Intermittent Catheterization
Comprehensive Nursing Care Guide
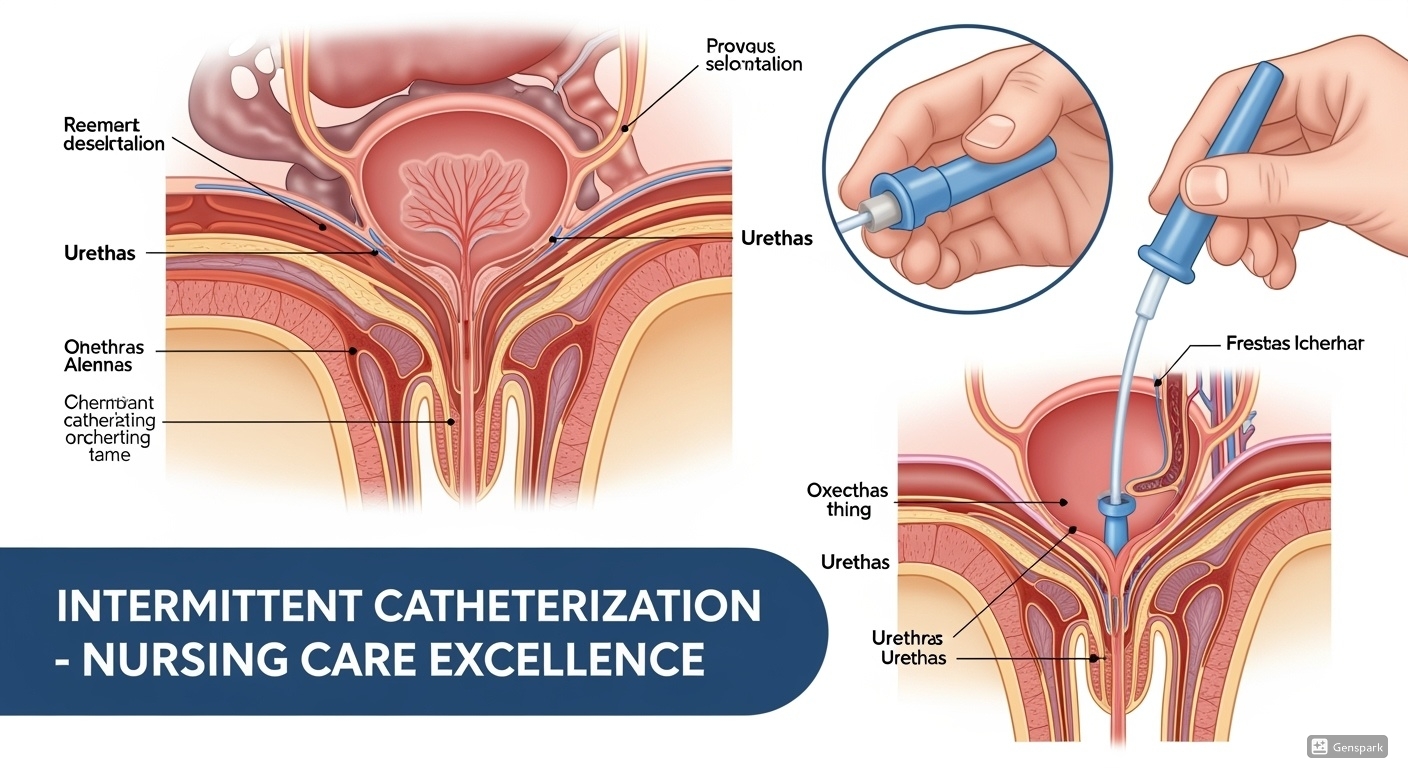
Table of Contents
Introduction
What is Intermittent Catheterization?
Intermittent catheterization (IC) is the gold standard for bladder management in patients with urinary retention or incomplete bladder emptying. It involves the periodic insertion and removal of a catheter to drain urine from the bladder, mimicking normal bladder function while preventing complications associated with indwelling catheters.
Clinical Pearl
IC significantly reduces the risk of urinary tract infections compared to indwelling catheters because it prevents biofilm formation and maintains natural bladder defense mechanisms.
