Chikungunya: A Community Health Nursing Perspective
Comprehensive Notes on Epidemiology, Prevention, Control, Screening, Diagnosis, and Management
Table of Contents
Introduction to Chikungunya
Chikungunya is a viral disease transmitted to humans by infected mosquitoes. It causes fever and severe joint pain, which is often debilitating and can persist for months or even years. The name “chikungunya” derives from a word in the Kimakonde language, meaning “to become contorted,” and describes the stooped appearance of sufferers with joint pain.
Key Facts about Chikungunya
- Caused by Chikungunya virus (CHIKV), an RNA virus belonging to the Alphavirus genus of the family Togaviridae
- Primarily transmitted by Aedes aegypti and Aedes albopictus mosquitoes
- Clinical illness occurs in 72-97% of infected individuals
- No specific antiviral treatment is available
- First described during an outbreak in southern Tanzania in 1952
- Has caused outbreaks in over 60 countries across Africa, Asia, Europe, and the Americas
Epidemiology of Chikungunya
Understanding the epidemiology of Chikungunya is crucial for community health nurses to develop effective prevention and control strategies.
Global Distribution
Chikungunya was initially limited to Africa, Asia, and the Indian subcontinent. However, since 2004, the virus has rapidly expanded its geographical range:
| Region | Key Outbreaks | Estimated Cases | Vector |
|---|---|---|---|
| Africa | Kenya (2004), Tanzania, Sudan | 500,000+ | Mainly Aedes aegypti |
| Asia | India (2006), Thailand, Indonesia | 1.5 million+ | Aedes aegypti and Aedes albopictus |
| Caribbean | First cases in 2013, rapid spread | 1 million+ | Mainly Aedes aegypti |
| Americas | Brazil, Colombia, US (Florida) | 2.5 million+ | Aedes aegypti and Aedes albopictus |
| Europe | Italy (2007), France (2010, 2014) | Hundreds | Mainly Aedes albopictus |
Incidence and Prevalence
The true incidence of Chikungunya is difficult to determine due to:
- Underreporting of cases
- Misdiagnosis with dengue and other febrile illnesses
- Limited surveillance systems in many endemic areas
- Asymptomatic cases (estimated at 3-28% of infections)
During outbreaks, attack rates can range from 30-75% of the population. The seroprevalence in endemic regions can reach 75% following major outbreaks.
Seasonality and Climate Factors
Chikungunya transmission shows seasonal patterns strongly influenced by climate factors that affect mosquito activity:
- Higher incidence during rainy seasons in tropical regions
