Carbohydrates: A Comprehensive Guide for Nursing Students
Digestion, Absorption, Metabolism & Blood Glucose Regulation
Introduction
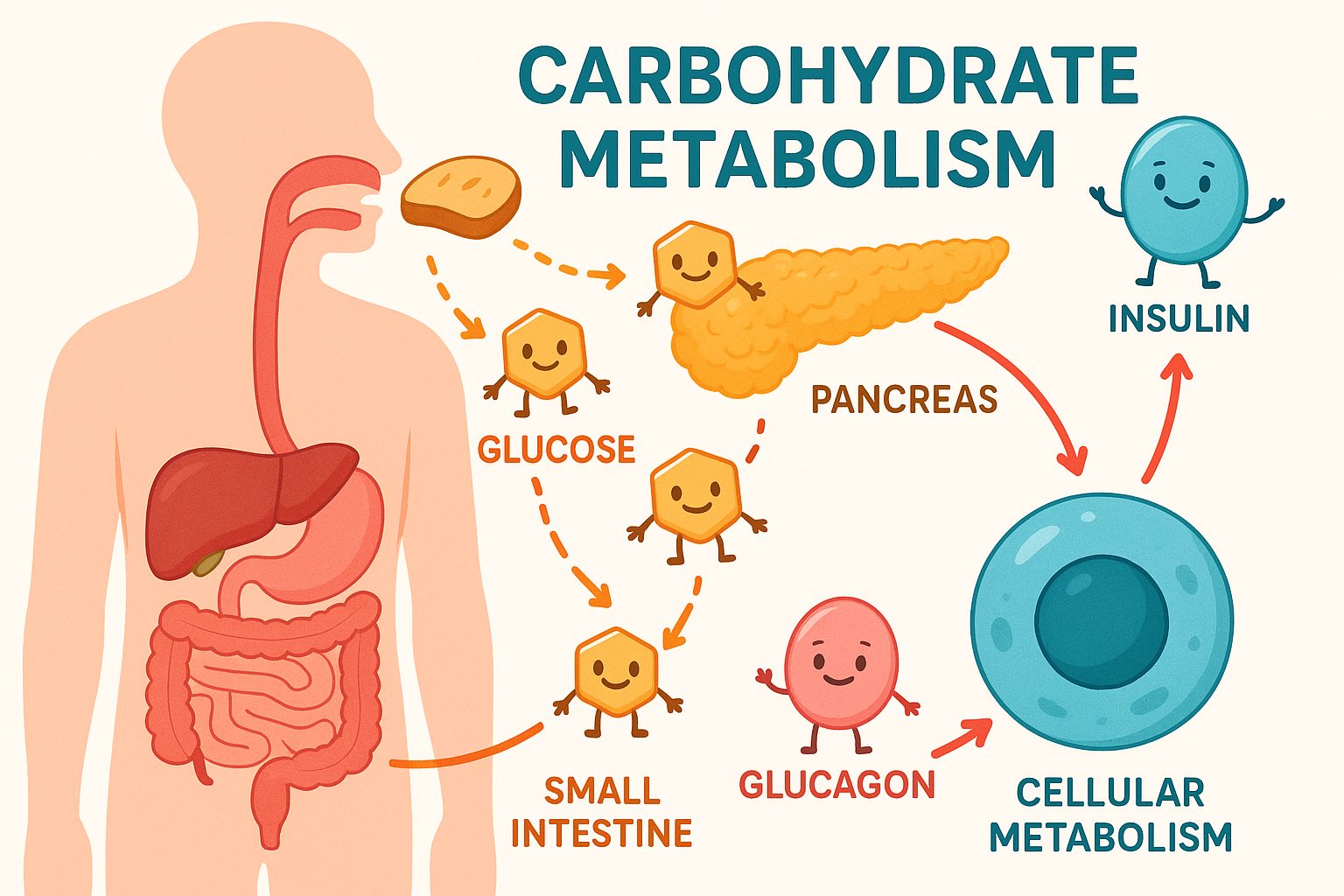
Carbohydrates are the body’s primary source of energy and one of the three essential macronutrients alongside proteins and fats. Understanding carbohydrate metabolism is crucial for nursing practice, particularly in managing patients with diabetes, metabolic disorders, and nutritional needs. This comprehensive guide explores the journey of carbohydrates from ingestion to cellular utilization, emphasizing clinical applications and nursing interventions.
