Biological Basis of Human Behavior
Comprehensive Nursing Notes
Visual Overview
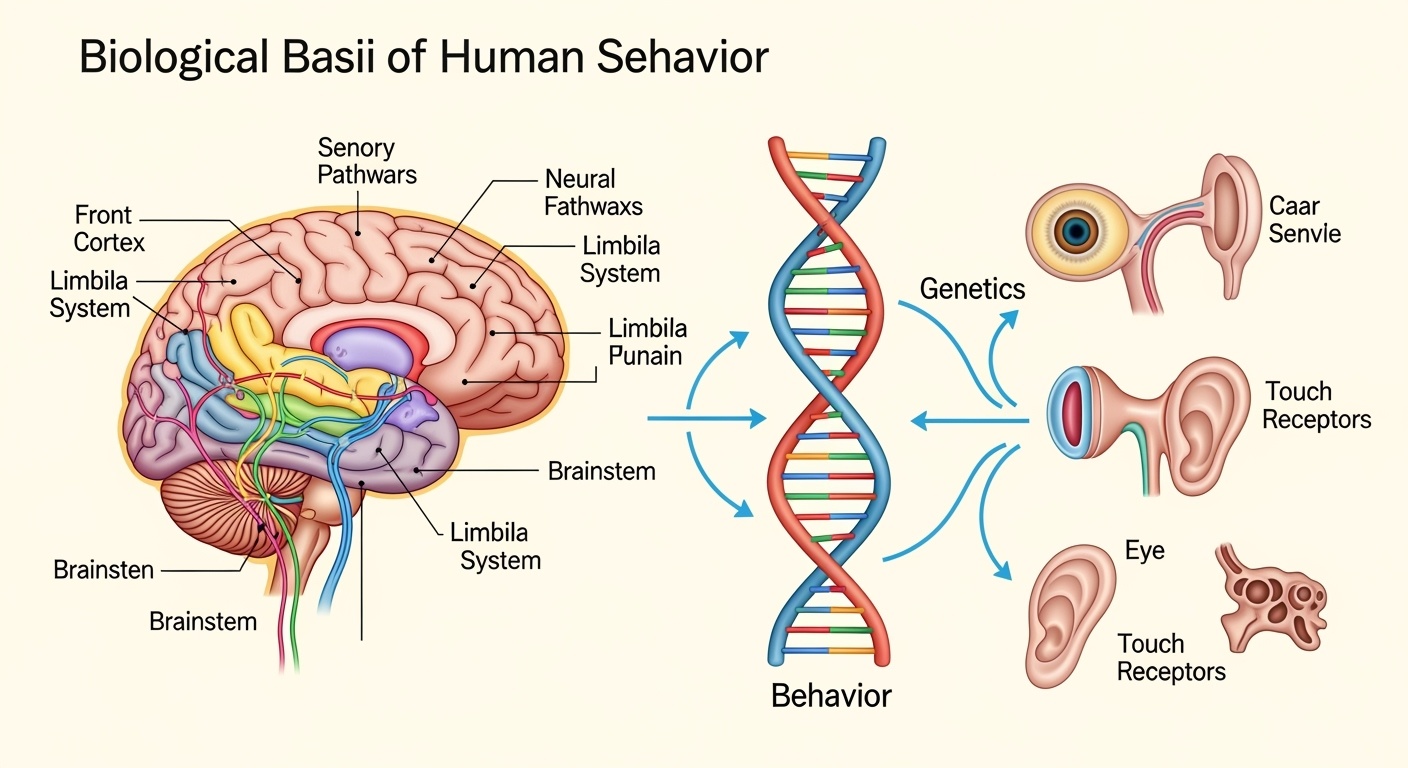
The interconnected relationship between genetics, brain structure, sensory processing, and human behavior
Learning Objectives
Introduction
Human behavior emerges from complex interactions between biological, psychological, and environmental factors. Understanding these foundations is crucial for nursing professionals who must assess, interpret, and respond to diverse patient behaviors in clinical settings. The biological basis of behavior encompasses genetic predispositions, neuroanatomical structures, neurotransmitter systems, and sensory processing mechanisms that collectively influence how individuals think, feel, and act.
Clinical Relevance for Nurses
- Predicting patient responses to stress, pain, and medical interventions
- Understanding behavioral manifestations of neurological conditions
- Tailoring communication strategies based on sensory capabilities
- Recognizing genetic risk factors for behavioral health issues
Memory Aid: BRAIN Framework
Body-Mind Relationship
The body-mind relationship represents the fundamental interconnection between physical and psychological processes. This bidirectional relationship means that physical states influence mental processes, while psychological states can manifest as physical symptoms. For nurses, understanding this relationship is essential for holistic patient care and effective therapeutic interventions.
