Bleeding in Early Pregnancy
Abortion, Ectopic Pregnancy, and Vesicular Mole
Comprehensive Nursing Education Notes
Table of Contents
Introduction to Early Pregnancy Hemorrhage
Early pregnancy hemorrhage is a critical condition that occurs within the first 20 weeks of gestation and may indicate serious complications. It represents a significant cause of maternal morbidity and mortality worldwide. Nurses play a pivotal role in recognizing signs of abnormal bleeding, assessing the patient’s condition, and implementing timely interventions.
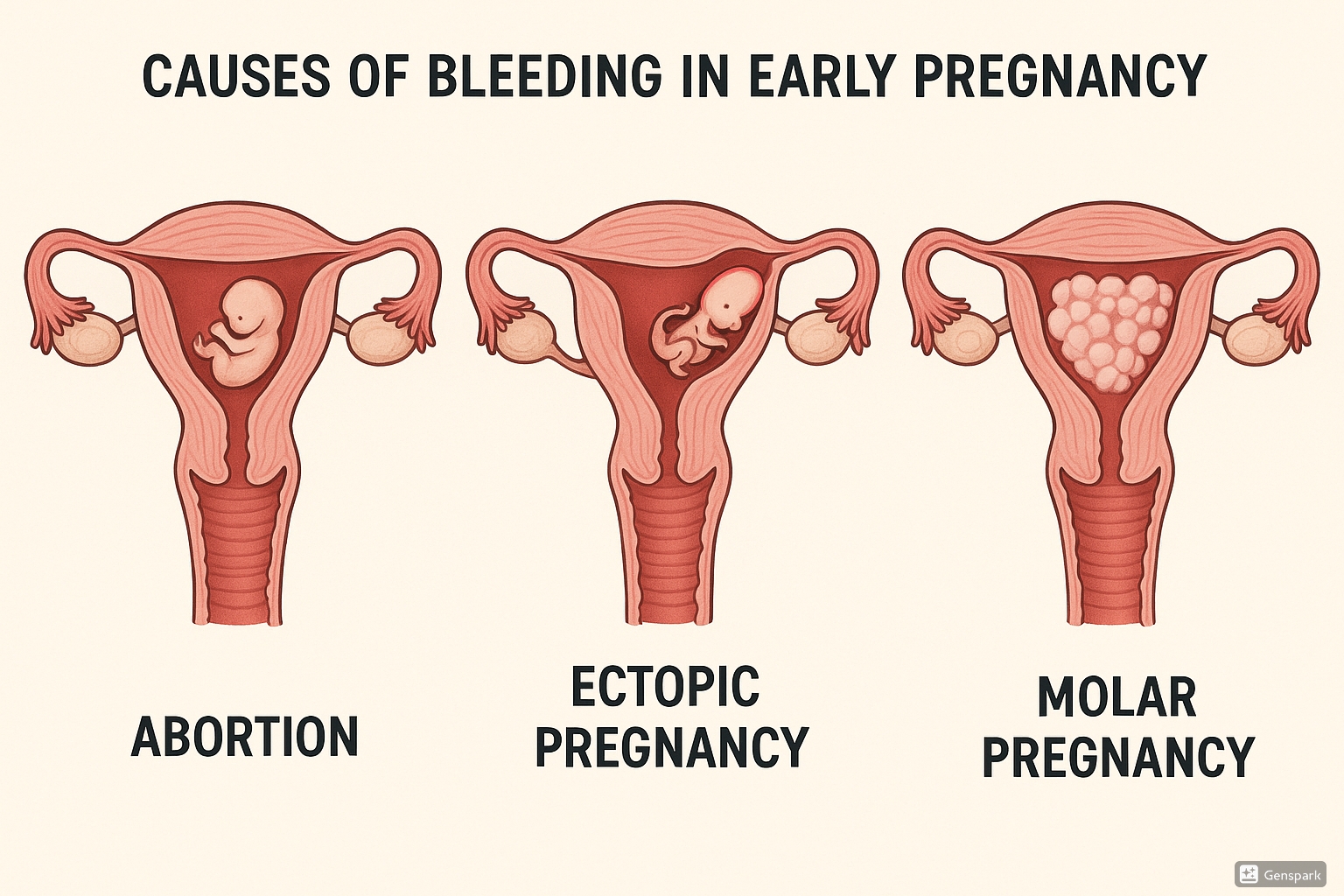
Vaginal bleeding in early pregnancy affects approximately 20-30% of all pregnancies. While many cases resolve without complications, significant hemorrhage requires immediate medical attention and may indicate one of three major conditions:
- Abortion (Miscarriage): Spontaneous or induced termination of pregnancy before 20 weeks gestation
- Ectopic Pregnancy: Implantation of fertilized ovum outside the uterine cavity, most commonly in the fallopian tube
- Vesicular (Hydatidiform) Mole: Abnormal proliferation of trophoblastic tissue with potential for malignant transformation
Key Nursing Consideration
Every pregnant woman presenting with vaginal bleeding should be assessed for hemodynamic stability. Vital signs monitoring is critical to detect signs of hypovolemic shock due to excessive hemorrhage.
