Carbohydrates
Comprehensive Nursing Notes
Essential macronutrient knowledge for nursing practice
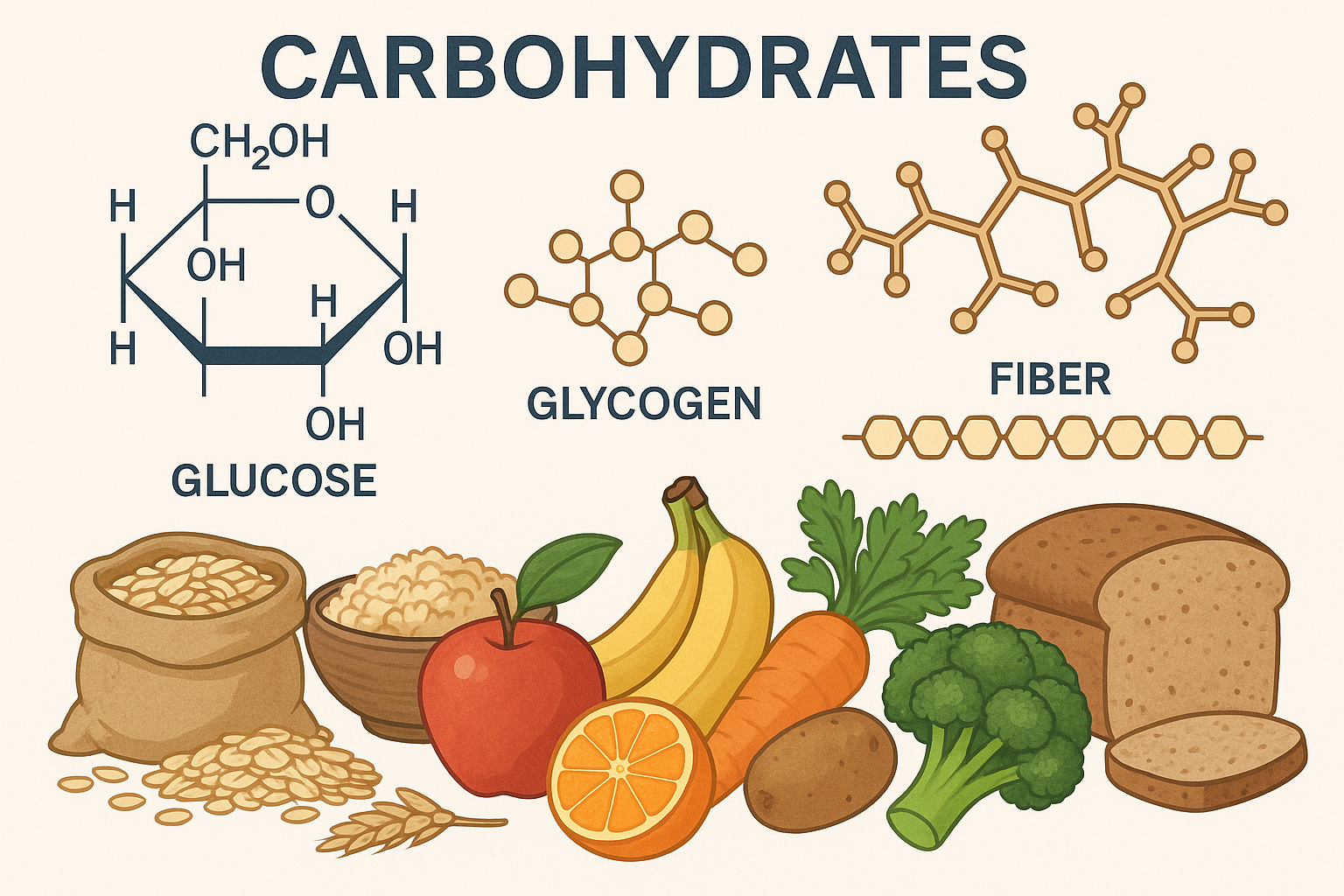
Figure 1: Carbohydrate molecular structures and dietary sources
Introduction to Carbohydrates
Carbohydrates are organic compounds composed of carbon, hydrogen, and oxygen atoms in a 1:2:1 ratio, representing the body’s primary and most efficient energy source. For nursing professionals, understanding carbohydrate metabolism, functions, and clinical implications is crucial for comprehensive patient care, nutritional assessment, and therapeutic intervention planning.
