Aphthous Ulcers: Management in Community Health Nursing
Table of Contents
1. Introduction 2. Definition and Overview 3. Types of Aphthous Ulcers 4. Clinical Features 5. Screening and Diagnosis 5.1 Differential Diagnosis 5.2 Diagnostic Mnemonic 6. Predisposing Factors 7. Management and Treatment 7.1 First Aid Measures 7.2 Treatment Mnemonic 8. Standing Orders Protocol 9. Nursing Care Plans 10. Patient Education 11. Global Best Practices 12. Conclusion 13. References1. Introduction
Aphthous ulcers, commonly known as canker sores, represent one of the most frequent oral mucosal disorders encountered in community health nursing practice. These painful lesions affect up to 25% of the population worldwide and can significantly impact a patient’s quality of life, affecting eating, speaking, and overall comfort. This comprehensive guide provides community health nurses with essential knowledge for identifying, screening, and managing aphthous ulcers in primary care settings.
2. Definition and Overview
Aphthous ulcers are recurrent, painful, round or oval ulcerations of the oral mucosa characterized by a yellow-gray central fibrinous membrane surrounded by an erythematous (red) halo. Unlike herpes simplex lesions, aphthous ulcers are not preceded by vesicles and are not contagious. They predominantly affect non-keratinized oral mucosa (inner cheeks, lips, tongue, soft palate, and floor of the mouth).
The exact etiology of aphthous ulcers remains unclear, although several factors have been implicated:
- Genetic predisposition (family history in 24-46% of cases)
- Immunological dysfunction
- Nutritional deficiencies (iron, vitamin B12, folate)
- Local trauma
- Psychological stress
- Hormonal changes
- Food sensitivities
- Certain medications
While most aphthous ulcers are benign and resolve spontaneously, recurrent episodes can be debilitating, necessitating proper management strategies by community health nurses.
3. Types of Aphthous Ulcers
Aphthous ulcers are classified into three main types based on their clinical presentation, size, number, and healing patterns:
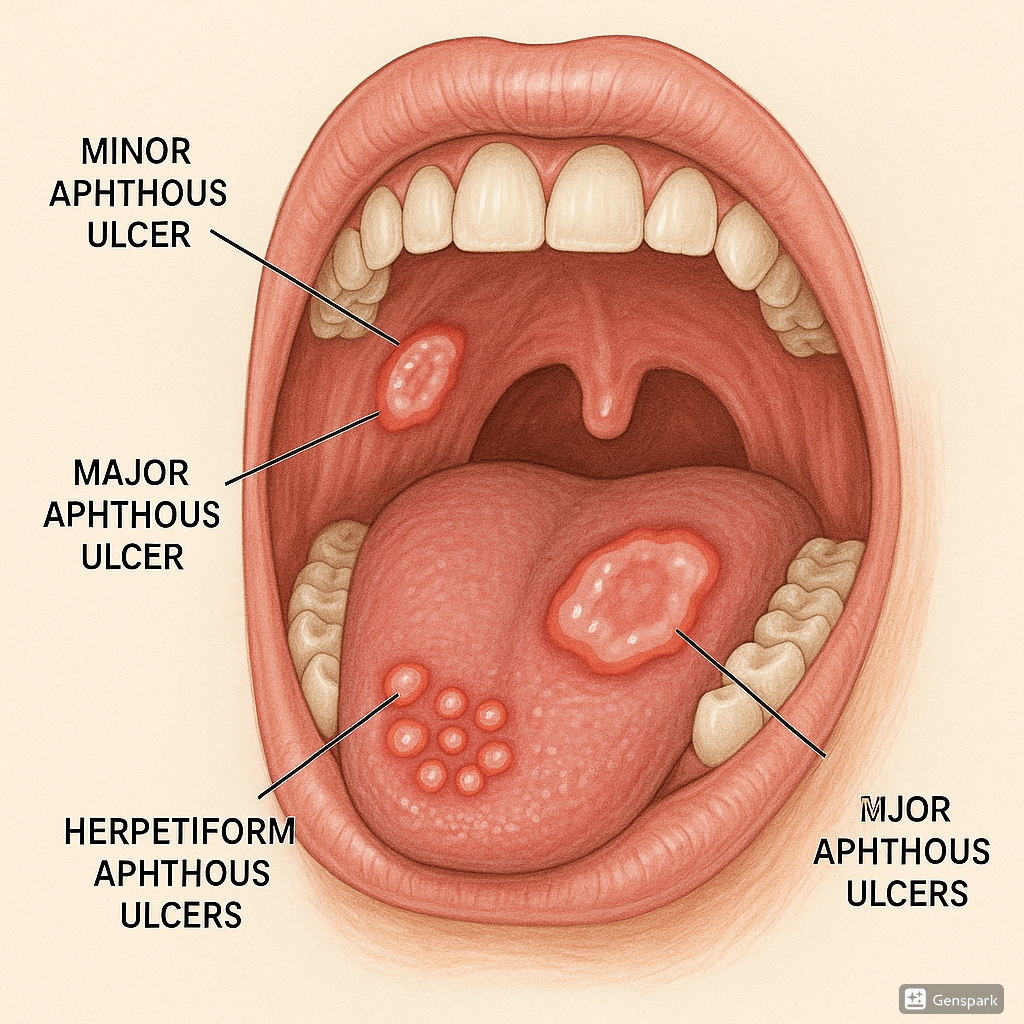
Figure 1: The three main types of aphthous ulcers: minor (left), major (center), and herpetiform (right)
| Characteristic | Minor Aphthous Ulcers | Major Aphthous Ulcers | Herpetiform Aphthous Ulcers |
