Table of Contents
- Introduction
- Definition & Overview
- Epidemiology & Significance
- Pathophysiology
- Risk Factors
- Clinical Presentation
- Diagnosis
- Management & Treatment
- Nursing Care
- Complications
- Prognosis
- Prevention Strategies
- Patient Education
- Global Practices & Guidelines
- Ethical Considerations
- Resources for Nurses
- References
Introduction
Amniotic fluid embolism (AFE) represents one of the most catastrophic complications in obstetric care. Despite its rarity, affecting approximately 1 in 40,000 deliveries, it remains a significant contributor to maternal mortality worldwide, with mortality rates ranging from 20% to 60%. As a nursing student, understanding this condition is critical as immediate recognition and prompt intervention can dramatically alter outcomes in these emergency situations.
The unpredictable nature of amniotic fluid embolism makes it particularly challenging for healthcare providers. It can occur during labor, delivery, or in the immediate postpartum period with little warning. The condition is characterized by the sudden onset of acute hypoxia, hypotension, and coagulopathy, creating a clinical picture that rapidly deteriorates without immediate intervention.
This comprehensive guide aims to equip nursing students with the knowledge to recognize, respond to, and provide appropriate care for patients experiencing amniotic fluid embolism. We will explore the pathophysiology, risk factors, clinical manifestations, diagnostic approaches, management strategies, and specific nursing care interventions essential for optimal patient outcomes.
Definition & Overview
Definition: Amniotic fluid embolism is an obstetric emergency characterized by the entry of amniotic fluid contents into the maternal circulatory system, triggering a severe inflammatory response similar to anaphylaxis and resulting in cardiopulmonary collapse and coagulopathy.
Historically, amniotic fluid embolism was thought to be purely mechanical—amniotic fluid physically obstructing pulmonary vessels. However, modern understanding recognizes it as a complex immunological response to fetal antigens that enter maternal circulation, causing a systemic inflammatory response syndrome (SIRS).
The condition has been renamed by some experts as “Anaphylactoid Syndrome of Pregnancy” to better reflect its immunological nature rather than a simple embolic phenomenon. This distinction is important for understanding both the pathophysiology and treatment approaches.
AFE typically presents as a biphasic process: an initial cardiopulmonary phase characterized by hypoxia and hypotension, followed by a hemorrhagic phase marked by massive obstetric hemorrhage and disseminated intravascular coagulation (DIC). This condition requires immediate, multidisciplinary intervention and is considered a true obstetric emergency.
Epidemiology & Significance
The true incidence of amniotic fluid embolism is difficult to determine due to challenges in diagnosis and varying reporting systems across countries. Current estimates suggest:
- Incidence: 1 in 20,000 to 1 in 80,000 pregnancies
- Mortality rate: 20-60%, with significant improvement in recent decades due to advances in critical care
- Accounts for approximately 5-10% of maternal deaths in developed countries
