - Misconception: Float is static throughout the project.
Reality: Float changes as the project progresses and activities are completed earlier or later than planned. - Misconception: Float only matters for non-critical activities.
Reality: Monitoring consumed float helps predict if non-critical activities might become critical.
Applications in Healthcare and Nursing
Critical Path Analysis has numerous applications in healthcare settings, helping to optimize workflows, improve patient outcomes, and enhance resource utilization. Let’s explore how this technique can be applied in nursing practice and healthcare management.
Clinical Pathway Development
Using CPA to create standardized care pathways for common conditions like pneumonia, myocardial infarction, or post-operative care, ensuring evidence-based interventions occur at optimal times.
Discharge Planning
Streamlining the discharge process by identifying critical activities and dependencies, reducing delays and improving patient satisfaction.
Department Workflow Optimization
Analyzing and improving workflows in emergency departments, operating rooms, or outpatient clinics to reduce wait times and increase throughput.
Staff Scheduling
Using CPA to determine optimal staffing patterns based on critical pathway activities and peak workload periods in various clinical areas.
Quality Improvement Projects
Planning and managing quality improvement initiatives such as reducing healthcare-associated infections or implementing new safety protocols.
Health IT Implementation
Managing the implementation of new electronic health records systems or clinical decision support tools with minimal disruption to patient care.
Figure 7: Example of clinical pathway mapping in healthcare
Benefits of Critical Path Analysis in Healthcare
- Improved Resource Utilization: Identifying critical pathways helps allocate staff, equipment, and supplies more effectively
- Reduced Length of Stay: Streamlined care pathways minimize unnecessary delays
- Enhanced Care Coordination: Clear visual representation of care processes improves interdisciplinary communication
- Data-Driven Decision Making: Analyzing actual vs. planned durations provides insights for continuous improvement
- Standardization of Care: Critical pathways promote evidence-based practices and reduce unwarranted variation
- Risk Mitigation: Identifying critical activities helps focus risk management efforts
Real-World Application: Emergency Department Throughput
An emergency department applied Critical Path Analysis to reduce patient length of stay. They identified the following critical pathway:
- Patient arrival/registration (5 min)
- Initial nurse triage (10 min)
- Physician assessment (15 min)
- Laboratory testing (45 min)
- Physician decision-making (10 min)
- Treatment administration (variable)
- Discharge process (15 min)
By analyzing this pathway, they identified that laboratory testing was the biggest bottleneck. Interventions implemented:
- Point-of-care testing for common labs
- Dedicated phlebotomist during peak hours
- Standardized order sets for common presentations
Result: Average ED length of stay decreased from 240 minutes to 180 minutes, improving patient satisfaction and department capacity.
Case Studies and Examples
Let’s examine practical examples of Critical Path Analysis applied in various healthcare scenarios to better understand its real-world application and benefits.
Case Study 1: Surgical Pathway Optimization
Background:
A surgical department was experiencing delays and inefficiencies in their perioperative process, leading to case cancellations and staff overtime.
Application of Critical Path Analysis:
- Mapped the entire perioperative process from pre-admission testing to PACU discharge
- Identified key activities and dependencies
- Estimated realistic durations for each activity
- Created a network diagram and calculated the critical pathway
- Analyzed float for non-critical activities
Findings:
The critical pathway included patient arrival, anesthesia preparation, surgical procedure, and immediate recovery. The analysis revealed that operating room turnover time and delayed starts were the most significant constraints on the critical pathway.
Interventions:
- Implemented parallel processing for room turnover activities
- Created standardized setup protocols for common procedures
- Rescheduled pre-operative activities with large float to off-peak times
- Added a dedicated nurse coordinator to monitor critical pathway activities
Results:
- Average turnover time reduced from 45 to 25 minutes
- On-time start rate improved from 60% to 85%
- Surgical case volume increased by 12% without adding staff
- Staff overtime decreased by 20%
Case Study 2: Stroke Care Pathway
Background:
A hospital’s stroke team wanted to improve their door-to-treatment time for ischemic stroke patients eligible for thrombolytic therapy (tPA), where the national standard is 60 minutes.
