Abnormal Fetal Presentations: A Comprehensive Guide for Nursing Students
1. Introduction
Abnormal fetal presentations occur in approximately 3-4% of all pregnancies at term. They represent significant challenges in obstetric care and can lead to increased maternal and fetal morbidity and mortality if not managed appropriately. Understanding these presentations is vital for nursing students and healthcare providers to ensure optimal outcomes during labor and delivery.
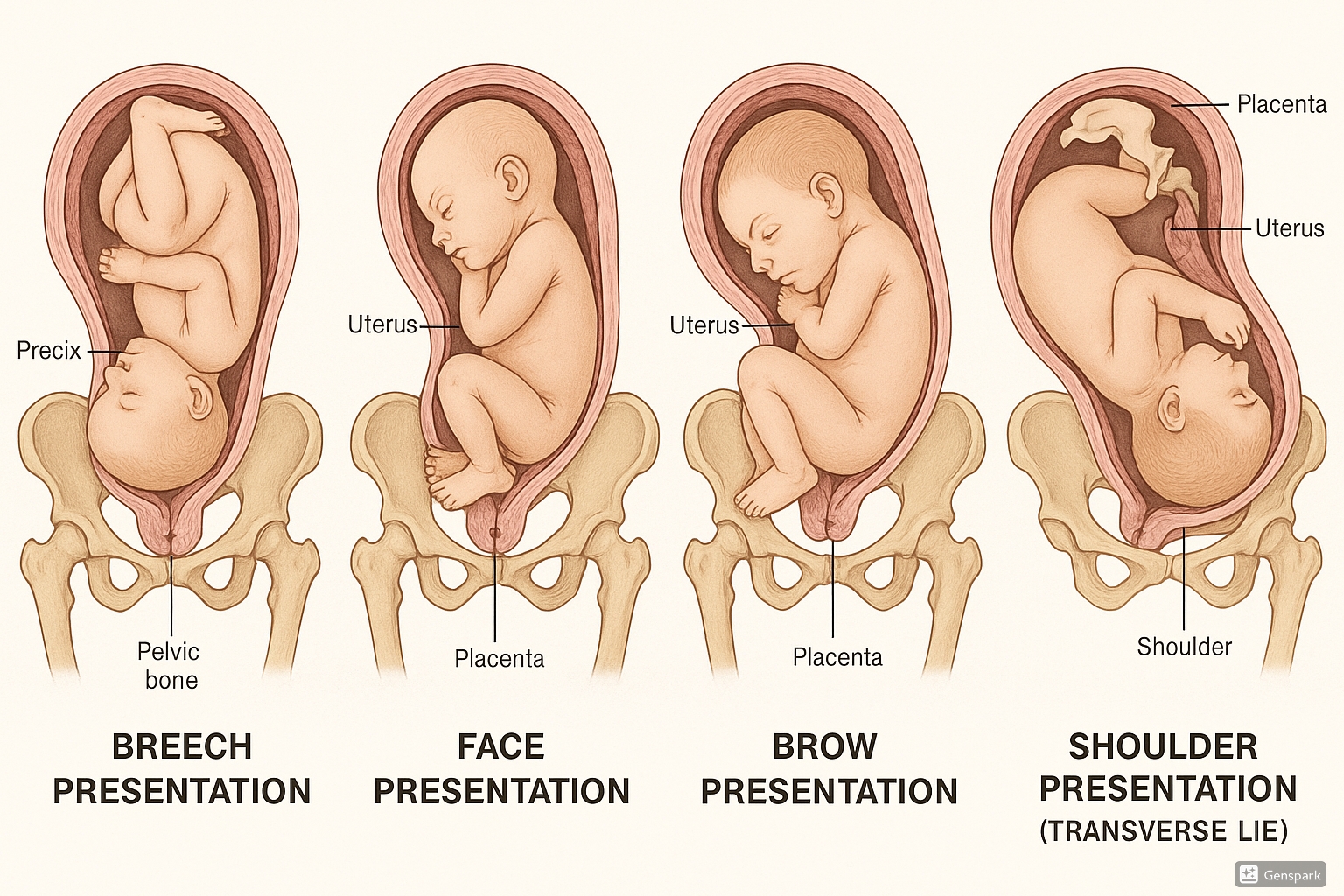
Figure 1: Various types of abnormal fetal presentations: breech, face, brow, and shoulder (transverse lie)
2. Normal vs. Abnormal Fetal Presentations
| Type | Description | Incidence | Primary Concern |
|---|---|---|---|
| Vertex (Normal) | Head-down with chin tucked to chest | 96-97% at term | Standard delivery approach |
| Breech | Buttocks or feet presenting first | 3-4% at term | Risk of cord prolapse, head entrapment |
| Face | Face presenting due to hyperextended neck | 0.2% (1:600 deliveries) | Potential for obstructed labor |
| Brow | Forehead presenting with partially extended neck | 0.01-0.1% (1:500-1:4000) | Largest presenting diameter, often impossible for vaginal delivery |
| Shoulder/Transverse | Fetus lying horizontally across uterus | 0.3% at term | Vaginal birth physically impossible, obstetric emergency |
V – Vertex is the normal presentation (head down, chin to chest)
E – Efficiency of the birth canal is maximized with vertex position
R – Rotation is natural during a vertex delivery
T – The smallest diameter (suboccipitobregmatic, 9.5 cm) presents first
E – Exit through the birth canal is smoothest with vertex
X – eXpect this position in 96-97% of pregnancies
3. Breech Presentation
Breech presentations account for approximately 3-4% of all pregnancies at term. While 20% of fetuses are in breech position at 28 weeks, most revert to cephalic presentation spontaneously, leaving only 3% breech at term.
3.1 Types of Breech Presentation
Both legs are flexed at the hips and knees (baby appears to be sitting “cross-legged”).
Both legs are flexed at the hips and extended at the knees. Most common type (65-70% of breech presentations).
One or both legs extended at the hip, with feet or foot as the presenting part. Has highest risk of cord prolapse.
3.2 Risk Factors
| Maternal Factors | Fetal Factors |
|---|---|
| Multiparity | Prematurity |
| Uterine anomalies (septate uterus) | Macrosomia |
| Uterine fibroids | Polyhydramnios |
| Placenta previa | Multiple pregnancy |
| Previous breech delivery | Fetal abnormalities (e.g., anencephaly) |
| Contracted pelvis | Fetal neurological disorders |
3.3 Diagnosis & Assessment
