Planning and Organizing in Nursing Education
Comprehensive guide to effective planning strategies in nursing education
Table of Contents
Introduction to Planning in Nursing Education
Effective planning is the cornerstone of successful nursing education programs. It provides structure, direction, and purpose to educational activities, ensuring that nursing students receive comprehensive training that meets professional standards.
Why is Planning Important in Nursing Education?
Well-executed planning ensures that nursing programs effectively develop competent professionals who can deliver high-quality patient care. It creates a roadmap for achieving educational objectives while optimizing resources and time.
This comprehensive guide explores various aspects of planning and organizing in nursing education, from philosophical foundations to practical implementation strategies. We’ll examine how institutions develop and execute plans that support student learning and professional development in the dynamic healthcare environment.
Note: Throughout nursing education, planning occurs at multiple levels—institutional, programmatic, and instructional—all working together to create cohesive educational experiences.
Philosophy, Objectives, and Mission of Nursing Colleges
A nursing college’s philosophy, objectives, and mission form the foundation of all educational planning activities. These elements articulate the institution’s core values, educational approach, and desired outcomes.
Nursing Education Philosophy
The philosophy of nursing education reflects faculty beliefs about:
- The nature of nursing and nursing education
- People and their environment
- Health and healthcare delivery
- Teaching and learning processes
- Professional development

Fig 1: A visual representation of nursing education philosophy components
Philosophy of Nursing Education
A nursing education philosophy is a statement that articulates the program’s beliefs about nursing, education, and how students develop into professional nurses. It guides curriculum development, teaching methodologies, and evaluation strategies.
Objectives in Nursing Education
Educational objectives are specific, measurable statements that describe what students should know and be able to do upon program completion. They flow directly from the program’s philosophy and mission.
Types of Educational Objectives
- Terminal objectives: Broad statements describing expected competencies at graduation
- Level objectives: Expectations for students at each academic level
- Course objectives: Specific learning outcomes for individual courses
- Unit objectives: Goals for specific content areas within courses
Mnemonic: “SMART” Objectives in Nursing Education
- Specific – Clearly define what students will learn
- Measurable – Can be assessed through evaluation methods
- Achievable – Realistic given program resources and time
- Relevant – Connected to nursing practice needs
- Time-bound – Accomplished within a defined timeframe
Mission of Nursing Colleges
The mission statement articulates the institution’s purpose, scope, and aspirations. It serves as a guiding framework for all program planning and decision-making.
Key Components of a Nursing College Mission
- Educational focus (teaching, research, service)
- Target student population and geographic scope
- Commitment to professional standards and ethics
- Emphasis on innovation and evidence-based practice
- Connection to healthcare community needs
“The mission, philosophy, and objectives of nursing education programs establish the foundation upon which all curricular planning and implementation decisions are built.”
Effective planning in nursing education begins with aligning these philosophical elements into a cohesive framework that guides all educational activities. When properly developed, these elements provide consistency and direction for faculty and students while ensuring that the program meets the needs of the healthcare community it serves.
Organization Structure of School/College
The organizational structure of a nursing school/college creates the framework within which educational planning occurs. A well-designed structure clarifies roles, responsibilities, and reporting relationships, facilitating efficient communication and decision-making.

Fig 2: Sample organizational structure of a nursing school
Common Organizational Models
| Organizational Model | Key Features | Planning Implications |
|---|---|---|
| Hierarchical Structure | Clear chain of command; multiple management levels | Planning flows from top leadership down; formal approval processes |
| Matrix Structure | Dual reporting relationships; project teams | Collaborative planning; integration across program areas |
| Shared Governance | Faculty committees; distributed decision-making | Participatory planning processes; faculty ownership |
| Flat Structure | Few management layers; decentralized authority | Agile planning; rapid response to changing needs |
Key Roles in Nursing Education Organization
Administrative Roles
- Dean/Director: Overall leadership and strategic planning
- Associate/Assistant Deans: Oversee specific program areas
- Department Chairs: Manage faculty and curriculum within specialties
- Program Coordinators: Implement planning at program level
Faculty/Support Roles
- Faculty: Implement teaching and evaluate learning
- Clinical Coordinators: Arrange clinical placements
- Simulation Coordinators: Manage lab facilities
- Student Services Staff: Support student needs
Organizational Committees Critical for Planning
- Curriculum Committee: Oversees program content and structure
- Assessment Committee: Evaluates program outcomes
- Faculty Development Committee: Plans professional growth activities
- Resource Allocation Committee: Manages budgeting and facilities
- Clinical Partnerships Committee: Develops relationships with healthcare facilities
Communication Pathways
Effective organizational structure facilitates communication essential for planning:
- Downward communication: Disseminating policies, procedures, and decisions
- Upward communication: Providing feedback and identifying needs
- Horizontal communication: Coordinating activities across departments
- Diagonal communication: Cross-functional project collaboration
Impact on Planning Effectiveness
The organizational structure directly influences how effectively a nursing program can plan and implement educational activities. Clear roles, efficient communication channels, and appropriate decision-making processes create an environment where planning can thrive.
