Biology and Human Welfare
Complete Nursing Guide to Pathogens and Immunology
Health and Disease: Foundational Concepts
Understanding the dynamic relationship between health and disease forms the cornerstone of nursing practice. Health represents a state of complete physical, mental, and social well-being, not merely the absence of disease. This holistic definition, established by the World Health Organization, guides modern healthcare approaches and emphasizes the multifaceted nature of human wellness.
Key Concept: Disease Triangle
Disease occurrence depends on three interconnected factors: the host (patient), the agent (pathogens or other causative factors), and the environment. Understanding this triangle helps nurses implement comprehensive prevention strategies.
Disease manifests through various mechanisms, with infectious diseases caused by pathogens representing a significant category in healthcare settings. Pathogens disrupt normal physiological processes through direct cellular damage, toxin production, or immune system activation. The severity and progression of disease depend on factors including pathogen virulence, host immunity, and environmental conditions.
Clinical Application
Scenario: When assessing a patient with suspected pneumonia, nurses evaluate the disease triangle components: host factors (age, immunity, comorbidities), potential pathogens (Streptococcus pneumoniae, viruses), and environmental factors (recent hospitalization, community exposure).
Understanding Pathogens: Disease-Causing Microorganisms
Critical Knowledge for Nurses
Pathogens are microorganisms capable of causing disease in humans. Understanding pathogen characteristics, transmission modes, and control measures is essential for effective nursing practice and infection prevention.
| Pathogen Type | Characteristics | Common Examples | Nursing Implications |
|---|---|---|---|
| Bacteria | Single-celled prokaryotes, reproduce rapidly, produce toxins | Staphylococcus aureus, E. coli, Tuberculosis | Antibiotic therapy, strict asepsis, isolation precautions |
| Viruses | Non-cellular, require host cells for replication, highly specific | Influenza, COVID-19, Hepatitis B | Antiviral medications, vaccination, droplet precautions |
| Fungi | Eukaryotic organisms, opportunistic infections, spore formation | Candida albicans, Aspergillus, Dermatophytes | Antifungal therapy, moisture control, immunocompromised care |
| Parasites | Complex life cycles, host dependency, organ-specific tropism | Malaria parasites, Helminths, Protozoa | Antiparasitic drugs, vector control, sanitation measures |
Pathogens employ various strategies to establish infection and cause disease. These mechanisms include adhesion to host cells, invasion of tissues, immune system evasion, and toxin production. Understanding these pathogenic mechanisms enables nurses to recognize early signs of infection and implement appropriate interventions.
The virulence of pathogens varies significantly, influenced by factors such as genetic composition, environmental conditions, and host susceptibility. Some pathogens demonstrate high virulence, causing severe disease even in healthy individuals, while others primarily affect immunocompromised patients. This variability underscores the importance of individualized patient assessment and care planning.
Parasitic Infections: Complex Host-Pathogen Relationships
Types of Human Parasites
Protozoa
Single-celled organisms causing malaria, amoebiasis, and sleeping sickness
Helminths
Multicellular worms including roundworms, tapeworms, and flukes
Ectoparasites
External parasites like lice, mites, and fleas
Transmission Mechanisms
- Water-borne: Contaminated water sources transmit Giardia and Cryptosporidium
- Food-borne: Undercooked meat harbors Trichinella and Taenia species
- Vector-borne: Insects transmit malaria, leishmaniasis, and filariasis
- Direct contact: Person-to-person transmission of scabies and lice
Critical Nursing Alert
Parasitic infections often present with nonspecific symptoms, making diagnosis challenging. Nurses must maintain high clinical suspicion, especially in patients with travel history, immunocompromised states, or exposure to endemic areas.
Parasitic pathogens have evolved sophisticated mechanisms to survive within human hosts while evading immune responses. These organisms often exhibit complex life cycles involving multiple developmental stages and, in some cases, intermediate hosts. Understanding these cycles is crucial for nurses to recognize infection patterns and implement effective prevention strategies.