- Abdominal palpation (Leopold’s maneuvers): Hard, round fetal head palpated in upper part of uterus; irregular buttocks in pelvis
- Fetal heart sounds auscultated higher on maternal abdomen than expected
- Vaginal examination may reveal soft, irregular presenting part (buttocks) or foot
- Meconium-stained liquor may be present (common in breech deliveries and not always indicative of fetal distress)
Confirmation of breech presentation is typically done through ultrasound, which can identify the type of breech and detect any fetal or uterine abnormalities that may predispose to breech presentation.
3.4 Management & Nursing Care
External Cephalic Version (ECV)
Procedure to manually turn the fetus to a cephalic presentation through the maternal abdomen, typically performed at 37 weeks.
- Pre-procedure assessment:
- Confirm gestational age and breech presentation via ultrasound
- Perform non-stress test to ensure fetal well-being
- Check for contraindications (placenta previa, uterine anomaly, multiple pregnancy, etc.)
- Procedure preparation:
- Explain procedure and obtain informed consent
- Administer tocolytic agent if ordered (e.g., terbutaline) to relax uterus
- Position patient comfortably, empty bladder
- Ensure continuous fetal monitoring
- Post-procedure care:
- Continue fetal monitoring for at least 30 minutes
- Monitor for complications (vaginal bleeding, SROM, contractions)
- Administer RhIG if mother is Rh-negative
- Educate about signs of labor or decreased fetal movement
Cesarean Section
Current guidelines generally recommend planned cesarean delivery for breech presentations at term, particularly for primigravid women, based on evidence of reduced perinatal morbidity and mortality compared to vaginal breech birth.
Vaginal Breech Birth
May be considered in specific circumstances with experienced providers and careful patient selection.
B – Be alert for cord prolapse
R – Recognize type of breech (frank, complete, footling)
E – External cephalic version is first-line treatment
E – Evaluate for cesarean section candidacy
C – Continuous fetal monitoring during labor
H – Have resuscitation equipment ready
3.5 Complications
- Umbilical cord prolapse: 1% risk in breech vs. 0.5% in vertex
- Head entrapment: Fetal body delivers but head becomes trapped
- Premature rupture of membranes
- Birth asphyxia: Secondary to delay in delivery
- Intracranial hemorrhage: From rapid compression of head during delivery
- Brachial plexus injuries: Due to maneuvers during delivery
4. Face Presentation
Face presentation is rare, occurring in approximately 1 in 600 deliveries (0.2%). In this presentation, the mentum (chin) is the denominator, meaning the position is described by the location of the chin relative to the maternal pelvis.