- Peak transmission during warm, humid months in temperate regions
- Climate change is expanding the geographical range of vector mosquitoes
- Urbanization creates more breeding sites for Aedes mosquitoes
Transmission Cycle
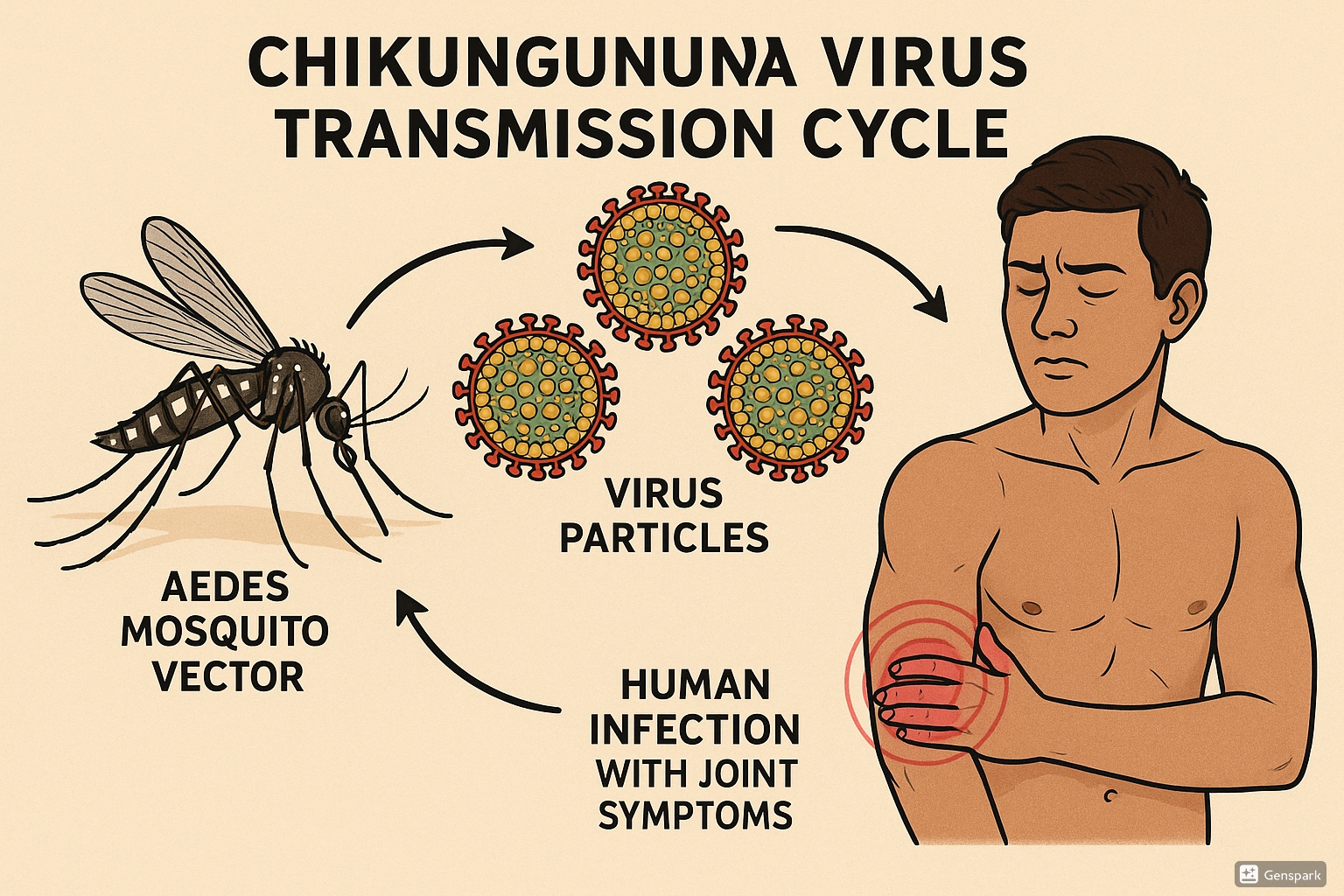
Figure 1: Chikungunya Transmission Cycle – Showing the Aedes mosquito vector, virus particles, and human infection with resulting joint symptoms
Vectors and Transmission Modes
The primary vectors for Chikungunya are:
- Aedes aegypti – Primary urban vector, breeds in artificial containers
- Aedes albopictus (Asian tiger mosquito) – More adaptive to temperate climates, contributing to geographical expansion
Vector Characteristics Important for Nursing Assessment
- Both species are day-biting mosquitoes with peak activity during early morning and late afternoon
- They breed in clean, stagnant water found in containers like flower pots, buckets, and discarded tires
- Aedes mosquitoes have a limited flight range (usually <100 meters) and tend to stay near human habitations
- Female mosquitoes can lay eggs multiple times during their lifetime
- Eggs can survive desiccation for up to one year, making eradication challenging
Transmission Cycle
The transmission of Chikungunya follows this cycle:
- Virus Acquisition: Female mosquito becomes infected by feeding on a viremic human
- Extrinsic Incubation Period: Virus replicates in mosquito’s midgut (8-10 days)
- Virus Transmission: Infected mosquito bites a susceptible human
- Intrinsic Incubation Period: Virus replicates in human (typically 3-7 days, range 1-12 days)
- Viremia: Infected person develops high viral load in blood
- Continued Transmission: Uninfected mosquitoes feed on viremic humans, continuing the cycle
Other Transmission Routes
While mosquito-borne transmission is the primary route, Chikungunya can occasionally be transmitted through:
- Maternal-fetal transmission: Possible during pregnancy, particularly near delivery (intrapartum)
- Blood transfusion: Rare but documented cases
- Laboratory exposure: Accidental exposure in healthcare settings
Important for Community Health Nurses
Unlike dengue, Chikungunya has a higher proportion of symptomatic cases (72-97%). This means most infected individuals will show symptoms, facilitating case detection. However, during the acute phase, patients have high viremia and serve as effective reservoirs for mosquito infection, making prompt isolation and protection from mosquito bites critical.
