Comprehensive Forensic Nursing
Team Members, Roles, and Responsibilities
A complete educational resource for nursing students on forensic teams, roles, and nursing care for victims of violence
Table of Contents
Introduction to Forensic Nursing
Forensic nursing represents a specialized domain where healthcare and legal systems intersect. It involves the application of nursing science combined with forensic science to public and legal proceedings, addressing both clinical and legal aspects of trauma and death investigation.
Forensic nursing is officially defined by the International Association of Forensic Nurses (IAFN) as “the practice of nursing globally when health and legal systems intersect.”
The essential role of forensic nurses includes providing specialized care to victims of violence while simultaneously preserving evidence, documenting injuries, and collaborating with legal authorities—all while maintaining patient dignity and confidentiality.
This comprehensive guide delves into the multifaceted aspects of forensic nursing teams, their compositions, and the holistic care they provide across physical, psychological, cultural, and legal domains.
Forensic Team Members and Their Roles

Core Team Composition
A comprehensive forensic team operates as a multidisciplinary unit where each member contributes unique expertise to address the complex needs of violence victims. The effectiveness of forensic nursing interventions often depends on successful team collaboration.
| Team Member | Primary Responsibilities | Interaction with Forensic Nurse |
|---|---|---|
| Forensic Nurse Examiner (FNE) |
|
Central team coordinator, often serves as the bridge between medical and legal systems |
| Forensic Physician |
|
Collaborates with forensic nurses on complex cases requiring physician expertise |
| Law Enforcement Officers |
|
Works closely with forensic nurses to ensure evidence integrity and case development |
| Social Workers |