- Survival often accompanies significant neurological impairment in 50% of cases
AFE remains one of the leading causes of sudden maternal death in developed countries, along with hemorrhage, hypertensive disorders, and thromboembolism. The unpredictability of this condition makes prevention challenging, highlighting the importance of rapid recognition and response.
Pathophysiology
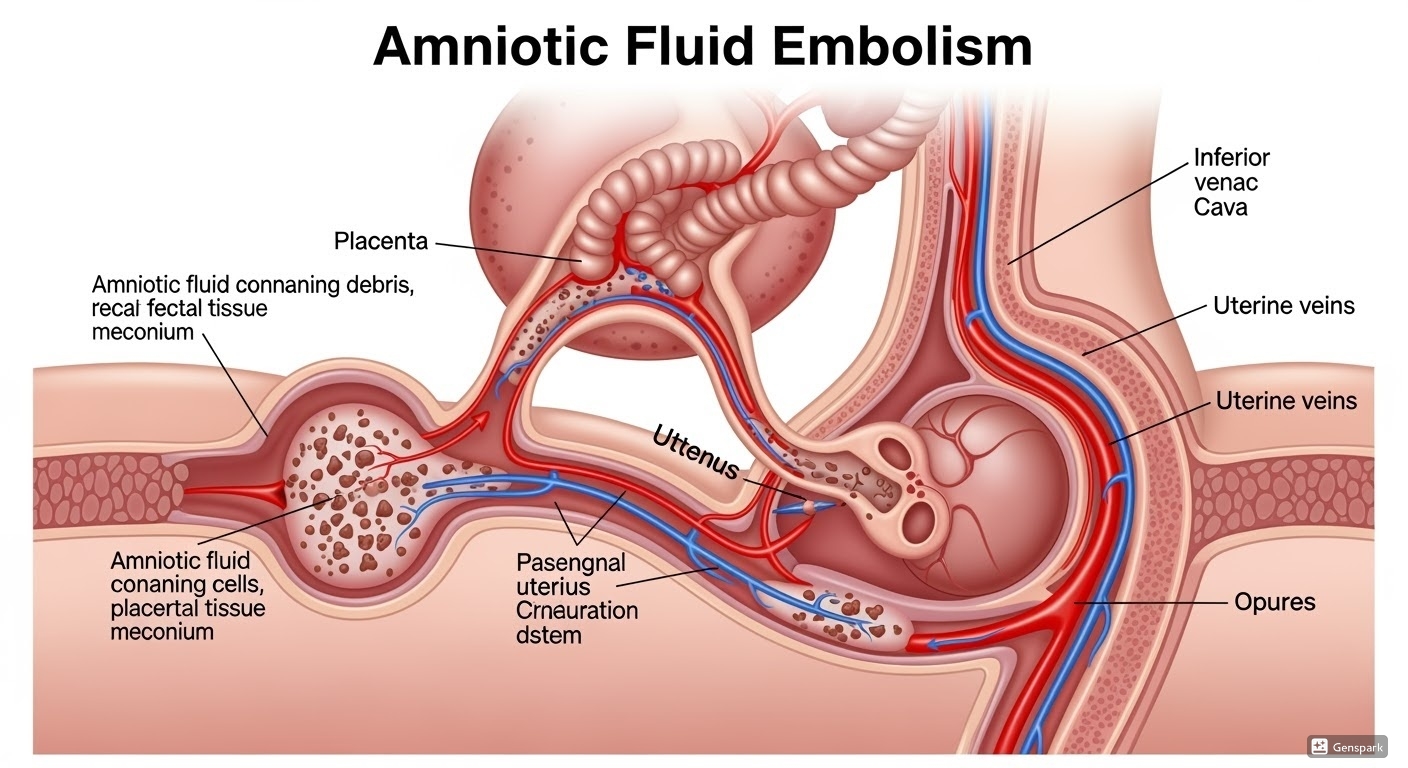
Figure 1: Pathophysiology of amniotic fluid embolism showing entry of amniotic fluid containing fetal cells, hair, and debris into maternal circulation through uterine veins.
The pathophysiology of amniotic fluid embolism involves a complex sequence of events that leads to the characteristic clinical manifestations:
Entry Mechanism
Amniotic fluid containing fetal components (squamous cells, vernix, lanugo, meconium, and other debris) enters the maternal circulation through:
- Tears in the uterine veins during contractions or placental separation
- Endocervical veins during labor or cesarean delivery
- Placental site following delivery
- Sites of uterine trauma or incision
Biphasic Response
The maternal response to amniotic fluid in circulation occurs in two phases:
| Phase | Timeframe | Pathophysiology | Clinical Manifestations |
|---|---|---|---|
| Phase 1: Pulmonary |
Immediate |
|
|
| Phase 2: Hemorrhagic |
Within 30-60 minutes |
|
|
Immunological Components
Rather than simple mechanical obstruction, AFE is now understood as an immunological reaction to fetal antigens, similar to anaphylaxis:
- Maternal immune response to foreign fetal antigens
- Release of endogenous mediators including histamine, bradykinin, cytokines, and prostaglandins
- Complement activation
- Mast cell degranulation
- Inflammatory cascade activation leading to:
- Bronchospasm
- Pulmonary vasoconstriction
- Myocardial depression
- Increased capillary permeability
- DIC activation
Key Pathophysiological Concept:
The severity of amniotic fluid embolism appears to correlate with the volume of amniotic fluid entering maternal circulation and individual maternal susceptibility to these fetal antigens, which may explain why some women develop catastrophic responses while others experience milder manifestations.
Risk Factors
While amniotic fluid embolism is largely unpredictable, certain factors have been associated with increased risk:
Maternal Factors
- Advanced maternal age (>35 years)
- Multiparity (especially grand multiparity)
- History of allergies or atopy
- History of previous cesarean deliveries
- Preexisting maternal comorbidities (hypertension, diabetes)
Pregnancy-Related Factors
- Tumultuous labor with intense, frequent contractions
- Placental abnormalities (placenta previa, placental abruption)
- Polyhydramnios
- Multiple gestation
- Intrauterine fetal demise
Procedural Factors
- Cesarean delivery
- Operative vaginal delivery (forceps, vacuum)
- Manual removal of placenta
- Cervical trauma
- Amnioinfusion
- Intrauterine pressure catheter placement
Fetal Factors
- Male fetal gender (slight association)
- Macrosomia
- Meconium-stained amniotic fluid
Important Note:
The presence of risk factors does not reliably predict AFE occurrence. Many cases occur in women with no identifiable risk factors, highlighting the importance of vigilance in all obstetric patients.
