Care of Fever Patients with Urinary Diversions
Comprehensive Nursing Study Notes
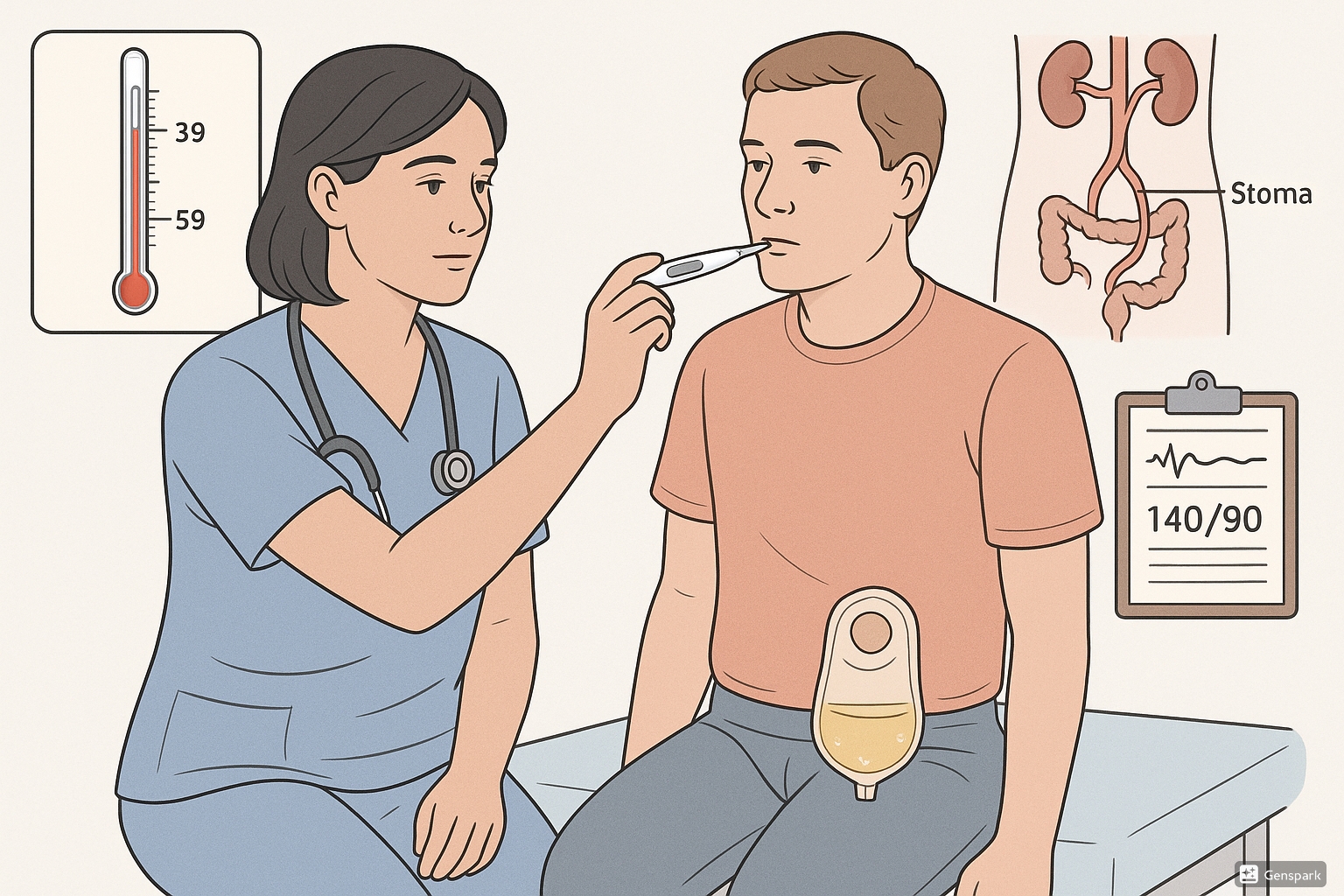
Figure 1: Comprehensive fever assessment in patients with urinary diversions
Learning Objectives
- Identify types of urinary diversions and their complications
- Assess fever patterns in patients with urinary diversions
- Implement evidence-based nursing interventions for fever management
- Recognize signs and symptoms of urinary tract infections in diverted patients
- Provide patient education on prevention strategies
- Apply critical thinking skills in clinical decision-making
Introduction
Urinary diversions are surgical procedures that reroute urine flow when the normal urinary tract is compromised by disease, trauma, or congenital abnormalities. Patients with urinary diversions face unique challenges, particularly regarding infection prevention and fever management. Understanding the complexities of caring for these patients is crucial for providing optimal nursing care and preventing serious complications.