Key Nursing Consideration
Carbohydrates provide 4 calories per gram and should comprise 45-65% of total daily caloric intake for optimal physiological function. This macronutrient directly impacts blood glucose levels, making monitoring essential for patients with diabetes, metabolic disorders, and critical illness.
Carbohydrate Composition
Carbohydrates are classified into three primary structural categories based on their molecular complexity and digestibility. Each category serves distinct physiological functions and requires specific nursing considerations.
Starches (Complex Carbohydrates)
Molecular Structure:
Amylopectin: Branched glucose polymers
Formula: (C₆H₁₀O₅)ₙ
Physiological Processing:
Nursing Implementation for Starch Management:
- Monitor postprandial glucose levels 1-2 hours after complex carbohydrate meals
- Educate patients on portion control using the plate method (1/4 plate for starches)
- Assess for digestive enzymes deficiency in patients with malabsorption
- Recommend whole grain sources over refined starches for improved glycemic control
- Consider timing of starch intake with insulin administration for diabetic patients
Sugars (Simple Carbohydrates)
Monosaccharides
- • Glucose (dextrose)
- • Fructose (fruit sugar)
- • Galactose (milk sugar component)
Disaccharides
- • Sucrose (table sugar)
- • Lactose (milk sugar)
- • Maltose (malt sugar)
Added Sugars
- • High fructose corn syrup
- • Honey
- • Maple syrup
Mnemonic for Sugar Metabolism:
“GFG Makes Sweet Lactose Memories”
Glucose, Fructose, Galactose → Maltose, Sucrose, Lactose
Clinical Alert:
Simple sugars cause rapid blood glucose elevation within 15-30 minutes of ingestion. This is critical for treating hypoglycemia but requires careful monitoring in diabetic patients.
Nursing Interventions for Sugar Management:
Assessment:
- • Monitor blood glucose trends
- • Assess for lactose intolerance symptoms
- • Evaluate dental health status
- • Screen for sugar addiction behaviors
Intervention:
- • Administer glucose tablets for hypoglycemia
- • Provide lactase supplements as needed
- • Educate on hidden sugar sources
- • Implement gradual sugar reduction strategies
Cellulose (Dietary Fiber)
Structural Properties:
Linear glucose chains
Indigestible by human enzymes
Fiber Categories:
- Soluble: Pectin, gums, mucilages
- Insoluble: Cellulose, hemicellulose, lignin
Physiological Benefits:
Nursing Assessment and Intervention for Fiber:
Assessment:
- • Bowel movement frequency
- • Stool consistency (Bristol scale)
- • Abdominal comfort
- • Dietary fiber intake
Intervention:
- • Gradual fiber increase (5g/week)
- • Ensure adequate hydration
- • Monitor for GI distress
- • Educate on fiber sources
Monitoring:
- • Blood glucose levels
- • Cholesterol trends
- • Weight changes
- • Medication absorption
Recommended Daily Allowance (RDA)
The Dietary Reference Intakes (DRIs) provide evidence-based recommendations for carbohydrate consumption across different life stages and physiological conditions. Nurses must understand these guidelines to provide appropriate nutritional counseling and assess dietary adequacy.
General Population RDA:
Special Populations:
| Age Group | Total Carbs (g/day) | Fiber (g/day) | Added Sugars (% calories) | Nursing Considerations |
|---|---|---|---|---|
| Children 1-3 years | 130 | 19 | ≤10% | Focus on whole fruits, avoid juice excess |
| Children 4-8 years | 130 | 25 | ≤10% | Establish healthy eating patterns |
| Adolescents 9-18 years | 130 | 26-38 | ≤10% | Address growth spurts and activity needs |
| Adults 19-50 years | 130 | 25-38 | ≤10% | Lifestyle modification counseling |
| Adults 51+ years | 130 | 21-30 | ≤10% | Monitor for medication interactions |
Mnemonic for Fiber Requirements:
“25 For Women, 38 For Men”
Easy recall: Women need 25g fiber daily, men need 38g daily (ages 19-50)
Nursing Role in RDA Implementation:
Assessment Strategies:
- • Conduct 24-hour dietary recalls
- • Use food frequency questionnaires
- • Calculate carbohydrate-to-insulin ratios
- • Monitor HbA1c trends in diabetic patients
- • Assess fiber intake using validated tools
Education Priorities:
- • Teach carbohydrate counting techniques
- • Demonstrate portion size visualization
- • Explain glycemic index concepts
- • Provide culturally appropriate meal planning
- • Address barriers to dietary adherence
Dietary Sources of Carbohydrates
Understanding carbohydrate sources enables nurses to provide comprehensive nutritional counseling, develop appropriate meal plans, and help patients make informed food choices. Different sources provide varying nutritional profiles and metabolic effects.