Risk Factor Strength of Association
| Risk Factor | Odds Ratio | Strength of Association |
|---|---|---|
| Maternal age > 35 years | 2.2 | Moderate |
| Cesarean delivery | 5.7 | Strong |
| Placenta previa/abruption | 3.5 | Moderate |
| Eclampsia | 11.5 | Very Strong |
| Medical induction of labor | 3.86 | Moderate |
| Polyhydramnios | 3.0 | Moderate |
| Fetal distress | 1.7 | Weak |
| Grand multiparity | 4.3 | Moderate to Strong |
Clinical Presentation
Amniotic fluid embolism typically presents suddenly and catastrophically during labor, delivery, or in the immediate postpartum period, though cases can occur during pregnancy termination, amniocentesis, or trauma. The classic presentation develops within minutes of inciting events.
Classic Triad
The classic triad of AFE consists of:
- Respiratory Distress – Sudden onset dyspnea, tachypnea, cyanosis
- Cardiovascular Collapse – Hypotension, shock, cardiac arrest
- Coagulopathy – DIC, uncontrolled hemorrhage
Clinical Phases
AFE typically manifests in two distinct clinical phases:
| Phase | Clinical Features |
|---|---|
| Initial Phase (Cardiopulmonary) |
|
| Secondary Phase (Hemorrhagic) |
|
Varying Presentations
Not all cases of amniotic fluid embolism present with the full classic triad. There is a spectrum of severity:
- Fulminant Cases: Rapid progression to cardiac arrest and death within minutes (classic presentation)
- Subacute Cases: More gradual onset with predominant hypoxia or coagulopathy
- Mild Cases: Potentially underdiagnosed, presenting as transient respiratory distress or unexplained postpartum hemorrhage
Mnemonic: “EMBOLI-C”
For recognizing clinical features of Amniotic Fluid Embolism:
- E – Embolism symptoms (dyspnea, chest pain)
- M – Mental status changes (anxiety, agitation, loss of consciousness)
- B – Blood pressure drop (hypotension, shock)
- O – Oxygen saturation decrease (hypoxemia, cyanosis)
- L – Left heart failure (pulmonary edema)
- I – Irregular heartbeat (arrhythmias)
- C – Coagulation abnormalities (DIC, hemorrhage)
Diagnosis
Diagnosing amniotic fluid embolism presents a significant challenge as there is no single definitive diagnostic test. Diagnosis is primarily clinical, based on the presentation and exclusion of other conditions.
Diagnostic Criteria
The Society for Maternal-Fetal Medicine (SMFM) and Amniotic Fluid Embolism Foundation proposed the following diagnostic criteria:
Four Essential Criteria:
- Acute hypotension or cardiac arrest
- Acute hypoxemia (dyspnea, cyanosis, or respiratory arrest)
- Coagulopathy or severe hemorrhage in the absence of other explanations
- All of these occurring during labor, cesarean delivery, or within 30 minutes of delivery
AND absence of fever during labor
Laboratory Findings
While not diagnostic on their own, certain laboratory findings support the diagnosis:
| Test | Typical Finding in AFE | Clinical Significance |
|---|---|---|
| Complete Blood Count | Thrombocytopenia, anemia | Consistent with consumption coagulopathy |
| Coagulation Profile | Prolonged PT/PTT, decreased fibrinogen, elevated D-dimer | Indicates DIC |
| Arterial Blood Gas | Respiratory acidosis, metabolic acidosis, hypoxemia | Reflects respiratory failure and tissue hypoperfusion |
| Cardiac Enzymes | Elevated troponin | Indicates myocardial damage |
| Tryptase Levels | May be elevated | Supports anaphylactoid mechanism |
| Complement Levels | Decreased | Consistent with complement activation |
| Special Stains* | Presence of fetal squamous cells, lanugo, vernix in maternal circulation | Historically considered diagnostic but now recognized as non-specific |
*Note: The presence of fetal elements in maternal circulation was historically considered diagnostic but is now recognized as non-specific, as these elements can be found in women without AFE.
Diagnostic Imaging
- Chest X-ray: May show pulmonary edema, ARDS pattern, or cardiomegaly
- Echocardiography: May demonstrate right ventricular dilatation, pulmonary hypertension, left ventricular dysfunction
- CT Pulmonary Angiography: May exclude pulmonary embolism but usually non-specific for AFE
Differential Diagnosis
Given the non-specific presentation, several other conditions must be excluded:
Cardiovascular/Respiratory
- Pulmonary thromboembolism
- Myocardial infarction
- Cardiomyopathy (including peripartum)
- Air embolism
- Aspiration pneumonitis
- Anaphylaxis
Obstetric/Hemorrhagic
- Placental abruption
- Uterine rupture
- Primary postpartum hemorrhage
- Severe preeclampsia/eclampsia/HELLP syndrome
- Septic shock
- Transfusion reaction
Diagnostic Challenge:
The diagnosis of amniotic fluid embolism remains primarily clinical. It is essentially a diagnosis of exclusion made after ruling out other causes of sudden cardiopulmonary collapse during the peripartum period. The definitive diagnosis is often only confirmed at autopsy in fatal cases.
Management & Treatment
Management of amniotic fluid embolism requires prompt, coordinated multidisciplinary effort focused on maternal resuscitation and support of failing organ systems. There is no specific treatment that targets the underlying pathophysiology.
