Breast Self-Examination
Complete Nursing Guide for Early Detection
Table of Contents
Introduction to Breast Self-Examination
Breast self-examination (BSE) represents a fundamental component of women’s healthcare and early detection strategies for breast cancer. As nursing professionals, understanding the comprehensive approach to breast self-examination enables us to provide evidence-based patient education and support early intervention protocols. This examination technique empowers women to become familiar with the normal characteristics of their breast tissue, facilitating the identification of potential changes that warrant professional evaluation.
The practice of breast self-examination has evolved significantly over the past decades, with current guidelines emphasizing breast awareness rather than rigid monthly examinations. However, the fundamental principles and techniques of breast self-examination remain crucial knowledge for nursing students and practitioners. Understanding these principles enables nurses to educate patients effectively about breast health maintenance and early detection strategies.
Key Learning Objectives
- Understand the anatomy and physiology relevant to breast self-examination
- Master the systematic approach to conducting breast self-examination
- Differentiate between normal and abnormal breast findings
- Develop effective patient education strategies for breast self-examination
- Implement appropriate documentation and follow-up protocols
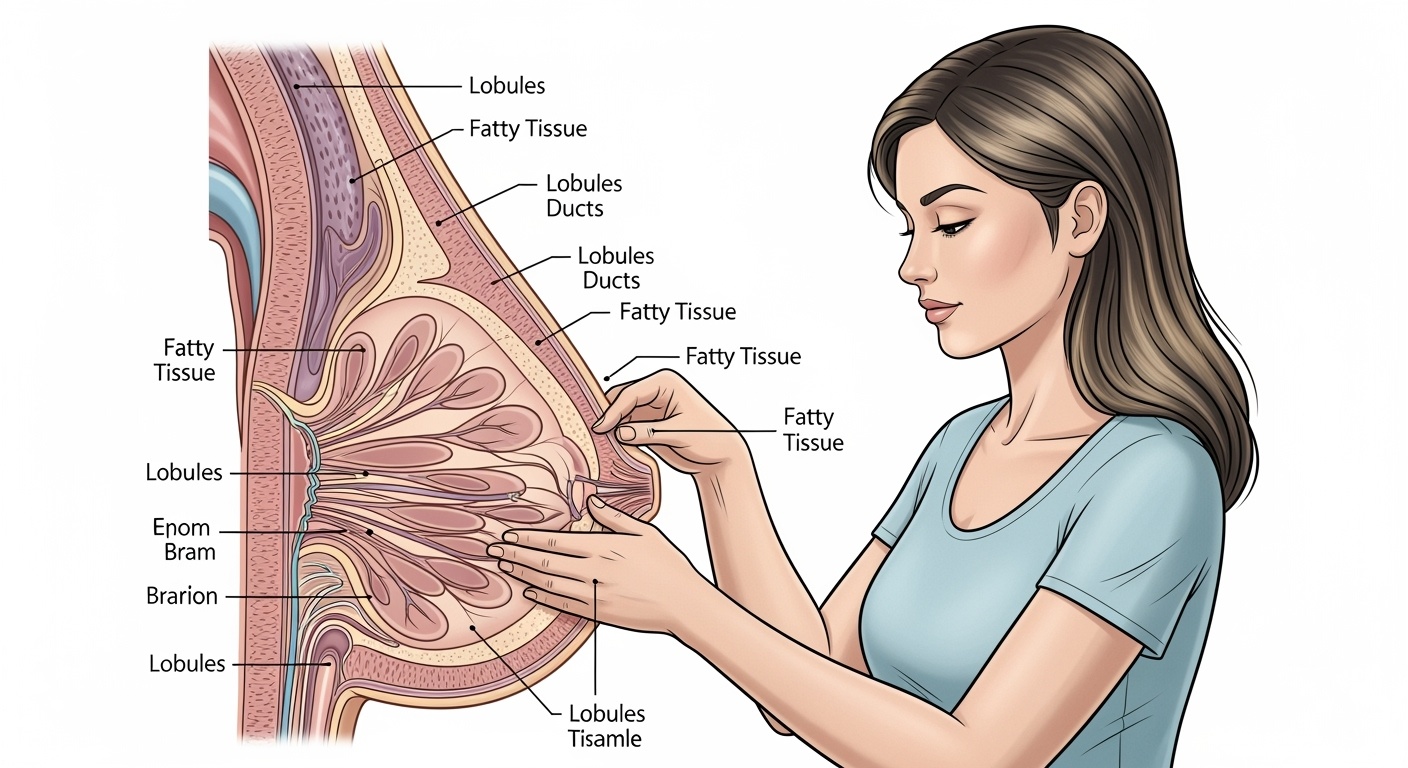
Breast Anatomy and Physiology
Understanding breast anatomy forms the foundation for effective breast self-examination instruction and interpretation. The breast consists of glandular tissue, supportive stroma, and overlying skin, with significant anatomical variations among individuals. This knowledge enables nurses to provide accurate patient education regarding normal breast characteristics and potential areas of concern during breast self-examination.