|---|---|---|---|
| Prevalence | 80-85% of cases | 10-15% of cases | 5-10% of cases |
| Size | Small (< 1 cm), typically 4-5 mm | Large (> 1 cm), can reach 3 cm | Very small (1-3 mm) |
| Number | 1-5 ulcers | 1-10 ulcers | Multiple (5-100 ulcers) |
| Location | Non-keratinized mucosa (labial, buccal, floor of mouth, ventral/lateral tongue) | Any oral site, particularly lips, soft palate, tonsillar fauces | Lateral margins and ventral surface of tongue, floor of mouth |
| Healing Time | 7-14 days | 2-6 weeks or longer | 7-14 days |
| Scarring | No scarring | Often leaves scarring | Rarely leaves scarring |
| Pain Level | Moderate | Severe, may affect eating/speaking | Severe due to multiple lesions |
| Special Notes | Most common form, often recurs | Common in HIV patients, may be associated with systemic conditions | More common in females, later age of onset |
Minor Aphthous Ulcers
Minor aphthous ulcers are the most common form, accounting for approximately 85% of all cases. These superficial lesions are typically less than 1 cm in diameter (usually around 4-5 mm) and occur on non-keratinized mucosa. They have a round or oval shape with a yellow-white center surrounded by an erythematous halo. Minor aphthous ulcers heal within 10-14 days without scarring, despite years of recurrence.
Major Aphthous Ulcers
Major aphthous ulcers (also known as Sutton’s disease or periadenitis mucosa necrotica recurrens) represent 10-15% of cases. These lesions are larger (>1 cm), deeper, and more painful than minor ulcers. They may persist for weeks to months and often heal with scarring. Major aphthous ulcers can cause significant discomfort, affecting eating, speaking, and swallowing. They are frequently observed in patients with HIV infection.
Herpetiform Aphthous Ulcers
Despite the name, herpetiform aphthous ulcers are not caused by herpes virus. They comprise only 5-10% of all aphthous ulcer cases. These are characterized by multiple (5-100), small (1-3 mm) ulcers that may coalesce to form larger irregular ulcerations with marked erythema. Commonly affecting the lateral/ventral tongue surface and floor of the mouth, these ulcers typically heal within 7-14 days. Herpetiform aphthous ulcers predominantly affect females and have a later age of onset compared to other types.