Immediate Interventions
Initial Resuscitation Priorities:
- Immediate 100% oxygen via non-rebreather mask
- Early intubation and mechanical ventilation for respiratory distress
- Lung-protective ventilation strategies
- Establish multiple large-bore IV access
- Aggressive fluid resuscitation with crystalloids
- Vasopressors and inotropes for hemodynamic support
- Position patient in left lateral position to minimize aortocaval compression
- CPR if cardiac arrest occurs
- If undelivered: emergency cesarean delivery once initial maternal stabilization begun
- Pediatric team attendance for neonatal resuscitation
Specific Treatments
Management of Coagulopathy
| Blood Product/Component | Dosing | Indication |
|---|---|---|
| Packed Red Blood Cells | Units as needed to maintain hemoglobin >8 g/dL | Restore oxygen-carrying capacity |
| Fresh Frozen Plasma | 15-30 mL/kg | Replace coagulation factors |
| Platelets | 1 unit per 10 kg when platelets <50,000/μL | Correct thrombocytopenia |
| Cryoprecipitate | 10 units when fibrinogen <100 mg/dL | Replace fibrinogen |
| Tranexamic Acid | 1 g IV over 10 minutes, second dose if bleeding continues | Antifibrinolytic to reduce bleeding |
| Fibrinogen Concentrate | 4-8 g IV | Rapidly increase fibrinogen levels |
Hemodynamic Support
- Vasopressors: Norepinephrine (first-line) or phenylephrine to maintain adequate blood pressure
- Inotropes: Dobutamine or epinephrine for cardiac support
- Mechanical Support: Consider ECMO (extracorporeal membrane oxygenation) in refractory cases
- Pulmonary Vasodilators: Inhaled nitric oxide or prostacyclin for pulmonary hypertension
Management of Obstetric Hemorrhage
- Uterotonic Agents: Oxytocin, methylergonovine, carboprost for uterine atony
- Intrauterine Balloon Tamponade
- Surgical Interventions:
- Uterine compression sutures (B-Lynch)
- Uterine or internal iliac artery ligation
- Interventional radiology for arterial embolization
- Hysterectomy as last resort
Advanced Support Measures
Cardiopulmonary Support
- Arterial line for continuous BP monitoring
- Central venous catheter for fluid management
- Pulmonary artery catheter for hemodynamic monitoring
- Echocardiography to guide management
- ECMO for refractory hypoxemia or cardiogenic shock
- ARDS management protocols
Other Supportive Measures
- Correction of acidosis
- Maintenance of normothermia
- Seizure prophylaxis/management
- Renal replacement therapy for acute kidney injury
- Stress-dose steroids if hemodynamically unstable
- Prevention of secondary complications (DVT prophylaxis, stress ulcer prevention)
Experimental/Theoretical Therapies
While not standard practice, the following have been reported in case reports:
- Recombinant activated Factor VII for refractory bleeding
- High-dose corticosteroids to mitigate inflammatory response
- C1 esterase inhibitor to modulate complement activation
- Immunotherapy targeting inflammatory mediators
- Hemofiltration or plasmapheresis to remove inflammatory mediators
Mnemonic: “RESCUE-AFE”
For the management priorities in Amniotic Fluid Embolism:
- R – Resuscitation (ABC, CPR if needed)
- E – Emergency delivery if undelivered
- S – Support cardiovascular function (fluids, vasopressors)
- C – Correct coagulopathy (blood products)
- U – Uterine hemorrhage control
- E – ECMO for refractory cases
- A – Acidosis correction
- F – Factor replacement (clotting factors, fibrinogen)
- E – Evaluate end-organ damage
Nursing Care
Nurses play a pivotal role in the early recognition, prompt response, and ongoing management of amniotic fluid embolism. Effective nursing care can significantly impact patient outcomes in this life-threatening emergency.