Anatomical Structures
Glandular Tissue
- 15-20 mammary ducts extending from nipple
- Lobular structures containing milk-producing cells
- Ductal system for milk transport
- Hormonal responsiveness throughout menstrual cycle
Supporting Structures
- Cooper’s ligaments providing structural support
- Pectoralis major muscle beneath breast tissue
- Fatty tissue comprising majority of breast volume
- Lymphatic drainage system for immune function
Physiological Variations
Breast tissue undergoes continuous changes throughout a woman’s life, influenced by hormonal fluctuations, age, and reproductive status. During breast self-examination education, nurses must emphasize these normal variations to prevent unnecessary anxiety while maintaining vigilance for pathological changes. Understanding these physiological patterns enhances the effectiveness of breast self-examination as a screening tool.
Clinical Importance of Breast Self-Examination
The clinical significance of breast self-examination extends beyond simple cancer detection to encompass comprehensive breast health awareness and patient empowerment. While mammography remains the gold standard for breast cancer screening, breast self-examination serves as a complementary tool that enhances overall breast health monitoring. Nursing professionals play a crucial role in educating patients about the appropriate integration of breast self-examination into their healthcare routine.
Early Detection
Facilitates identification of breast changes between clinical examinations
Breast Awareness
Develops familiarity with normal breast characteristics and patterns
Patient Empowerment
Encourages active participation in personal healthcare management
Statistical Significance
| Detection Method | Percentage of Cancers Detected | Average Tumor Size |
|---|---|---|
| Breast Self-Examination | 25-30% | 2.1 cm |
| Clinical Examination | 20-25% | 1.8 cm |
| Mammography | 45-50% | 1.1 cm |
Pre-Examination Preparation
Proper preparation significantly enhances the effectiveness and accuracy of breast self-examination. Nurses must educate patients about optimal timing, environmental considerations, and psychological preparation to ensure successful implementation of breast self-examination techniques. This preparation phase establishes the foundation for consistent and thorough breast health monitoring.
Optimal Timing
Premenopausal Women
Perform breast self-examination 7-10 days after menstruation begins when breast tissue is least tender and swollen.
- Hormonal levels are most stable
- Breast tissue density is minimized
- Optimal palpation sensitivity
Postmenopausal Women
Choose a consistent date each month, such as the first day of the month, for regular breast self-examination.
- Establish routine examination schedule
- Maintain consistency for comparison
- Consider calendar reminders
Environmental Preparation
Creating an appropriate environment for breast self-examination enhances patient comfort and examination thoroughness. Nurses should emphasize the importance of privacy, adequate lighting, and comfortable positioning to facilitate effective breast self-examination performance. These environmental factors contribute significantly to the quality and consistency of the examination process.
Essential Preparation Elements
- Private, comfortable environment free from interruptions
- Good lighting to visualize breast contours and skin changes
- Large mirror for visual inspection
- Comfortable room temperature to prevent muscle tension
- Adequate time allocation without rushing
Step-by-Step Breast Self-Examination Procedure
The systematic approach to breast self-examination involves both visual inspection and palpation techniques. Nursing education must emphasize the importance of following a consistent, methodical approach to ensure comprehensive examination of all breast tissue. This standardized procedure enhances the detection of subtle changes and maintains examination reliability over time.
Phase 1: Visual Inspection
1 Arms at Sides Position
Stand before a mirror with arms relaxed at sides. Observe both breasts for overall symmetry, size variations, and skin characteristics. This position allows natural breast positioning for baseline assessment during breast self-examination.