|
Partners with forensic nurses to address immediate and long-term psychosocial needs |
| Evidence Technicians |
|
Receives and processes evidence collected by forensic nurses |
| Victim Advocates |
|
Works alongside forensic nurses to ensure victim-centered approach to care |
| Prosecutors/Legal Team |
|
Consults with forensic nurses on evidence documentation and prepares them for testimony |
| Mental Health Professionals |
|
Receives referrals from forensic nurses for ongoing psychological care |
Communication Pathways Within Forensic Teams
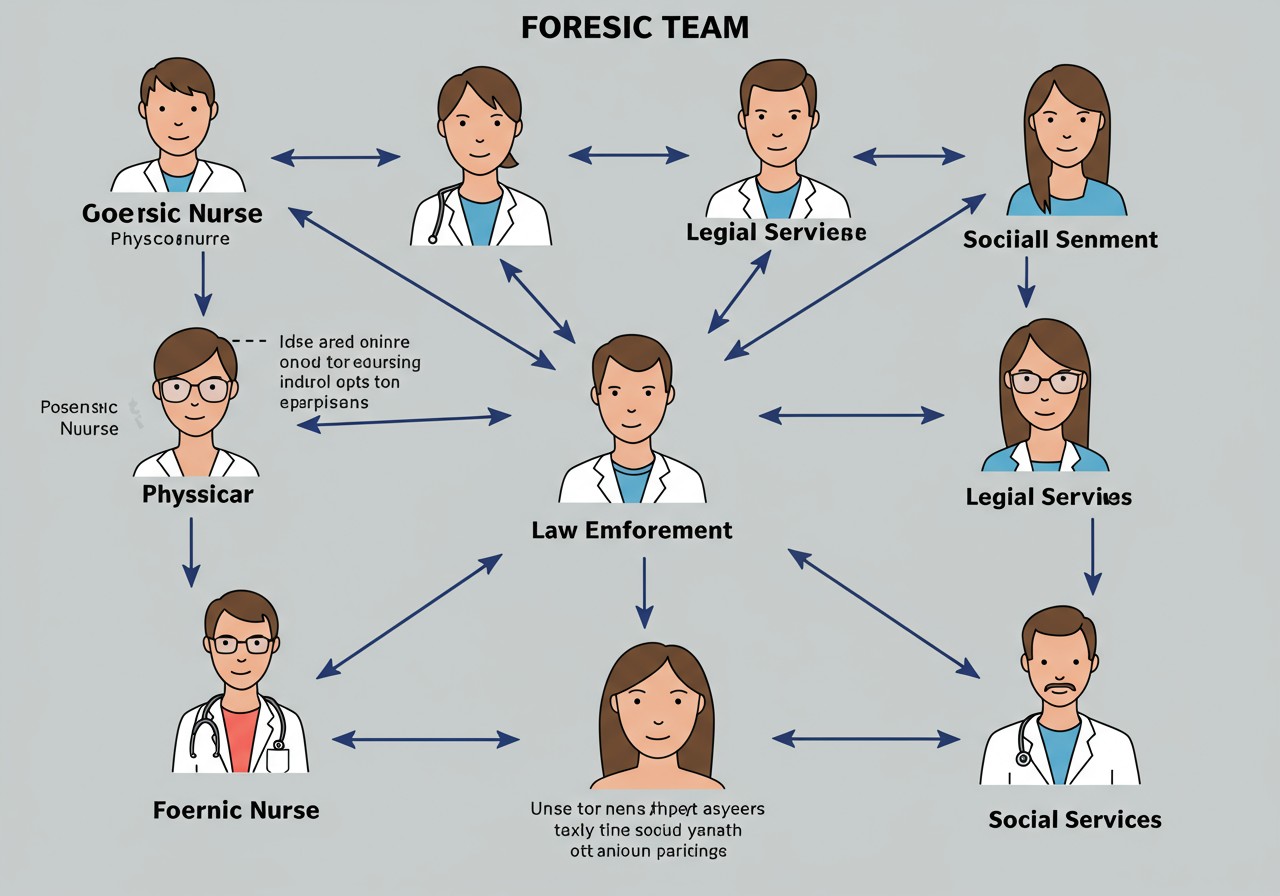
Effective communication is the foundation of successful forensic team operations. Information must flow seamlessly between team members while maintaining confidentiality and preserving evidence integrity.
Mnemonic: “TEAMS” – Essential Elements of Forensic Team Communication
- T – Timely reporting of findings to appropriate team members
- E – Explicit documentation using standardized terminology
- A – Accurate information sharing without assumptions
- M – Multidisciplinary collaboration through regular case conferences
- S – Secure information transfer respecting privacy and evidence integrity
Physical Aspects of Forensic Nursing Care
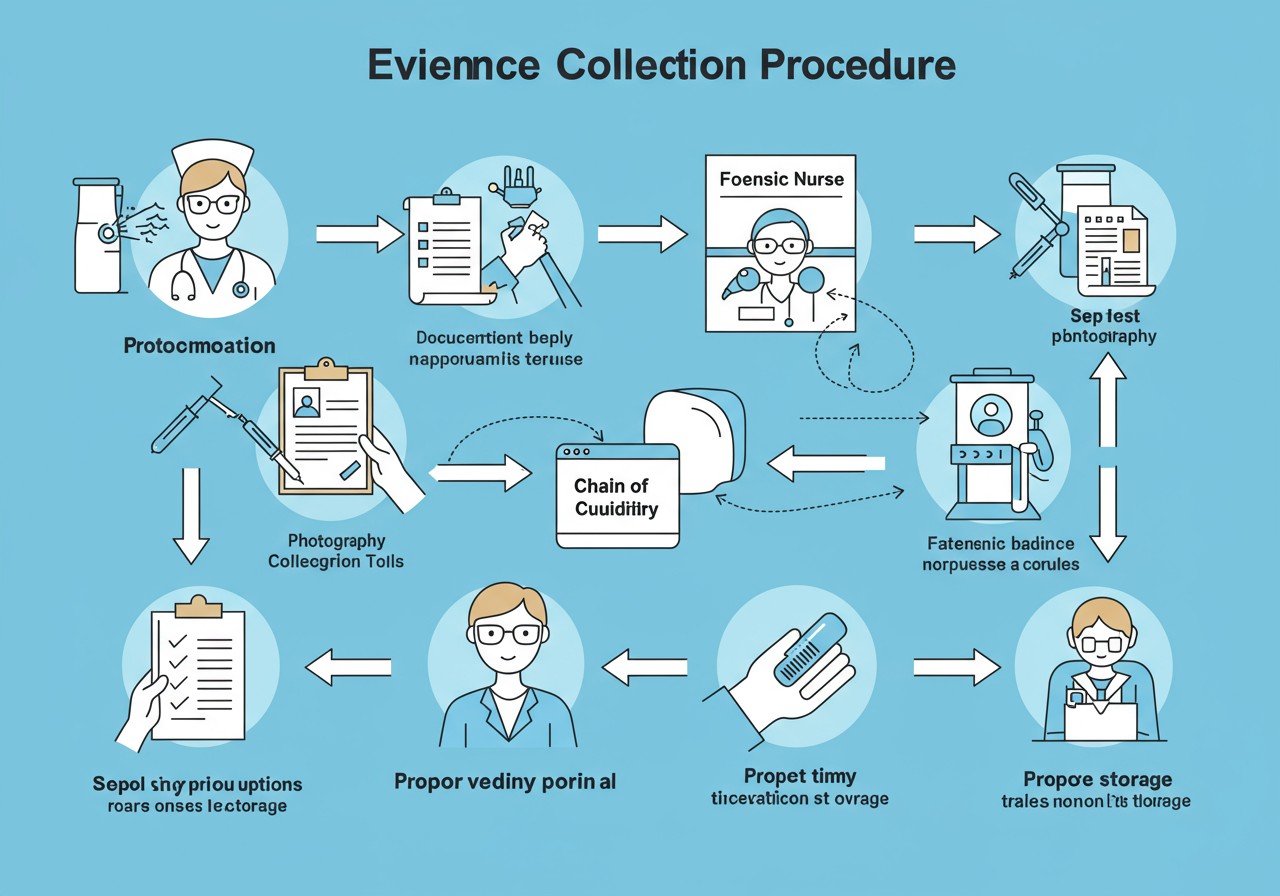
Evidence Collection and Documentation
The forensic nurse’s approach to physical care combines therapeutic nursing interventions with meticulous evidence collection. This dual focus requires specialized skills and strict adherence to protocols.
Initial Assessment
Forensic nurses perform a comprehensive physical assessment, identifying and documenting all injuries while simultaneously addressing immediate medical needs. This includes vital signs, general appearance, and injury patterns.
Evidence Collection
Using specialized kits and techniques, forensic nurses collect biological samples (blood, saliva, hair, fibers), photograph injuries, obtain clothing, and preserve trace evidence. Each step follows strict chain of custody protocols.