4. Clinical Features
Recognizing the clinical features of aphthous ulcers is essential for community health nurses to differentiate them from other oral lesions. Common clinical characteristics include:
Key Clinical Features of Aphthous Ulcers
- Prodromal symptoms: Burning, tingling, or pricking sensation 24-48 hours before ulcer appearance
- Appearance: Round or oval ulcers with well-defined borders
- Base: Yellow-gray fibrinous membrane (necrotic tissue)
- Border: Elevated, clearly demarcated erythematous (red) halo
- Pain: Considerable pain disproportionate to size, especially when eating acidic or spicy foods
- Location: Predominantly on non-keratinized (movable) oral mucosa
- Recurrence: Tendency to recur at regular or irregular intervals
- Absence of vesicles: Unlike herpes simplex lesions, aphthous ulcers do not develop from vesicles
The clinical presentation varies according to the type of aphthous ulcers as detailed in the previous section. Minor aphthous ulcers are superficial with clearly defined margins, while major aphthous ulcers are deeper with irregular edges. Herpetiform ulcers may be difficult to visualize individually due to their small size and tendency to coalesce.
The pain associated with aphthous ulcers typically peaks during the first 3-4 days and gradually diminishes as healing progresses. In severe cases, especially with major or multiple herpetiform ulcers, patients may experience difficulty in eating, speaking, and swallowing, potentially leading to dehydration and nutritional deficiencies.
5. Screening and Diagnosis
Aphthous ulcers are primarily diagnosed based on clinical presentation and patient history. Laboratory tests are rarely required except in cases of severe, persistent, or atypical presentations. A systematic approach to screening and diagnosis includes:
Clinical Assessment
- History taking: Document frequency, duration, pattern of recurrence, associated symptoms, and potential triggers
- Physical examination: Thorough examination of the oral cavity with adequate lighting and retraction of mobile tissues
- Inspection: Note number, size, shape, location, and appearance of ulcers
- Palpation: Assess for induration, fixation to underlying tissues (suggestive of malignancy)
- External examination: Check for cervical lymphadenopathy
Key Diagnostic Questions for Community Health Nurses
| Assessment Area | Key Questions |
|---|---|
| Duration & Pattern |
|
| Symptoms |
|
| Potential Triggers |
|
| Medical History |
|
| Risk Assessment |
|
Laboratory Investigations
Laboratory tests are not routinely required for typical aphthous ulcers but may be indicated in cases of:
- Severe, frequent, or atypical presentations
- Suspected systemic association
- Persistent ulceration (>3 weeks)
- Poor response to conventional therapy
When indicated, the following investigations may be considered:
| Investigation | Purpose |
|---|---|
| Complete blood count | To identify anemia or other hematological abnormalities |
| Serum iron, ferritin, vitamin B12, folate | To identify nutritional deficiencies |
| Erythrocyte sedimentation rate (ESR)/C-reactive protein (CRP) | To detect inflammatory conditions |
| Anti-gliadin and anti-endomysial antibodies | If celiac disease is suspected |
| Biopsy | For persistent, atypical, or suspicious lesions to rule out malignancy |
5.1 Differential Diagnosis
Community health nurses must be able to differentiate aphthous ulcers from other oral lesions that may present similarly:
| Condition | Key Differentiating Features |
|---|---|
| Herpes simplex virus (HSV) infection | Preceded by vesicles, primarily affects keratinized mucosa (gingiva, hard palate), clustered lesions, prodromal tingling with fever and malaise |
| Traumatic ulcer | History of trauma, irregular shape, corresponds to source of trauma (e.g., sharp tooth), resolves when cause removed |
| Oral cancer | Single, persistent ulcer (>3 weeks), indurated borders, typically painless, cervical lymphadenopathy, risk factors (tobacco, alcohol) |
| Oral lichen planus | Often bilateral, white lacy pattern (Wickham’s striae), affects both attached and movable mucosa |
| Erythema multiforme | Sudden onset, target lesions on skin, crusting of lips, affects both attached and movable mucosa |