Carbohydrate Metabolism: From Digestion to Cellular Energy
Carbohydrate Structure and Classification
Key Concept: Carbohydrate Hierarchy
All carbohydrates are built from simple sugar units (monosaccharides) that combine to form increasingly complex structures.
| Classification | Structure | Examples | Digestion Speed | Clinical Significance |
|---|---|---|---|---|
| Monosaccharides | Single sugar units (C₆H₁₂O₆) | Glucose, Fructose, Galactose | Immediate absorption | Rapid blood glucose elevation |
| Disaccharides | Two sugar units (C₁₂H₂₂O₁₁) | Sucrose, Lactose, Maltose | Quick digestion | Fast glucose response |
| Oligosaccharides | 3-10 sugar units | Maltodextrins, Raffinose | Moderate digestion | Intermediate glucose response |
| Polysaccharides | Long chains of sugars | Starch, Glycogen, Cellulose | Slow digestion | Sustained glucose release |
Memory Aid: “My Dog Owns Plenty”
Disaccharides – Double units
Polysaccharides – Plenty of units
Carbohydrate Digestion and Absorption
Digestive Journey of Carbohydrates
Mouth
Salivary α-amylase begins starch breakdown
Stomach
Acid inactivates amylase, minimal digestion
Pancreas
Pancreatic α-amylase continues breakdown
Small Intestine
Brush border enzymes complete digestion
Brush Border Enzymes
- Sucrase: Sucrose → Glucose + Fructose
- Lactase: Lactose → Glucose + Galactose
- Maltase: Maltose → Glucose + Glucose
- Isomaltase: α-1,6 bonds in starch
Absorption Mechanisms
- Glucose/Galactose: SGLT1 (Na⁺ dependent)
- Fructose: GLUT5 (facilitated diffusion)
- Exit: GLUT2 (basolateral)
- Portal circulation: To liver first
Nursing Implications: Digestion & Absorption
Assessment Considerations:
- • Monitor for carbohydrate malabsorption symptoms
- • Assess for lactose intolerance in patients
- • Evaluate GI disorders affecting absorption
- • Consider medication effects on digestion
Patient Education:
- • Explain importance of chewing thoroughly
- • Discuss timing of carbohydrate intake
- • Educate about lactose-free alternatives
- • Promote understanding of fiber benefits
Carbohydrate Metabolism Pathways
Glycolysis
Purpose: Break down glucose for immediate energy
Location: Cytoplasm of all cells
Products: 2 ATP, 2 NADH, 2 Pyruvate
Key Enzymes: Hexokinase, Phosphofructokinase, Pyruvate kinase
Glycogenesis
Purpose: Store glucose as glycogen
Location: Liver and muscle
Stimulus: High blood glucose, insulin
Key Enzyme: Glycogen synthase
Gluconeogenesis
Purpose: Create glucose from non-carbohydrate sources
Location: Primarily liver
Substrates: Amino acids, lactate, glycerol
Stimulus: Fasting, low blood glucose
Glycolysis Mnemonic: “Goodness Gracious, Father Franklin Did Go By Picking Pears”
Glucose-6-phosphate
Fructose-6-phosphate
Fructose-1,6-bisphosphate
Dihydroxyacetone phosphate
Bisphosphoglycerate
Phosphoglycerate
Phosphoenolpyruvate
Pyruvate
Metabolic Regulation: Fed vs Fasting States
Fed State (Anabolic)
- • Glycolysis ↑ (energy production)
- • Glycogenesis ↑ (glucose storage)
- • Lipogenesis ↑ (fat synthesis)
- • Protein synthesis ↑
- • Gluconeogenesis ↓
Fasting State (Catabolic)
- • Glycogenolysis ↑ (glucose release)
- • Gluconeogenesis ↑ (glucose synthesis)
- • Lipolysis ↑ (fat breakdown)
- • Protein breakdown ↑
- • Glycogenesis ↓
Blood Glucose Regulation
Normal Blood Glucose Range: 70-100 mg/dL (3.9-5.6 mmol/L)
Tight regulation is essential for proper organ function, especially brain and red blood cells.