Clinical Manifestations
Understanding the clinical presentation of Chikungunya is essential for early detection and management. The disease typically progresses through three phases:
| Phase | Timeline | Symptoms | Nursing Implications |
|---|---|---|---|
| Acute Phase | Days 1-14 |
|
|
| Subacute Phase | Weeks 2-12 |
|
|
| Chronic Phase | Beyond 3 months |
|
|
Distinctive Features of Chikungunya
The hallmark feature of Chikungunya is severe debilitating joint pain, which:
- Is typically symmetric and polyarticular, affecting multiple joints
- Most commonly affects wrists, ankles, knees, elbows, and small joints of hands and feet
- May cause swelling, redness, and limited range of motion
- Can persist for months to years in some patients (post-Chikungunya chronic inflammatory rheumatism)
Mnemonic for Chikungunya Symptoms: “CHIKV”
- C – Crippling joint pain (arthralgia)
- H – High fever (>39°C/102°F)
- I – Intense muscle pain (myalgia)
- K – Kin involvement (rash)
- V – Viremia for 5-7 days
Atypical and Severe Manifestations
Although Chikungunya is typically non-fatal, severe and atypical manifestations can occur, particularly in vulnerable populations:
- Neurological: Encephalitis, meningoencephalitis, Guillain-Barré syndrome, seizures
- Cardiovascular: Myocarditis, pericarditis, heart failure
- Ocular: Uveitis, retinitis, optic neuritis
- Renal: Nephritis, acute renal failure
- Hepatic: Hepatitis, liver failure
- Skin: Severe bullous lesions, hyperpigmentation
- Hemorrhagic manifestations: Rare but reported
Risk Factors and Vulnerable Populations
Community health nurses should identify individuals at increased risk for Chikungunya infection and severe disease:
Risk Factors for Infection
- Environmental factors:
- Living in or traveling to endemic areas
- Poor housing conditions (lack of screens, air conditioning)
- Inadequate water storage practices
- Presence of standing water around residences
- Behavioral factors:
- Outdoor activities during peak mosquito biting hours
- Not using personal protective measures (repellents, appropriate clothing)
- Poor compliance with community vector control measures
Vulnerable Populations for Severe Disease
Certain populations are at higher risk for severe complications and chronic symptoms:
| Population Group | Specific Risks | Nursing Considerations |
|---|---|---|
| Neonates |
|
|
| Elderly (>65 years) |
|
|
| Individuals with comorbidities |
|
|
| Pregnant women |
|
|
| Individuals with pre-existing arthritis |
|
|
Risk Factors for Chronic Arthritis
Research has identified several factors that increase the risk of developing persistent joint symptoms after acute Chikungunya infection:
- Age >45 years
- Female gender
- Pre-existing joint disorders
- Severe acute disease (high fever, intense polyarthralgia)
- Delayed initiation of appropriate treatment
Prevention and Control Measures
Community health nurses play a pivotal role in preventing and controlling Chikungunya outbreaks through various interventions at individual, household, and community levels.