- Note natural breast contour and positioning
- Observe skin color and texture uniformity
- Identify any visible lumps or indentations
- Check nipple position and appearance
2 Arms Raised Position
Raise both arms overhead and observe breast changes with muscle contraction. This position reveals skin dimpling, asymmetry, or other abnormalities that may not be visible during relaxed positioning in breast self-examination.
- Look for skin pulling or dimpling
- Note changes in breast shape or contour
- Observe nipple direction and symmetry
- Check for unusual bulging or indentations
3 Hands on Hips Position
Place hands firmly on hips and press inward to contract chest muscles. This position emphasizes the underlying muscle structure and may reveal subtle skin changes during breast self-examination assessment.
- Contract pectoral muscles by pressing hands into hips
- Observe for skin dimpling or retraction
- Note any asymmetrical muscle contraction effects
- Look for changes in breast mobility
Phase 2: Palpation Technique
4 Lying Position Setup
Lie flat with a pillow or folded towel under the shoulder of the breast being examined. This position distributes breast tissue evenly across the chest wall, facilitating thorough palpation during breast self-examination.
- Place pillow under right shoulder for right breast examination
- Raise right arm above head or place behind neck
- Ensure comfortable, stable positioning
- Switch sides for left breast examination
5 Palpation Technique
Use the pad portions of the three middle fingers to apply varying pressure levels. Move fingers in small circular motions, covering all breast tissue systematically during breast self-examination palpation.
- Light pressure: superficial tissue assessment
- Medium pressure: middle tissue layer evaluation
- Deep pressure: tissue against chest wall
- Maintain finger contact throughout examination
6 Systematic Coverage Pattern
Follow a consistent pattern such as vertical strips, spiral, or wedge method to ensure complete breast tissue coverage. The vertical strip method is most commonly recommended for comprehensive breast self-examination.
- Start at the armpit and move vertically down
- Move across breast in parallel lines
- Include area from collarbone to bra line
- Extend from breastbone to armpit area
Critical Examination Areas
Pay special attention to the upper outer quadrant and axillary tail, where approximately 50% of breast cancers develop. Include examination of lymph node regions in the armpit, above the collarbone, and below the collarbone during comprehensive breast self-examination.
Normal vs. Abnormal Findings in Breast Self-Examination
Distinguishing between normal and abnormal findings constitutes a critical component of breast self-examination education. Nurses must provide clear, specific guidance to help patients identify concerning changes while recognizing normal anatomical variations. This knowledge prevents unnecessary anxiety while maintaining appropriate vigilance for pathological conditions requiring medical evaluation.
Normal Findings
Breast Tissue Characteristics
- Natural asymmetry between breasts
- Firm, elastic tissue consistency
- Smooth, even skin texture
- Moveable, soft fatty tissue areas
Cyclical Changes
- Premenstrual breast tenderness
- Temporary size variations
- Hormonal sensitivity patterns
- Mild texture changes with cycle
Abnormal Findings
Concerning Physical Changes
- New lumps or thickened areas
- Skin dimpling or puckering
- Nipple inversion or discharge
- Persistent breast pain
Visual Abnormalities
- Orange peel skin appearance
- Unusual redness or warmth
- Size or shape changes
- Visible lumps or bulging
Breast Self-Examination Decision Tree
| Finding Type | Characteristics | Recommended Action | Timeframe |
|---|---|---|---|
| New Discrete Lump | Hard, immobile, painless | Immediate medical evaluation | Within 1-2 weeks |
| Nipple Discharge | Bloody, spontaneous, unilateral | Medical assessment required | Within 2-4 weeks |
| Skin Changes | Dimpling, puckering, redness | Professional examination | Within 2-3 weeks |
| Cyclical Tenderness | Bilateral, premenstrual | Continue monitoring | Next routine visit |
Patient Education Guidelines for Breast Self-Examination
Effective patient education regarding breast self-examination requires a comprehensive, culturally sensitive approach that addresses individual learning needs and concerns. Nurses must develop educational strategies that promote long-term adherence to breast self-examination practices while addressing common barriers and misconceptions. This educational foundation empowers patients to take active roles in their breast health management.