Assessment
Initial Assessment
- Respiratory: Rate, depth, use of accessory muscles, oxygen saturation
- Cardiovascular: Pulse quality, blood pressure, capillary refill, cardiac rhythm
- Neurological: Level of consciousness, pupillary response
- Integumentary: Color, cyanosis, diaphoresis
- Obstetric: Uterine tone, vaginal bleeding
- Fetal: Fetal heart rate pattern if undelivered
Ongoing Assessment
- Hemodynamic: Continuous cardiac monitoring, invasive pressure monitoring
- Respiratory: ABG values, ventilator parameters
- Fluid Balance: Intake/output, pulmonary status
- Coagulation: Bleeding sites, laboratory values
- Renal: Urine output, color, specific gravity
- Laboratory: Serial hemoglobin, coagulation studies, lactate
- Pain/Comfort: If patient is conscious
Interventions
Emergency Response
- Activate emergency response system/code team
- Position patient appropriately (left lateral if undelivered)
- Administer high-flow oxygen
- Establish multiple IV access with large-bore catheters
- Prepare emergency equipment (intubation supplies, defibrillator)
- Assist with resuscitation efforts
- Document events chronologically
- Communicate with obstetric, anesthesia, critical care teams
Respiratory Support
- Assist with intubation and ventilation management
- Monitor oxygen saturation continuously
- Position for optimal oxygenation
- Suction airway as needed
- Monitor ventilator settings and patient-ventilator synchrony
- Monitor ABG results and adjust care accordingly
Hemodynamic Support
- Administer fluids as prescribed
- Set up and manage vasopressor/inotrope infusions
- Titrate medications according to hemodynamic parameters
- Assist with central line and arterial line placement
- Monitor cardiac output and other hemodynamic values
- Maintain continuous cardiac monitoring
Hemorrhage and Coagulopathy Management
- Administer blood products as ordered
- Monitor for signs of transfusion reactions
- Assess bleeding sites and quantify blood loss
- Apply pressure to bleeding sites when appropriate
- Maintain accurate intake and output records
- Assist with procedures for hemorrhage control
Monitoring
| Parameter | Frequency | Nursing Considerations |
|---|---|---|
| Vital signs | Every 5-15 minutes during acute phase; hourly when stabilized | Note trends and changes requiring immediate intervention |
| Neurological status | Every 30-60 minutes | Monitor GCS, pupillary response, sedation assessment |
| Respiratory status | Continuous | Ventilator parameters, oxygen saturation, breath sounds |
| Hemodynamic parameters | Continuous | CVP, arterial pressure, cardiac output if monitored |
| Bleeding assessment | Every 15-30 minutes initially | Check dressings, drains, incisions, vaginal bleeding |
| Urine output | Hourly | Goal >0.5 mL/kg/hr |
| Laboratory values | As ordered, typically q4-6h initially | Trend CBC, coagulation studies, lactate, ABGs |
Nursing Diagnosis
- Impaired Gas Exchange related to ventilation-perfusion mismatch secondary to pulmonary vascular obstruction
- Decreased Cardiac Output related to reduced myocardial contractility and altered preload/afterload
- Deficient Fluid Volume related to active blood loss and third-spacing
- Ineffective Peripheral Tissue Perfusion related to compromised circulation and coagulopathy
- Risk for Ineffective Cerebral Tissue Perfusion related to hypotension and hypoxemia
- Ineffective Protection related to coagulopathy and immunological response
- Anxiety (family) related to sudden critical condition and uncertain prognosis
- Interrupted Family Processes related to critical illness and separation from newborn
- Risk for Post-Trauma Syndrome related to life-threatening event
Comprehensive Care Plan
Acute Phase
- Maintain Patent Airway and Adequate Oxygenation
- Assist with intubation and mechanical ventilation
- Monitor oxygen saturation continuously
- Maintain head of bed elevation 30-45°
- Suction airway as needed
- Optimize Hemodynamic Status
- Administer fluids and blood products as ordered
- Monitor response to fluid boluses
- Titrate vasopressors and inotropes to achieve hemodynamic targets
- Report significant changes in hemodynamic parameters
- Manage Coagulopathy
- Administer blood components per protocol
- Monitor for signs of ongoing bleeding
- Apply pressure to accessible bleeding sites
- Monitor laboratory values to guide therapy
- Prevent Further Complications
- Implement core measures for critical care (DVT prophylaxis, stress ulcer prophylaxis)
- Maintain normothermia
- Monitor for signs of infection
- Prevent pressure injuries
Stabilization and Recovery Phase
- Support Organ Recovery
- Monitor organ function through laboratory values
- Implement renal protective strategies
- Provide lung-protective ventilation
- Early mobilization when stable
- Psychological Support
- Provide emotional support to family
- Explain procedures and patient status in understandable terms
- Facilitate family presence when appropriate
- Arrange for mental health support as needed
- Mother-Baby Bonding
- Facilitate interaction with baby when mother’s condition allows
- Support breastfeeding if desired and possible
- Provide updates on baby’s condition
- Preparation for Discharge/Transfer
- Educate about follow-up care
- Ensure understanding of medication regimens
- Connect with support services
- Provide information about post-traumatic stress resources
Key Nursing Consideration:
Remember that amniotic fluid embolism impacts not only the mother but her entire family. Emotional support and clear communication are vital components of comprehensive care. Additionally, this event often occurs during what should be a joyous time, making the psychological impact particularly severe.
Complications
Amniotic fluid embolism can lead to several serious complications affecting multiple organ systems. Understanding these potential complications is essential for anticipatory nursing care.