| Pemphigus/pemphigoid | Begins as bullae that rupture forming erosions, positive Nikolsky’s sign, may have skin involvement |
| Hand, foot, and mouth disease | Affects children, accompanying fever, skin lesions on hands and feet, multiple oral lesions |
| Drug-induced ulceration | Temporal relationship with drug initiation, may resolve with drug discontinuation |
Warning Signs Requiring Referral
Community health nurses should immediately refer patients when the following warning signs are present:
- Single ulcer persisting for more than 3 weeks
- Ulcer with indurated (hard) borders or base
- Unexplained lymphadenopathy
- Ulcers that are painless (unusual for aphthous ulcers)
- Progressive enlargement of the ulcer
- Recurrent ulcers with systemic symptoms (fever, weight loss)
- Multiple or severe ulcerations in immunocompromised patients
5.2 Diagnostic Mnemonic
Mnemonic for Assessing Aphthous Ulcers: “APHTHOUS”
A – Appearance: Round/oval with yellow-gray center and red halo
P – Pain: Present and often disproportionate to size
H – History: Previous episodes, family history, potential triggers
T – Time course: Duration, healing pattern, and recurrence
H – Health conditions: Associated systemic diseases or nutritional deficiencies
O – Oral location: Typically on non-keratinized mucosa
U – Underlying factors: Stress, trauma, medications, diet
S – Size and number: Classify type based on size and quantity of lesions
6. Predisposing Factors
Community health nurses should be aware of various factors that may predispose individuals to aphthous ulcers to provide comprehensive care and preventive guidance:
| Category | Predisposing Factors | Nursing Implications |
|---|---|---|
| Genetic Factors | Family history (24-46% of cases), certain HLA types | Identify genetic predisposition through family history assessment |
| Trauma | Toothbrush injury, sharp tooth edges, dental treatments, cheek biting | Educate on proper oral hygiene techniques, recommend dental evaluation for sharp edges |
| Nutritional Deficiencies | Iron, vitamin B1, B2, B6, B12, folate, zinc | Screen for deficiencies, recommend dietary modifications or supplements as appropriate |
| Food Sensitivities | Chocolate, coffee, peanuts, almonds, strawberries, tomatoes, cheese, gluten | Recommend food diary to identify potential triggers, consider elimination diet |
| Hormonal Changes | Menstrual cycle, pregnancy, menopause | Note correlation with hormonal fluctuations, educate on potential cyclical pattern |
| Psychological Factors | Stress, anxiety, psychological disorders | Assess stress levels, provide stress management strategies, consider referral for persistent psychological issues |
| Medications | NSAIDs, nicorandil, sodium hypochlorite, phenobarbital, beta-blockers | Review medication history, consider alternative medications if temporal relationship established |
| Systemic Conditions | Inflammatory bowel disease, celiac disease, Behçet’s syndrome, HIV, immunodeficiency | Screen for associated symptoms, refer for further evaluation if systemic disease suspected |
| Lifestyle Factors | Smoking cessation (paradoxically), alcohol consumption | Note that aphthous ulcers may increase temporarily after smoking cessation; continue to encourage cessation with supportive measures |
Interestingly, tobacco smoking appears to have a protective effect against aphthous ulcers. Studies suggest that the increased keratinization of oral mucosa in smokers may render it less susceptible to ulceration. However, many patients report an increase in aphthous ulcers upon smoking cessation, which should not discourage cessation efforts but may warrant additional supportive treatment during this period.
Understanding these predisposing factors is crucial for implementing targeted preventive strategies and identifying potential underlying conditions requiring further investigation or specialist referral.
7. Management and Treatment
The management of aphthous ulcers focuses on symptomatic relief, reducing ulcer duration, and preventing recurrence. Treatment approaches should be tailored to the severity, frequency, and impact on the patient’s quality of life.