Application of Critical Path Analysis:
- Documented all steps in the acute stroke pathway from ED arrival to tPA administration
- Collected data on actual time spent on each activity
- Created a network diagram showing dependencies
- Calculated the critical pathway and identified bottlenecks
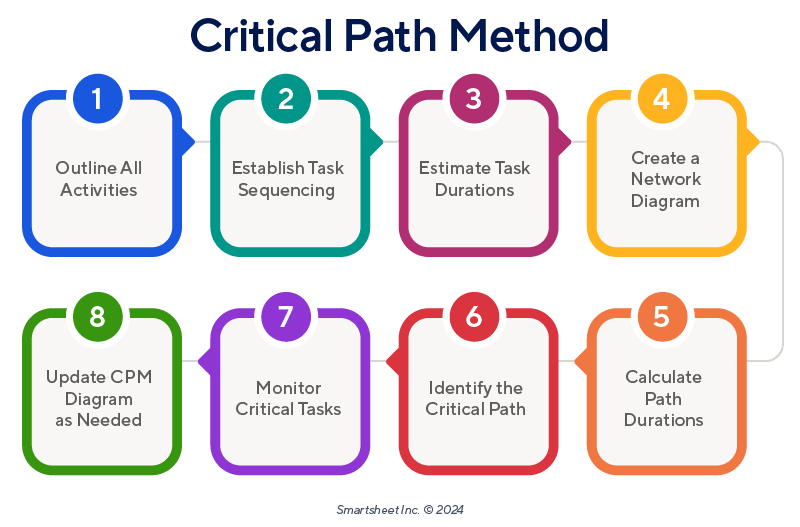
Figure 8: General critical path analysis steps that were applied to the stroke care pathway
Findings:
The critical pathway included triage, CT scan, radiologist interpretation, and neurologist decision. The CT scan and its interpretation were identified as the primary bottlenecks.
Interventions:
- Implemented a “stroke alert” protocol that prioritized CT scans for suspected stroke patients
- Established telemedicine connections for remote radiologist consultation
- Relocated the tPA medication to the ED (previously stored in pharmacy)
- Created parallel workflows for lab testing and clinical assessment
Results:
- Average door-to-needle time reduced from 75 minutes to 45 minutes
- Percentage of eligible patients receiving tPA increased from 60% to 88%
- Patient outcomes improved with earlier treatment
Case Study 3: Nursing Shift Handover Process
Background:
A medical unit was experiencing lengthy shift handover processes that frequently extended 30-45 minutes beyond scheduled shift times, resulting in overtime costs and staff dissatisfaction.
Application of Critical Path Analysis:
- Mapped all activities involved in the handover process
- Identified dependencies between activities
- Estimated time required for each component
- Constructed a network diagram and determined the critical pathway
Findings:
The critical pathway included chart review, preparation of handover notes, and face-to-face reporting. Non-critical activities with significant float included certain documentation tasks and room inspections.
Interventions:
- Implemented a standardized SBAR (Situation, Background, Assessment, Recommendation) handover template
- Moved non-critical documentation to earlier in the shift
- Introduced bedside handover to combine patient assessment and reporting
- Staggered arrival times for oncoming shift to reduce waiting
Results:
- Average handover time reduced from 45 minutes to 25 minutes
- Overtime costs decreased by 35%
- Staff satisfaction scores regarding handover process improved by 40%
- Patient satisfaction increased due to improved continuity of care
Mnemonics for Critical Path Analysis
Memorizing key concepts in Critical Path Analysis can be challenging. These mnemonics will help nursing students remember important aspects of the methodology.