Abortion (Miscarriage)
Abortion refers to the termination of pregnancy before 20 weeks gestation or when the fetus weighs less than 500 grams. Spontaneous abortion (miscarriage) occurs in approximately 10-15% of clinically recognized pregnancies, with the majority occurring in the first trimester due to chromosomal abnormalities.
Types of Abortion
| Type | Characteristics | Clinical Presentation | Bleeding Risk |
|---|---|---|---|
| Threatened Abortion | Vaginal bleeding with a closed cervical os | Mild cramping, minimal hemorrhage | Low to moderate |
| Inevitable Abortion | Vaginal bleeding with dilated cervical os | Moderate to severe cramping, moderate hemorrhage | Moderate |
| Incomplete Abortion | Partial expulsion of products of conception | Severe cramping, heavy hemorrhage | High |
| Complete Abortion | Total expulsion of products of conception | Diminishing cramping, decreasing hemorrhage | Initially high, then decreasing |
| Missed Abortion | Fetal demise without expulsion | Absence of fetal heart tones, brown vaginal discharge | Low, but risk of DIC with prolonged retention |
| Septic Abortion | Infection of the products of conception | Fever, purulent discharge, uterine tenderness | Moderate to high, with septic shock risk |
| Recurrent Abortion | Three or more consecutive spontaneous abortions | Repeated pattern of early pregnancy loss | Variable |
For remembering types of abortion:
- Missed abortion
- Inevitable abortion
- Septic abortion
- Complete abortion
- Abortion (threatened)
- Recurrent abortion
- Retained products (incomplete)
- Yields complications if untreated
Diagnosis
Diagnosis of abortion is based on clinical presentation, physical examination, laboratory tests, and ultrasound findings:
- History: Pregnancy symptoms, onset of vaginal bleeding, amount of hemorrhage, associated pain
- Physical Examination: Vital signs, abdominal examination, speculum examination to assess cervical dilatation and products of conception
- Laboratory Tests:
- Complete blood count to assess hemorrhage severity
- Quantitative β-hCG levels (may be decreasing or lower than expected)
- Blood type and Rh status
- Coagulation profile if significant bleeding
- Ultrasound: Transvaginal ultrasound to evaluate gestational sac, fetal pole, cardiac activity, and retained products
Management
Management depends on the type of abortion and clinical presentation:
| Type | Management Approach |
|---|---|
| Threatened Abortion |
|
| Inevitable/Incomplete Abortion |
|
| Complete Abortion |
|
| Missed Abortion |
|
| Septic Abortion |
|
| Recurrent Abortion |
|
Nursing Care
Physical Care
- Monitor vital signs, especially for signs of hypovolemic shock
- Quantify hemorrhage using standardized methods (count pads, weigh)
- Administer IV fluids as ordered
- Administer pain medication as prescribed
- Prepare patient for procedures (D&C, medication administration)
- Observe for signs of infection (fever, foul-smelling discharge)
- Monitor laboratory values (hemoglobin, hematocrit, WBC)
- Preserve expelled tissue for pathological examination
Psychosocial Care
- Provide emotional support and create a supportive environment
- Acknowledge the loss and grief
- Provide information about the grieving process
- Involve support persons when appropriate
- Offer spiritual support as desired by the patient
- Provide referrals to support groups and counseling
- Discuss future conception plans when appropriate
- Document patient’s emotional responses
Critical Nursing Alert
Monitor patients with abortion for signs of excessive hemorrhage including tachycardia, hypotension, pallor, dizziness, and decreased urinary output. Report significant blood loss (>500 mL) or hemodynamic instability immediately.