Educational Strategies
Hands-On Demonstration
- Use breast models for technique practice
- Guide patient through proper finger positioning
- Demonstrate pressure variations and patterns
- Allow return demonstration for skill validation
Educational Materials
- Provide written instructions with illustrations
- Share video resources for technique review
- Offer multilingual educational materials
- Create personalized reminder systems
Communication Techniques
- Use clear, non-medical language
- Address cultural sensitivities and beliefs
- Encourage questions and open dialogue
- Provide reassurance about normal variations
Addressing Common Concerns
Fear and Anxiety Management
Many patients experience anxiety about performing breast self-examination due to fear of finding abnormalities. Nurses must address these concerns through education about breast cancer statistics, early detection benefits, and the low probability of cancer in young women.
- Normalize anxiety as common response
- Emphasize empowerment through knowledge
- Discuss statistical reassurance appropriately
- Provide coping strategies for examination anxiety
Technique Confidence Building
Patients often worry about performing breast self-examination incorrectly or missing important findings. Building confidence requires repeated practice, validation of technique, and reassurance about learning curves in developing examination skills.
- Emphasize that proficiency develops over time
- Validate correct technique performance
- Encourage regular practice for skill development
- Provide follow-up opportunities for questions
Key Educational Messages for Breast Self-Examination
- Breast self-examination complements but does not replace professional screening
- Most breast lumps discovered are benign and non-cancerous
- Familiarity with normal breast characteristics enhances change detection
- Early detection significantly improves treatment outcomes
- Professional evaluation is always available for concerning findings
Documentation and Follow-up for Breast Self-Examination
Comprehensive documentation of breast self-examination education and patient responses ensures continuity of care and facilitates ongoing assessment of patient compliance and concerns. Nurses must maintain detailed records that support quality improvement initiatives and provide evidence of patient education effectiveness. This documentation serves both clinical and legal purposes in healthcare delivery.
Documentation Components
| Documentation Component | Required Details | Example Documentation |
|---|---|---|
| Education Provided | Topics covered, methods used, duration | “BSE instruction provided using demonstration model, 30 minutes, all techniques demonstrated” |
| Patient Response | Understanding level, questions asked, concerns | “Patient verbalized understanding, expressed concern about technique accuracy” |
| Return Demonstration | Technique accuracy, areas needing reinforcement | “Patient performed BSE correctly with minimal guidance, reviewed palpation pressure” |
| Follow-up Plan | Next education session, monitoring schedule | “Follow-up BSE review scheduled for next visit, provided written materials” |
Follow-up Protocols
Systematic follow-up ensures continued patient adherence to breast self-examination practices and provides opportunities for ongoing education and support. Nurses should establish regular check-in schedules that align with routine healthcare visits while accommodating individual patient needs and risk factors.
Initial Follow-up (2-4 weeks)
- Assess technique retention and accuracy
- Address questions or concerns that arose
- Reinforce proper examination timing
- Evaluate comfort level with procedure
Ongoing Monitoring (3-6 months)
- Review adherence to examination schedule
- Discuss any findings or concerns
- Update technique as needed
- Coordinate with screening mammography
Special Considerations in Breast Self-Examination
Various patient populations require modified approaches to breast self-examination education and implementation. Nurses must consider individual factors such as age, reproductive status, medical history, and cultural background when providing breast self-examination instruction. These considerations ensure that education is relevant, appropriate, and effective for diverse patient populations.
Population-Specific Modifications
Pregnancy and Lactation
Breast changes during pregnancy and lactation require modified breast self-examination techniques and adjusted expectation setting. Nurses must educate patients about normal physiological changes while maintaining vigilance for pathological conditions.
- Expect increased breast size and sensitivity
- Modify palpation pressure for comfort
- Continue examinations despite tissue changes
- Recognize normal lactation-related findings
Elderly Patients
Age-related changes in dexterity, vision, and cognition may require adaptations to traditional breast self-examination techniques. Nurses should assess individual capabilities and provide appropriate modifications to ensure effective examination performance.
- Assess manual dexterity limitations
- Provide adequate lighting recommendations
- Consider caregiver involvement when appropriate
- Simplify instructions for cognitive limitations
High-Risk Patients
Patients with elevated breast cancer risk require enhanced education about breast self-examination while understanding its limitations in high-risk screening protocols. These patients often need more frequent professional surveillance complementing breast self-examination practices.