Nursing Tip
Patient adherence to IC programs is crucial for success. Early education, proper technique training, and ongoing support are essential components of quality nursing care.
Historical Context
The clean intermittent catheterization technique was pioneered by Jack Lapides in the 1970s, revolutionizing bladder management for patients with neurogenic bladder dysfunction. This breakthrough demonstrated that regular bladder evacuation was more important than sterile technique for preventing complications.
Learning Objectives
Knowledge Objectives
- Understand the anatomical and physiological basis for intermittent catheterization
- Identify indications and contraindications for IC
- Describe different catheterization techniques and their applications
- Recognize potential complications and their management
Skills Objectives
- Perform safe and effective intermittent catheterization procedures
- Educate patients and caregivers on proper IC techniques
- Develop individualized catheterization care plans
- Implement evidence-based infection prevention strategies
Anatomy & Physiology Review
Urinary System Overview
Upper Urinary Tract
- Kidneys: Filter blood and produce urine
- Ureters: Transport urine to bladder
- Ureterovesical junction: Prevents reflux
Lower Urinary Tract
- Bladder: Stores and expels urine
- Urethra: Conduit for urine elimination
- Sphincters: Control urinary continence
Memory Aid – BLADDER Function
- Bladder filling (storage phase)
- Low pressure storage
- Adequate capacity (400-600ml)
- Detrusor muscle accommodation
- Differentiated voiding reflex
- Effective emptying
- Reflexes coordinated
Catheter Insertion Pathway
Key Definitions
Intermittent Catheterization (IC)
Drainage or aspiration of the bladder with subsequent removal of the catheter, performed at regular intervals.
Clean Intermittent Catheterization (CIC)
IC performed using clean technique, typically in home settings by patients or caregivers.
Aseptic Technique
IC performed using sterile catheter, sterile gloves, and sterile lubricant in healthcare settings.
Post-Void Residual (PVR)
Volume of urine remaining in the bladder after voluntary voiding.
Neurogenic Bladder
Bladder dysfunction resulting from neurological disorders affecting normal bladder control.
Urinary Retention
Inability to empty the bladder completely or at all, leading to urine accumulation.
Indications & Contraindications
Indications
Neurogenic Conditions
- • Spinal cord injury/disease
- • Multiple sclerosis
- • Spina bifida
- • Traumatic brain injury
- • Stroke with bladder dysfunction
Non-Neurogenic Conditions
- • Benign prostatic hyperplasia
- • Urethral strictures
- • Postoperative urinary retention
- • Overflow incontinence
- • Detrusor underactivity
Postoperative Indications
- • Post-incontinence surgery
- • Botulinum toxin injection
- • Bladder augmentation
- • Urinary diversions
Contraindications
Absolute Contraindications
- • High intravesical pressure requiring continuous drainage
- • Severe urethral trauma or disruption
Relative Contraindications
- • Poor manual dexterity without caregiver support
- • Active urethritis or prostatitis
- • Significant visible hematuria
- • Recent urethral surgery
- • Cognitive impairment without support
Temporary Contraindications
- • Acute urinary tract infection
- • Severe pain or discomfort
- • Acute urethral obstruction
Clinical Decision Making
Key Principle: IC should only be performed when there are symptoms or complications from residual urine volume, not based solely on post-void residual measurements. The decision must consider individual patient factors, quality of life, and potential benefits versus risks.
Catheterization Techniques
Technique Comparison
| Technique | Environment | Catheter | Gloves | Lubricant | Evidence Level |
|---|---|---|---|---|---|
| Sterile | Operating room | Sterile | Sterile | Sterile | LE 4 |
| Aseptic | Healthcare facility | Sterile | Sterile | Sterile | LE 1b |
| Non-touch | Healthcare facility | Sterile/Ready-to-use | Non-sterile | Pre-lubricated | LE 1a |
| Clean | Home setting | Sterile | None | Clean/Sterile | LE 1b |
Healthcare Setting Recommendations
- Aseptic technique for immunocompromised patients
- Non-touch technique for standard hospital patients
- Hydrophilic catheters preferred for reduced trauma
- Single-use catheters mandatory in healthcare settings
Home Setting Recommendations
- Clean technique appropriate for home use
- Hand hygiene essential before procedure
- Genital cleansing with soap and water
- Sterile catheters preferred over reusable
Research Evidence
CDC Guidelines 2024: Moderate-quality evidence shows no significant difference in UTI rates between sterile and clean technique for intermittent catheterization in non-acute care settings. Clean technique is recommended as a practical alternative to sterile technique for most patients.