4.1 Etiology & Risk Factors
Face presentation results from extension of the fetal neck instead of the normal flexion. Multiple factors can contribute:
| Maternal Factors | Fetal Factors |
|---|---|
| Contracted maternal pelvis | Anencephaly |
| Platypelloid pelvis | Multiple loops of umbilical cord around the neck |
| Multiparity | Neck masses (goiter, cystic hygroma) |
| Previous cesarean delivery | Macrosomia |
| Polyhydramnios | Fetal hyperextension |
F – Fetal abnormalities (anencephaly)
A – Abundance of amniotic fluid (polyhydramnios)
C – Cephalopelvic disproportion
E – Extended neck (cord around neck)
S – Small maternal pelvis
4.2 Diagnosis & Assessment
Face presentation is typically diagnosed during the second stage of labor via vaginal examination. It can be challenging to diagnose and may sometimes be misidentified as breech.
- On vaginal examination:
- Ability to palpate orbital ridges, nose, malar eminences, mouth, and chin
- Important to identify position of mentum (chin) – anterior, posterior, or transverse
- Abdominal palpation:
- Deep groove felt between occiput and back
- Cephalic prominence on same side as small parts
- Ultrasound confirmation:
- Shows hyperextended fetal neck
- Chin separated from chest
4.3 Management & Nursing Care
Management depends primarily on the position of the mentum (chin):
| Mentum Position | Management | Rationale |
|---|---|---|
| Mentum Anterior | Trial of vaginal delivery may be attempted | Chin can rotate under symphysis pubis, allowing delivery by flexion |
| Mentum Posterior | Cesarean delivery recommended | Birth canal obstruction prevents vaginal delivery, as the face cannot extend further |
| Mentum Transverse | Expectant management with close monitoring | May rotate to anterior or posterior position; if posterior, cesarean indicated |
- Continuous electronic fetal monitoring:
- Heart rate abnormalities are common in face presentations
- Use external transducers to avoid trauma to fetal face/eyes
- If internal monitoring necessary, place on bony parts
- Labor management:
- Anticipate longer labor duration due to larger presenting diameters
- Position mother to optimize fetal descent
- Provide emotional support – abnormal presentations increase maternal anxiety
- Preparation for potential cesarean delivery:
- Maintain NPO status
- Have IV access established
- Complete pre-op documentation
- Neonatal care preparation:
- Alert neonatal team of face presentation
- Prepare for potential facial edema, trauma, or respiratory distress
- Have resuscitation equipment ready
4.4 Complications
- Prolonged labor: Due to larger presenting diameter
- Fetal distress: Heart rate abnormalities common
- Facial edema and trauma: Pressure and mechanical forces during labor
- Airway obstruction: From facial swelling
- Increased cesarean delivery rates
- Higher NICU admission rates
5. Brow Presentation
Brow presentation is considered the rarest form of malpresentation, with an incidence of 1 in 500 to 1 in 4000 deliveries. In this presentation, the largest diameter of the fetal head (occipitomental, 13.5 cm) presents to the maternal pelvis, making vaginal delivery extremely difficult or impossible.
5.1 Etiology & Risk Factors
Risk factors are similar to those for face presentation but may include:
- Cephalopelvic disproportion
- Multiparity with pendulous abdomen
- Fetal anomalies
- Placenta previa
- Preterm fetus
- Multiple gestation
- Polyhydramnios
- Previous cesarean section
5.2 Diagnosis & Assessment
- On vaginal examination:
- Anterior fontanelle and orbital ridges palpable
- Mouth and chin not palpable (distinguishing from face presentation)
- Posterior fontanelle not palpable (distinguishing from vertex presentation)
- Abdominal examination:
- Head high and difficult to engage
- Less pronounced groove between head and back than face presentation
- Progress assessment:
- Presenting part slow to descend
- Prolonged labor often evident
The diagnosis is typically not made until after the membranes have ruptured and the head has begun to engage in a fixed presentation. Many brow presentations will spontaneously convert to either vertex or face presentation during labor.
