Alternative Birthing Positions: Women’s Preferred Choices in Third Trimester
Comprehensive guide for nursing students on evidence-based birthing position options
Table of Contents
- 1. Introduction to Birthing Positions
- 2. Physiological Benefits of Alternative Birthing Positions
- 3. Types of Alternative Birthing Positions
- 4. Assessment and Selection of Appropriate Positions
- 5. Maternal Benefits and Outcomes
- 6. Fetal Benefits and Outcomes
- 7. Cultural Considerations in Birthing Positions
- 8. Nursing Role in Supporting Alternative Positions
- 9. Helpful Mnemonics for Birthing Positions
- 10. Evidence-Based Practices and Research
- 11. Case Studies and Scenarios
- 12. Global Practices in Birthing Positions
- 13. References and Resources
1. Introduction to Birthing Positions
Throughout history, women have intuitively used various birthing positions during labor and delivery. The traditional supine or lithotomy position became standardized in Western medicine primarily for provider convenience rather than maternal benefit. Today, evidence supports that alternative birthing positions offer numerous advantages for both mother and baby during the third trimester and labor process.
Modern maternity care increasingly recognizes the importance of offering women choices in birthing positions that support physiological birth processes. These positions work with gravity, optimize pelvic dimensions, improve fetal descent, and enhance maternal comfort and control during labor.
Key Concepts in Alternative Birthing Positions
- Gravity-assisted positions promote fetal descent
- Upright positions can increase pelvic diameters by up to 30%
- Movement between positions helps manage discomfort
- Position changes may improve fetal positioning
- Women who use alternative positions report greater satisfaction with birth experience
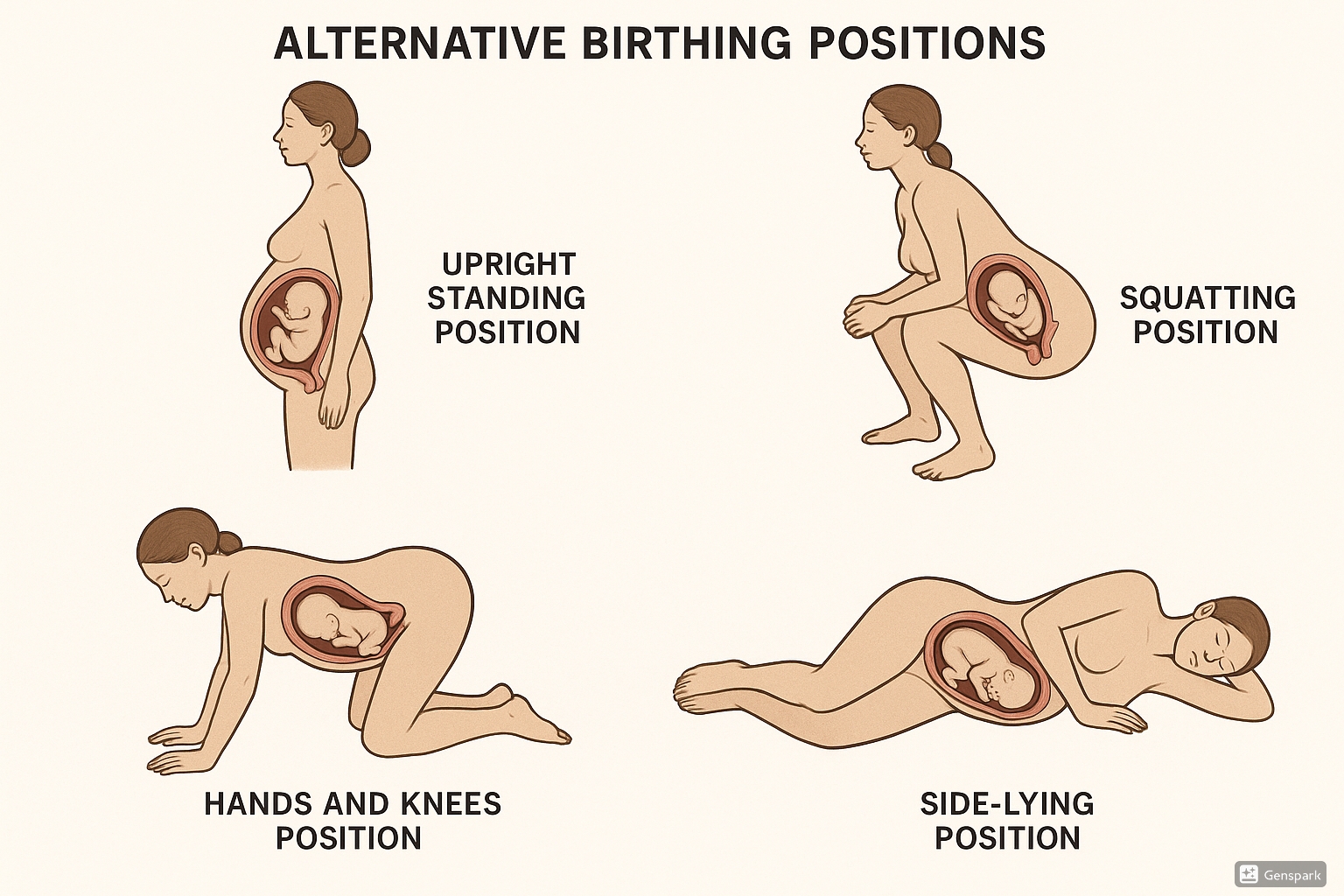
Figure 1: Illustration of common alternative birthing positions used during labor
2. Physiological Benefits of Alternative Birthing Positions
Understanding the physiological advantages of various birthing positions helps nursing professionals provide evidence-based guidance to women in the third trimester. Different positions affect pelvic dimensions, oxygen flow, muscular efficiency, and gravitational assistance during labor.
Pelvic Dynamics in Different Positions
The pelvis is not a fixed structure but can change dimensions based on position:
| Pelvic Measurement | Effect in Upright Positions | Effect in Supine Position |
|---|---|---|
| Pelvic Outlet Diameter | Increases by 20-30% | Reduced by pressure of sacrum |
| Anteroposterior Diameter | Increases by 0.5-2cm | May be compromised |
| Sacral Mobility | Enhanced, allowing “give” during descent | Limited by pressure against surface |