Equipment & Supplies
Catheter Types & Features
Catheter Materials
- PVC: Cost-effective, standard option
- Silicone: Biocompatible, reduced allergic reactions
- Polyurethane: Durable, smooth surface
- Latex-free: Prevents hypersensitivity reactions
Catheter Coatings
- Hydrophilic: Water-activated, reduces friction
- Pre-lubricated: Gel coating, ready-to-use
- Antimicrobial: Silver-coated (not available in US)
- Uncoated: Requires external lubrication
Catheter Tips
- Nelaton (straight): Standard tip for most patients
- Coudé (curved): For enlarged prostate/obstruction
- Tiemann: Curved tip for difficult insertion
- Introducer tip: Protected insertion sleeve
Essential Supplies
Supply Checklist
Catheter Sizing Guide
Adults: 12-16 Fr (most common: 14 Fr)
Male length: 16-18 inches (40-45 cm)
Female length: 6-8 inches (15-20 cm)
Pediatric: 8-12 Fr (age-dependent)
Safety Considerations
- • Latex-free products mandatory due to allergy risk
- • Single-use catheters preferred to prevent infection
- • Proper disposal of used catheters and supplies
- • Expiration date checking before use
Catheterization Procedures
Procedure Memory Aid – CATHETER
- Consent and explanation
- Assemble equipment
- Thorough hand hygiene
- Hygienic positioning
- Examine and cleanse genitals
- Technique – insert catheter
- Empty bladder completely
- Record and dispose properly
Male Catheterization
Preparation
Explain procedure, ensure privacy, position patient supine with legs slightly apart
Hand Hygiene & Gloving
Perform thorough hand hygiene, don appropriate gloves per technique
Genital Cleansing
Retract foreskin, cleanse glans and meatus with soap and water, front to back
Catheter Preparation
Activate hydrophilic coating or apply lubricant to catheter tip and shaft
Insertion
Insert catheter slowly at 45° angle, advance until urine flows, then 2cm further
Drainage & Removal
Allow complete bladder emptying, slowly withdraw catheter while draining
Female Catheterization
Preparation
Explain procedure, ensure privacy, position patient supine with knees bent and apart
Hand Hygiene & Gloving
Perform thorough hand hygiene, don appropriate gloves per technique
Genital Cleansing
Separate labia, cleanse from front to back: labia majora, minora, then meatus
Catheter Preparation
Activate hydrophilic coating or apply lubricant to catheter tip
Insertion
Insert catheter slowly upward and backward until urine flows, advance completely into bladder
Drainage & Removal
Allow complete bladder emptying, slowly withdraw catheter while draining
Catheterization Decision Flowchart
Clinical Pearls
- • Gentle technique prevents urethral trauma and patient discomfort
- • Never force catheter insertion; resistance may indicate obstruction
- • Complete emptying is essential; reposition catheter if flow stops
- • Slow withdrawal ensures complete bladder drainage
Patient Education
15 Consensus-Based Education Statements
Based on the 2023 expert consensus conference, these evidence-based statements guide best practices for intermittent catheterization education and patient care.