Starch Sources (Complex Carbohydrates)
Whole Grains
- • Brown rice (23g/cup cooked)
- • Quinoa (39g/cup cooked)
- • Oats (32g/cup cooked)
- • Barley (44g/cup cooked)
- • Whole wheat bread (12g/slice)
Starchy Vegetables
- • Sweet potato (27g/medium)
- • Regular potato (37g/medium)
- • Corn (31g/cup)
- • Peas (25g/cup)
- • Winter squash (22g/cup)
Legumes
- • Black beans (45g/cup)
- • Lentils (40g/cup)
- • Chickpeas (45g/cup)
- • Kidney beans (40g/cup)
- • Split peas (41g/cup)
Clinical Pearl:
Whole grain sources have a lower glycemic index compared to refined counterparts, providing more stable blood glucose levels. This is particularly important for patients with diabetes or metabolic syndrome.
Sugar Sources (Simple Carbohydrates)
Natural Sugar Sources
Added Sugar Sources
Hidden Sugar Sources – Nursing Alert:
Unexpected Sources:
- • Pasta sauce (12g/cup)
- • Salad dressing (8g/2 tbsp)
- • Ketchup (4g/tbsp)
- • Granola bar (12g/bar)
- • Flavored yogurt (26g/cup)
Label Reading Tips:
- • Check “Total Sugars” on nutrition label
- • Look for “Added Sugars” specifically
- • Identify sugar aliases (corn syrup, maltose)
- • Consider ingredients list order
- • Calculate daily sugar percentage
Fiber Sources
Soluble Fiber Sources
Insoluble Fiber Sources
Nursing Strategies for Dietary Source Education:
Assessment:
- • Food preference evaluation
- • Cultural dietary patterns
- • Economic considerations
- • Cooking skills assessment
- • Access to healthy foods
Education:
- • Demonstrate food label reading
- • Provide portion size guides
- • Teach meal planning skills
- • Explain glycemic index concepts
- • Address common misconceptions
Follow-up:
- • Monitor dietary adherence
- • Assess clinical outcomes
- • Modify recommendations as needed
- • Provide ongoing support
- • Celebrate progress achieved
Functions of Carbohydrates
Carbohydrates serve multiple critical physiological functions beyond energy provision. Understanding these functions enables nurses to appreciate the clinical significance of adequate carbohydrate intake and recognize deficiency or excess symptoms.
Primary Energy Source
Cellular Energy Production:
Organ-Specific Requirements:
Cannot use fatty acids for energy
Essential for cardiac rhythm
No mitochondria for fat oxidation
Clinical Significance:
Hypoglycemia (blood glucose <70 mg/dL) can cause neurological symptoms including confusion, seizures, and coma. Nurses must recognize early signs and intervene promptly with rapid-acting carbohydrates.
Protein Sparing Function
Metabolic Pathway:
Clinical Implications:
Fat Metabolism Regulation
Mnemonic: “Fats Burn in a Carbohydrate Flame”
Without adequate carbohydrates, fat metabolism becomes incomplete, leading to ketone body formation and potential acidosis.
Normal Fat Metabolism:
Carbohydrate Deficiency:
Gastrointestinal Function
Digestive Health
- • Promotes beneficial bacteria
- • Maintains gut barrier integrity
- • Supports mucus production
- • Prevents constipation
Motility Enhancement
- • Stimulates peristalsis
- • Increases stool bulk
- • Reduces transit time
- • Prevents diverticulosis
Metabolic Benefits
- • Produces short-chain fatty acids
- • Lowers cholesterol
- • Improves insulin sensitivity
- • Reduces inflammation
Central Nervous System Function
Neurological Requirements:
Hypoglycemia Symptoms:
- • Tremors, sweating
- • Anxiety, irritability
- • Hunger, weakness
- • Confusion, difficulty concentrating
- • Seizures, loss of consciousness
- • Coma (if untreated)
Nursing Assessment of Carbohydrate Functions:
Physiological Indicators:
- • Blood glucose levels (70-100 mg/dL fasting)
- • Energy levels and fatigue assessment
- • Cognitive function evaluation
- • Bowel movement patterns
- • Wound healing progress
- • Muscle mass maintenance
Intervention Strategies:
- • Monitor blood glucose per protocol
- • Assess nutritional intake adequacy
- • Educate on balanced carbohydrate intake
- • Coordinate with dietitian for meal planning
- • Document response to interventions
- • Adjust care plan based on outcomes
Nursing Implementation in Clinical Practice
Effective nursing implementation of carbohydrate knowledge requires integration of assessment skills, clinical judgment, patient education, and interdisciplinary collaboration. This section provides comprehensive guidance for applying carbohydrate concepts in various clinical settings.