Acute Complications
- Cardiac arrest
- Sudden maternal death
- Massive hemorrhage
- Disseminated intravascular coagulation
- Acute respiratory distress syndrome (ARDS)
- Multiple organ dysfunction syndrome
- Hypoxic-ischemic brain injury
- Fetal distress and death
Intermediate Complications
- Acute kidney injury
- Liver dysfunction
- Pancreatitis
- Secondary infections
- Ventilator-associated pneumonia
- Venous thromboembolism
- Prolonged ICU stay
- Need for prolonged ventilation
Long-term Complications
- Neurological sequelae
- Cognitive impairment
- Chronic respiratory issues
- Psychological trauma
- Post-traumatic stress disorder
- Depression and anxiety
- Impaired quality of life
- Sheehan syndrome (postpartum pituitary necrosis)
Maternal and Fetal Impact
| Outcome | Incidence | Contributing Factors |
|---|---|---|
| Maternal Mortality | 20-60% |
|
| Neurological Damage | Up to 50% of survivors |
|
| Fetal Mortality | 10-40% |
|
| Neonatal Neurological Damage | Variable |
|
Prevention of Secondary Complications:
While the primary event of amniotic fluid embolism cannot typically be prevented, careful nursing care can help reduce secondary complications through:
- Early recognition and intervention
- Vigilant monitoring for signs of deterioration
- Proactive management of coagulopathy
- Adherence to critical care bundles for ventilator management, infection prevention, and DVT prophylaxis
- Early mobilization when patient condition allows
- Psychological support for trauma prevention
Prognosis
The prognosis for patients with amniotic fluid embolism has improved over recent decades but remains guarded. Outcomes depend largely on early recognition, prompt intervention, and access to advanced critical care resources.
Factors Affecting Prognosis
Positive Prognostic Factors
- Rapid recognition and intervention
- Prompt initiation of supportive measures
- Immediate availability of blood products
- Multidisciplinary team approach
- Absence of cardiac arrest
- Shorter time to hemodynamic stabilization
- Access to advanced critical care resources
Negative Prognostic Factors
- Cardiac arrest as initial presentation
- Delay in diagnosis and treatment
- Severe coagulopathy
- Need for CPR lasting >15 minutes
- Development of multiple organ dysfunction
- Severe hypoxic brain injury
- Limited access to advanced critical care
Long-term Outcomes
For survivors of amniotic fluid embolism, the road to recovery can be complex and prolonged:
| Outcome Domain | Common Findings | Nursing Implications |
|---|---|---|
| Physical Recovery |
|
|
| Psychological Recovery |
|
|
| Family Impact |
|
|
| Future Pregnancy |
|
|
Recent Trends in Outcomes
Modern data suggests improving outcomes for amniotic fluid embolism cases:
- Mortality rates have decreased from >60% to 20-40% in recent decades
- Approximately 15-25% of survivors have some degree of permanent neurological impairment
- Nearly 50% of survivors without neurological damage can return to their previous level of function, though often with psychological sequelae
- Improved recognition and management of DIC has significantly improved survival
- Access to ECMO and other advanced cardiac support has salvaged previously fatal cases
Recurrence Risk:
Unlike some obstetric complications, amniotic fluid embolism does not appear to have a significant risk of recurrence in subsequent pregnancies. However, women who have experienced AFE often choose not to pursue future pregnancies due to psychological trauma and fear. Those who do become pregnant again should receive specialized high-risk obstetric care with detailed delivery planning.
Prevention Strategies
Because amniotic fluid embolism is largely unpredictable and occurs without warning, there are no proven strategies for primary prevention. However, certain clinical practices may theoretically reduce risk or improve outcomes.
Potential Risk Reduction
- Avoid tumultuous labor with excessive uterine activity
- Judicious use of labor induction and augmentation
- Consider gentle cesarean technique when indicated
- Careful management of placental delivery
- Vigilance with amnioinfusion procedures
- Early identification and management of placental abnormalities
Preparedness Measures
- Emergency obstetric protocols and drills
- Rapid response team availability
- Immediate access to blood bank resources
- Massive transfusion protocols
- Clear transfer agreements with tertiary care centers
- Multi-disciplinary simulation training
Early Recognition
While not strictly prevention, early recognition can significantly improve outcomes:
- Education of all obstetric staff about warning signs
- High index of suspicion in the peripartum period
- Prompt investigation of unexplained dyspnea or hypotension during labor, delivery, or immediate postpartum
- Low threshold for activating emergency response protocols
- Implementation of maternal early warning scoring systems
Important Consideration:
There is no screening test currently available to identify patients at risk for amniotic fluid embolism. The condition remains unpredictable, underscoring the importance of vigilance and preparedness in all obstetric settings.
Patient Education
Patient education related to amniotic fluid embolism primarily focuses on survivors and their families. Because of the unexpected nature of the condition and its typical occurrence during a critical period, pre-event education is not typically part of routine prenatal care.