Pre-Education Assessment
Assess patient’s:
- • Understanding of diagnosis and need for catheterization
- • Knowledge of urinary tract anatomy
- • General health status and cognitive ability
- • Physical ability to perform procedure
- • Motivation and emotional readiness
- • Need for psychological support
- • Availability of caregiver support
Social Determinants of Health
Consider impact of:
- • Health literacy levels
- • Socioeconomic factors
- • Cultural and religious beliefs
- • Language barriers
- • Family support systems
- • Access to supplies and healthcare
- • Housing and privacy considerations
Essential Education Components
Technical Skills
Knowledge Areas
Teaching Methodology Best Practices
Instructional Approaches
- • Multimodal learning: Verbal, written, and hands-on
- • Demonstration: Show before patient practice
- • Return demonstration: Verify competence
- • Reinforcement: Repeat key concepts
- • Praise and encouragement: Build confidence
Educational Resources
- • Written materials: Take-home instructions
- • Video resources: Visual learning aids
- • Equipment samples: Hands-on practice
- • Contact information: 24/7 support access
- • Follow-up schedule: Ongoing support plan
Patient Education Memory Aid – EDUCATE
- Explain procedure and benefits
- Demonstrate proper technique
- Understand individual needs
- Confirm competence with return demo
- Address questions and concerns
- Teach complication recognition
- Ensure follow-up support
Evidence-Based Recommendations
Grade A Clean technique is recommended for intermittent self-catheterization
Grade A Single-use catheters are recommended over reusable catheters
Grade B Routine follow-up within 2-4 weeks to reinforce instruction
Grade B Hydrophilic catheters reduce friction and improve comfort
Complications & Management
Complication Categories
Understanding, preventing, and managing complications is essential for safe intermittent catheterization practice. Most complications are preventable with proper technique and patient education.
Infectious Complications
Urinary Tract Infections (UTIs)
Incidence: Most common complication, especially in neurogenic patients
Risk Factors:
- • Infrequent catheterization
- • Bladder overdistension (>500ml)
- • Poor catheterization technique
- • Inadequate fluid intake
- • Uncoated catheters
Prevention: LE 1a
- • Use hydrophilic-coated catheters
- • Maintain catheterization frequency
- • Ensure adequate fluid intake
- • Proper hand hygiene
Epididymo-orchitis
Presentation: Scrotal pain, swelling, fever
Management: Antibiotic therapy, supportive care
Traumatic Complications
Urethral Trauma/Hematuria
Causes: Forced insertion, inadequate lubrication, catheter reuse
Prevention: LE 1a
- • Use hydrophilic-coated catheters
- • Adequate lubrication
- • Gentle technique
- • Proper catheter sizing
Urethral Stricture
Risk: Higher in males, long-term catheterization
Prevention: Minimize trauma, use appropriate catheters
Meatal Stenosis
Presentation: Difficulty inserting catheter, reduced flow
Management: Urological consultation, dilatation
Risk Stratification Framework
| Risk Level | Patient Factors | Interventions | Monitoring |
|---|---|---|---|
| Low | Good technique, compliant, hydrophilic catheters | Standard education, routine follow-up | Annual assessment |
| Moderate | Occasional technique issues, uncoated catheters | Enhanced education, catheter upgrade | Quarterly assessment |
| High | Frequent UTIs, poor technique, trauma history | Intensive education, specialty referral | Monthly assessment |
When to Seek Emergency Care
- • Inability to insert catheter after multiple attempts
- • Gross hematuria that doesn’t clear with subsequent catheterizations
- • Signs of sepsis: fever, chills, altered mental status
- • Severe pain during or after catheterization
- • Autonomic dysreflexia in spinal cord injury patients
Evidence-Based Management
- • Only treat symptomatic UTIs LE 1b
- • Avoid prophylactic antibiotics for asymptomatic bacteriuria
- • Maintain bladder volume <500ml to prevent overdistension
- • Use hydrophilic catheters to reduce trauma and infection
Nursing Implementation
Comprehensive Nursing Approach
Successful nursing implementation of intermittent catheterization requires a holistic approach that addresses technical competence, patient education, psychosocial support, and continuous quality improvement.