Physical → Mental Pathway
(Pain, fatigue, illness)
(Stress hormones, neurotransmitters)
(Mood, cognition, behavior)
Mental → Physical Pathway
(Stress, anxiety, depression)
(HPA axis, autonomic nervous system)
(Tension, GI issues, immune changes)
Nursing Implementation: Body-Mind Assessment
Assessment Focus
- • Psychosomatic symptoms
- • Stress manifestations
- • Coping mechanisms
- • Sleep patterns
- • Appetite changes
Interventions
- • Relaxation techniques
- • Mindfulness practices
- • Progressive muscle relaxation
- • Therapeutic communication
- • Environmental modifications
Evaluation
- • Symptom reduction
- • Stress level monitoring
- • Functional improvement
- • Quality of life measures
- • Patient satisfaction
Physiological Mechanisms
Stress Response System
The hypothalamic-pituitary-adrenal (HPA) axis coordinates the body’s response to stress, releasing cortisol and other hormones that affect mood, memory, and immune function.
- • Hypothalamus: CRH release
- • Pituitary: ACTH secretion
- • Adrenals: Cortisol production
Neurotransmitter Systems
Chemical messengers that bridge the gap between physical and mental states, influencing mood, behavior, and physiological functions.
- • Serotonin: Mood, sleep, appetite
- • Dopamine: Motivation, reward
- • GABA: Anxiety, relaxation
Genetics and Behavior
Genetic factors contribute approximately 40-60% of the variance in many behavioral traits, including personality dimensions, cognitive abilities, and susceptibility to mental health conditions. Understanding genetic influences helps nurses appreciate individual differences in patient responses and develop personalized care approaches.
Memory Aid: GENES Framework
Heritability of Behavioral Traits
Key Genetic Mechanisms
Single Nucleotide Polymorphisms (SNPs)
Single DNA base variations affecting neurotransmitter function, drug metabolism, and stress response.
Epigenetic Modifications
Environmental influences on gene expression without changing DNA sequence.
Copy Number Variants
Deletions or duplications of DNA segments affecting brain development.
Nursing Implementation: Genetic Considerations
Assessment Strategies
- Comprehensive family history collection
- Three-generation pedigree analysis
- Ethnic and cultural background considerations
- Environmental exposure history
Care Planning
- Risk stratification based on genetic factors
- Personalized intervention approaches
- Medication selection considerations
- Lifestyle modification recommendations
Patient Education
- Genetic counseling referrals when appropriate
- Risk communication and interpretation
- Preventive strategies discussion
- Family planning considerations
Inheritance of Behavior
Behavioral inheritance involves complex patterns of genetic transmission that influence temperament, cognitive abilities, and predisposition to psychological conditions. Understanding these inheritance patterns helps nurses anticipate potential behavioral challenges and implement preventive interventions across the lifespan.
Mendelian Inheritance
Simple dominant/recessive patterns affecting specific behavioral traits, such as certain forms of intellectual disability or metabolic disorders affecting behavior.
- • Huntington’s disease (autosomal dominant)
- • Phenylketonuria behavioral effects (autosomal recessive)
- • Fragile X syndrome (X-linked)
Polygenic Inheritance
Multiple genes contribute to behavioral traits, creating continuous distributions rather than discrete categories.
- • Intelligence and cognitive abilities
- • Personality dimensions (Big Five)
- • Susceptibility to mood disorders
Epigenetic Inheritance
Environmental influences on gene expression that can be transmitted across generations without DNA sequence changes.
- • Trauma and stress exposure
- • Nutritional influences
- • Early life experiences
Behavioral Inheritance Flowchart
Clinical Applications in Nursing
Risk Assessment Tools
Systematic collection of behavioral health information across three generations to identify patterns and risks.
Quantitative assessment of genetic burden for behavioral conditions based on family history and genetic testing.
Preventive Interventions
Screening protocols for at-risk individuals to enable early intervention and prevention strategies.
Targeted recommendations for stress management, nutrition, and environmental modifications to reduce risk expression.
Memory Aid: INHERIT Framework
Brain and Behavior
The human brain serves as the primary organ governing behavior through complex networks of neurons, neurotransmitters, and specialized regions. Understanding neuroanatomical structures and their functional relationships is essential for nurses to comprehend how brain injuries, diseases, and medications affect patient behavior and to develop appropriate interventions.