For Survivors
Understanding the Event
- Clear explanation of what happened
- Reinforcement that AFE was not preventable
- Addressing misconceptions and guilt
- Information about the rarity of the condition
- Written materials for later reference
Recovery Process
- Expected physical recovery timeline
- Common psychological responses
- Potential long-term effects
- When to seek medical attention
- Importance of follow-up appointments
- Rehabilitation expectations if applicable
Support Resources
- Support group information
- Mental health resources
- AFE Foundation contact information
- Online communities for survivors
- Financial assistance programs
- Legal resources if needed
For Families
Supporting the Survivor
- Understanding normal recovery processes
- Recognizing signs of complications or distress
- Supporting bonding with the newborn
- Managing caregiver stress and burnout
- Communication strategies during recovery
- When and how to access emergency care
Addressing Grief and Trauma
- Processing traumatic birth experience
- Grief support (especially in maternal or fetal loss cases)
- Partner’s response to trauma
- Helping siblings understand
- Family counseling resources
- Self-care for family caregivers
Future Pregnancy Counseling
- Information about recurrence risk (considered to be minimal)
- Discussion of psychological readiness for future pregnancy
- Preconception care recommendations
- Referral to maternal-fetal medicine specialists
- Considerations for delivery planning in future pregnancies
- Alternative family building options if desired
Educational Materials
Key Resources to Provide:
- The AFE Foundation provides support and resources for families affected by amniotic fluid embolism
- Written information explaining AFE in clear, non-medical language
- Contact information for specialized counseling services
- Medical summary documentation for the patient’s records
- Follow-up care schedule and expectations
- Signs and symptoms that would warrant immediate medical attention
Global Practices & Guidelines
Management approaches for amniotic fluid embolism vary somewhat across different regions and healthcare systems, though the core principles remain similar. Here’s an overview of global practices and guidelines:
| Organization/Region | Key Recommendations | Special Considerations |
|---|---|---|
| American College of Obstetricians and Gynecologists (ACOG) |
|
Recommends consideration of ECMO in appropriate settings |
| Royal College of Obstetricians and Gynaecologists (RCOG) |
|
Emphasizes the importance of simulation training for rare emergencies |
| Society for Obstetric Anesthesia and Perinatology (SOAP) |
|
Includes recommendations for use of thromboelastography to guide blood product administration |
| World Health Organization (WHO) |
|
Addresses management in low-resource settings with limited blood product availability |
| Japan Society of Obstetrics and Gynecology |
|
Higher reported incidence of AFE in Japan has led to more focused research and protocols |
Innovative Approaches
Some regions have developed innovative approaches to improve outcomes in cases of amniotic fluid embolism:
- Australia/New Zealand: National registry and biobank for AFE cases to facilitate research
- Netherlands: Mobile ECMO teams that can be deployed to community hospitals
- United Kingdom: Confidential Enquiry into Maternal Deaths provides detailed case review and learning
- Canada: Provincially organized maternal transport networks
- United States: AFE Foundation led research and support initiatives
Low-Resource Settings
Management of amniotic fluid embolism in low-resource settings presents significant challenges:
Challenges
- Limited blood bank resources
- Restricted access to advanced critical care
- Delayed recognition due to competing priorities
- Lack of specialized equipment
- Transportation difficulties for referral
Adaptations
- Blood donation programs for family members
- Basic life support training emphasis
- Manual ventilation techniques
- Simplified diagnostic criteria
- Mobile health consultation services
Best Practice Implementation:
Regardless of location or resources, implementing regular emergency drills and simulation training for rare but catastrophic events like amniotic fluid embolism has been shown to improve team response, reduce delays in intervention, and potentially improve outcomes.
Ethical Considerations
Amniotic fluid embolism presents several unique ethical challenges for healthcare providers due to its sudden onset, high mortality rate, and occurrence during what should be a joyful life event.
Maternal-Fetal Conflict
In cases where the mother is undelivered when AFE occurs, healthcare teams face complex decisions:
- Balancing maternal resuscitation needs with fetal concerns
- Timing of emergency cesarean delivery during maternal collapse
- Resource allocation between maternal and neonatal teams
- Decision-making when maternal prognosis is extremely poor
End-of-Life Decisions
The rapid deterioration in AFE cases may lead to difficult conversations about:
- Continuation of extraordinary measures
- Withdrawal of life-sustaining treatments
- Organ donation considerations
- Surrogate decision-making when the patient cannot participate
- Religious or cultural considerations regarding death and dying
Communication Challenges
The sudden nature of AFE creates unique communication challenges:
With Families
- Delivering devastating news during what was expected to be a celebratory time
- Explaining a complex condition with limited time
- Discussing uncertain outcomes and prognosis
- Supporting decision-making in crisis