When designing or evaluating organizational structures, nursing education leaders should consider how the structure supports strategic and operational planning processes. Aligning structure with the institution’s mission and philosophy enhances the program’s ability to achieve its educational objectives.
Curriculum Planning in Nursing Education
Curriculum planning is a systematic process of designing educational experiences that prepare students to meet the demands of professional nursing practice. It involves organizing content, learning activities, and evaluation strategies into a cohesive program of study.

Fig 3: The process of curriculum development in nursing education
Key Principles of Curriculum Planning
- Alignment with professional standards (e.g., AACN Essentials, NLN Competencies)
- Progression from simple to complex concepts and skills
- Integration of theory and practice throughout the program
- Incorporation of current healthcare trends and evidence-based practice
- Flexibility to accommodate diverse student needs and learning styles
The Curriculum Planning Process
Mnemonic: “ADDIE” Curriculum Planning Model
- Analyze – Assess needs and determine educational goals
- Design – Create the curriculum framework and structure
- Develop – Prepare detailed content and learning activities
- Implement – Deliver the curriculum to students
- Evaluate – Assess effectiveness and make improvements
Curriculum Frameworks
A curriculum framework provides the conceptual structure for organizing content and learning experiences. Common frameworks in nursing education include:
| Framework Type | Description | Planning Implications |
|---|---|---|
| Competency-Based | Organized around specific skills and abilities | Requires clear definition of performance expectations |
| Concept-Based | Structured around key nursing concepts | Emphasizes conceptual understanding over content memorization |
| Problem-Based | Uses clinical problems as organizing principle | Integrates clinical reasoning throughout curriculum |
| Systems-Based | Organized by body systems or healthcare delivery systems | Facilitates integration of anatomy, physiology, and pathophysiology |
Note: Many nursing programs use hybrid approaches that combine elements of different frameworks to create the most effective curriculum for their specific context and student population.
Curriculum Mapping
Curriculum mapping is a planning tool that visually represents how program components fit together, showing:
- Where specific content and competencies are introduced, reinforced, and mastered
- Relationships between courses and learning experiences
- Alignment with program outcomes and professional standards
- Potential gaps or redundancies in the curriculum
Factors Influencing Curriculum Planning
- Regulatory requirements: Accreditation standards, state board of nursing regulations
- Healthcare trends: Changing patient demographics, technological advances
- Institutional context: Mission, resources, faculty expertise
- Student characteristics: Academic preparation, learning needs
- Community needs: Local healthcare workforce demands
Effective curriculum planning is a collaborative process involving faculty, administrators, students, and community stakeholders. It requires ongoing review and revision to ensure that the program remains relevant and effective in preparing nurses for contemporary practice.
Planning Teaching and Learning Experiences
Planning teaching and learning experiences translates curriculum frameworks into actual educational activities. This level of planning focuses on creating engaging, effective learning opportunities that help students achieve course and program objectives.
Course Planning
Course planning involves developing detailed blueprints for individual courses, including:
- Course syllabus: Objectives, content outline, evaluation methods
- Content sequencing: Logical progression of topics
- Time allocation: Hours devoted to each content area
- Theory-practice balance: Integration of classroom and clinical learning
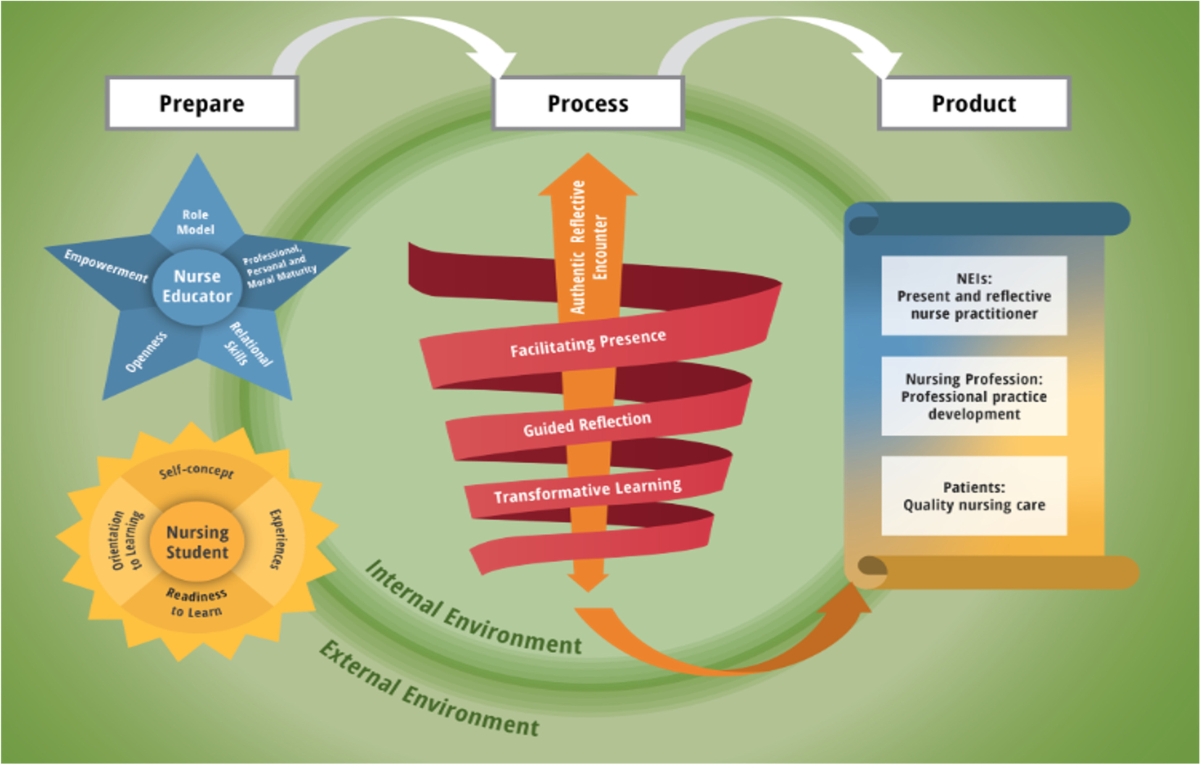
Fig 4: Conceptual model for nurse educators in planning learning experiences
Teaching Methods and Strategies
Effective planning includes selecting appropriate teaching methods that align with learning objectives and student needs:
| Teaching Method | Best Used For | Planning Considerations |
|---|---|---|
| Lecture | Introducing new concepts, providing foundation knowledge | Incorporate active learning strategies; use visual aids |