Fever in patients with urinary diversions often indicates infection, which can rapidly progress to serious systemic complications if not promptly recognized and treated. This comprehensive guide provides nursing students with essential knowledge for providing evidence-based care to this vulnerable population.
Types of Urinary Diversions
Incontinent Diversions
Ileal Conduit (Most Common)
- Uses 12-18 cm segment of ileum
- Ureters anastomosed to proximal end
- Distal end brought to abdominal surface as stoma
- Continuous urine drainage into external pouch
Colonic Conduit
- Uses segment of colon
- Less common than ileal conduit
- May have better mucus production
Continent Diversions
Indiana Pouch
- Internal reservoir created from cecum and ascending colon
- Catheterizable stoma
- Patient empties pouch 4-6 times daily
Orthotopic Neobladder
- Artificial bladder connected to urethra
- Patient voids through urethra
- Requires intact urinary sphincter
Memory Aid: Types of Urinary Diversions
Remember “I COIN”:
- Ileal conduit (Incontinent)
- Colonic conduit (Incontinent)
- Orthotopic neobladder (Continent)
- Indiana pouch (Continent)
- Needs assessment for each type differ!
Fever Assessment in Urinary Diversion Patients
Definition and Significance
Fever Definitions:
- Low-grade: 100.4°F – 102°F (38°C – 38.9°C)
- Moderate: 102°F – 104°F (38.9°C – 40°C)
- High-grade: >104°F (>40°C)
- Hyperpyrexia: >106°F (>41.1°C)
Clinical Significance:
- UTI is most common cause of fever
- Higher risk of ascending infection
- Potential for rapid sepsis development
- May indicate anastomotic leak
Comprehensive Fever Assessment Tool
Vital Signs
- • Temperature (route and frequency)
- • Heart rate and rhythm
- • Blood pressure
- • Respiratory rate and pattern
- • Oxygen saturation
Urinary Assessment
- • Urine output quantity
- • Urine color and clarity
- • Odor characteristics
- • Presence of blood or sediment
- • Stoma appearance
Systemic Signs
- • Mental status changes
- • Chills and rigors
- • Fatigue and malaise
- • Nausea and vomiting
- • Back or flank pain
Assessment Mnemonic: “FEVER WATCH”
F – Frequency of temperature checks
E – Examine urine characteristics
V – Vital signs monitoring
E – Evaluate mental status
R – Review intake and output
W – Watch for chills and rigors
A – Assess pain levels
T – Test urine if possible
C – Check stoma and surrounding skin
H – History of recent changes
Common Causes of Fever in Urinary Diversion Patients
Primary Causes (Most Common)
Urinary Tract Infections (70-80%)
- Bacterial colonization of conduit
- Ascending infection to kidneys
- Common organisms: E. coli, Klebsiella, Pseudomonas
- Higher risk due to altered anatomy
Pyelonephritis
- Upper urinary tract infection
- Presents with high fever and back pain
- Risk of sepsis if untreated
Surgical Site Infections
- Wound infections
- Intra-abdominal abscesses
- Anastomotic leaks with secondary infection
Secondary Causes
Metabolic Complications
- Hyperchloremic acidosis
- Electrolyte imbalances
- Dehydration-related fever
Mechanical Complications
- Ureteral obstruction
- Conduit obstruction
- Stomal complications
Other Systemic Causes
- Pneumonia
- Deep vein thrombosis
- Drug reactions
- Cancer recurrence
Diagnostic Approach Flowchart
• Vital signs
• Mental status
• Pain assessment
• Urine appearance
• Output measurement
• Stoma examination
• Respiratory
• Cardiovascular
• GI symptoms
• Antibiotics per protocol
• Increase fluid intake
• Monitor closely
• Immediate physician notification
• IV access
• Consider ICU transfer
Evidence-Based Nursing Interventions