The clinical manifestations of parasitic infections vary widely depending on the organism, infection site, and host immune response. Some parasites cause acute symptoms immediately after infection, while others establish chronic infections with subtle, long-term health consequences. This diversity requires nurses to maintain broad differential diagnoses when assessing patients with unexplained symptoms.
Nursing Assessment Example
Patient Presentation: A 35-year-old patient presents with intermittent fever, fatigue, and recent travel to Southeast Asia. Nursing assessment includes detailed travel history, food and water consumption patterns, insect bite evaluation, and systematic symptom documentation to identify potential parasitic pathogens.
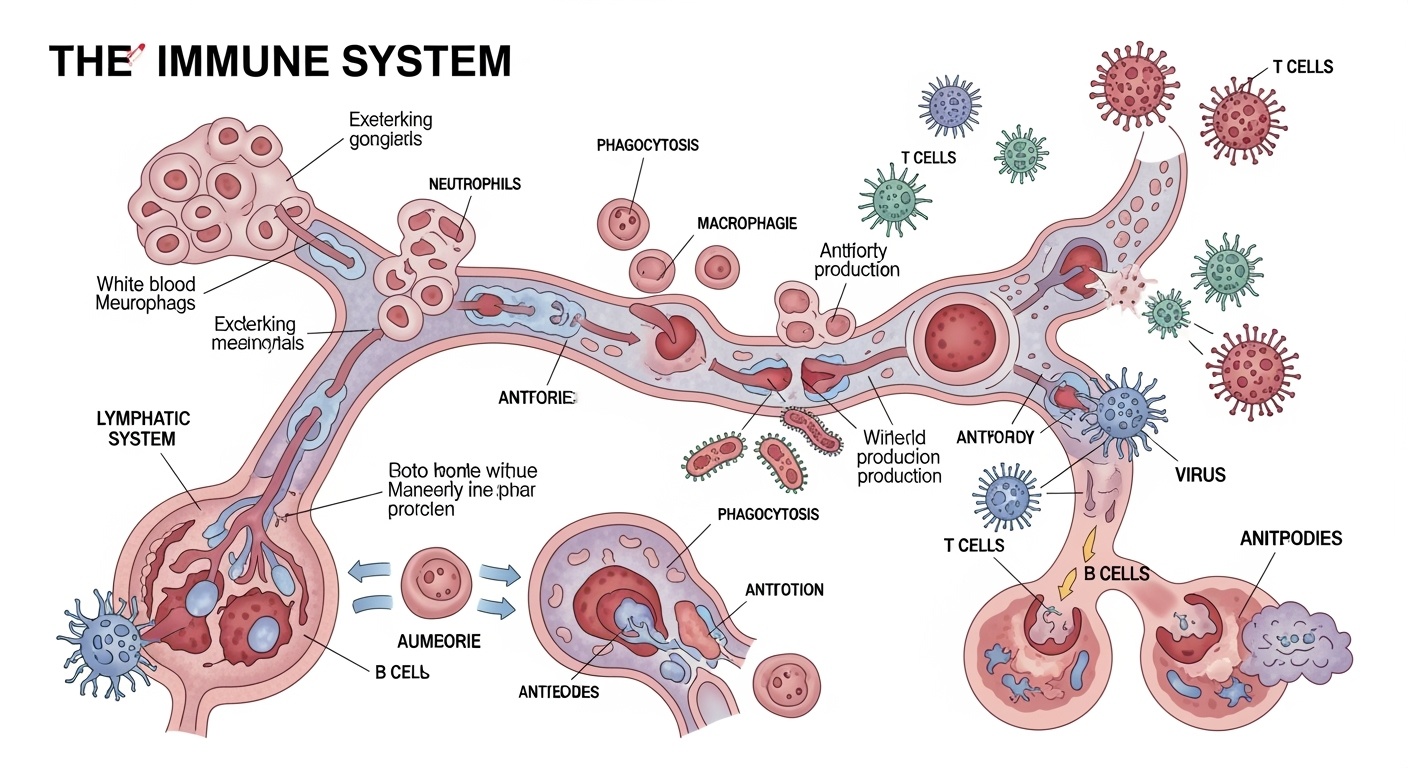
Basic Concepts of Immunology: Body’s Defense System
The Immune System: Your Body’s Army
The immune system represents a sophisticated network of cells, tissues, and organs working collectively to defend against pathogens and maintain homeostasis. For nurses, understanding immunology is essential for patient assessment, medication administration, and infection control practices.