Assessment & Planning
Initial Patient Assessment
Physical Assessment:
- • Manual dexterity and range of motion
- • Visual acuity and cognitive function
- • Genital anatomy and sensation
- • Mobility and positioning needs
Psychosocial Assessment
Evaluate:
- • Motivation and readiness to learn
- • Anxiety and coping mechanisms
- • Support system availability
- • Cultural and religious considerations
Environmental Assessment
Consider:
- • Home bathroom accessibility
- • Privacy and dignity needs
- • Storage and disposal options
- • Travel and workplace considerations
Education & Training
Competency-Based Training
Core Competencies:
- • Demonstrate correct technique
- • Explain rationale for each step
- • Recognize complications
- • Perform troubleshooting
Progressive Learning Plan
Phase 1: Knowledge and observation
Phase 2: Supervised practice
Phase 3: Independent demonstration
Phase 4: Competency validation
Individualized Approach
Customize based on:
- • Learning style preferences
- • Literacy level and language
- • Physical limitations
- • Psychosocial needs
Quality Indicators & Outcomes
Process Indicators
- • Adherence to catheterization schedule
- • Proper technique demonstration
- • Appropriate catheter selection
- • Timely follow-up completion
Clinical Outcomes
- • UTI incidence rate
- • Urethral trauma events
- • Bladder function preservation
- • Complication-free catheterization
Patient-Reported Outcomes
- • Quality of life scores
- • Confidence in self-care
- • Satisfaction with care
- • Psychosocial well-being
Documentation Template
Date/Time: ___________
Catheter Type/Size: ___________
Technique Used: ___________
Urine Volume: ___________
Urine Characteristics: ___________
Patient Tolerance: ___________
Complications: ___________
Education Provided: ___________
Follow-up Plan: ___________
Nurse Signature: ___________
Nursing Best Practices
- • Establish rapport before beginning technical training
- • Use positive reinforcement to build confidence
- • Address concerns immediately to prevent anxiety
- • Provide written instructions for reference at home
- • Schedule regular follow-up to ensure continued success
Evidence-Based Practice
2024 EAUN Guidelines Summary
The European Association of Urology Nurses (EAUN) 2024 guidelines provide the most current evidence-based recommendations for intermittent catheterization practice, incorporating systematic reviews and expert consensus.
Grade A Recommendations
Catheter Selection
LE 1a Grade A Use hydrophilic-coated or pre-lubricated catheters to reduce infection and trauma
Evidence: Multiple systematic reviews demonstrate significant reduction in UTI rates and urethral trauma with coated catheters.
UTI Management
LE 1b Grade A Only treat symptomatic UTIs in IC users
Evidence: Randomized controlled trials show no benefit from treating asymptomatic bacteriuria.
Cleansing Technique
LE 1a Grade A Clean urethral meatus with water and pH-neutral soap
Evidence: Meta-analysis shows no benefit of antiseptic solutions over soap and water.
Grade B & C Recommendations
Catheterization Frequency
LE 4 Grade C Bladder volume should not exceed 400-500ml
Evidence: Expert consensus based on physiological principles of bladder compliance.
Patient Education
LE 2b Grade B Provide written, verbal, and practical education
Evidence: Cohort studies demonstrate improved outcomes with multimodal education approaches.
Follow-up Care
LE 2b Grade B Ongoing support and follow-up essential for QoL
Evidence: Longitudinal studies show reduced complications with regular follow-up.
Clinical Scenario Application
Case: 45-year-old male with incomplete spinal cord injury, new to intermittent catheterization
Evidence-Based Approach:
- • Catheter selection: Hydrophilic-coated, 14Fr, Coudé tip (Grade A)
- • Technique: Clean technique for home use (Grade A)
- • Frequency: Every 4-6 hours, volume <500ml (Grade C)
- • Education: Multimodal approach with written materials (Grade B)
- • Follow-up: Phone call at 1 week, visit at 2 weeks (Grade B)
Current Research Priorities
Emerging Areas:
- • Digital health technologies for IC management
- • Personalized catheter selection algorithms
- • Long-term quality of life outcomes
- • Economic evaluations of different catheter types
- • Optimal training methods for healthcare providers
Key References
1. Vahr Lauridsen S, et al. (2024). EAUN Guidelines on Urethral Intermittent Catheterisation in Adults. European Association of Urology Nurses.
2. Quallich S, et al. (2023). Patient Education in Intermittent Catheterization: A Consensus Statement. Journal of Wound, Ostomy & Continence Nursing.
3. CDC. (2024). Evidence Review for Catheter-Associated Urinary Tract Infection Prevention. Centers for Disease Control and Prevention.