| Pelvic Floor Tension | Optimally balanced | Potential increased tension |
Cardiovascular Effects
- Upright birthing positions prevent aortocaval compression
- Improved venous return from lower extremities
- Enhanced cardiac output by 10-15%
- Reduced risk of maternal hypotension
- Better placental perfusion and fetal oxygenation
Respiratory Benefits
- Increased lung capacity in vertical positions
- Reduced pressure on diaphragm
- Improved oxygen exchange
- Enhanced energy availability for labor
- Lower perceived exertion during contractions
Research Highlight:
Studies show that women who labor in alternative birthing positions experience average labor duration reductions of up to 25% compared to those limited to supine positioning (Lawrence et al., 2013).
3. Types of Alternative Birthing Positions
Each birthing position offers unique benefits and may be more suitable at different stages of labor. Women should be encouraged to try various positions and find what feels most comfortable and effective for their individual needs.
3.1 Standing/Upright Positions
Standing and other upright birthing positions utilize gravity to assist fetal descent through the birth canal. These positions are particularly helpful during early and active labor phases.
Benefits:
- Maximizes gravitational assistance
- Increases pelvic outlet dimensions
- Improves alignment of fetus with pelvis
- Enhances efficiency of contractions
- Reduces back pain
Considerations:
- May be tiring over prolonged periods
- Requires sufficient strength and balance
- May be challenging with epidural anesthesia
- Requires support person or structure
Nursing Implementation:
- Offer support for balance (partner, bar, or birth ball)
- Encourage rocking and swaying movements
- Monitor for signs of fatigue
- Provide alternating options for rest
- Ensure adequate hydration
3.2 Squatting Positions
Squatting is one of the most effective birthing positions for maximizing pelvic outlet dimensions. It can increase the pelvic outlet by up to 28% compared to the supine position.
Benefits:
- Maximum pelvic outlet expansion
- Optimal use of gravity
- Strong pushing leverage
- Reduced need for episiotomy
- May shorten second stage of labor
Considerations:
- Physically demanding
- Difficult to maintain for extended periods
- May increase perineal pressure
- Not suitable with most epidurals
Nursing Implementation:
- Utilize squat bar or partner support
- Consider supported squatting with birth stool
- Encourage practice during pregnancy
- Alternate with rest positions
- Monitor perineal tissues for excessive edema
3.3 Hands and Knees Position
The hands and knees position (all-fours) is particularly beneficial for relieving back pain and facilitating rotation of posterior-positioned babies. This birthing position also reduces pressure on the maternal abdomen.