Major Brain Regions and Functions
Frontal Cortex
Executive functions, decision-making, personality, impulse control, working memory
Limbic System
Emotion regulation, memory formation, motivation, fear processing
Brainstem
Arousal, consciousness, sleep-wake cycles, autonomic functions
Neurotransmitter Systems
Dopamine System
Reward, motivation, motor control, attention
Serotonin System
Mood regulation, sleep, appetite, impulse control
GABA System
Inhibitory control, anxiety reduction, muscle relaxation
Nursing Applications: Neurological Assessment
Behavioral Assessment
- Level of consciousness (Glasgow Coma Scale)
- Cognitive function (Mini-Mental State Exam)
- Mood and affect evaluation
- Motor function and coordination
- Speech and language abilities
Warning Signs
- Sudden personality changes
- Altered level of consciousness
- New onset confusion or agitation
- Memory loss or disorientation
- Impaired judgment or reasoning
Interventions
- Environmental modifications for safety
- Cognitive stimulation activities
- Behavioral management strategies
- Family education and support
- Medication administration and monitoring
Memory Aid: BRAIN-WAVE Assessment
Psychology and Sensation: Sensory Processes
Sensory processes form the foundation of human perception and behavior by detecting, transmitting, and interpreting environmental stimuli. Understanding normal and abnormal sensory function is crucial for nurses to assess patient capabilities, modify care environments, and implement appropriate interventions for individuals with sensory impairments or alterations.
Sensory Processing Pathway
Sensation
Sensory receptors detect physical stimuli and convert them into neural signals
Transmission
Neural pathways carry sensory information to the brain for processing
Perception
Brain interprets and gives meaning to sensory information based on experience
Sensory Systems Overview
Normal vs. Abnormal Sensory Function
Normal Function
20/20 vision, normal color perception, adequate peripheral vision
Hearing threshold 0-25 dB, speech discrimination >90%
Normal two-point discrimination, intact pain and temperature sensation
Impaired Function
Reduced acuity, visual field defects, color blindness
Conductive or sensorineural hearing loss, tinnitus
Decreased sensation, paresthesia, numbness
Abnormal Function
False sensory perceptions without external stimuli
Excessive response to normal sensory stimuli
Inability to recognize objects despite intact sensation
Nursing Implementation: Sensory Assessment and Care
Comprehensive Sensory Assessment
- • Visual acuity testing (Snellen chart)
- • Visual field evaluation
- • Pupil response and accommodation
- • Eye movement and coordination
- • Whisper test and Weber test
- • Rinne test for conduction
- • Audiometry when indicated
- • Ear canal and tympanic membrane inspection
- • Light touch and pressure sensation
- • Two-point discrimination testing
- • Pain and temperature sensation
- • Vibration and position sense
Adaptive Interventions
- • Adequate lighting and contrast
- • Noise reduction strategies
- • Clear pathways and safety measures
- • Sensory stimulation or reduction as needed
- • Hearing aids and amplification devices
- • Visual aids and magnification tools
- • Communication boards and alternatives
- • Tactile feedback systems
- • Face-to-face positioning for lip reading
- • Clear, slow speech patterns
- • Written instructions and visual cues
- • Touch and gesture communication
Memory Aid: SENSES Assessment Framework
Summary and Key Takeaways
Essential Nursing Knowledge
Understanding the biological basis of human behavior equips nurses with the foundational knowledge needed to provide comprehensive, evidence-based care. The integration of genetics, neuroanatomy, sensory function, and psychological processes creates a framework for assessing, planning, and implementing individualized nursing interventions that address both physical and behavioral health needs.
Critical Concepts
- Holistic Assessment: Consider biological, psychological, and environmental factors in patient evaluation
- Individual Variability: Genetic and experiential differences influence patient responses and care needs
- Preventive Focus: Early identification and intervention can modify behavioral health outcomes
- Interdisciplinary Care: Collaboration enhances comprehensive behavioral health management
Clinical Applications
- Risk Assessment: Use genetic and family history to identify behavioral health risks
- Care Individualization: Tailor interventions based on sensory capabilities and neurological function
- Environmental Modification: Adapt care settings to support optimal sensory and cognitive function
- Patient Education: Provide appropriate information considering cognitive and sensory abilities
Integrated Nursing Care Model
References and Further Reading
Essential Textbooks
- Psychiatric Mental Health Nursing (Townsend & Morgan)
- Foundations of Psychiatric Mental Health Nursing (Varcarolis)
- Neuroscience for Nurses (Evans & Pearson)
Professional Resources
- American Psychiatric Nurses Association (APNA)
- National Institute of Mental Health (NIMH)
- International Society of Psychiatric-Mental Health Nurses