Injury Documentation
Forensic nurses document injuries using anatomical diagrams, standardized terminology, measurement tools, and photography. Documentation includes size, shape, color, location, and pattern of each injury.
Medical Treatment
While preserving evidence, forensic nurses provide necessary medical interventions, including wound care, medication administration, and coordination of diagnostic tests and specialty consultations.
Chain of Custody
Maintaining proper chain of custody for all collected evidence is critical. Each item must be properly labeled, secured, and transferred with documentation of every person who handles it.
A forensic nurse’s documentation serves two crucial purposes: guiding medical treatment and providing legal evidence. Every detail must be accurate, objective, and comprehensive.
Specialized Physical Assessments by Injury Type
| Type of Violence | Key Assessment Elements | Specialized Evidence Collection |
|---|---|---|
| Sexual Assault |
|
|
| Intimate Partner Violence |
|
|
| Child Abuse |
|
|
| Elder Abuse |
|
|
| Human Trafficking |
|
|
Mnemonic: “PRESERVE” – Physical Evidence Collection Principles
- P – Prioritize patient care while collecting evidence
- R – Record all findings immediately and thoroughly
- E – Establish chain of custody for all specimens
- S – Secure evidence in proper containers/packaging
- E – Explain procedures to patient before performing them
- R – Respect patient dignity throughout examination
- V – Verify all documentation is complete and accurate
- E – Ensure proper transfer of evidence to authorities
Cultural and Spiritual Aspects
Cultural Considerations in Forensic Nursing
Cultural competence is essential in forensic nursing practice. Violence occurs across all cultural backgrounds, but cultural factors influence how victims experience trauma, seek help, and engage with healthcare and legal systems.