Benefits:
- Excellent for back pain relief
- Facilitates fetal rotation from posterior position
- Reduces pressure on hemorrhoids
- Allows pelvic rocking for comfort
- Provides good access for back massage
Considerations:
- May cause wrist and knee discomfort
- Requires adequate padding for joints
- Limited eye contact with care providers
- More difficult for electronic fetal monitoring
Nursing Implementation:
- Provide adequate cushioning for knees and hands
- Teach pelvic rocking techniques
- Facilitate partner involvement for back massage
- Monitor fetal heart tones with portable devices
- Suggest position variations (leaning on birth ball)
3.4 Side-Lying Position
Side-lying is an excellent resting birthing position that still offers some of the benefits of upright positions while allowing the mother to conserve energy. It’s also one of the most compatible positions with epidural anesthesia.
Benefits:
- Reduces perineal pressure and tearing
- Maintains good placental perfusion
- Compatible with epidural anesthesia
- Allows rest between contractions
- Prevents aortocaval compression
Considerations:
- Less gravitational assistance
- May require additional support for leg positioning
- Can cause hip discomfort without proper support
- Potential uneven pressure on perineum
Nursing Implementation:
- Provide pillows between knees and under upper arm
- Alternate sides periodically
- Position upper leg with support to open pelvis
- Monitor for pressure points on ears and shoulders
- Consider combining with peanut ball for pelvic opening
3.5 Birthing Ball Positions
Birthing balls provide versatile support for various birthing positions. They allow movement, pelvic rocking, and bouncing that can enhance comfort and labor progress.
Benefits:
- Promotes optimal fetal positioning
- Encourages pelvic mobility
- Provides comfort through gentle movement
- Supports upright posture with less fatigue
- Can be used in multiple positions (sitting, leaning)
Considerations:
- Requires proper ball size for height
- Potential safety concerns without supervision
- Limited stability for some women
- May not be suitable with ruptured membranes
Nursing Implementation:
- Ensure proper inflation and size
- Teach safe techniques for mounting/dismounting
- Demonstrate various positions (sitting, kneeling over)
- Provide supervision for safety
- Clean ball between patients according to protocol
3.6 Water Birth Positions
Immersion in water offers unique advantages for laboring women, with multiple birthing positions possible within the birthing tub or pool.
Benefits:
- Buoyancy reduces pressure on joints
- Facilitates easier position changes
- Potential pain reduction through hydrotherapy
- Supports perineal tissues during stretching
- May reduce need for pharmacological pain relief
Considerations:
- Limited availability in some facilities
- Specific safety protocols required
- Temperature regulation is critical
- May complicate continuous monitoring
- Not suitable for all high-risk situations
Nursing Implementation:
- Maintain water temperature between 97-99°F (36.1-37.2°C)
- Use waterproof Doppler for intermittent monitoring
- Ensure privacy and maintain dignity
- Have extraction plan in case of emergency
- Follow facility protocol for water birth procedures
4. Assessment and Selection of Appropriate Positions
Selecting appropriate birthing positions requires comprehensive assessment of multiple factors. Nurses play a crucial role in guiding women toward positions that address their specific needs while considering safety and physiological benefits.
Assessment Factors for Position Selection
| Assessment Category | Key Considerations | Recommended Positions |
|---|---|---|
| Fetal Position |
|
|
| Labor Progress |
|
|
| Pain Location |
|
|
| Anesthesia Status |
|
|
| Maternal Conditions |
|
|
Assessment Tool: P.O.S.I.T.I.O.N.S
Use this mnemonic for comprehensive assessment before recommending birthing positions:
P: Progress of labor and stage
O: Obstetric history and risk factors
S: Signs of fetal position and presentation
I: Intensity and location of discomfort
T: Treatment interventions in place (IV, monitoring)
I: Individual preferences and cultural factors
O: Obstacles (physical limitations, obesity)
N: Nurturing environment and support persons
S: Stamina and energy levels
5. Maternal Benefits and Outcomes
Research demonstrates significant maternal benefits from utilizing alternative birthing positions during labor and delivery. These benefits extend beyond comfort to include measurable clinical outcomes.