- Managing family expectations and hope
Within Healthcare Team
- Clear communication during emergency response
- Transparent discussions about prognosis and limitations
- Debriefing after traumatic events
- Documentation of rare events for learning
- Supporting team members affected by adverse outcomes
Resource Allocation
AFE cases often require significant resources:
- Large volumes of blood products that may impact availability for other patients
- Multiple specialty teams engaged simultaneously
- Intensive care resources for potentially extended periods
- ECMO or other advanced technologies that may be limited
- Balancing resource use with likelihood of favorable outcome
Ethical Framework for Decision-Making:
When facing ethical dilemmas in amniotic fluid embolism cases, healthcare teams should:
- Prioritize patient autonomy when possible through advance directives or previously stated wishes
- Engage in shared decision-making with family members
- Consider the principles of beneficence and non-maleficence
- Maintain transparency about prognosis and uncertainty
- Involve ethics consultation for complex cases
- Document decision-making processes clearly
Resources for Nurses
Nurses caring for patients with amniotic fluid embolism or those interested in learning more can access these valuable resources:
Professional Organizations
- American College of Obstetricians and Gynecologists (ACOG) – Practice Bulletins on Critical Care in Pregnancy
- Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN) – Emergency Obstetric Care Resources
- Society of Critical Care Medicine (SCCM) – Obstetric Critical Care Guidelines
- Amniotic Fluid Embolism Foundation – Clinical information and support resources
- International Society of Obstetric Medicine – Global perspective on obstetric emergencies
Educational Resources
Online Learning
- Advanced Life Support in Obstetrics (ALSO) courses
- Maternal Critical Care e-learning modules
- Simulation scenarios for obstetric emergencies
- Webinars on management of obstetric emergencies
- Virtual case studies on AFE recognition and management
Clinical Tools
- AFE emergency response checklists
- Massive transfusion protocol guidelines
- Mobile apps for obstetric emergencies
- Point-of-care reference cards
- Team communication tools for emergency response
Research Opportunities
- AFE Registry – International registry for case reporting
- Maternal morbidity and mortality review committees
- Quality improvement initiatives in maternal care
- Clinical trials related to hemorrhage management
- Nursing research on supportive care for survivors
Support for Healthcare Providers
Caring for patients with AFE can be emotionally challenging. Resources for healthcare providers include:
- Critical incident stress debriefing services
- Peer support programs for healthcare providers
- Employee assistance programs
- Second victim support resources
- Reflective practice groups
Practice Improvement:
Regular team-based simulation training for rare obstetric emergencies like amniotic fluid embolism has been shown to improve response times, team communication, and potentially patient outcomes. Consider advocating for regular simulations in your practice setting.
References
- Clark SL, Romero R, Dildy GA, et al. Proposed diagnostic criteria for the case definition of amniotic fluid embolism in research studies. Am J Obstet Gynecol. 2016;215(4):408-412.
- Society for Maternal-Fetal Medicine (SMFM), Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215(2):B16-B24.
- Fitzpatrick KE, Tuffnell D, Kurinczuk JJ, Knight M. Incidence, risk factors, management and outcomes of amniotic-fluid embolism: a population-based cohort and nested case-control study. BJOG. 2016;123(1):100-109.
- Kobayashi H, Akasaka J, Naruse K, et al. Comparison of the different definition criteria for the diagnosis of amniotic fluid embolism. J Clin Diagn Res. 2017;11(7):QC18-QC21.
- McDonnell N, Knight M, Peek MJ, et al. Amniotic fluid embolism: an Australian-New Zealand population-based study. BMC Pregnancy Childbirth. 2015;15:352.
- Conde-Agudelo A, Romero R. Amniotic fluid embolism: an evidence-based review. Am J Obstet Gynecol. 2009;201(5):445.e1-13.
- Busardò FP, Frati P, Zaami S, Fineschi V. Amniotic fluid embolism pathophysiology suggests the new diagnostic armamentarium: β-tryptase and complement fractions C3-C4 are the indispensable working tools. Int J Mol Sci. 2015;16(3):6557-6570.
- Sultan P, Seligman K, Carvalho B. Amniotic fluid embolism: update and review. Curr Opin Anaesthesiol. 2016;29(3):288-296.
- Oi H, Naruse K, Koike N, et al. Predictor of mortality in patients with amniotic fluid embolism. J Obstet Gynaecol Res. 2014;40(4):941-945.
- Stafford I, Sheffield J. Amniotic fluid embolism. Obstet Gynecol Clin North Am. 2007;34(3):545-viii.
- Knight M, Berg C, Brocklehurst P, et al. Amniotic fluid embolism incidence, risk factors and outcomes: a review and recommendations. BMC Pregnancy Childbirth. 2012;12:7.
- Moore J, Baldisseri MR. Amniotic fluid embolism. Crit Care Med. 2005;33(10 Suppl):S279-S285.
- Vanderlinden J, Roelants F. Association between amniotic fluid embolism and second-line uterotonic use in case of postpartum hemorrhage: a retrospective comparative study. J Matern Fetal Neonatal Med. 2019;32(24):4081-4087.
- Legendre G, Bouet PE, Sentilhes L. Amniotic fluid embolism: A rare diagnosis with a various clinical presentation. J Gynecol Obstet Hum Reprod. 2020;49(8):101778.
- Ito F, Akasaka J, Koike N, Uekuri C, Shigemitsu A, Kobayashi H. Incidence, diagnosis and pathophysiology of amniotic fluid embolism. J Obstet Gynaecol. 2014;34(7):580-584.