Treatment Goals:
- Reduce pain and discomfort
- Promote healing and shorten duration
- Prevent or reduce frequency of recurrence
- Address underlying factors when identifiable
- Maintain adequate nutrition and hydration
Treatment Approaches Based on Severity:
| Severity Level | Clinical Presentation | Recommended Management |
|---|---|---|
| Mild | Occasional minor ulcers, minimal impact on daily life |
|
| Moderate | Frequent minor or occasional major ulcers, moderate pain affecting eating/speaking |
|
| Severe | Frequent major or herpetiform ulcers, significant impact on quality of life |
|
7.1 First Aid Measures
First-line interventions that community health nurses can recommend for immediate relief include:
First Aid for Aphthous Ulcers
- Rinse with warm salt water (½ teaspoon salt in 8 oz warm water) several times daily
- Apply ice directly to the ulcer for temporary numbing
- Rinse with alcohol-free antimicrobial mouthwash containing chlorhexidine
- Apply over-the-counter topical anesthetics (e.g., benzocaine gel, lidocaine viscous)
- Use barrier pastes (e.g., Orabase) to protect ulcers from further irritation
- Apply milk of magnesia directly to ulcers several times daily
- Mix equal parts hydrogen peroxide and water as a rinse (do not swallow)
- Avoid irritating foods (spicy, acidic, salty, hard/crunchy)
- Maintain hydration and consider liquid nutritional supplements if eating is difficult
- Use a soft-bristled toothbrush and gentle technique
Pharmacological Management:
| Category | Examples | Mechanism/Use | Nursing Considerations |
|---|---|---|---|
| Topical Anesthetics | Benzocaine (Orajel), lidocaine 2% viscous, benzydamine | Temporary pain relief by numbing the area | Short duration (30-60 min), apply before meals to aid eating, avoid excessive use |
| Protective Barriers | Carmellose gelatin paste (Orabase), sucralfate suspension | Forms physical barrier over ulcer, reducing irritation | Apply to dry mucosa, reapply after eating/drinking |
| Antimicrobial Mouthwashes | Chlorhexidine gluconate 0.2%, tetracycline suspension | Reduces secondary infection, tetracycline may inhibit collagenase | Chlorhexidine may stain teeth with prolonged use, avoid in children under 12 |
| Topical Corticosteroids | Triamcinolone acetonide (Kenalog in Orabase), fluocinonide, clobetasol | Reduces inflammation and speeds healing | Apply directly to ulcer 2-3 times daily, best used early in ulcer development |
| Topical Anti-inflammatories | Amlexanox 5% paste, diclofenac gel | Reduces inflammation and speeds healing | Apply 4 times daily until healing, works best if started at prodromal stage |
| Systemic Medications | Prednisone, colchicine, pentoxifylline, dapsone, thalidomide | For severe, recurrent cases resistant to topical therapy | Require prescription and specialist supervision, significant side effect profiles |
| Nutritional Supplements | Vitamin B complex, folate, iron, zinc | Addresses deficiencies that may predispose to ulcers | Only effective in cases of confirmed deficiency |
Alternative and Complementary Approaches:
- Laser therapy: Low-level laser therapy has shown efficacy in reducing pain and promoting healing
- Honey: Medical-grade honey has antimicrobial and anti-inflammatory properties
- Aloe vera gel: May have soothing and healing properties
- Chamomile tea rinses: Anti-inflammatory and soothing properties
- Licorice root extract: Contains glycyrrhizin with anti-inflammatory properties
7.2 Treatment Mnemonic
Mnemonic for Treating Aphthous Ulcers: “ULCERS”
U – Understand the type and severity of ulcers to guide treatment approach
L – Lessen pain with topical anesthetics and analgesics
C – Control inflammation with corticosteroids or anti-inflammatory agents
E – Eliminate triggers and address underlying factors
R – Restore nutrition and correct deficiencies
S – Support healing with protective barriers and proper oral hygiene
8. Standing Orders Protocol
Standing orders allow community health nurses to implement specific interventions for aphthous ulcers based on predetermined protocols without direct physician involvement for each case. These protocols enhance timely care delivery while ensuring appropriate management and referral when needed.
STANDING ORDERS PROTOCOL FOR APHTHOUS ULCERS IN COMMUNITY HEALTH SETTINGS
PURPOSE:
To guide community health nurses in the assessment, management, and appropriate referral of patients presenting with aphthous ulcers.
ELIGIBILITY:
This protocol applies to registered nurses, licensed practical nurses, and advanced practice nurses working in community health settings who have received appropriate training in oral assessment and management of aphthous ulcers.
ASSESSMENT PROTOCOL:
- Perform comprehensive oral examination with adequate lighting and retraction of mobile tissues.