Physiological Benefits
- Reduced labor duration by average of 1-2 hours
- Decreased perception of pain intensity
- Lower rates of instrumental delivery (20-30% reduction)
- Fewer episiotomies (up to 25% reduction)
- Improved maternal blood pressure stability
- More effective contractions with less fatigue
- Lower rates of perineal trauma
Psychological Benefits
- Enhanced sense of control during birth process
- Improved satisfaction with birth experience
- Reduced anxiety and fear
- Increased confidence in body’s abilities
- Greater feeling of active participation
- More positive birth memories
- Potential reductions in postpartum depression risk
Research Highlight:
A systematic review of 25 studies (Gupta et al., 2017) found that women using upright birthing positions experienced:
- 25% reduction in assisted deliveries
- 54% reduction in episiotomy rates
- Shorter second stage of labor (mean difference of 6.16 minutes)
- Lower reported pain scores and higher satisfaction
6. Fetal Benefits and Outcomes
Alternative birthing positions offer significant advantages for the fetus during labor and delivery, optimizing blood flow, oxygen delivery, and the mechanics of birth.
Fetal Advantages of Alternative Positions
| Benefit Category | Description | Optimal Positions |
|---|---|---|
| Oxygenation | Improved placental perfusion and oxygen transfer due to reduced compression of maternal blood vessels | Side-lying, upright, hands and knees |
| Fetal Alignment | Better alignment of fetal head with pelvic inlet and through birth canal | Upright positions, squatting, lunging |
| Fetal Rotation | Facilitation of internal rotation from unfavorable positions | Hands and knees, asymmetric positions |
| Fetal Heart Rate | More stable FHR patterns with fewer decelerations | Side-lying, hands and knees |
| Cord Compression | Reduced risk of cord compression | Hands and knees, side-lying |
Clinical Note:
When fetal heart rate abnormalities occur during labor, changing the mother’s position is often the first intervention. Position changes can resolve up to 40% of non-reassuring fetal heart rate patterns by improving placental perfusion and relieving cord compression.
Research indicates that neonates born to mothers who utilized alternative birthing positions may have:
- Higher Apgar scores at 5 minutes
- Lower rates of NICU admission
- Reduced birth trauma (such as shoulder dystocia)
- Fewer cases of meconium aspiration
7. Cultural Considerations in Birthing Positions
Cultural traditions and beliefs significantly influence women’s preferences for birthing positions. Understanding and respecting these cultural perspectives enhances patient-centered care and improves birth experiences.
Cultural Traditions in Birthing Positions
| Cultural Background | Traditional Birthing Positions | Cultural Context | Nursing Considerations |
|---|---|---|---|
| Traditional African | Sitting on low stools, squatting with support | Female relatives provide support; birthing as community event | Incorporate support persons; offer low seating options |
| Native American | Kneeling, semi-sitting, tree-hanging positions | Connection to earth; presence of female elders | Allow for vertical positions; incorporate traditional supporters |
| Latin American | Hammock-supported positions, kneeling | Strong family involvement; traditional midwifery practices | Support family presence; provide fabric supports |
| Asian (various) | Squatting, kneeling, side-lying | Balance of elements; privacy concerns; avoidance of cold | Maintain warmth; provide privacy screens; offer squatting supports |
| Middle Eastern | Kneeling, supported standing | Gender considerations; modest coverage important | Same-gender providers when possible; ensure proper draping |
Cultural Humility in Supporting Birthing Positions
The nursing approach to cultural considerations in birthing positions should include:
- Asking women about cultural preferences during prenatal education
- Including cultural considerations in birth plans
- Avoiding assumptions based on cultural background
- Adapting hospital environments to accommodate traditional positions
- Supporting the integration of cultural practices with evidence-based care
- Documenting preferences and ensuring communication among team members
8. Nursing Role in Supporting Alternative Positions
Nurses play a pivotal role in educating, supporting, and advocating for women who wish to use alternative birthing positions. Effective nursing interventions can significantly enhance the success of these positions.
Prenatal Education
- Provide information on birthing position options during prenatal classes
- Demonstrate positions and practice techniques
- Discuss benefits and considerations of each position
- Address partner/support person role in maintaining positions
- Incorporate positions into birth plan discussions
- Offer resources for home practice
Intrapartum Support
- Assess mother’s preferences and limitations
- Suggest birthing positions appropriate to labor stage
- Provide physical support during position changes
- Adapt monitoring techniques to maintain positions
- Document effectiveness of various positions
- Coach breathing and relaxation specific to each position
Nursing Interventions by Labor Stage
| Labor Stage | Recommended Positions | Nursing Support Actions |
|---|---|---|
| Early First Stage (Latent) | Walking, standing, sitting on birth ball |
|
| Active First Stage | Upright positions, hands and knees, standing lean |
|
| Transition | Side-lying, supported squatting, leaning |
|
| Second Stage (Pushing) | Squatting, semi-sitting, hands and knees |
|
| With Epidural | Side-lying, supported sitting, modified positions |
|
Safety Considerations
When supporting women in alternative birthing positions, nurses must:
- Ensure adequate staff support for position changes
- Monitor maternal fatigue and suggest position rotation
- Maintain continuous fetal monitoring when indicated
- Have emergency procedures in place for rapid position change if needed
- Document positions used and maternal/fetal responses
9. Helpful Mnemonics for Birthing Positions
Mnemonics help nursing students remember key concepts about birthing positions and their applications in clinical practice.