- Emphasize complementary role with enhanced screening
- Provide more frequent follow-up support
- Address anxiety related to increased risk
- Coordinate with specialized breast health services
Cultural Considerations
Cultural beliefs, values, and practices significantly influence patient acceptance and adherence to breast self-examination recommendations. Nurses must develop cultural competence to provide sensitive, appropriate education that respects individual beliefs while promoting optimal breast health practices.
Cultural Sensitivity Guidelines
- Respect modesty requirements and privacy preferences
- Address cultural beliefs about breast touching and examination
- Provide culturally appropriate educational materials
- Consider family involvement in healthcare decisions
- Acknowledge cultural perspectives on cancer and screening
Evidence-Based Practice in Breast Self-Examination
Current evidence regarding breast self-examination effectiveness continues to evolve, with nursing practice requiring integration of the most recent research findings and professional guidelines. Understanding the evidence base enables nurses to provide accurate, current information to patients while advocating for evidence-based breast health practices. This foundation supports informed patient decision-making and optimal health outcomes.
Current Research Findings
Recent studies have provided nuanced perspectives on breast self-examination effectiveness, moving beyond simple cancer detection rates to consider broader impacts on breast health awareness and patient empowerment. Nurses must understand these research findings to provide balanced, evidence-based education that accurately represents both benefits and limitations of breast self-examination practices.
Research Benefits
- Increased breast health awareness and knowledge
- Enhanced patient engagement in healthcare
- Improved communication with healthcare providers
- Early detection of interval cancers
- Reduced anxiety through familiarity
Research Limitations
- No significant mortality reduction demonstrated
- Potential for increased false positive findings
- Variable technique quality among patients
- Limited effectiveness in detecting small tumors
- Possible delay in professional screening compliance
Professional Guidelines
Major healthcare organizations have developed nuanced recommendations regarding breast self-examination that emphasize informed choice and breast awareness rather than mandatory monthly examinations. Nurses must understand these evolving guidelines to provide current, appropriate guidance to patients seeking breast health information.
| Organization | Current Recommendation | Key Rationale |
|---|---|---|
| American Cancer Society | Optional, informed choice for women 20+ | Emphasizes breast awareness over routine examination |
| American College of Obstetricians | Encourage breast self-awareness | Focus on familiarity with normal breast characteristics |
| National Comprehensive Cancer Network | Consider for high-risk patients | Complement enhanced screening protocols |
Implications for Nursing Practice
Evidence-based breast self-examination education requires balancing research findings with individual patient needs and preferences. Nurses should present information objectively while supporting informed patient decision-making about breast self-examination practices.
- Present balanced information about benefits and limitations
- Support individual patient preferences and decisions
- Emphasize breast awareness over rigid examination schedules
- Integrate breast self-examination with comprehensive breast health education
- Maintain current knowledge of evolving research and guidelines
Conclusion: Integrating Breast Self-Examination into Comprehensive Care
Breast self-examination represents one component of a comprehensive approach to breast health that includes professional screening, clinical examinations, and patient education. For nursing professionals, mastering breast self-examination education requires understanding both the technical aspects of the procedure and the broader context of breast health promotion. This knowledge enables nurses to provide evidence-based, patient-centered education that supports informed decision-making and optimal health outcomes.
The evolving evidence base surrounding breast self-examination emphasizes the importance of individualized approaches that consider patient risk factors, preferences, and capabilities. Rather than promoting universal adherence to rigid examination schedules, current practice focuses on developing breast awareness and encouraging open communication between patients and healthcare providers about breast health concerns.
Successful implementation of breast self-examination education requires ongoing assessment, follow-up, and adaptation to individual patient needs. Nurses must remain current with evolving research and guidelines while maintaining focus on the fundamental goals of breast health promotion: early detection, patient empowerment, and comprehensive healthcare engagement. Through thoughtful, evidence-based education, breast self-examination can contribute meaningfully to overall breast health strategies and patient well-being.
Key Takeaways for Nursing Practice
- Breast self-examination education should emphasize technique quality over examination frequency
- Patient education must address both benefits and limitations of breast self-examination
- Cultural sensitivity and individual adaptation enhance education effectiveness
- Documentation and follow-up support sustained patient engagement and skill development
- Integration with comprehensive breast health education optimizes patient outcomes
- Evidence-based practice requires ongoing professional development and guideline awareness