Cultural Influences on Care
- Communication styles and language barriers
- Attitudes toward authority figures
- Gender roles and expectations
- Views on privacy and modesty
- Help-seeking behaviors
- Perceptions of violence and victimhood
- Family involvement in decision-making
Cultural Assessment Elements
- Preferred language for communication
- Cultural identification and practices
- Gender and examiner preferences
- Immigration status concerns
- Community support structures
- Traditional healing practices
- Cultural meanings associated with trauma
When working with patients from diverse cultural backgrounds, forensic nurses must balance culturally responsive care with forensic evidence collection requirements. This may include modifying examination approaches while maintaining evidence integrity.
Cultural Competence Strategies
| Strategy | Implementation in Forensic Nursing |
|---|---|
| Use professional interpreters | Utilize certified medical interpreters rather than family members to ensure accurate communication and confidentiality during sensitive discussions. |
| Adapt examination procedures | Modify approaches to accommodate cultural needs while maintaining evidence integrity (e.g., positioning, draping techniques, gender of examiner). |
| Engage cultural brokers | Work with community representatives who can help bridge cultural gaps and explain unfamiliar medical and legal processes. |
| Provide culturally specific resources | Connect patients with organizations that serve specific cultural communities and understand their unique needs. |
| Recognize historical trauma | Acknowledge how historical experiences of discrimination or mistreatment by healthcare or legal systems may affect current trust and engagement. |
Spiritual Dimensions of Forensic Nursing Care
Spirituality often provides meaning, purpose, and coping resources for victims of violence. Forensic nurses incorporate spiritual care while respecting diverse belief systems and avoiding assumptions about religious practices.
Spiritual Impact of Violence
- Questioning of faith or belief systems
- Spiritual distress or crisis
- Feelings of punishment or abandonment
- Loss of meaning or purpose
- Challenges to worldview
- Finding spiritual strength in recovery
Spiritual Care Interventions
- Respectful inquiry about spiritual needs
- Accommodating religious practices when possible
- Facilitating access to spiritual care providers
- Supporting meaningful rituals
- Respecting objects of spiritual significance
- Creating space for existential questions
Mnemonic: “DIVERSE” – Cultural and Spiritual Care Framework
- D – Dialogue about cultural and spiritual preferences
- I – Incorporate cultural practices into care plan
- V – Value diversity in responses to trauma
- E – Engage appropriate cultural/spiritual resources
- R – Respect individual beliefs without judgment
- S – Support cultural identity as a strength
- E – Evaluate own biases and assumptions
Legal Aspects of Forensic Nursing
Legal Framework
Forensic nursing practice exists at the intersection of healthcare and legal systems. Understanding the legal context is essential for effective forensic nursing care and appropriate evidence handling.
Key Legal Considerations
| Legal Aspect | Implications for Forensic Nursing |
|---|---|
| Informed Consent |
|
| Mandatory Reporting |
|
| Chain of Custody |
|
| Documentation Standards |
|
| Privacy and Confidentiality |
|
The forensic nurse’s documentation may become crucial evidence in legal proceedings, potentially years after the examination. Every detail must be recorded with the understanding that it may be scrutinized in court.
Medicolegal Documentation Principles
Documentation in forensic nursing serves both medical and legal purposes. Proper documentation techniques are essential for creating records that can withstand legal scrutiny while supporting patient care.
Essential Documentation Elements
- Date and time documentation began/ended
- Patient’s verbatim statements (in quotes)
- Detailed injury descriptions with measurements
- Anatomical diagrams with injury mapping
- Photographic documentation with scales
- Evidence collection details and locations
- Chain of custody documentation
- Consent processes and patient choices
- Names and roles of all individuals present
Documentation Pitfalls to Avoid
- Using subjective or conclusory language
- Diagnosing “abuse” (describe findings instead)
- Incomplete documentation of procedures
- Gaps in timeline documentation
- Illegible handwriting or inconsistent abbreviations
- Failing to document patient non-compliance
- Contradictions between written and photographic evidence
- Retrospective additions without proper notation
- Alterations to records after completion
Mnemonic: “LEGAL” – Documentation Standards
- L – Legible and logical organization of information
- E – Exact measurements and precise descriptions
- G – Graphic documentation with diagrams and photos
- A – Accurate quotations and objective observations
- L – Localized findings with anatomical specificity
Assisting Forensic Team Beyond Scope of Practice
Collaboration While Maintaining Professional Boundaries
Even when specific procedures fall outside a nurse’s scope of practice, forensic nurses play a crucial supporting role within the multidisciplinary team. Understanding the boundaries of practice while facilitating comprehensive care requires careful navigation.