Innate Immunity
- First line of defense against pathogens
- Non-specific immune responses
- Physical barriers (skin, mucous membranes)
- Cellular components (neutrophils, macrophages)
- Chemical mediators (complement, interferons)
Adaptive Immunity
- Specific responses to particular pathogens
- Memory formation for future encounters
- B cells producing antibodies
- T cells mediating cellular immunity
- Vaccination effectiveness basis
| Immune Cell Type | Primary Function | Clinical Significance | Nursing Considerations |
|---|---|---|---|
| Neutrophils | First responders to bacterial infections | Elevated in acute bacterial infections | Monitor for neutropenia in immunocompromised patients |
| Lymphocytes | Adaptive immune responses, memory formation | Increased in viral infections, decreased in immunodeficiency | Assess vaccination status, monitor for opportunistic infections |
| Macrophages | Phagocytosis, antigen presentation | Key in chronic inflammation and wound healing | Important in wound care assessment and healing progression |
| Eosinophils | Defense against parasites, allergic reactions | Elevated in parasitic infections and allergies | Consider parasitic screening in appropriate clinical contexts |
The immune response to pathogens involves a carefully orchestrated sequence of events beginning with pathogen recognition and culminating in pathogen elimination and memory formation. This process requires coordination between various immune cell types, chemical mediators, and anatomical structures. Disruption at any level can lead to increased susceptibility to infections or autoimmune diseases.
Immunocompromised patients represent a particularly vulnerable population requiring specialized nursing care. Conditions such as HIV/AIDS, cancer chemotherapy, organ transplantation, and advanced age can significantly impair immune function, increasing susceptibility to opportunistic pathogens that rarely cause disease in healthy individuals.
Immunology in Nursing Practice
Scenario: When caring for a post-chemotherapy patient, nurses must understand that reduced neutrophil counts increase infection risk from normally harmless pathogens. This knowledge guides implementation of protective isolation, strict hand hygiene, and early recognition of infection signs.
Microbes in Human Welfare: Beyond Pathogenic Roles
The Beneficial Side of Microbiology
While much attention focuses on pathogenic microorganisms, beneficial microbes play crucial roles in human welfare, environmental sustainability, and healthcare advancement. Understanding these positive applications helps nurses appreciate the broader context of microbiology in health promotion.
Sewage Treatment
Microorganisms break down organic waste, purifying water and protecting public health
Energy Generation
Biogas production through microbial fermentation provides sustainable energy alternatives
Biofertilizers
Beneficial bacteria enhance soil fertility and crop production naturally
Sewage Treatment Applications
Microorganisms form the backbone of modern wastewater treatment systems, transforming harmful pathogens and organic pollutants into harmless byproducts. Aerobic bacteria consume organic matter in activated sludge processes, while anaerobic microorganisms generate methane in digesters. These biological processes effectively remove pathogens, reducing disease transmission and protecting water resources.
Key Microbial Processes:
- Primary treatment: Physical separation and settling
- Secondary treatment: Biological degradation by microorganisms
- Tertiary treatment: Advanced microbial processes for pathogen removal
- Sludge treatment: Anaerobic digestion producing biogas
Biogas and Energy Generation
Anaerobic microorganisms convert organic waste into methane-rich biogas, providing renewable energy while reducing waste disposal problems. This process occurs in specially designed digesters where pathogens and other microorganisms work symbiotically to break down complex organic compounds. The resulting biogas can power healthcare facilities, particularly in resource-limited settings.