Glucose Homeostasis Mechanism
Glycogenesis ↑
Gluconeogenesis ↑
| Hormone | Source | Stimulus | Target Organs | Primary Actions |
|---|---|---|---|---|
| Insulin | Pancreatic β-cells | ↑ Blood glucose ↑ Amino acids |
Liver, muscle, adipose tissue | ↑ Glucose uptake ↑ Glycogenesis ↑ Lipogenesis |
| Glucagon | Pancreatic α-cells | ↓ Blood glucose ↑ Amino acids |
Liver | ↑ Glycogenolysis ↑ Gluconeogenesis |
| Epinephrine | Adrenal medulla | Stress, exercise | Liver, muscle | ↑ Glycogenolysis ↑ Gluconeogenesis |
| Cortisol | Adrenal cortex | Stress, fasting | Liver, muscle | ↑ Gluconeogenesis ↑ Protein breakdown |
Insulin Actions Mnemonic: “SLIM”
Lowers blood glucose
Moves glucose into cells
Carbohydrate-Related Disorders
Diabetes Mellitus Type 1
Pathophysiology: Autoimmune destruction of β-cells
Onset: Usually childhood/adolescence
Treatment: Insulin therapy (essential)
Complications: DKA, hypoglycemia, long-term vascular damage
Diabetes Mellitus Type 2
Pathophysiology: Insulin resistance + β-cell dysfunction
Onset: Usually adulthood
Treatment: Lifestyle, oral medications ± insulin
Complications: HHS, cardiovascular disease, nephropathy
Hypoglycemia vs Hyperglycemia: Clinical Recognition
Hypoglycemia (<70 mg/dL)
Memory Aid: “Cold and Clammy, Need Some Candy”
- • Shakiness, tremor
- • Sweating, cool skin
- • Hunger, nausea
- • Confusion, irritability
- • Rapid heartbeat
- • Weakness, fatigue
Hyperglycemia (>180 mg/dL)
Memory Aid: “Hot and Dry, Sugar High”
- • Polydipsia (excessive thirst)
- • Polyuria (frequent urination)
- • Polyphagia (excessive hunger)
- • Blurred vision
- • Fatigue, weakness
- • Slow wound healing
| Disorder | Blood Glucose | Key Symptoms | Emergency Treatment | Prevention |
|---|---|---|---|---|
| Hypoglycemia | <70 mg/dL | Shakiness, sweating, confusion | 15g fast-acting carbs Glucagon if severe |
Regular meals, monitor BG |
| DKA | >250 mg/dL | Kussmaul breathing, fruity odor | IV fluids, insulin, electrolytes | Medication adherence |
| HHS | >600 mg/dL | Severe dehydration, altered mental status | IV fluids, gradual insulin | Adequate hydration, monitoring |
DKA Triad Mnemonic: “HAK”
(>250 mg/dL)
(pH <7.3)
(in blood/urine)
Nursing Applications and Interventions
Assessment Priorities
- Monitor blood glucose levels regularly
- Assess for signs of hypo/hyperglycemia
- Review medication adherence
- Evaluate dietary intake patterns
- Check for diabetic complications
- Assess psychosocial factors
Care Planning
- Develop individualized meal plans
- Establish monitoring schedules
- Plan exercise programs
- Coordinate with healthcare team
- Address patient education needs
- Prepare for emergency situations
Patient Education: Carbohydrate Counting
Basic Principles:
- • 15g carbs = 1 serving
- • Read nutrition labels
- • Measure portion sizes
- • Track total daily carbs
Common Portions:
- • 1 slice bread = 15g
- • 1/2 cup rice = 15g
- • 1 small apple = 15g
- • 1 cup milk = 12g
Teaching Tips:
- • Use visual aids
- • Practice with food models
- • Provide reference cards
- • Encourage food diaries
| Nursing Diagnosis | Related Factors | Goals | Interventions | Evaluation |
|---|---|---|---|---|
| Risk for Unstable Blood Glucose | Medication non-adherence Dietary changes Illness/stress |
Maintain BG 80-130 mg/dL Prevent complications |
Monitor BG q4h Administer insulin as ordered Provide diabetic diet |
BG within target range No hypoglycemic episodes |
| Deficient Knowledge | New diagnosis Complex medication regimen |
Demonstrate understanding Perform self-care |