Supporting Other Forensic Team Members
| Team Member | How Forensic Nurses Assist | Professional Boundaries |
|---|---|---|
| Forensic Pathologist/Medical Examiner |
|
|
| Law Enforcement |
|
|
| Legal Team/Prosecutors |
|
|
| Social Services |
|
|
| Mental Health Professionals |
|
|
Forensic nursing is fundamentally collaborative. The most effective forensic nurses recognize their scope limitations while actively facilitating the work of team members with different expertise, always keeping the patient’s wellbeing at the center.
Professional Development for Expanded Scope
Forensic nurses can expand their scope of practice through specialized education and certification, allowing them to take on more advanced forensic roles:
Advanced Certifications
- Sexual Assault Nurse Examiner (SANE-A, SANE-P)
- Advanced Forensic Nurse Examiner
- Forensic Nurse Death Investigator
- Legal Nurse Consultant
- Clinical Forensic Specialist
Expanded Competencies
- Advanced evidence collection techniques
- Specialized injury interpretation
- Expert witness testimony
- Forensic photography certification
- Advanced strangulation assessment
Victim Journey: Admission to Discharge
Comprehensive Forensic Nursing Care Across the Continuum
Forensic nursing care extends throughout the patient’s healthcare journey, from initial admission through discharge, referral, or in some cases, death. Each phase requires specific considerations to balance forensic and therapeutic needs.
Initial Admission/Triage
The forensic nurse’s responsibilities begin at first contact with the healthcare system:
- Recognizing potential forensic cases during triage
- Preserving evidence when immediate medical needs addressed
- Initiating chain of custody for clothing/items
- Coordinating appropriate examination space
- Activating forensic team response
- Addressing immediate safety concerns
- Documenting initial disclosures and observations
Forensic Assessment and Evidence Collection
Once immediate medical needs are addressed, the forensic examination proceeds:
- Obtaining informed consent for forensic procedures
- Conducting detailed forensic interview
- Performing comprehensive physical assessment
- Collecting biological and trace evidence
- Photodocumenting injuries and findings
- Maintaining continuous chain of custody
- Providing prophylactic treatments as indicated
Ongoing Care and Monitoring
For patients requiring continued medical care:
- Ensuring care providers understand forensic implications
- Documenting evolving injury patterns
- Protecting evidence during routine care
- Monitoring for additional disclosures
- Coordinating forensic follow-up needs
- Providing ongoing emotional support
- Facilitating communication with investigative team
Discharge Planning
Preparing patients for transition from healthcare setting:
- Assessing safety for discharge
- Creating detailed follow-up plan
- Providing referrals to specialized services
- Educating about legal process and expectations
- Ensuring understanding of medication and treatments
- Documenting discharge location and individuals present
- Facilitating safe transportation arrangements
Referral to Community Resources
Connecting patients with ongoing support systems:
- Making warm handoffs to community agencies
- Providing comprehensive resource lists
- Scheduling follow-up appointments
- Coordinating with victim advocates
- Ensuring understanding of safety planning
- Facilitating connection with legal resources
- Establishing communication channels for questions
Care in the Event of Death
When violence results in fatality:
- Preserving evidence postmortem
- Documenting findings before transport
- Coordinating with medical examiner/coroner
- Supporting family members
- Providing culturally sensitive end-of-life care
- Maintaining chain of custody for belongings
- Facilitating organ/tissue donation when appropriate
Forensic nurses serve as continuity providers throughout a victim’s healthcare journey, ensuring that forensic considerations are maintained even as different specialists and departments become involved in care.