| Case Studies | Developing clinical reasoning and decision-making | Select realistic scenarios; align with course content |
| Simulation | Practicing skills in safe environment; team training | Develop scenarios; plan pre-briefing and debriefing |
| Problem-Based Learning | Promoting critical thinking and self-directed learning | Create authentic problems; plan facilitation approach |
| Team-Based Learning | Developing collaboration skills; peer teaching | Design effective team assignments; structure accountability |
| Flipped Classroom | Maximizing active learning time; application of knowledge | Create pre-class materials; plan interactive activities |
Mnemonic: “VARK” Learning Styles in Planning
- Visual – Include diagrams, charts, videos in teaching plans
- Auditory – Incorporate discussions, lectures, audio resources
- Reading/Writing – Provide texts, handouts, writing activities
- Kinesthetic – Plan hands-on activities, simulations, role-plays
Lesson Planning
Detailed lesson plans are essential microlevels of planning that guide individual teaching sessions:
Elements of an Effective Lesson Plan
- Specific learning objectives for the session
- Pre-requisite knowledge students should possess
- Content outline with key points to cover
- Teaching/learning activities with time allocations
- Resources and materials needed
- Formative assessment strategies
- Contingency plans for unexpected situations
Technology Integration Planning
Modern nursing education requires thoughtful planning for technology integration:
- Learning management systems (LMS): Organizing course materials and activities
- Virtual simulation: Creating immersive learning experiences
- Mobile applications: Supporting point-of-care learning
- Collaborative tools: Facilitating group work and discussion
- Assessment technologies: Evaluating student performance
Planning for Diverse Learners
Inclusive teaching planning considers student diversity in terms of:
- Learning styles and preferences
- Educational backgrounds and prior experiences
- Cultural and linguistic diversity
- Students with disabilities or learning differences
Effective planning of teaching and learning experiences requires continuous reflection and adjustment based on student feedback and performance. The most successful plans maintain flexibility while providing clear structure and direction for both faculty and students.
Clinical Facilities: Master Plan and Rotation
Clinical education is a cornerstone of nursing programs, requiring meticulous planning to ensure students gain appropriate experiences in healthcare settings. This involves creating master plans and clinical rotation schedules that optimize learning opportunities while managing logistical challenges.
Master Plan Definition
A master plan is an overall academic year plan denoting the placement of particular groups of students, including theoretical blocks, partial blocks (half clinical & half theory), clinical blocks, examinations, vacations, and co-curricular activities.
Purpose of Master Plan in Clinical Education
- Provides an advanced plan before implementing curricular activities
- Ensures all stakeholders are aware of student placements
- Facilitates more effective coordination
- Helps students and teachers prepare adequately
- Allows for necessary modifications based on changing situations
- Enables faculty to plan leave and vacation without disrupting teaching
Principles of Preparing Master Plan
- Plan in accordance with the curriculum requirements
- Develop plans well in advance of the academic year
- Ensure theoretical instruction precedes clinical experience
- Distribute each subject throughout the academic year for continuity
- Allocate additional hours beyond minimum requirements to accommodate unforeseen changes
- Follow teaching maxims when planning activities
- Ensure activities are feasible for both faculty and students
Factors to Consider in Master Planning
- Course objectives and requirements
- Academic year duration and structure
- Statutory body requirements (e.g., INC, state boards)
- Institutional protocols and preferences
- Number of students and available groups
- Number and size of available clinical departments
- Faculty availability and expertise

Fig 5: Model guideline flowchart for healthcare planning applicable to clinical rotations
Clinical Rotation Planning
Clinical Rotation Plan
A clinical rotation plan is a statement explaining the order of clinical postings for various groups of nursing students in relevant clinical areas and community health settings as per requirements laid down by statutory bodies.