Comprehensive Carbohydrate Assessment
Subjective Assessment:
- 24-hour dietary recall
- Food preferences and aversions
- Cultural dietary practices
- Economic factors affecting food choices
- Cooking skills and kitchen access
- Energy levels throughout day
- Hunger and satiety patterns
- Digestive symptoms
- Mood and cognitive changes
Objective Assessment:
- Fasting glucose (70-100 mg/dL)
- HbA1c (<7% for diabetics)
- Lipid profile
- Albumin and prealbumin
- Electrolytes
- Weight trends and BMI
- Muscle mass assessment
- Skin integrity and wound healing
- Neurological function
Assessment Mnemonic: “CARBS”
Appetite and preferences
Recent weight changes
Blood glucose monitoring
Symptoms of imbalance
Care Planning and Goal Setting
| Nursing Diagnosis | Expected Outcomes | Interventions | Evaluation Criteria |
|---|---|---|---|
| Imbalanced nutrition: less than body requirements | Patient will consume 45-65% of calories from carbohydrates within 1 week | Dietary consultation, meal planning, education | Dietary intake records, weight stabilization |
| Risk for unstable blood glucose | Blood glucose will remain 70-180 mg/dL | Glucose monitoring, medication administration, dietary coordination | Glucose logs, HbA1c trends |
| Deficient knowledge about carbohydrate counting | Patient will demonstrate accurate carb counting | Education sessions, practice exercises, resource provision | Return demonstration, verbal understanding |
| Constipation related to low fiber intake | Regular bowel movements (every 1-2 days) | Fiber education, hydration promotion, activity encouragement | Bowel movement frequency, stool consistency |
Implementation Strategies by Clinical Setting
Acute Care Setting:
- Monitor glucose every 4-6 hours
- Coordinate meal timing with medications
- Assess NPO status and alternative feeding
- Document intake and output
- Bedside glucose monitoring instruction
- Hypoglycemia recognition and treatment
- Discharge planning with dietary needs
Community Health Setting:
- Diabetes prevention education
- Healthy eating workshops
- Grocery store tours
- Cooking demonstrations
- Regular HbA1c monitoring
- Medication adherence support
- Lifestyle modification counseling
- Support group facilitation
Patient and Family Education
Teaching Strategies:
Visual Learning:
- • Food models and portion guides
- • Carbohydrate counting charts
- • Grocery store mapping
- • Meal planning worksheets
Hands-on Practice:
- • Glucose meter demonstrations
- • Food label reading exercises
- • Portion size estimation
- • Menu planning activities
Technology Integration:
- • Mobile apps for carb counting
- • Online diabetes education
- • Glucose monitoring apps
- • Virtual cooking classes
Education Pearls:
- • Start with small, achievable goals
- • Use culturally appropriate examples
- • Provide written materials in appropriate language
- • Involve family members in education sessions
- • Schedule regular follow-up appointments
Evaluation and Outcome Measurement
Short-term Outcomes (1-4 weeks):
Long-term Outcomes (3-12 months):
Evidence-Based Practice Integration:
Research Applications:
- • Implement evidence-based glucose protocols
- • Use validated assessment tools
- • Apply current dietary guidelines
- • Incorporate technology solutions
- • Measure patient satisfaction scores
Quality Improvement:
- • Track clinical outcomes data
- • Analyze readmission rates
- • Evaluate education effectiveness
- • Monitor medication adherence
- • Assess cost-effectiveness
Key Takeaways for Nursing Practice
Essential Knowledge:
- Carbohydrates provide 4 calories per gram and should comprise 45-65% of daily calories
- Minimum requirement of 130g daily prevents protein catabolism and ketosis
- Fiber intake should be 25-38g daily for optimal health benefits
- Added sugars should be limited to <10% of total daily calories
Clinical Applications:
- Monitor blood glucose levels regularly in at-risk patients
- Educate patients on carbohydrate counting and portion control
- Assess for signs of hypoglycemia and hyperglycemia
- Collaborate with dietitians for comprehensive nutritional care
These notes are designed for educational purposes and should be used in conjunction with current evidence-based practice guidelines and institutional protocols.
Last updated: 2025 | For nursing students and healthcare professionals