M.O.V.E.M.E.N.T
For benefits of alternative birthing positions:
M: Maximizes gravitational assistance
O: Optimizes pelvic dimensions
V: Vascular circulation improved
E: Enhances contraction efficiency
M: Maternal comfort and control
E: Expedites fetal descent
N: Naturally aligns fetal position
T: Trauma to perineum reduced
P.O.S.I.T.I.O.N
For matching positions to labor needs:
P: Pain location determines best position
O: Occiput posterior? Try hands and knees
S: Second stage uses squatting/upright positions
I: Individualize based on woman’s comfort
T: Transition stage benefits from supported positions
I: Interval rest in side-lying between contractions
O: Optimize with props and supports
N: Never restrict movement unnecessarily
U.P.R.I.G.H.T
For physiological benefits of upright birthing positions:
U: Utilizes gravity for easier descent
P: Pelvic diameter increased significantly
R: Respiratory function enhanced
I: Improves contraction efficiency
G: Greater maternal sense of control
H: Helps align fetus with birth canal
T: Tissue trauma rates reduced
10. Evidence-Based Practices and Research
Contemporary research provides strong evidence supporting the use of alternative birthing positions in modern maternity care. Understanding this evidence helps nurses advocate for position options based on science.
Key Research Findings
| Research Focus | Key Findings | Clinical Implications |
|---|---|---|
| Labor Duration |
|
|
| Perineal Outcomes |
|
|
| Pain Management |
|
|
| Maternal Satisfaction |
|
|
| Instrumental Delivery |
|
|
Research Spotlight:
The Cochrane Review by Lawrence et al. (2013) examined 25 trials (5,218 women) and found that women who used upright birthing positions experienced:
- First stage of labor shortened by approximately 1.36 hours
- 29% reduction in epidural rate
- Significantly higher satisfaction scores
- No adverse effects for mother or baby
This research supports offering women choices in positioning throughout labor and delivery as a standard of care.
11. Case Studies and Scenarios
Case studies help nursing students apply knowledge about birthing positions to clinical scenarios they may encounter in practice.
Case Study 1: Occiput Posterior Position
Scenario: Maria, a 28-year-old G1P0, is at 6cm dilation. She reports intense back pain, and vaginal exam reveals the fetus is in occiput posterior position. Contractions are regular but progress has slowed in the last 2 hours.
Recommended Birthing Positions:
- Hands and knees position
- Lunging with one foot elevated
- Asymmetrical standing with one foot elevated
- Side-lying with upper leg supported high
Nursing Interventions:
- Educate about OP position and potential resolution
- Suggest position rotation every 30 minutes
- Apply counterpressure during contractions
- Encourage pelvic rocking in hands-knees position
- Document fetal position changes and response to interventions
Outcome: After 90 minutes of position changes focusing on hands and knees and asymmetric standing, the fetus rotated to occiput anterior. Maria’s back pain decreased significantly, and labor progressed to complete dilation within 2 hours.
Case Study 2: Labor with Epidural
Scenario: Jasmine, a 31-year-old G2P1, has received an epidural at 5cm dilation. She has good pain relief but limited lower extremity mobility. Labor has been progressing slowly over the past 3 hours with minimal cervical change.
Recommended Birthing Positions:
- Side-lying with peanut ball
- Alternating side-lying (30-60 minute intervals)
- Modified supported sitting with leg support
- Supported semi-prone position
Nursing Interventions:
- Assist with position changes every 30-45 minutes
- Use pillows/peanut ball to maintain optimal pelvic opening
- Monitor pressure points and skin integrity
- Educate about importance of position changes despite epidural
- Document effectiveness of positions on labor progress
Outcome: With regular position changes including extended periods with the peanut ball between her knees in side-lying position, Jasmine progressed to complete dilation over the next 4 hours and delivered vaginally in supported semi-sitting position.