Principles in Planning Clinical Rotation
- Clinical supervisors must be familiar with the rotation plan
- Students should be posted where they will receive maximum supervision
- Each student should receive all required experiences on a rotation basis
- Avoid overcrowding in any clinical area
- Students should enter and leave clinical areas at designated times
- Theoretical instruction should precede or coincide with related clinical experiences
- Maintain appropriate teacher-student ratios (e.g., 1:4 in general areas, 1:1 in critical care)
Mnemonic: “CLINICAL” Rotation Planning Essentials
- Comprehensive coverage of required experiences
- Logical progression from simple to complex
- Integration of theory with practice
- Number of students appropriate to setting
- Instructional support consistently available
- Communication with facility partners
- Adequate duration for meaningful learning
- Learning objectives clearly defined
Components of Clinical Rotation Schedule
- Student group assignments
- Clinical site locations
- Specific units or departments
- Rotation dates and times
- Faculty assignments
- Preceptor information (if applicable)
- Specific learning objectives for each rotation
Benefits of Effective Clinical Planning
- Enhanced supervision of students
- Comprehensive exposure to required experiences
- Prevention of overcrowding in clinical areas
- Simplified evaluation process
- Reduced confusion among teachers and students
- Achievement of all learning objectives by students
Note: Clinical rotation plans should be regularly reviewed and adjusted based on feedback from students, faculty, and clinical partners to ensure optimal learning experiences and address any emerging challenges.
The master plan and clinical rotation schedule are vital planning tools that ensure nursing students receive well-structured, comprehensive clinical experiences. Careful attention to these aspects of planning contributes significantly to developing competent, confident nursing graduates ready for professional practice.
Summary and Key Takeaways
Effective planning and organizing in nursing education create the foundation for successful student learning experiences and program outcomes. Throughout this comprehensive guide, we’ve explored various dimensions of educational planning, from philosophical underpinnings to practical implementation strategies.
Key Principles of Effective Planning in Nursing Education
- Align all planning activities with program philosophy, mission, and objectives
- Develop clear organizational structures that support educational goals
- Create curriculum plans that integrate theory and practice
- Design teaching and learning experiences that address diverse student needs
- Implement comprehensive clinical rotation plans that maximize learning opportunities
The Planning Continuum in Nursing Education
Remember that planning in nursing education occurs along a continuum:
- Strategic planning: Long-term direction and goals (3-5 years)
- Programmatic planning: Overall curriculum structure and organization
- Course planning: Specific course content and assessments
- Instructional planning: Individual teaching sessions and activities
- Clinical planning: Rotations and practice experiences
Each level of planning informs and influences the others, creating an integrated system that supports student learning and program effectiveness.
Planning as an Ongoing Process
Successful planning in nursing education is not a one-time event but an ongoing, cyclical process that involves:
- Assessment: Gathering data about current performance and needs
- Development: Creating plans based on assessment findings
- Implementation: Putting plans into action
- Evaluation: Assessing the effectiveness of implemented plans
- Revision: Adjusting plans based on evaluation results
“Thoughtful planning creates the architecture for educational excellence in nursing, ensuring that graduates are prepared to meet the complex challenges of contemporary healthcare practice.”
By mastering the principles and practices of effective planning in nursing education, faculty and administrators can create programs that not only meet regulatory requirements but also inspire excellence in teaching and learning. The result is nursing graduates who possess the knowledge, skills, and professional attributes needed to provide high-quality care in diverse healthcare settings.
Nursing Education Management
Comprehensive Guide for Nursing Students
Table of Contents
1. Introduction to Nursing Education Management
Effective management of nursing education programs requires careful planning, organization, and administration of various resources. This comprehensive guide explores the critical aspects of nursing education management, including budget planning, infrastructure development, record-keeping, committee functioning, and clinical experience coordination.
The 5 Pillars of Nursing Education Management
Successful nursing education programs rest on five essential pillars that administrators must carefully manage:
- Budget Planning: Allocation and utilization of financial resources
- Infrastructure Development: Physical facilities that support learning
- Records Management: Documentation and information systems
- Committee Organization: Collaborative governance structures
- Clinical Experience Coordination: Practical training opportunities
Mnemonic: “BIRC-C”
Remember the five key areas of nursing education management with “BIRC-C”:
- Budget planning
- Infrastructure facilities
- Records and reports
- Committees and functioning
- Clinical experiences
2. Budget Planning
Budget planning is the cornerstone of effective educational management. It involves the strategic allocation of financial resources to support various aspects of nursing education programs.