Primary Prevention Strategies
These strategies aim to prevent Chikungunya infection by controlling vectors and reducing human-vector contact:
Personal Protection Measures
- Use of EPA-registered insect repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus
- Wearing long-sleeved shirts and long pants
- Using permethrin-treated clothing and gear
- Staying in places with air conditioning or window/door screens
- Using bed nets in endemic areas, especially during daytime naps
Household Vector Control
- Weekly emptying and cleaning of water-holding containers
- Proper disposal of solid waste
- Covering water storage containers
- Clearing rain gutters and flat roofs of standing water
- Using larvicides in standing water that cannot be eliminated
- Indoor residual spraying in high-risk areas
Community-level Interventions
- Environmental management to reduce breeding sites
- Community cleanup campaigns
- Biological control using larvivorous fish or Bacillus thuringiensis israelensis
- Space spraying during outbreaks
- Implementation of integrated vector management (IVM) programs
- Community participation and mobilization
Health Education Strategies
- Public awareness campaigns about Chikungunya transmission
- Education on recognition of symptoms
- School-based educational programs
- Training of community health workers
- Use of mass media, social media, and mobile health platforms
- Door-to-door education in high-risk areas
Mnemonic for Vector Control: “ABCDE”
- A – Avoid mosquito bites (repellents, clothing)
- B – Be aware of peak biting times (early morning, late afternoon)
- C – Cover, empty, or clean water containers weekly
- D – Discard unnecessary containers that collect water
- E – Educate community about mosquito breeding and disease transmission
Secondary Prevention Strategies
These strategies focus on early detection and prompt management to prevent complications and further transmission:
- Enhanced surveillance systems to detect outbreaks early
- Rapid case identification through awareness of clinical symptoms
- Vector surveillance to monitor mosquito density and infection rates
- Contact tracing in newly affected areas
- Isolation precautions for infected individuals during the viremic phase
- Mosquito protection for infected individuals to prevent further transmission
Special Considerations for High-Risk Settings
Community health nurses should prioritize prevention in high-risk settings:
| Setting | Specific Interventions |
|---|---|
| Schools |
|
| Healthcare facilities |
|
| Construction sites |
|
| Residential institutions |
|
Current Status of Chikungunya Vaccines
As of now, there is no commercially available vaccine for Chikungunya. However, several vaccine candidates are in various stages of clinical development, including:
- Live-attenuated vaccines
- Virus-like particle (VLP) vaccines
- Inactivated vaccines
- DNA vaccines
Community health nurses should stay updated on vaccine development progress and be prepared to integrate vaccination into prevention strategies when available.
Screening and Diagnosis
Community health nurses play a crucial role in the early detection of Chikungunya cases through screening, case definition application, and facilitating appropriate diagnostic testing.
Case Definition and Screening
The World Health Organization provides the following case definitions for Chikungunya:
Suspected Case
Patient with acute onset of fever >38.5°C (101.3°F) AND severe arthralgia/arthritis not explained by other medical conditions, AND residing or having visited epidemic or endemic areas within 2 weeks before symptom onset.
Confirmed Case
A suspected case with laboratory confirmation of Chikungunya virus infection through one of the following methods:
- Virus isolation
- Detection of viral RNA by RT-PCR
- Detection of IgM antibodies in a single serum sample
- Four-fold increase in IgG antibody titers in paired serum samples
Screening Questions for Community Health Nurses
When screening for Chikungunya, community health nurses should ask:
- Have you experienced sudden onset of high fever in the past two weeks?
- Are you experiencing severe joint pain in multiple joints?
- Do you have a rash on your body?
- Have you traveled to or do you live in an area with known Chikungunya cases?
- Have you been bitten by mosquitoes recently?
- Are others in your household or community experiencing similar symptoms?