Ectopic Pregnancy
An ectopic pregnancy occurs when a fertilized ovum implants outside the uterine cavity. Approximately 95% of ectopic pregnancies occur in the fallopian tubes. This condition accounts for 2% of all pregnancies but is responsible for up to 9% of pregnancy-related deaths due to the risk of severe internal hemorrhage if rupture occurs.
| Location | Frequency | Hemorrhage Risk |
|---|---|---|
| Ampullary (fallopian tube) | 80% | High |
| Isthmic (fallopian tube) | 12% | Very high (earlier rupture) |
| Fimbrial (fallopian tube) | 5% | Moderate |
| Cornual/Interstitial | 2% | Extremely high (later rupture with massive hemorrhage) |
| Abdominal | <1% | Variable |
| Cervical | <1% | High |
| Ovarian | <1% | Moderate |
Etiology and Risk Factors
For remembering ectopic pregnancy risk factors:
- Tubal surgery or pathology (PID, surgery, endometriosis)
- Reproductive technology (IVF)
- Intrauterine device use
- Previous ectopic pregnancy
- Old age (advanced maternal age)
- Delayed ovulation/fertilization
Any condition that impairs or prevents the migration of the fertilized ovum to the uterine cavity can predispose to ectopic pregnancy. The most common cause is tubal damage from previous pelvic inflammatory disease (PID).
Diagnosis
Clinical Presentation
- Amenorrhea (missed period)
- Vaginal bleeding (usually lighter than normal period)
- Unilateral lower abdominal or pelvic pain
- Referred shoulder pain (diaphragmatic irritation from intraperitoneal blood)
- Syncope or dizziness if significant hemorrhage
- Urge to defecate (pressure on rectum)
- Positive pregnancy test
Diagnostic Tests
- Quantitative β-hCG (typically lower than expected for gestational age)
- Transvaginal ultrasound (empty uterus with adnexal mass)
- Culdocentesis (rarely performed now; positive for non-clotting blood)
- Complete blood count (may show anemia from hemorrhage)
- Laparoscopy (definitive diagnosis)
- Serial β-hCG measurements (slower rise than normal intrauterine pregnancy)
Emergency Recognition
The classic triad of ruptured ectopic pregnancy is:
- Amenorrhea (missed period)
- Abdominal/pelvic pain (severe, sudden, unilateral)
- Vaginal bleeding
However, only about 50% of patients present with this classic triad. Any woman of reproductive age presenting with acute abdominal pain should be evaluated for ectopic pregnancy.