Teach carb counting Demonstrate BG monitoring Provide written materials |
Verbalizes understanding Performs return demonstration |
| Imbalanced Nutrition | Poor dietary choices Irregular meal patterns |
Maintain stable weight Optimal nutrition |
Consult dietitian Monitor food intake Educate about meal planning |
Follows meal plan Stable weight |
Diabetes Management Mnemonic: “GLUCOSE BAD”
Lifestyle modifications
Understanding of condition
Compliance with medications
Stress management
Eye examinations
Blood pressure control
Annual lab work
Diet education
Clinical Scenarios & Case Studies
Case Study 1: Hypoglycemia
Scenario: A 45-year-old diabetic patient presents with shakiness, sweating, and confusion. BG = 55 mg/dL.
Immediate Actions:
- • Give 15g fast-acting carbs (glucose tablets, juice)
- • Recheck BG in 15 minutes
- • Repeat treatment if still <70 mg/dL
- • Provide complex carb snack once stable
Follow-up: Investigate cause, adjust insulin regimen, reinforce education.
Case Study 2: DKA
Scenario: A 28-year-old Type 1 diabetic with BG = 380 mg/dL, ketones +3, pH = 7.2, rapid deep breathing.
Priority Interventions:
- • Establish IV access, begin fluid resuscitation
- • Start continuous insulin infusion
- • Monitor electrolytes (especially K+)
- • Assess neurological status
Goals: Gradual BG reduction, ketone clearance, acid-base balance restoration.
Additional Memory Aids & Quick References
Insulin Types: “RALNG”
- Rapid-acting (Aspart, Lispro) – 15 min onset
- Acting Regular – 30 min onset
- Long-acting (Glargine, Detemir) – 1-2 hr onset
- NPH – 2-4 hr onset
- Glulisine – 15 min onset
Diabetic Complications: “FRIENDS”
- Foot problems
- Retinopathy
- Infections
- Erectile dysfunction
- Nephropathy
- Dermopathy
- Stroke risk
Quick Reference: Carbohydrate Calculations
Hypoglycemia Treatment:
- • 15g glucose tablets
- • 4 oz fruit juice
- • 6-8 oz regular soda
- • 1 tbsp honey
Carb Counting:
- • 1 carb choice = 15g
- • 45-60g per meal
- • 15g per snack
- • Insulin:carb ratio varies
Normal Values:
- • Fasting: 70-100 mg/dL
- • 2hr post-meal: <140 mg/dL
- • HbA1c: <7% (goal)
- • Random: <200 mg/dL
Conclusion
Understanding carbohydrate metabolism is fundamental to nursing practice, particularly in managing patients with diabetes and metabolic disorders. The journey from carbohydrate ingestion to cellular energy production involves complex physiological processes that require careful monitoring and intervention.
Key takeaways for nursing practice include recognizing the signs and symptoms of glucose imbalances, understanding the importance of medication timing and dietary education, and implementing appropriate interventions for both acute and chronic conditions. The mnemonics and memory aids provided serve as practical tools for clinical decision-making and patient education.
Successful diabetes management requires a collaborative approach involving patient education, lifestyle modifications, medication adherence, and regular monitoring. As healthcare providers, nurses play a crucial role in empowering patients to manage their condition effectively and prevent complications through evidence-based interventions and compassionate care.
Final Nursing Pearls
Always Remember:
- • Prevention is better than treatment
- • Patient education is paramount
- • Individualize care plans
- • Monitor for complications
Best Practices:
- • Use evidence-based protocols
- • Collaborate with healthcare team
- • Maintain accurate documentation
- • Provide emotional support