Diagnostic Testing
Laboratory diagnosis of Chikungunya depends on the time since symptom onset:
| Diagnostic Method | Optimal Timing | Specimen Type | Advantages/Limitations |
|---|---|---|---|
| Viral Culture | 0-7 days after onset | Serum, plasma |
|
| RT-PCR | 0-7 days after onset | Serum, plasma, CSF, synovial fluid |
|
| IgM ELISA | 5+ days after onset | Serum |
|
| IgG ELISA | 10+ days after onset (paired specimens) | Serum |
|
| Point-of-care Rapid Diagnostic Tests | Varies by test | Serum, whole blood |
|
Diagnostic Algorithm for Community Health Nurses
- Initial Assessment: Screen using case definition criteria
- Symptom Duration Assessment:
- ≤7 days: Collect specimens for RT-PCR
- >7 days: Collect specimens for serological testing
- Sample Collection and Transport: Ensure proper handling and cold chain maintenance
- Result Interpretation: Correlate with clinical findings
- Notification: Report confirmed cases to public health authorities
Differential Diagnosis
Chikungunya shares clinical features with several other diseases, which must be considered in the differential diagnosis:
| Disease | Key Distinguishing Features |
|---|---|
| Dengue |
|
| Zika |
|
| Malaria |
|
| Leptospirosis |
|
| Rheumatic fever |
|
Co-infection Awareness
In endemic areas, co-infection of Chikungunya with dengue or Zika is possible as they share the same vector. Community health nurses should consider this possibility when symptoms are atypical or severe, or when there is a poor response to treatment.
Primary Management
There is no specific antiviral treatment for Chikungunya. Management is primarily supportive and focuses on alleviating symptoms and preventing complications. Community health nurses play a vital role in educating patients and families about appropriate home-based care.
Acute Phase Management
The goals during the acute phase are to relieve symptoms, maintain hydration, and monitor for complications:
Symptom Management
- Fever control: Acetaminophen/paracetamol (avoid aspirin due to bleeding risk and NSAIDs until dengue is ruled out)
- Pain management: After excluding dengue, NSAIDs may be used for joint pain
- Skin rash: Calamine lotion for itching; cool compresses
- Rest: Advise adequate rest and limited joint movement during acute phase
Hydration and Nutrition
- Encourage increased fluid intake (water, oral rehydration solution)
- Monitor for signs of dehydration, especially in vulnerable populations
- Recommend small, frequent, nutritionally balanced meals
- Assess for difficulty swallowing or feeding, particularly in elderly patients
Home Care Instructions for Patients with Chikungunya
- Take acetaminophen/paracetamol as directed for fever and pain
- Rest in bed under a mosquito net or in a screened room to prevent mosquito bites during the viremic period
- Drink plenty of fluids to prevent dehydration
- Apply cool compresses to painful joints
- Use mosquito repellent on exposed skin
- Return to the healthcare facility if experiencing:
- Persistent high fever beyond 5 days
- Decreased urine output or dark urine
- Severe abdominal pain
- Persistent vomiting
- Bleeding from any site
- Altered mental status
- Difficulty breathing
Subacute and Chronic Phase Management
For patients who develop persistent symptoms beyond the acute phase:
| Intervention Category | Specific Approaches | Nursing Considerations |
|---|---|---|
| Pharmacological |
|
|
| Physical Therapy |
|
|
| Non-pharmacological Pain Management |
|
|
| Lifestyle Modifications |
|
|
Important Medication Considerations
When managing Chikungunya, community health nurses should be aware of these important medication considerations:
- Avoid aspirin during the acute phase due to risk of bleeding and Reye’s syndrome in children
- Avoid NSAIDs until dengue fever is ruled out (can worsen bleeding in dengue)
- Use corticosteroids with caution and only for short duration due to risk of rebound symptoms and adverse effects
- Monitor kidney and liver function in patients on long-term NSAID therapy
- Consider drug interactions with chronic medications, especially in elderly patients
Special Population Considerations
Management approaches must be adapted for specific populations:
- Pregnant women: Acetaminophen/paracetamol is preferred for pain and fever. NSAIDs should be avoided, especially in the third trimester. Close monitoring for vertical transmission near delivery.
- Neonates: Supportive care with close monitoring for encephalopathy. Severe cases may require intensive care.