P-A-T-H-S
Steps to Create a Critical Pathway
- P Plan – Define project scope and objectives
- A Activities – Identify all required tasks
- T Times & Dependencies – Estimate durations and establish relationships
- H Highlight – Create network diagram and calculate critical path
- S Shorten & Schedule – Optimize and implement the plan
C-R-I-T-I-C-A-L
Key Elements of Critical Path Analysis
- C Calculation – Forward and backward pass
- R Relationships – Task dependencies
- I Identification – Finding zero float activities
- T Time – Duration estimation and management
- I Integration – Connecting all activities
- C Constraints – Resource and time limitations
- A Analysis – Examining for improvement opportunities
- L Logic – Systematic and sequential reasoning
F-L-O-A-T
Understanding Float Concepts
- F Flexibility – Amount of scheduling leeway
- L Latest minus Earliest – Calculation method (LS-ES)
- O Optimization – Use float for resource leveling
- A Absent in critical path activities (zero float)
- T Types – Total, Free, and Independent Float
N-U-R-S-E
Applying Critical Path in Nursing
- N Network all care activities and dependencies
- U Understand critical vs. non-critical activities
- R Resource allocation based on critical pathway
- S Streamline workflows by optimizing the pathway
- E Evaluate outcomes and adjust as needed
Summary and Key Takeaways
Critical Path Analysis is a powerful tool for nursing management that helps optimize workflows, allocate resources efficiently, and improve patient care. By identifying the sequence of activities that determine the minimum project duration, nurses and healthcare managers can focus their attention on the most crucial aspects of care delivery.
Key Takeaways:
- Critical Path Analysis helps identify the sequence of activities that directly affects overall project duration.
- The critical pathway consists of activities with zero float that cannot be delayed without delaying the entire project.
- Forward pass calculation determines the earliest start and finish times, while backward pass determines the latest start and finish times.
- Understanding float allows for strategic resource allocation and flexibility in scheduling non-critical activities.
- In healthcare, CPA can be applied to clinical pathways, department workflows, quality improvement initiatives, and more.
- Effective implementation requires clear identification of activities, accurate duration estimates, and proper analysis of dependencies.
- Regular monitoring and adjustment of the critical pathway is essential as the project progresses.
Implementation Tips for Nursing Practice
- Start Small: Begin with a well-defined process like medication administration or discharge planning before tackling more complex workflows.
- Involve Stakeholders: Include representatives from all disciplines involved in the process for comprehensive activity identification.
- Collect Data: Use real-time data to validate duration estimates and identify areas for improvement.
- Use Visual Tools: Leverage software or visual aids to create and communicate the critical pathway.
- Continually Reassess: Healthcare environments are dynamic; regularly review and update your critical pathway analysis.
- Focus on Patient-Centered Outcomes: Ensure that pathway optimizations improve patient care, not just operational metrics.
References
- AHRQ. (2023). Critical Path Method – Digital Healthcare Research. https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit/all-workflow-tools/critical-path-method
- Panchbhai, T. (2020). Application of critical path analysis in clinical trials. Perspectives in Clinical Research, 7(1), 26-31. https://pmc.ncbi.nlm.nih.gov/articles/PMC4759980/
- Coffey, R. J., Richards, J. S., Remmert, C. S., LeRoy, S. S., Schoville, R. R., & Baldwin, P. J. (2005). An introduction to critical paths. Quality Management in Healthcare, 14(1), 46-55. https://journals.lww.com/qmhcjournal/fulltext/2005/01000/an_introduction_to_critical_paths.5.aspx
- Workamajig. (2023). How to Use Critical Path Method for Complete Beginners. https://www.workamajig.com/blog/critical-path-method
- Smartsheet. (2023). Beginner’s Guide to Critical Path Method. https://www.smartsheet.com/critical-path-method
- Wrike. (2023). The Critical Path Method in Project Management: A Full Guide. https://www.wrike.com/blog/critical-path-is-easy-as-123/
- Asana. (2023). Critical path method: How to use CPM for project management. https://asana.com/resources/critical-path-method
- ProjectEngineer. (2023). How to Calculate Total Float. https://www.projectengineer.net/how-to-calculate-total-float/
- Pearce, C. (2016). Critical path planning for discharging older adults using a functional dependency and risk prediction model. Healthcare Financial Management Journal, 11(3), 151-162.
- Coffey, R. J., Richards, J. S., Remmert, C. S., LeRoy, S. S., Schoville, R. R., & Baldwin, P. J. (1992). An Introduction to Critical Paths. Quality Management in Health Care, 1(1), 45-54.