Healthcare Applications:
- Hospital waste management and energy recovery
- Rural clinic power generation from organic waste
- Sterilization equipment energy supply in remote areas
- Reduced healthcare carbon footprint through renewable energy
Biofertilizers and Food Security
Beneficial microorganisms enhance agricultural productivity through nitrogen fixation, phosphorus solubilization, and plant growth promotion. These biofertilizers reduce dependence on chemical fertilizers while improving soil health and crop yields. The connection to human health occurs through improved food security and reduced exposure to chemical residues, though nurses should be aware that some biofertilizers may occasionally harbor pathogens requiring proper handling.
Types of Beneficial Microorganisms:
- Rhizobium species: Nitrogen fixation in legumes
- Azotobacter: Free-living nitrogen fixers
- Phosphate-solubilizing bacteria: Enhance phosphorus availability
- Mycorrhizal fungi: Improve nutrient and water uptake
One Health Concept
The One Health approach recognizes the interconnection between human health, animal health, and environmental health. Beneficial microbes in environmental applications like sewage treatment and agriculture directly impact human health by reducing pathogen exposure and improving food security.
Nursing Applications and Clinical Implications
Infection Prevention and Control
Standard Precautions
Apply to all patients regardless of infection status, assuming all body fluids may contain pathogens
Transmission-Based Precautions
Additional measures for patients with known or suspected infections with specific pathogens
Hand Hygiene
Most effective single measure to prevent transmission of pathogens in healthcare settings
Patient Assessment and Monitoring
Early Recognition
Identify subtle signs of infection, especially in immunocompromised patients
Risk Assessment
Evaluate patient factors that increase susceptibility to specific pathogens
Systematic Monitoring
Track vital signs, laboratory values, and clinical symptoms for infection indicators
Critical Nursing Competencies
Microbiological Knowledge
- • Understanding pathogen characteristics and behavior
- • Recognizing transmission patterns and risk factors
- • Interpreting laboratory results and culture reports
- • Knowledge of antimicrobial resistance patterns
Immunological Assessment
- • Evaluating immune status and vaccination history
- • Recognizing immunocompromised states
- • Understanding inflammatory responses
- • Monitoring for adverse immunological reactions
Case Study: Multidrug-Resistant Pathogen Management
Scenario: A 68-year-old diabetic patient develops a wound infection with methicillin-resistant Staphylococcus aureus (MRSA), a challenging pathogen requiring specialized nursing interventions.
Nursing Assessments
- • Wound appearance, drainage, and odor documentation
- • Systemic infection signs (fever, elevated WBC)
- • Patient’s immune status and risk factors
- • Previous antibiotic exposure history
Interventions
- • Contact isolation precautions implementation
- • Proper wound care with sterile technique
- • Antibiotic administration per sensitivity results
- • Patient and family education on prevention
Antimicrobial Stewardship
Nurses play a crucial role in antimicrobial stewardship by ensuring appropriate antibiotic administration, monitoring for adverse effects, and educating patients about proper medication compliance. Understanding how pathogens develop resistance helps nurses advocate for responsible antibiotic use.
Key Takeaways for Nursing Practice
Pathogen Understanding
Comprehensive knowledge of pathogens, their characteristics, and transmission mechanisms forms the foundation for effective infection prevention and patient care.
Immune System Support
Understanding immunology enables nurses to support patient immunity through vaccination advocacy, nutrition counseling, and recognition of immunocompromised states.
Holistic Perspective
Recognizing beneficial microbes and their role in human welfare provides a balanced understanding of microbiology beyond pathogenic relationships.
Excellence in nursing requires continuous learning and application of microbiological principles
Stay updated with current research, maintain evidence-based practice, and prioritize patient safety through infection prevention measures.