- Elderly patients: Careful medication selection considering comorbidities and drug interactions. More frequent monitoring for complications and dehydration.
- Patients with comorbidities: Individualized approach with attention to potential exacerbation of underlying conditions.
Referral Criteria
Community health nurses should recognize when patients with Chikungunya require referral to higher levels of care.
Indications for Immediate Referral
- Neurological manifestations: Altered consciousness, seizures, meningoencephalitis, Guillain-Barré syndrome
- Cardiovascular complications: Chest pain, arrhythmias, heart failure
- Severe dehydration: Decreased urine output, dizziness, extreme weakness
- Respiratory distress: Tachypnea, dyspnea, hypoxemia
- Hepatic dysfunction: Jaundice, significantly elevated liver enzymes
- Renal dysfunction: Decreased urine output, elevated creatinine
- Hemorrhagic manifestations: Unusual bleeding from any site
- Neonates with suspected perinatal transmission
- Pregnant women with severe symptoms or near delivery
Referral for Specialized Management
Some patients may require referral to specialists for ongoing management:
| Specialist | Indications for Referral | What to Include in Referral |
|---|---|---|
| Rheumatologist |
|
|
| Neurologist |
|
|
| Physical Therapist |
|
|
| Mental Health Specialist |
|
|
Referral Process
Community health nurses should follow these steps when referring patients:
- Document comprehensive assessment findings
- Communicate clearly with receiving facility or specialist
- Provide a summary of treatments already attempted
- Include relevant laboratory and diagnostic results
- Explain the referral process to the patient and family
- Facilitate transportation arrangements when necessary
- Follow up to ensure the patient received care
- Request feedback from the receiving provider
Mnemonic for Referral Assessment: “REFER”
- R – Risk assessment (identify high-risk features)
- E – Evaluate severity of symptoms
- F – Functional impact assessment
- E – Existing resources assessment (what’s available locally)
- R – Requirements for specialized care
Follow-up Care
Comprehensive follow-up care is essential for patients recovering from Chikungunya, particularly those with persistent symptoms. Community health nurses are ideally positioned to provide continuity of care and monitor for complications.
Follow-up Schedule
The frequency and duration of follow-up depend on symptom severity and recovery progress:
| Patient Category | Recommended Schedule | Key Assessment Points |
|---|---|---|
| Uncomplicated cases with resolution of acute symptoms |
|
|
| Patients with persistent joint symptoms |
|
|
| High-risk patients (elderly, comorbidities) |
|
|
| Pregnant women with Chikungunya |
|
|
| Patients with atypical or severe manifestations |
|
|
Components of Follow-up Assessments
A comprehensive follow-up assessment should include:
Physical Assessment
- Joint examination (swelling, tenderness, range of motion)
- Vital signs
- Skin assessment for persistent rash
- Neurological assessment if indicated
- Functional assessment (ability to perform ADLs)
- Pain assessment using standardized tools
Psychosocial Assessment
- Mental health screening for depression and anxiety
- Impact on family roles and relationships
- Ability to work and financial implications
- Coping strategies
- Support system evaluation
- Quality of life assessment
Treatment Evaluation
- Medication adherence and effectiveness
- Side effect monitoring
- Physical therapy progress
- Response to non-pharmacological interventions
- Need for treatment modifications
- Specialist recommendations review
Education Reinforcement
- Disease progression and expected recovery
- Self-management strategies
- Symptoms requiring immediate attention
- Joint protection techniques
- Vector control measures to protect family
- Community resources available
Long-term Monitoring Considerations
For patients with chronic symptoms, ongoing monitoring should include:
- Periodic laboratory assessment: Complete blood count, inflammatory markers, liver and kidney function if on long-term medications
- Quality of life reassessment: Using validated tools to track improvement or deterioration
- Functional capacity evaluation: Objective measurement of progress in physical capabilities
- Comorbidity management: Ensure underlying conditions are optimally controlled
- Psychosocial support needs: Reassess as the chronic condition persists
Documentation Tools for Follow-up
Community health nurses should use structured documentation tools to ensure comprehensive follow-up:
- Joint symptom diary: Track location, severity, and duration of joint symptoms
- Pain scales: Visual analog scale or numerical rating scale
- Functional assessment scales: Health Assessment Questionnaire (HAQ) or similar tools
- Quality of life measures: SF-36 or disease-specific tools
- Mental health screening: PHQ-9 for depression, GAD-7 for anxiety
Nursing Care Plan
A comprehensive nursing care plan for patients with Chikungunya addresses their specific needs across the continuum of care.