Needs Assessment
Budget Preparation
Approval Process
Implementation
Evaluation
2.1 Faculty & Staff Budget Planning
Allocating resources for human capital is typically the largest expenditure in nursing education management. This includes salaries, benefits, professional development, and recruitment costs.
| Budget Category | Components | Considerations |
|---|---|---|
| Salaries | Base pay, increments, bonuses | Qualifications, experience, market rates |
| Benefits | Health insurance, retirement plans | Legal requirements, competitive packages |
| Professional Development | Conferences, workshops, certifications | Required CE credits, institutional goals |
| Recruitment | Advertising, interview expenses | Staffing needs, turnover rates |
| Adjunct Faculty | Part-time instructors, guest lecturers | Course loads, specialty needs |
Faculty-to-Student Ratio Planning
Effective management requires maintaining appropriate faculty-to-student ratios:
- Classroom instruction: 1:30-40
- Skills laboratory: 1:10-15
- Clinical settings: 1:8-10 (varies by regulatory requirements)
2.2 Equipment & Supplies Budget
This category encompasses consumable supplies and durable equipment needed for educational delivery. Effective management requires balancing immediate needs with long-term investments.
Consumable Supplies
- Medical disposables (gloves, syringes, dressings)
- Office supplies (paper, pens, folders)
- Cleaning and maintenance supplies
- Printing materials (handouts, exams)
- Simulation consumables
Durable Equipment
- Medical equipment (BP apparatus, stethoscopes)
- Office equipment (desks, chairs, cabinets)
- Educational technology (projectors, screens)
- Safety equipment (fire extinguishers, first aid kits)
- Specialized teaching equipment
Mnemonic: “The 4 Rs of Equipment Budgeting”
- Replace (worn-out or obsolete items)
- Repair (maintenance of existing equipment)
- Restock (consumable supplies)
- Renew (update technology and methods)
2.3 AV Aids & Lab Equipment
Audiovisual aids and laboratory equipment are essential teaching tools that require specialized management and budgeting considerations.
| Category | Essential Items | Budget Considerations |
|---|---|---|
| AV Equipment | Projectors, screens, smart boards, speakers | Installation, warranties, compatibility, upgrades |
| Simulation Equipment | Mannequins, simulators, task trainers | High initial cost, maintenance contracts, training |
| Basic Lab Equipment | Hospital beds, vital sign equipment, IV stands | Durability, replacement cycles, quantity needed |
| Specialized Equipment | Ventilators, ECG machines, delivery models | Specialty program requirements, industry standards |
| Digital Resources | Virtual simulations, learning software | Licensing fees, updates, server requirements |
Common AV & Lab Budget Pitfalls
Avoid these common management mistakes:
- Underestimating maintenance costs (typically 10-15% of purchase price annually)
- Neglecting staff training on new equipment
- Failing to budget for software updates and licensing renewals
- Not planning for technological obsolescence
- Inadequate storage and security provisions
2.4 Library Resources
A robust library budget ensures students and faculty have access to current knowledge resources, requiring careful management of both physical and digital assets.
Print Resources
- Textbooks (core and specialty)
- Reference books
- Print journals and periodicals
- Student study guides
- Test preparation materials
Digital Resources
- E-book subscriptions
- Online journal databases
- Evidence-based practice resources
- Clinical decision support tools
- Research databases
Library Budget Allocation Formula
A balanced approach to library management typically follows this distribution:
- Core textbooks and references: 30-35%
- Journal subscriptions (print and digital): 25-30%
- Online databases and resources: 20-25%
- New acquisitions and updates: 10-15%
- Library management software: 5-10%
2.5 Computers & Maintenance
Technology infrastructure requires substantial initial investment and ongoing management for maintenance, upgrades, and support services.
| Budget Category | Components | Planning Considerations |
|---|---|---|
| Hardware | Computers, servers, printers, network equipment | 3-5 year replacement cycle, specifications needed |
| Software | Operating systems, educational software, security software | Licensing models (perpetual vs. subscription), compatibility |
| IT Support | Technicians, help desk, training | In-house vs. outsourced, response time requirements |
| Maintenance Contracts | Extended warranties, service agreements | Coverage levels, response guarantees, exclusions |
| Infrastructure | Internet connectivity, Wi-Fi, network security | Bandwidth requirements, security levels, redundancy |
Mnemonic: “SETUP” – Technology Budget Essentials
- Software (educational programs, administrative systems)
- Equipment (computers, printers, networking hardware)
- Technical support (IT personnel, help desk services)
- Upkeep (maintenance contracts, repairs, updates)
- Protection (security systems, data backup, disaster recovery)
3. Infrastructure Facilities
Physical infrastructure provides the foundation for nursing education and requires strategic management to create optimal learning environments. Infrastructure planning must align with educational objectives, regulatory requirements, and future growth projections.