B – Between fontanelle and orbital ridges
R – Root of nose palpable
O – Occipitomental diameter presents (largest fetal diameter at 13.5 cm)
W – Watch for conversion to face or vertex
5.3 Management & Nursing Care
Persistent brow presentation generally requires a cesarean section, as the larger cephalic diameter prevents engagement in the pelvis for vaginal delivery unless the fetus is very small or the maternal pelvis is exceptionally large.
- Ongoing assessment:
- Monitor for spontaneous conversion to face or vertex
- Continuous electronic fetal monitoring
- Frequent vaginal examinations to assess for changes in presentation
- Cesarean preparation:
- Inform the patient about the need for likely cesarean section
- Complete pre-operative documentation and preparation
- Support during preparation for surgery
- Psychological support:
- Address anxiety and fears related to change in birth plan
- Provide clear information about the reason for cesarean delivery
- Involve support person in care decisions when possible
5.4 Complications
- Obstructed labor: Due to the unfavorably large presenting diameter
- Increased risk of uterine rupture if obstruction is undetected
- Maternal exhaustion from prolonged labor
- Fetal distress: From prolonged labor and head compression
- Birth trauma: If vaginal delivery is attempted
- Facial and forehead edema in the newborn
6. Shoulder Presentation (Transverse Lie)
Transverse lie occurs in approximately 0.3% of term pregnancies. This presentation constitutes an absolute feto-pelvic disproportion, making vaginal delivery physically impossible. It is an obstetric emergency due to the risk of obstructed labor, uterine rupture, and fetal distress.
6.1 Etiology & Risk Factors
- Grand multiparity: 5 deliveries or more
- Uterine anomalies: Septate or bicornuate uterus
- Placenta previa
- Multiple pregnancy
- Prematurity
- Polyhydramnios
- Uterine fibroids or pelvic masses
- Prior cesarean section
- Fetal anomalies
6.2 Diagnosis & Assessment
- Abdominal examination:
- Uterus appears unusually wide: transverse axis nearly equivalent to longitudinal axis
- Fundal height less than expected for gestational age (often under 30 cm at term)
- Fetal head palpable in one flank, breech in the other
- Vaginal examination:
- Empty true pelvis or shoulder palpable
- Sometimes arm prolapsing from vagina in neglected cases
- Ultrasound confirmation:
- Fetal spine oriented perpendicularly to maternal spine
- Can identify specific variety (dorso-anterior, dorso-posterior)
T – Transversely positioned fetus
R – Round abdomen (wider than usual)
A – Abnormally low fundal height for gestation
N – No presenting part in pelvis
S – Shoulder may be palpable on vaginal exam
V – Vacuum delivery contraindicated
E – Empty pelvis on examination
R – Requires cesarean delivery
S – Side-to-side fetal poles on examination
E – Emergency if in active labor
6.3 Management & Nursing Care
This presentation should ideally be diagnosed before labor begins. Management depends on gestational age, labor status, and fetal viability:
| Clinical Situation | Management |
|---|---|
| Before labor, fetus alive |
|
| In labor, membranes intact |
|
| In labor, membranes ruptured |
|
| Fetus dead |
|
- Emergency preparation:
- Recognize this as an obstetric emergency requiring immediate intervention
- Place two large-bore IV lines for potential rapid fluid administration
- Prepare for emergency cesarean delivery
- Monitor maternal vital signs frequently
- Fetal monitoring:
- Continuous electronic fetal monitoring if possible
- Be vigilant for signs of fetal compromise
- Preventive care:
- If recognized before labor, help coordinate appropriate follow-up
- Educate about the importance of birth planning in this high-risk situation
- Positioning:
- If in a remote setting without immediate surgical capability, position in Trendelenburg or knee-chest to prevent cord prolapse
6.4 Complications
- Obstructed labor: Inevitable if vaginal delivery attempted
- Uterine rupture: High risk if obstruction not relieved
- Cord prolapse: Increased risk with rupture of membranes
- Maternal hemorrhage
- Fetal distress and death if not delivered promptly
- Arm prolapse in neglected cases
7. Best Practices in Abnormal Fetal Presentations
All pregnant women should undergo presentation assessment by 36 weeks gestation. Early identification of abnormal presentations allows time for version attempts and birth planning.