Immediate Interventions (0-2 hours)
Temperature Management
- Monitor temperature every 1 hour initially
- Administer antipyretics as ordered
- Use cooling measures if >102°F
Fluid Management
- Assess hydration status
- Encourage oral fluids if tolerated
- Consider IV fluids if dehydrated
Specimen Collection
- Obtain urine specimen for analysis
- Blood cultures if indicated
- Document collection time and method
Ongoing Interventions (2-24 hours)
Medication Administration
- Administer antibiotics as prescribed
- Monitor for adverse reactions
- Ensure therapeutic drug levels
Monitoring
- Vital signs every 4 hours
- Intake and output documentation
- Pain assessment and management
Supportive Care
- Nutritional support
- Rest and comfort measures
- Emotional support
Clinical Pearl: The “Silent UTI” Phenomenon
⚠️ Important: Patients with urinary diversions may not exhibit classic UTI symptoms!
Missing Classic Symptoms:
- No dysuria (patient doesn’t void normally)
- No urgency or frequency
- No suprapubic pain
Key Indicators to Watch:
- Fever may be the ONLY sign
- Change in urine odor or appearance
- Unexplained fatigue or confusion
- Back pain (suggests upper tract involvement)
Complications and Red Flag Signs
Serious Complications
Sepsis/Septic Shock
Signs:
- Fever >101.3°F or <96.8°F
- HR >90 bpm
- RR >20 or PaCO2 <32
- WBC >12,000 or <4,000
- Altered mental status
- Hypotension
Pyelonephritis
Signs:
- High fever with chills
- Flank or back pain
- Nausea and vomiting
- Costovertebral angle tenderness
- Cloudy, foul-smelling urine
Anastomotic Leak
Signs:
- Abdominal pain and distention
- Peritonitis signs
- Decreased urine output
- Fluid collection on imaging
- Persistent fever
Red Flag Warning System
GREEN
Stable vital signs
Normal mentation
Good urine output
YELLOW
Low-grade fever
Mild symptoms
Monitor closely
ORANGE
High fever
Systemic symptoms
Notify physician
RED
Sepsis signs
Shock symptoms
Emergency response
Patient and Family Education
Prevention Strategies
Hydration
- Drink 8-10 glasses of water daily
- Avoid excessive caffeine
- Monitor urine color (pale yellow goal)
Hygiene Practices
- Proper hand hygiene before/after stoma care
- Keep peristomal skin clean and dry
- Change pouching system regularly
Equipment Management
- Use anti-reflux valves
- Empty pouch when 1/3 full
- Use night drainage system
When to Seek Medical Attention
Immediate (Call 911)
- Fever >103°F with chills
- Severe confusion or altered consciousness
- Difficulty breathing
- Chest pain
- Signs of shock
Urgent (Call within hours)
- Fever >100.4°F
- Severe back or flank pain
- Nausea and vomiting
- Decreased urine output
- Blood in urine
Soon (Call within 24 hours)
- Change in urine odor or appearance
- Persistent fatigue
- Mild abdominal discomfort
- Stoma changes
Patient Teaching Memory Aid: “FLUSH OUT INFECTION”
F – Fluids: Drink plenty of water
L – Look for fever and chills
U – Urine changes: color, odor, blood
S – Stoma care: keep clean
H – Hygiene: wash hands frequently
O – Output: monitor urine production
U – Urgent care: know when to call
T – Temperature: check regularly
I – Infection signs: learn to recognize
N – Night drainage: use consistently
Implementation in Nursing Practice
Care Planning Framework
Assessment Phase
- Comprehensive history taking
- Physical examination focusing on urinary system
- Risk factor identification
- Baseline vital signs establishment
- Laboratory data review
Planning Phase
- Individualized care plan development
- Goal setting with patient/family
- Interdisciplinary collaboration
- Resource allocation