3.1 College & Classroom Infrastructure
The physical campus and classroom environments significantly impact learning outcomes and require thoughtful management to meet educational standards.
| Infrastructure Component | Design Considerations | Management Requirements |
|---|---|---|
| Classrooms | Seating capacity, acoustics, ventilation, lighting | Regular maintenance, technology upgrades, flexible configurations |
| Faculty Offices | Privacy, storage, meeting space | Allocation system, furnishing standards, security |
| Administrative Spaces | Reception, record storage, conference rooms | Accessibility, workflow efficiency, security protocols |
| Common Areas | Student lounges, cafeteria, outdoor spaces | Cleaning schedules, usage policies, safety monitoring |
| Accessibility Features | Ramps, elevators, accessible restrooms | ADA compliance, regular inspections, accommodation processes |
Classroom Space Requirements
Effective classroom management requires adequate space allocation:
- Lecture classrooms: 25-30 sq. ft. per student
- Interactive learning spaces: 35-40 sq. ft. per student
- Demonstration rooms: 45-50 sq. ft. per student
- Simulation spaces: 50-60 sq. ft. per student
3.2 Hostel Facilities
Residential facilities for nursing students require comprehensive management systems to ensure safety, comfort, and an environment conducive to study.
Essential Hostel Components
- Student rooms (single/shared accommodations)
- Bathroom and shower facilities
- Common study areas
- Recreation spaces
- Dining facilities or kitchenettes
- Laundry services
- Security systems and personnel
Hostel Management Systems
- Accommodation allocation procedures
- Maintenance request protocols
- Safety and emergency protocols
- Resident supervision structure
- Visitor management policies
- Code of conduct enforcement
- Conflict resolution mechanisms
Mnemonic: “HOMES” – Essential Hostel Management Focus Areas
- Health and safety (emergency protocols, sanitization)
- Operations (daily functioning, staff management)
- Maintenance (repairs, renovations, cleanliness)
- Environment (study-friendly atmosphere, noise control)
- Support services (counseling, recreation, security)
3.3 Library & Laboratory Infrastructure
Specialized learning spaces require distinct infrastructure management approaches to facilitate both theoretical and practical education.
| Facility | Essential Features | Management Considerations |
|---|---|---|
| Main Library | Shelving, reading areas, reference section, checkout systems | Cataloging systems, inventory management, access hours |
| Digital Library | Computer stations, network access, database subscriptions | Authentication systems, usage tracking, technical support |
| Fundamentals Lab | Basic nursing equipment, practice stations, storage | Supply inventory, cleaning protocols, scheduling system |
| Simulation Lab | High-fidelity mannequins, control rooms, debriefing spaces | Technical support, scenario development, maintenance contracts |
| Specialty Labs | Area-specific equipment (maternity, pediatric, mental health) | Specialized maintenance, certification requirements, usage tracking |
Laboratory Space Planning Standards
Effective lab management requires appropriate space allocation:
- Skills laboratory: 50-60 sq. ft. per student
- Simulation laboratories: 70-80 sq. ft. per student
- Storage areas: Approximately 20% of total laboratory space
- Debriefing/conference spaces: 25-30 sq. ft. per student
- Control/observation rooms: 150-200 sq. ft. per simulation room
3.4 Computer & Transport Facilities
Supporting infrastructure systems that facilitate learning and access require specialized management approaches.
Computer Lab Requirements
- Adequate workstations (1:4 student ratio minimum)
- Reliable internet connectivity
- Printing and scanning facilities
- Specialized nursing software
- Technical support availability
- Data security systems
- Accessibility accommodations
Transport Facility Management
- Vehicle fleet (buses, vans)
- Driver employment and certification
- Maintenance and safety inspections
- Route planning and scheduling
- Transportation to clinical sites
- Emergency transportation protocols
- Accessibility accommodations
Transport Management Challenges
Effective transportation management must address these common challenges:
- Coordinating varied clinical rotation schedules
- Ensuring timely arrival for clinical placements
- Managing transportation costs (fuel, maintenance, insurance)
- Ensuring safety and emergency preparedness
- Accommodating students with special needs
- Managing transportation during inclement weather
4. Records & Reports
Effective records management is essential for maintaining educational standards, meeting regulatory requirements, and supporting decision-making. A comprehensive records system encompasses student, staff, faculty, and administrative documentation.
Creation
Verification
Storage
Access
Disposition
4.1 Student Records
Student records document academic progress, clinical experiences, and personal information, requiring careful management for both operational and compliance purposes.
| Record Category | Essential Components | Management Considerations |
|---|---|---|
| Academic Records | Admission documents, transcripts, grades, attendance | FERPA compliance, retention schedule, access controls |
| Clinical Records | Skills checklists, clinical hours, evaluations | Verification process, competency tracking, site requirements |
| Health Records | Immunizations, health clearances, accident reports | HIPAA compliance, confidentiality, clinical site requirements |
| Disciplinary Records | Incident reports, remediation plans, outcomes | Due process documentation, confidentiality, legal review |
| Financial Records | Tuition payments, scholarships, financial aid | Audit trails, reconciliation processes, compliance |
Mnemonic: “FACTS” – Student Records Essentials
- Financial documents (tuition, fees, scholarships)
- Academic performance (grades, evaluations, progression)
- Clinical experiences (hours, competencies, sites)
- Technical requirements (immunizations, certifications)
- Support services (advising, accommodations, counseling)
4.2 Staff & Faculty Records
Personnel records document qualifications, performance, and professional development, requiring systematic management for both administrative and regulatory purposes.