Management
Management of ectopic pregnancy depends on the patient’s clinical status, desire for future fertility, location and size of the ectopic mass, and β-hCG level:
| Treatment Option | Indications | Nursing Considerations |
|---|---|---|
| Medical Management (Methotrexate) |
|
|
| Surgical Management (Laparoscopy or Laparotomy) |
|
|
| Expectant Management |
|
|
Nursing Care
Emergency Care
- Establish large-bore IV access (16-18 gauge)
- Administer crystalloid fluids for volume replacement
- Monitor vital signs frequently (every 5-15 minutes if unstable)
- Assess for signs of hypovolemic shock from hemorrhage
- Prepare for emergency surgery if rupture suspected
- Administer O-negative blood if massive hemorrhage present
- Maintain NPO status in case surgery is needed
- Document intake/output and bleeding
Post-Treatment Care
- Provide pain management
- Administer anti-D immunoglobulin if Rh-negative
- Monitor for signs of infection
- Educate about follow-up appointments
- Discuss contraception (delay pregnancy for 3 months)
- Provide emotional support for pregnancy loss
- Discuss increased risk for future ectopic pregnancies
- Prepare discharge education on warning signs
Patient Education Topics
- Signs of recurrent ectopic pregnancy in future pregnancies
- Importance of early prenatal care in future pregnancies
- Warning signs of complications after treatment (fever, increased pain, heavy bleeding)
- Sexual activity restrictions during recovery
- Risk factors for ectopic pregnancy and how to minimize them
Vesicular Mole (Hydatidiform Mole)
A vesicular (hydatidiform) mole is an abnormal form of pregnancy characterized by trophoblastic proliferation and hydropic degeneration of placental villi. It is part of a spectrum of gestational trophoblastic diseases (GTD) and can lead to persistent trophoblastic disease or choriocarcinoma if not properly managed.
Etiology and Types
The incidence of vesicular mole varies geographically, with higher rates in Southeast Asia (1 in 120 pregnancies) compared to North America and Europe (1 in 1,500 pregnancies). Risk factors include:
- Maternal age <20 or >35 years (especially >40)
- Previous molar pregnancy (7-10 times increased risk)
- Dietary deficiencies (low protein, folic acid, carotene)
- Asian ethnicity
- Blood group A female with blood group O male (controversial)
| Type | Genetic Features | Characteristics | Malignant Potential |
|---|---|---|---|
| Complete Mole | 46,XX (90%) – all paternal origin Usually from single sperm fertilizing empty egg |
|
15-20% develop persistent GTD |
| Partial Mole | Triploid (69,XXY or 69,XXX) Two paternal sets + one maternal set |
|
2-4% develop persistent GTD |
Diagnosis
Clinical Presentation
- Vaginal bleeding (often brownish hemorrhage)
- Uterus larger than dates (in 50%)
- Severe nausea and vomiting (hyperemesis gravidarum)
- Early preeclampsia (before 20 weeks)
- Passage of grape-like vesicles
- Hyperthyroidism symptoms (tachycardia, tremors)
- Anemia (from chronic bleeding)
- No fetal heart tones or movements
Diagnostic Tests
- Ultrasound: “snowstorm” appearance with multiple cystic spaces
- Extremely elevated β-hCG (often >100,000 mIU/mL)
- Complete blood count (may show anemia)
- Thyroid function tests (may show hyperthyroidism)
- Chest X-ray (to rule out metastasis)
- Histopathological examination after evacuation
- Liver and renal function tests
- Coagulation profile
Management
The primary treatment for vesicular mole is evacuation of the uterine contents, followed by close monitoring to detect persistent disease:
- Pre-evacuation Assessment:
- Evaluate for anemia, electrolyte imbalance, coagulopathy
- Assess thyroid function
- Screen for metastatic disease
- Cross-match blood for potential hemorrhage
- Uterine Evacuation:
- Suction curettage (method of choice)
- Oxytocin administration after evacuation begins
- Careful monitoring for hemorrhage
- Histopathological examination of all evacuated tissue
- Post-evacuation Follow-up:
- Weekly β-hCG until negative for 3 consecutive weeks
- Monthly β-hCG for 6-12 months
- Reliable contraception for at least 1 year
- Chest X-ray every 2 months for 6 months
- Treatment of Persistent Disease:
- Chemotherapy (methotrexate or actinomycin D for low-risk)
- Combination chemotherapy (EMA-CO) for high-risk disease
- Hysterectomy may be considered for women who have completed childbearing
For vesicular mole management approach:
- Monitor β-hCG levels regularly
- Oxytocics after evacuation begins
- Long-term contraception (1 year)
- Avoid pregnancy for at least 1 year
- Report any abnormal bleeding promptly
Nursing Care
Pre-evacuation Care
- Monitor vital signs
- Assess bleeding patterns and quantify hemorrhage
- Establish IV access
- Prepare for excessive bleeding during procedure
- Provide emotional support
- Explain procedure and expectations
- Assist with diagnostic tests
Post-evacuation Care
- Monitor for hemorrhage and infection
- Assess vital signs and uterine tone
- Administer oxytocics as ordered
- Examine evacuated material
- Monitor for respiratory distress (trophoblastic embolization)
- Assess pain and provide analgesia
- Provide emotional support for pregnancy loss
Long-term Follow-up Care
- Educate about importance of follow-up β-hCG monitoring
- Discuss contraceptive options
- Emphasize importance of avoiding pregnancy for 1 year
- Teach self-assessment for abnormal bleeding
- Educate about increased risk in future pregnancies
- Provide referrals for emotional/psychological support
- Coordinate follow-up appointments
Critical Nursing Consideration
A vesicular mole has the potential for massive hemorrhage during evacuation due to the highly vascular nature of the trophoblastic tissue. Always have blood products available and monitor the patient closely for signs of hypovolemic shock and trophoblastic embolization (sudden chest pain, dyspnea, hypoxemia).