Discharge Planning for Violence Victims
| Discharge Component | Standard Elements | Forensic Considerations |
|---|---|---|
| Safety Assessment |
|
|
| Follow-up Care |
|
|
| Medication Management |
|
|
| Resource Referrals |
|
|
| Documentation |
|
|
Mnemonic: “TRANSIT” – Victim Care Continuum
- T – Triage with forensic awareness
- R – Respond to immediate medical and safety needs
- A – Assess comprehensively with documentation
- N – Navigate evidence collection protocols
- S – Strengthen coping resources and support
- I – Integrate multidisciplinary team approach
- T – Transition to appropriate ongoing care
Nurse as a Witness
Responsibilities in Legal Proceedings
Forensic nurses frequently serve as witnesses in legal proceedings, presenting their observations, findings, and documentation. This role requires specific knowledge and skills to effectively contribute to the truth-seeking function of the legal system.
Types of Witness Testimony
| Fact Witness | Testifying to personal observations, actions, and documentation without offering opinions or conclusions |
| Expert Witness | Providing opinions and interpretations based on specialized nursing knowledge and expertise |
| Custodian of Records | Authenticating and explaining medical records and documentation processes |
Legal Proceedings Involving Forensic Nurses
- Criminal trials
- Preliminary hearings
- Grand jury proceedings
- Depositions
- Child protective hearings
- Protective order hearings
- Civil litigation
- Military courts-martial
- Coroner’s inquests
Preparing for Testimony
Effective testimony requires thorough preparation to ensure accurate, professional presentation of forensic nursing findings:
Pre-Testimony Preparation
- Thoroughly review all documentation and photographs
- Refresh knowledge of relevant policies and protocols
- Meet with attorneys to understand scope of testimony
- Practice explaining technical terms in layperson language
- Review chain of custody documentation
- Prepare concise explanation of credentials and experience
- Anticipate potential challenging questions
During Testimony
- Speak clearly and concisely
- Maintain professional demeanor
- Answer only what is asked
- Request clarification of questions when needed
- Avoid speculation beyond expertise
- Acknowledge limitations of knowledge
- Refer to documentation as needed
- Use visual aids effectively when permitted
- Maintain patient dignity in descriptions
Post-Testimony Responsibilities
- Document testimony experience for professional records
- Review areas for improvement in future testimony
- Update education based on identified knowledge gaps
- Provide feedback on process to improve protocols
- Participate in debriefing if emotionally challenging
- Maintain confidentiality about proceedings
Forensic nurses must remember that their role in legal proceedings is to provide objective, factual information—not to advocate for a particular outcome. Maintaining professional neutrality is essential for credibility.
Challenges in Testimony
| Challenge | Effective Strategies |
|---|---|
| Cross-examination tactics |
|
| Technical terminology barriers |
|
| Documentation gaps |
|
| Emotional management |
|
Mnemonic: “TESTIFY” – Effective Witness Guidelines
- T – Truth always, without embellishment
- E – Explanation in clear, concise language
- S – Stay within your scope of expertise
- T – Thorough preparation with documentation review
- I – Impartial presentation of findings
- F – Focus on the question asked
- Y – Yield when questions exceed your knowledge
Conclusion: The Evolving Role of Forensic Nursing
Forensic nursing represents a specialized domain where healthcare and justice intersect. As a vital bridge between medical care and legal systems, forensic nurses provide comprehensive care to victims while preserving evidence and supporting the judicial process.
The effective forensic nurse integrates physical, psychosocial, cultural, spiritual, and legal aspects of care while collaborating with a multidisciplinary team. Understanding both the scope and limitations of the role allows forensic nurses to maintain professional boundaries while facilitating comprehensive care for victims of violence.
As the field continues to evolve, forensic nursing will remain at the forefront of trauma-informed care, evidence-based practice, and patient advocacy—ensuring that victims receive compassionate care while justice is served.
Forensic nursing represents the perfect synthesis of healthcare and justice—combining the compassion of nursing with the precision of forensic science to serve society’s most vulnerable populations.