Faculty Records Components
- Educational credentials and transcripts
- Licensure and certification documentation
- Teaching evaluations and peer reviews
- Professional development activities
- Research and publication history
- Committee service documentation
- Annual performance evaluations
Staff Records Components
- Employment applications and resumes
- Job descriptions and classification
- Performance evaluations
- Professional development records
- Attendance and leave records
- Disciplinary documentation
- Salary and benefits information
Faculty Qualification Documentation Requirements
Accreditation standards typically require faculty records management systems to verify:
- Educational preparation at appropriate degree level
- Current clinical expertise in teaching specialty
- Continuing education and professional development
- Active licensure and specialty certifications
- Teaching effectiveness and evaluation outcomes
- Scholarly activities and contributions to the profession
4.3 Administrative Records
Institutional records document operations, decisions, and compliance activities, requiring structured management for accountability and continuity.
| Record Category | Essential Components | Management Requirements |
|---|---|---|
| Policy & Procedure Documents | Student handbook, faculty manual, operational protocols | Version control, review schedule, approval documentation |
| Meeting Records | Minutes, attendance, decision documentation | Format standardization, archiving, accessibility |
| Accreditation Documents | Self-study reports, site visit records, correspondence | Evidence organization, timeline tracking, response documentation |
| Budget and Financial Records | Annual budgets, expenditure reports, audits | Security controls, reconciliation processes, retention requirements |
| Facilities and Safety Records | Maintenance logs, inspection reports, incident documentation | Compliance verification, action response, regular review |
Records Management System Requirements
Effective administrative records management systems must include:
- Clear retention schedules for all document types
- Secure storage with appropriate access controls
- Disaster recovery and backup systems
- Compliance with legal and regulatory requirements
- Efficient retrieval and reporting capabilities
- Regular audits and integrity checks
5. Committees & Functioning
Committee structures provide shared governance and distributed decision-making in nursing education programs. Effective committee management enhances institutional operations, ensures diverse input, and promotes transparency.
5.1 Types of Committees
Nursing education programs typically establish various committees to address specific functional areas, requiring distinct management approaches.
| Committee Type | Core Functions | Typical Membership |
|---|---|---|
| Curriculum Committee | Curriculum development, evaluation, revision | Faculty from all specialty areas, student representatives |
| Admissions Committee | Applicant review, selection criteria, admission decisions | Faculty, admissions staff, diversity officer |
| Student Affairs Committee | Student policies, grievances, progression issues | Faculty, student services staff, student representatives |
| Faculty Development Committee | Faculty orientation, continuing education, mentoring | Experienced faculty, educational specialists |
| Evaluation Committee | Program assessment, outcomes measurement, improvements | Assessment specialists, faculty representatives, administrators |
| Resource Management Committee | Budget review, resource allocation, infrastructure planning | Administrators, faculty representatives, financial specialists |
Advisory Committees Structure
External advisory committees provide important management input and typically include:
- Healthcare industry representatives
- Clinical partners and practice leaders
- Community stakeholders
- Alumni representatives
- Educational partners (other institutions)
- Regulatory or accreditation experts
- Patient/consumer advocates
5.2 Committee Formation & Structure
Establishing effective committees requires careful management of membership, leadership, and operational processes.
Committee Formation Best Practices
- Clearly defined purpose and scope
- Written charter or terms of reference
- Balanced representation across stakeholders
- Diversity in expertise and perspectives
- Defined terms of service (typically 2-3 years)
- Staggered membership for continuity
- Established leadership selection process
Committee Structure Elements
- Chair and co-chair roles
- Secretary or recorder position
- Regular meeting schedule
- Standard agenda format
- Decision-making process (consensus/voting)
- Reporting relationships
- Subcommittee formation procedures
Mnemonic: “CHAIRS” – Committee Formation Framework
- Charter (defined purpose and authority)
- Human resources (appropriate membership)
- Authority (decision-making parameters)
- Integration (connection to larger organization)
- Responsibilities (specific tasks and deliverables)
- Structure (operational framework and processes)
5.3 Effective Committee Functioning
Successful committees require ongoing management to maintain productivity, engagement, and alignment with institutional goals.
| Committee Process | Best Practices | Management Considerations |
|---|---|---|
| Meeting Management | Advance agendas, timed discussions, action-oriented minutes | Time efficiency, participation monitoring, follow-up processes |
| Decision Making | Evidence-based approaches, transparent processes | Documentation, stakeholder communication, implementation planning |
| Communication | Regular updates, clear reporting channels | Multi-directional communication, feedback loops |
| Work Distribution | Task assignment, subcommittee formation | Workload equity, timeline monitoring, accountability |
| Evaluation | Self-assessment, impact measurement | Continuous improvement, alignment with goals, effectiveness metrics |
Common Committee Dysfunction Indicators
Effective management requires monitoring for these warning signs:
- Chronic low attendance or engagement
- Meetings regularly exceeding scheduled time
- Recurring unresolved agenda items
- Domination by one or few members
- Lack of follow-through on action items
- Decision reversal or revisiting settled issues
- Mission drift from original charter
6. Clinical Experiences
Clinical education is the cornerstone of nursing education, requiring sophisticated management systems to ensure quality learning experiences, patient safety, and regulatory compliance.