4. Rognoni C, Tarricone R. (2017). Intermittent catheterisation with hydrophilic and non-hydrophilic catheters: systematic review and meta-analyses. BMC Urology.
Quality Improvement
Quality Improvement Framework
Continuous quality improvement in intermittent catheterization programs requires systematic measurement, analysis, and improvement of care processes and outcomes.
Key Performance Indicators
Clinical Indicators
- • UTI Rate: <2.5 per 1000 catheter-days
- • Urethral Trauma: <1% of catheterizations
- • Patient Adherence: >90% to prescribed schedule
- • Complication-Free Rate: >95%
Process Indicators
- • Education Completion: 100% of patients
- • Competency Validation: 100% before discharge
- • Follow-up Completion: >95% within 2 weeks
- • Proper Catheter Selection: 100%
Patient-Reported Indicators
- • Satisfaction Score: >4.5/5
- • Quality of Life: Improved from baseline
- • Confidence Level: >8/10
- • Perceived Support: >4/5
Improvement Strategies
Process Improvements
- • Standardized protocols for all settings
- • Competency-based training programs
- • Decision support tools for catheter selection
- • Automated reminders for follow-up care
Technology Integration
- • Electronic health records with IC templates
- • Mobile apps for patient self-monitoring
- • Telehealth platforms for remote support
- • Data analytics for outcome tracking
Staff Development
- • Regular training updates on evidence-based practice
- • Simulation-based learning for complex cases
- • Peer mentoring programs for new nurses
- • Interprofessional collaboration initiatives
PDSA Cycle for IC Quality Improvement
PLAN
Identify improvement opportunity, develop intervention
DO
Implement intervention on small scale
STUDY
Analyze results, measure outcomes
ACT
Standardize successful changes
Quality Improvement Priorities
Short-term Goals (3-6 months)
- • Implement standardized education protocols
- • Achieve 100% competency validation
- • Establish baseline outcome measurements
- • Develop staff training programs
Long-term Goals (1-2 years)
- • Reduce UTI rates by 25%
- • Improve patient satisfaction scores
- • Achieve sustainability of improvements
- • Expand program to all care settings
Summary & Key Takeaways
Essential Nursing Competencies
Mastery of intermittent catheterization requires integration of evidence-based knowledge, technical skills, patient education expertise, and compassionate care to achieve optimal patient outcomes.
Top Clinical Pearls
- • Hydrophilic catheters are gold standard for reducing complications
- • Clean technique is safe and effective for home use
- • Patient education is the cornerstone of successful IC programs
- • Regular follow-up prevents complications and ensures adherence
- • Individualized care addresses unique patient needs and circumstances
Nursing Excellence Tips
- • Build rapport before technical training begins
- • Address fears and concerns with empathy and patience
- • Use positive reinforcement to build confidence
- • Provide multiple learning modalities for different learning styles
- • Ensure accessibility to ongoing support and resources
Evidence-Based Practice Summary
Grade A Recommendations
- • Use hydrophilic-coated catheters LE 1a
- • Only treat symptomatic UTIs LE 1b
- • Clean meatus with soap and water LE 1a
- • Avoid latex-containing products LE 1b
Grade B Recommendations
- • Provide multimodal education LE 2b
- • Follow-up within 2-4 weeks LE 2b
- • Use single-use catheters LE 2a
- • Individualize catheter selection LE 2b
Final Memory Aid – NURSE EXCELLENCE
- Nurse-patient relationship foundation
- Understand individual patient needs
- Respect dignity and privacy
- Safety first in all procedures
- Evidence-based practice implementation
- Education with compassion and patience
- Xcellence in technical competency
- Continuous quality improvement
- Empowerment of patients and families
- Lifelong learning and professional development
- Leadership in advancing nursing practice
- Ethical practice and advocacy
- Nurturing therapeutic relationships
- Collaboration with interdisciplinary teams
- Evaluation and outcome measurement
Continuing Education & Professional Development
Recommended Learning Activities:
- • Attend urology nursing conferences and workshops
- • Participate in interprofessional education programs
- • Engage in quality improvement initiatives
- • Pursue specialty certifications in urological nursing
- • Contribute to research and evidence-based practice