Best Practices Worldwide
United Kingdom
The UK’s Early Pregnancy Assessment Units (EPAUs) provide specialized care for women experiencing bleeding in early pregnancy.
- Direct referral pathway for GPs and emergency departments
- Standardized protocols for hemorrhage management
- Dedicated nursing staff trained in early pregnancy complications
- Psychological support services integrated into care pathway
- National registry for vesicular moles with centralized follow-up
Netherlands
The Dutch healthcare system emphasizes midwifery care with clear referral pathways for complications:
- Risk assessment tools for ectopic pregnancy
- Expectant management protocols for stable patients
- Community follow-up for patients after early pregnancy loss
- Standardized bereavement support
- National guideline for management of early pregnancy hemorrhage
Australia
Australia has developed comprehensive telehealth services for rural areas:
- Remote assessment protocols for early pregnancy bleeding
- Flying doctor services for emergency evacuation
- Virtual consultation with specialists for remote nurses
- Point-of-care ultrasound training for rural practitioners
- Standardized algorithm for hemorrhage risk assessment
Innovative Global Approaches
Technology Integration
- Smartphone apps for tracking β-hCG trends after ectopic treatment
- Telemedicine follow-up for rural patients after molar evacuation
- Portable ultrasound devices with AI-assisted interpretation
- Online support groups for patients experiencing pregnancy loss
- Electronic health record alerts for missed follow-up appointments
Psychological Support
- Integration of mental health screening in early pregnancy units
- Culturally sensitive bereavement care protocols
- Partner-inclusive counseling after pregnancy loss
- Memory-making options after pregnancy loss
- Long-term follow-up for psychological wellbeing
Implementation Suggestion
Nursing units can develop a “Bleeding in Early Pregnancy” toolkit containing:
- Assessment checklists for different types of early pregnancy hemorrhage
- Patient education materials in multiple languages
- Bereavement support resources
- Referral pathways to specialized services
- Follow-up schedule templates for different conditions
Summary
Bleeding in early pregnancy represents a spectrum of conditions that require prompt assessment and appropriate management. Nurses play a crucial role in identifying the cause of hemorrhage, providing appropriate care, and supporting patients through potentially traumatic experiences.
| Condition | Key Distinguishing Features | Critical Nursing Interventions |
|---|---|---|
| Abortion | Uterine cramping, passage of tissue, open cervical os | Quantify bleeding, preserve tissue, emotional support |
| Ectopic Pregnancy | Unilateral pain, adnexal mass, empty uterus on ultrasound | Monitor for shock, prepare for emergency surgery |
| Vesicular Mole | Uterus larger than dates, grape-like vesicles, very high β-hCG | Prepare for excessive hemorrhage during evacuation, educate about follow-up |
Understanding the pathophysiology, clinical presentation, and management of these conditions enables nurses to provide safe, evidence-based care to women experiencing bleeding in early pregnancy. Prompt recognition of potential complications and timely intervention can prevent severe hemorrhage and improve patient outcomes.