6.1 Clinical Placement Management
Securing and coordinating appropriate clinical learning environments requires structured management processes and strong industry partnerships.
Partnership Development
Agreement Formalization
Scheduling
Student Preparation
Evaluation
| Placement Component | Critical Elements | Management Strategies |
|---|---|---|
| Clinical Site Agreements | Legal contracts, liability coverage, term specifications | Regular review, relationship maintenance, compliance monitoring |
| Clinical Capacity Planning | Site capacity assessment, student-to-preceptor ratios | Capacity forecasting, alternative site development, schedule optimization |
| Student Requirements | Health records, background checks, orientation completion | Centralized tracking, compliance deadlines, documentation systems |
| Site-Specific Orientation | Facility protocols, EMR training, safety procedures | Standardized orientation materials, completion verification, updates |
| Placement Coordination | Student assignments, rotation schedules, site communication | Dedicated coordinator role, tracking systems, communication protocols |
Clinical Site Portfolio Management
Optimal clinical education requires strategic management of a diverse clinical site portfolio:
- Acute care facilities (teaching and community hospitals)
- Ambulatory care settings (clinics, physician offices)
- Long-term care facilities (nursing homes, rehabilitation centers)
- Community health settings (public health departments, schools)
- Specialty settings (mental health, pediatric, women’s health)
- Emerging practice sites (telehealth, home health, correctional health)
6.2 Clinical Supervision Management
Effective clinical education requires structured supervision management to ensure learning objectives are met while maintaining patient safety standards.
Faculty Supervision Model
- Faculty directly supervises student group (1:8-10)
- Faculty provides instruction, guidance, evaluation
- Faculty maintains clinical expertise in specialty
- Faculty coordinates with clinical staff
- Faculty ensures clinical objectives are met
- Faculty conducts pre/post conferences
Preceptor Supervision Model
- Staff nurse serves as preceptor (1:1 or 1:2)
- Faculty oversees multiple preceptor relationships
- Preceptors require specific preparation
- More common in advanced clinical experiences
- Requires coordination between faculty and preceptors
- Includes regular faculty site visits
Mnemonic: “CLINICAL” – Supervision Management Framework
- Communication systems between all stakeholders
- Learning objectives clearly defined and shared
- Intervention guidelines for student performance issues
- Navigation of facility policies and procedures
- Integration of theory and practice emphasized
- Competency development tracked systematically
- Assessment methods standardized and documented
- Liaison relationships maintained with clinical partners
6.3 Clinical Evaluation Management
Assessing student performance in clinical settings requires comprehensive management systems to ensure fair, objective, and consistent evaluation.
| Evaluation Component | Assessment Methods | Management Considerations |
|---|---|---|
| Skills Performance | Direct observation, skills checklists, return demonstrations | Standardized evaluation tools, inter-rater reliability, remediation protocols |
| Critical Thinking | Care planning, case studies, clinical reasoning exercises | Rubric development, progressive complexity, feedback mechanisms |
| Professional Behaviors | Observation, self-assessment, peer feedback | Clear behavioral expectations, documentation systems, early intervention |
| Documentation Skills | Chart audits, care plan review, simulation documentation | Documentation standards, chart audit tools, feedback loops |
| Clinical Judgment | Simulation assessments, clinical decision-making tools | Structured debriefing, progressive expectations, competency frameworks |
Clinical Evaluation Management Challenges
Effective clinical evaluation management must address:
- Subjectivity in performance assessment
- Documentation of borderline performance
- Managing failing students in clinical settings
- Consistency across multiple evaluators
- Balancing formative and summative evaluation
- Legal considerations in clinical failure situations
- Accommodating students with learning differences
7. Conclusion
Effective nursing education management requires a systematic approach to planning, organizing, and evaluating all aspects of the educational program. The five key areas—budget planning, infrastructure facilities, records and reports, committees, and clinical experiences—are interconnected and must be managed comprehensively to ensure program quality and student success.
Key Management Integration Points
Successful nursing education programs integrate management across all domains:
- Strategic Alignment: All management decisions support program mission and goals
- Resource Optimization: Budget and infrastructure management enables educational excellence
- Information Systems: Records management provides data for continuous improvement
- Collaborative Governance: Committee management ensures inclusive decision-making
- Practice Integration: Clinical experience management bridges theory and practice
By implementing comprehensive management systems across these five domains, nursing education programs can create optimal learning environments, meet regulatory requirements, and develop competent, practice-ready graduates who will advance the nursing profession.