Case Study 3: Cultural Preferences in Birthing
Scenario: Amina, a 26-year-old G1P0 from Somalia, is admitted in active labor at 7cm dilation. Her birth plan indicates she wishes to deliver in a squatting position as per her cultural tradition. She has her mother and sister as support persons.
Recommended Birthing Positions:
- Supported deep squat during second stage
- Modified squatting with birth bar
- Birthing stool option
- Standing with deep knee bends during contractions
Nursing Interventions:
- Integrate family support persons into position support
- Prepare squatting supplies and equipment in advance
- Practice squatting position before second stage
- Discuss adaptations with provider team
- Ensure privacy and cultural sensitivity
Outcome: A birthing bar was installed, and family members were positioned to support Amina. She successfully delivered in a deep squat with minimal perineal trauma. She expressed high satisfaction with her birth experience and appreciation for the accommodation of her cultural preferences.
12. Global Practices in Birthing Positions
Different regions around the world have developed various approaches to birthing positions based on cultural traditions, medical systems, and evidence. Learning from global practices enriches nursing knowledge and care options.
European Approaches
Many European countries, particularly in Scandinavia and the Netherlands, have pioneered modern alternative birthing positions.
- Dutch model: Home births with midwifery support and diverse positions
- Swedish approach: Birthing stools and vertical positions standard in hospitals
- UK: Active Birth movement promoting position freedom
- German birth centers: Specialized equipment for position support
Asian Traditions
Many Asian cultures maintain traditional birthing positions that emphasize harmony and natural processes.
- Japanese: Semi-standing positions with support bars
- Traditional Chinese: Squatting with specific breathing techniques
- Indian Ayurvedic: Position changes based on labor phases
- Thai traditional: Rope-assisted upright positions
Innovative Programs
Notable programs integrating traditional and modern birthing position approaches:
- New Zealand: Integration of Maori birthing traditions in hospitals
- Brazilian “Humanized Birth” centers promoting position freedom
- Canadian First Nations birth centers with traditional positioning
- Australian Bush Nursing integration of Aboriginal practices
Best Practice Highlight: The Dutch Model
The Netherlands maintains one of the world’s highest rates of physiological birth and maternal satisfaction. A key element is their approach to birthing positions:
- Midwives trained extensively in supporting all birthing positions
- Home birth environment designed for position freedom
- Hospital birthing rooms equipped with bars, stools, balls, and mats
- Position changes actively encouraged throughout labor
- Physiological birth positioning integrated into standard protocols
This model demonstrates how integrating position choice throughout maternity care systems can improve outcomes and satisfaction.
13. References and Resources
Key References
- Gupta JK, Sood A, Hofmeyr GJ, Vogel JP. (2017). Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database of Systematic Reviews, Issue 5.
- Lawrence A, Lewis L, Hofmeyr GJ, Styles C. (2013). Maternal positions and mobility during first stage labour. Cochrane Database of Systematic Reviews, Issue 10.
- Kibuka M, Thornton J. (2017). Position in the second stage of labour for women with epidural anaesthesia. Cochrane Database of Systematic Reviews, Issue 2.
- Nieuwenhuijze MJ, Low LK, Korstjens I, Lagro-Janssen T. (2014). The role of maternity care providers in promoting shared decision making regarding birthing positions during second stage labor. Journal of Midwifery & Women’s Health, 59(3), 277-285.
- Priddis H, Dahlen H, Schmied V. (2012). What are the facilitators, inhibitors, and implications of birth positioning? A review of the literature. Women and Birth, 25(3), 100-106.
- Thies-Lagergren L, Kvist LJ, Christensson K, Hildingsson I. (2013). No reduction in instrumental vaginal births and no increased risk for adverse perineal outcome in nulliparous women giving birth on a birth seat: results of a Swedish randomized controlled trial. BMC Pregnancy and Childbirth, 13, 175.
- WHO. (2018). WHO recommendations: intrapartum care for a positive childbirth experience. World Health Organization, Geneva.
Online Resources for Further Learning
- American College of Nurse-Midwives – Position Paper on Physiologic Birth: www.midwife.org
- Evidence Based Birth – Birthing Positions Resources: www.evidencebasedbirth.com
- Lamaze International – Healthy Birth Practices: www.lamaze.org
- Spinning Babies – Optimal Positioning Techniques: www.spinningbabies.com
Video Resources
- Global Birth Initiative: Positions for Labor and Birth (educational series)
- Royal College of Midwives: Supporting Women in Alternative Birth Positions (training video)
- International MotherBaby Childbirth Organization: Optimal Birth Positioning (instructional series)