- Document the following characteristics of observed oral ulcers:
- Number, size, shape, and location of ulcers
- Appearance (color, borders, surrounding tissue)
- Duration of current ulcers
- Pain level (using standardized pain scale)
- Obtain relevant history including:
- Recurrence pattern and frequency
- Previous treatments and their effectiveness
- Potential triggers (trauma, stress, foods)
- Associated symptoms (local and systemic)
- Relevant medical conditions
- Current medications
- Screen for warning signs requiring immediate referral:
- Single ulcer persisting >3 weeks
- Indurated or rolled borders
- Unexplained lymphadenopathy
- Painless ulcers
- Progressive enlargement
- Systemic symptoms (fever, weight loss)
CLASSIFICATION AND MANAGEMENT GUIDELINES:
1. Minor Aphthous Ulcers (Typical Presentation)
Characterized by: Small (<1 cm), round/oval ulcers with yellow-gray center and red halo on non-keratinized mucosa, painful, healing within 7-14 days
Management:
- Provide patient education on condition and self-care measures
- Recommend warm salt water rinses (½ tsp salt in 8 oz water) 4-6 times daily
- Advise application of over-the-counter topical anesthetics (benzocaine gel) before meals
- Recommend protective barrier paste (Orabase) applied to dry ulcers 2-4 times daily
- Instruct on avoiding irritating foods/beverages and maintaining good oral hygiene
- May provide chlorhexidine gluconate 0.12% mouthwash to rinse twice daily (avoid in children under 12)
- For pain, recommend acetaminophen or ibuprofen as appropriate based on medical history
2. Major Aphthous Ulcers or Multiple/Recurrent Ulcers
Characterized by: Larger (>1 cm) and/or deeper ulcers, significant pain affecting eating/speaking, longer healing time (2-6 weeks), may leave scars
Management:
- Implement all measures for minor aphthous ulcers
- May provide triamcinolone acetonide 0.1% in Orabase to apply to ulcers 2-3 times daily (proper training required)
- Evaluate for nutritional deficiencies (refer for blood tests if indicated)
- Schedule follow-up evaluation in 7-10 days
- If no improvement after 10 days or worsening symptoms, refer to primary care provider
- Consider liquid nutritional supplements if eating is significantly affected
3. Complex Presentations
Characterized by: Severe/extensive ulceration, systemic symptoms, suspected association with underlying disease, unresponsive to basic measures
Management:
- Implement initial pain relief measures as for minor ulcers
- Refer to primary care provider or dentist within 24-48 hours
- Document all findings and interventions thoroughly
- Provide interim supportive care for pain and hydration
MANDATORY REFERRAL CRITERIA:
- Any single ulcer persisting for more than 3 weeks
- Ulcers with indurated margins or base
- Unexplained lymphadenopathy
- Atypical presentation or location
- Severe, persistent, or recurrent multiple ulcerations
- Ulcers associated with systemic symptoms
- Suspicion of underlying systemic disease
- No improvement after 10-14 days of management
- Recurrent episodes (>3 per year) of multiple or severe ulcers
DOCUMENTATION REQUIREMENTS:
- Complete description of ulcer(s) with measurements
- Detailed history including duration, symptoms, and recurrence pattern
- Assessment findings and classification of ulcer type
- Interventions implemented under standing orders
- Patient education provided
- Follow-up plan and any referrals made
- Response to treatment (at follow-up)
FOLLOW-UP PROTOCOL:
- For minor aphthous ulcers: Follow up by phone in 7 days if not resolved
- For major aphthous ulcers: Schedule in-person follow-up in 7-10 days
- For severe or complex cases: Follow up after specialist appointment
- Document all follow-up findings and outcomes
Standing Orders Authorized By: [Primary Care Physician/Medical Director Name]
Date of Implementation: [Date]
Review Date: [Review Date]
9. Nursing Care Plans
Community health nurses can develop comprehensive care plans for patients with aphthous ulcers using the nursing process framework:
| Nursing Diagnosis | Goals/Outcomes | Nursing Interventions | Evaluation Criteria |
|---|---|---|---|
| Acute Pain related to oral ulceration as evidenced by verbal reports of pain, difficulty eating, and protective behaviors |
|
|
|
| Impaired Oral Mucous Membrane related to inflammatory process as evidenced by ulceration, pain, and difficulty maintaining oral hygiene |
|
|
|
| Imbalanced Nutrition: Less Than Body Requirements related to pain with eating as evidenced by decreased intake and weight loss |
|
|
|
| Knowledge Deficit related to unfamiliarity with condition and management as evidenced by questions, misconceptions, and improper care techniques |
|
|
|
| Risk for Recurrence related to multiple predisposing factors as evidenced by history of recurrent episodes |
|
|
|
10. Patient Education
Community health nurses play a pivotal role in educating patients about aphthous ulcers. A comprehensive patient education plan should include:
Key Elements of Patient Education
Understanding the Condition:
- Basic explanation of what aphthous ulcers are and their non-contagious nature
- Common causes and triggers
- Typical duration and healing patterns
- Differences between aphthous ulcers and other oral lesions
Self-Care Measures:
- Proper oral hygiene with soft-bristled toothbrush and gentle technique
- Salt water rinses (preparation and technique)
- Appropriate use of over-the-counter products
- Dietary modifications to minimize pain
- Application techniques for topical medications
Preventive Strategies:
- Identifying and avoiding personal triggers
- Stress management techniques
- Maintaining good nutrition
- Addressing vitamin deficiencies if present
- Proper dental care to minimize trauma
When to Seek Medical Attention:
- Ulcers lasting longer than 3 weeks
- Unusually severe pain or difficulty eating/drinking
- Fever or other systemic symptoms
- Unusual appearance or location of ulcers
- Increasing size or worsening symptoms despite treatment
Educational Resources for Patients:
- Written handouts with self-care instructions
- Illustrated guides for medication application
- Food diary templates to identify dietary triggers
- Lists of recommended and foods to avoid
- Reliable websites for additional information
Common Patient Misconceptions to Address:
- Myth: Aphthous ulcers are contagious.
Fact: They are not contagious and cannot be transmitted to others. - Myth: Aphthous ulcers are caused by herpes virus.
Fact: They are not caused by herpes or any virus; they differ from cold sores. - Myth: All mouth ulcers are aphthous ulcers.
Fact: Other conditions can cause oral ulceration requiring different treatment. - Myth: Aphthous ulcers always indicate a serious underlying condition.
Fact: Most cases are benign, though persistent or unusual ulcers warrant evaluation. - Myth: There’s nothing you can do to prevent recurrence.
Fact: Identifying triggers and using preventive strategies can reduce frequency.
11. Global Best Practices
Community health nurses can benefit from understanding global approaches and best practices in the management of aphthous ulcers:
| Region/Country | Notable Practice | Potential Application in Community Nursing |
|---|---|---|
| Mediterranean Region | Use of medical-grade honey (particularly thyme honey) for its antimicrobial and healing properties | Recommend as a natural alternative in conjunction with conventional treatments, particularly in patients seeking natural remedies |
| India | Incorporation of turmeric in oral rinses for its anti-inflammatory properties (curcumin) | Suggest turmeric mouth rinse preparation (½ tsp in warm water) as complementary approach for inflammation reduction |
| United Kingdom | Structured screening protocols in primary care for early identification of serious oral conditions | Adapt UK’s “red flag” screening system for community settings to ensure timely referral of concerning lesions |
| South Korea | Integration of low-level laser therapy in primary care settings | Consider advocating for portable laser devices in community clinics for treatment of severe or recurrent cases |
| Brazil | Community-based oral health programs with specific aphthous ulcer management protocols | Implement preventive education in schools and community centers focusing on early recognition and management |
| Japan | Use of Kampo medicine (Japanese traditional herbal medicine) for recurrent aphthous stomatitis | Consider appropriate herbal supplements as complementary approach when conventional treatments are insufficient |
| Australia | Remote nursing protocols for managing oral conditions in rural and indigenous communities | Adapt telemedicine approaches for assessing and managing aphthous ulcers in underserved areas |
| Canada | Integration of oral health assessment into routine primary care nursing practice | Incorporate standardized oral examination as part of regular health assessment, particularly for high-risk groups |
Emerging Global Trends in Aphthous Ulcer Management:
- Preventive focus: Emphasis on identifying and addressing predisposing factors rather than just symptomatic treatment
- Integration of traditional and conventional approaches: Combining evidence-based conventional treatments with validated traditional remedies
- Multidisciplinary approach: Collaboration between nursing, dental, and medical professionals for comprehensive care
- Technological innovations: Use of mobile applications for tracking triggers, symptoms, and treatment response
- Education-centered interventions: Empowering patients with knowledge for self-management and prevention
12. Conclusion
Aphthous ulcers represent a common and often challenging condition encountered in community health nursing practice. While most cases are benign and self-limiting, they can significantly impact patients’ quality of life and occasionally signal underlying systemic conditions.