- Discharge planning initiation
Implementation Phase
- Interventions execution
- Continuous monitoring
- Patient education delivery
- Family involvement
- Documentation maintenance
Priority Nursing Diagnoses
Primary Diagnoses
Risk for Infection
Related to altered urinary tract anatomy and invasive procedures
Hyperthermia
Related to infectious process secondary to UTI
Deficient Fluid Volume
Related to fever and inadequate fluid intake
Secondary Diagnoses
Acute Pain
Related to inflammation and infection
Deficient Knowledge
Related to infection prevention strategies
Anxiety
Related to fear of complications and hospitalization
Quality Indicators for Excellence
Timeliness
Fever recognition within 30 minutes
Accuracy
Correct assessment 95% of time
Communication
Clear handoff communication
Outcomes
Reduced infection rates
Case Study Application
Case Scenario
Patient: Mrs. Sarah Johnson, 68-year-old female
History: Radical cystectomy with ileal conduit 3 months ago for bladder cancer
Admission: Emergency department at 2:00 AM
Chief Complaint: “I’ve been feeling sick for 2 days and now I have a fever”
Assessment Findings
Vital Signs: T: 102.1°F, HR: 98, BP: 110/70, RR: 22, O2 Sat: 96%
Mental Status: Alert but appears fatigued
Urine: Dark yellow, cloudy, strong odor
Stoma: Pink, moist, no surrounding irritation
Pain: 4/10 right flank pain
Other: Reports decreased appetite, mild nausea
Critical Thinking Questions
Q1: What is your primary nursing concern?
Q2: What immediate assessments would you perform?
Q3: What diagnostic tests would you anticipate?
Q4: What nursing interventions are priority?
Learning Points
- Fever in urinary diversion patients requires immediate attention
- Classic UTI symptoms may be absent
- Flank pain suggests upper urinary tract involvement
- Prompt antibiotic therapy is essential
- Hydration status must be carefully monitored
Key Takeaways and Summary
Essential Points to Remember
Fever may be the ONLY sign of UTI in urinary diversion patients
Early recognition and intervention prevent serious complications
Prevention through education is more effective than treatment
Interdisciplinary collaboration improves patient outcomes
Holistic care addresses physical, emotional, and educational needs
Clinical Competency Checklist
Master Memory Framework: “DIVERSION CARE”
D – Detect fever early
I – Investigate thoroughly
V – Vital signs monitoring
E – Evaluate urine characteristics
R – Report findings promptly
S – Support with fluids
I – Implement interventions
O – Observe for complications
N – Notify physician when needed
CARE – Continuous Assessment, Reassessment, Evaluation
References and Further Reading
Primary Sources
- 1. Falagas, M. E., & Vergidis, P. I. (2005). Urinary tract infections in patients with urinary diversion. American Journal of Kidney Diseases, 46(6), 1030-1037.
- 2. Cross, H. H., & Schempp, B. A. (2024). Nursing care for patients after urostomy surgery. American Journal of Nursing, 124(6), 28-36.
- 3. Memorial Sloan Kettering Cancer Center. (2024). About your urostomy. Patient education materials.
- 4. Wound, Ostomy, and Continence Nurses Society. (2024). Clinical practice guidelines for ostomy care.
Additional Resources
- 5. United Ostomy Associations of America. (2024). Educational resources and support materials.
- 6. Bladder Cancer Advocacy Network. (2024). Long-term management of urinary diversion.
- 7. National Institute of Diabetes and Digestive and Kidney Diseases. (2024). Urinary diversion information.
- 8. International Association for Enterostomal Therapy. (2024). Best practice guidelines.