Current guidelines recommend routine ultrasound examination at 35-36 weeks, which can substantially reduce the risk of unexpected abnormal presentation during labor.
Current evidence supports offering external cephalic version to all eligible women with breech presentation at term (>37 weeks). Recent studies show improved success rates with tocolytics and regional anesthesia.
The procedure should be performed in facilities equipped to handle emergency cesarean delivery, as approximately 0.5% of ECVs result in complications requiring emergency intervention.
The 2024 ACOG guidelines emphasize shared decision-making regarding delivery options. Women should receive comprehensive counseling about risks and benefits of cesarean versus vaginal delivery for abnormal presentations.
When vaginal breech birth is considered, this should include discussion of increased perinatal risks (1-2% risk of serious complications) and availability of skilled providers.
8. Critical Nursing Considerations
- Provide clear explanations of the abnormal presentation and its implications
- Address anxiety related to changes in birth plan if cesarean becomes necessary
- Ensure continuous support during labor, especially if attempting vaginal birth with breech or face presentation
- Position mother optimally based on specific presentation
- Monitor for signs of maternal exhaustion in prolonged labor
- Use continuous electronic fetal monitoring for all abnormal presentations
- Be vigilant for decelerations that may indicate cord compression
- For face presentations, use external transducers when possible to avoid facial trauma
- Document presenting part and position regularly during labor
- Establish reliable IV access early
- Ensure operating room readiness for potential cesarean delivery
- Have neonatal resuscitation equipment and personnel available
- Document all interventions, fetal responses, and maternal vital signs meticulously
- Assess newborn for trauma or edema related to presentation
- Monitor for respiratory complications, especially in face and brow presentations
- Provide extra support for breastfeeding if facial edema is present
- Assist with post-cesarean recovery if surgical delivery was required
- Address potential maternal feelings of disappointment if desired birth plan changed
9. Recent Updates in Management
- ACOG Practice Bulletin (2024): Recommends ultrasound screening at 36 weeks for all primigravid women to detect undiagnosed breech presentations.
- New ECV Protocols: Recent studies indicate higher success rates when ECV is performed with neuraxial analgesia (epidural or spinal), with success rates improving from 40% to over 60%.
- Breech Birth Revival: Select medical centers are reintroducing vaginal breech birth programs with strict selection criteria and specialized provider training, particularly for frank breech presentations.
- Preventing Malpositions: Increased emphasis on maternal positioning and mobility during labor to prevent or correct malpositions, with specific maternal positions shown to facilitate optimal fetal positioning.
- Interprofessional Simulation Training: Increased implementation of team-based simulation training for rare presentations (face, brow, compound) to maintain provider skills for these uncommon but critical situations.
10. References
- TeachMeObGyn. (2023). Breech Presentation. https://teachmeobgyn.com/pregnancy/fetal-abnormality/breech-presentation/
- StatPearls. (2024). Delivery, Face and Brow Presentation. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK567727/
- MSF Medical Guidelines. (2023). Transverse lie and shoulder presentation. https://medicalguidelines.msf.org/en/viewport/ONC/english/7-6-transverse-lie-and-shoulder-presentation-51417541.html
- MSF Medical Guidelines. (2023). Brow presentation. https://medicalguidelines.msf.org/en/viewport/ONC/english/7-10-brow-presentation-51417609.html
- ACOG. (2024). First and Second Stage Labor Management. https://www.acog.org/clinical/clinical-guidance/clinical-practice-guideline/articles/2024/01/first-and-second-stage-labor-management
- Bellussi, F., Ghi, T., Youssef, A., et al. (2017). The use of intrapartum ultrasound to diagnose malpositions and cephalic malpresentations. American Journal of Obstetrics and Gynecology, 217(6), 633-641.
- Ducarme, G., Ceccaldi, P.F., Chesnoy, V., et al. (2006). Face presentation: retrospective study of 32 cases at term. Gynecologie, Obstetrique & Fertilite, 34(5), 393-396.
- Safer Care Victoria. (2023). Breech presentation: diagnosis and management. https://www.safercare.vic.gov.au/best-practice-improvement/clinical-guidance/maternity/breech-presentation-diagnosis-and-management
- Zhang, Y., Fu, T., Chen, L., et al. (2024). Face presentation at term: incidence, risk factors and influence on maternal and neonatal outcomes. Archives of Gynecology and Obstetrics, 310(2), 923-931.