Community health nurses play a crucial role in the screening, diagnosis, and management of aphthous ulcers through:
- Systematic assessment and proper differentiation from other oral lesions
- Implementation of evidence-based management strategies following standing orders
- Providing comprehensive patient education for self-care and prevention
- Recognizing warning signs requiring prompt referral
- Addressing predisposing factors and nutritional deficiencies
- Monitoring treatment response and adjusting interventions accordingly
By developing expertise in managing aphthous ulcers, community health nurses can significantly improve patient comfort, promote optimal oral health, and ensure timely identification of potentially serious conditions. The structured approach outlined in these notes provides a comprehensive framework for delivering high-quality, evidence-based care for patients with aphthous ulcers in community settings.
13. References
- Tarakji, B., Gazal, G., Al-Maweri, S. A., Azzeghaiby, S. N., & Alaizari, N. (2015). Guideline for the diagnosis and treatment of recurrent aphthous stomatitis for dental practitioners. Journal of international oral health, 7(5), 74-80.
- Paleri, V., Staines, K., Sloan, P., Douglas, A., & Wilson, J. (2010). Evaluation of oral ulceration in primary care. Bmj, 340, c2639.
- Akintoye, S. O., & Greenberg, M. S. (2005). Recurrent aphthous stomatitis. Dental Clinics of North America, 49(1), 31-47.
- Natah, S. S., Konttinen, Y. T., Enattah, N. S., Ashammakhi, N., Sharkey, K. A., & Häyrinen-Immonen, R. (2004). Recurrent aphthous ulcers today: a review of the growing knowledge. International journal of oral and maxillofacial surgery, 33(3), 221-234.
- Scully, C., & Porter, S. (1989). Recurrent aphthous stomatitis: current concepts of etiology, pathogenesis and management. Journal of oral pathology & medicine, 18(1), 21-27.
- Chavan, M., Jain, H., Diwan, N., Khedkar, S., Shete, A., & Durkar, S. (2012). Recurrent aphthous stomatitis: a review. Journal of oral pathology & medicine, 41(8), 577-583.
- Barrons, R. W. (2001). Treatment strategies for recurrent oral aphthous ulcers. American Journal of Health-System Pharmacy, 58(1), 41-50.
- Wilkinson, J. (2015). Nurses’ reported use of standing orders in primary health care settings. Journal of primary health care, 7(1), 34-41.
- Pakfetrat, A., Mansourian, A., Momen-Heravi, F., Delavarian, Z., Momen-Beitollahi, J., Khalilzadeh, O., & Basir-Shabestari, S. (2010). Comparison of colchicine versus prednisolone in recurrent aphthous stomatitis: A double-blind randomized clinical trial. Clinical and investigative medicine, 33(3), E189-E195.
- Kozlak, S. T., Walsh, S. J., & Lalla, R. V. (2010). Reduced dietary intake of vitamin B12 and folate in patients with recurrent aphthous stomatitis. Journal of oral pathology & medicine, 39(5), 420-423.
- Altenburg, A., El-Haj, N., Micheli, C., Puttkammer, M., Abdel-Naser, M. B., & Zouboulis, C. C. (2014). The treatment of chronic recurrent oral aphthous ulcers. Deutsches Ärzteblatt International, 111(40), 665.
- Belenguer-Guallar, I., Jiménez-Soriano, Y., & Claramunt-Lozano, A. (2014). Treatment of recurrent aphthous stomatitis. A literature review. Journal of clinical and experimental dentistry, 6(2), e168.