| Nursing Diagnosis | Expected Outcomes | Nursing Interventions | Evaluation |
|---|---|---|---|
| Acute Pain related to joint inflammation |
|
|
|
| Hyperthermia related to viral infection |
|
|
|
| Impaired Physical Mobility related to joint pain and stiffness |
|
|
|
| Risk for Secondary Infection Transmission related to viremia |
|
|
|
| Deficient Knowledge related to disease process and management |
|
|
|
Nursing Priorities for Chronic Chikungunya Cases
For patients with chronic Chikungunya arthritis, nursing priorities include:
- Functional assessment and interventions to maintain independence
- Chronic pain management strategies beyond medications
- Psychological support for coping with chronic symptoms
- Education on activity pacing and energy conservation
- Coordination of multidisciplinary care (rheumatology, physical therapy, occupational therapy)
Community-based Interventions
Community health nurses are key implementers of population-level interventions to control Chikungunya and mitigate its impact.
Surveillance and Early Warning Systems
Effective surveillance is the foundation of Chikungunya prevention and control:
- Case-based surveillance: Identifying and reporting suspected and confirmed cases
- Syndromic surveillance: Monitoring clusters of fever and arthralgia
- Vector surveillance: Monitoring Aedes mosquito indices in high-risk areas
- Sentinel surveillance: Targeted monitoring in selected healthcare facilities
- Laboratory-based surveillance: Confirmation of suspected cases
Community Nursing Role in Surveillance
- Maintain case registers for suspected and confirmed cases
- Conduct active case finding during outbreaks
- Collect and transport specimens for testing
- Map cases to identify clusters and potential breeding sites
- Submit timely reports to public health authorities
- Participate in analysis of local surveillance data
Community Mobilization and Education
Empowering communities is essential for sustainable vector control:
Educational Strategies
- Community workshops and town hall meetings
- School-based education programs
- Distribution of educational materials
- House-to-house visits by health workers
- Mass media and social media campaigns
- Demonstration of vector control methods
Community Participation Approaches
- Formation of community vector control committees
- Training of community health volunteers
- Community cleanup campaigns
- School and youth involvement in vector control
- Faith-based organization partnerships
- Community-based vector surveillance
Outbreak Response
When Chikungunya outbreaks occur, community health nurses should implement a coordinated response:
- Alert and notification: Rapid reporting to authorities and community stakeholders
- Case management: Setting up treatment centers if needed, ensuring supplies of medicines
- Vector control intensification: Emergency space spraying, focused larviciding, community cleanup
- Risk communication: Clear, consistent messages about prevention and care-seeking
- Coordination: Working with multi-sectoral partners (local government, education, sanitation)
- Monitoring: Tracking outbreak progress and effectiveness of interventions
Mnemonic for Community Chikungunya Response: “VECTOR”
- V – Vigilant surveillance and case finding
- E – Educate the community about prevention
- C – Clean up breeding sites regularly
- T – Treat cases appropriately
- O – Organize community participation
- R – Report and document control activities
Vulnerable Population Outreach
Special attention should be given to reaching vulnerable populations:
- Pregnant women: Integration of Chikungunya prevention education into antenatal care
- Elderly populations: Education through senior centers, home visits, caregiver training
- Slum/informal settlements: Targeted vector control, community champions, adapted education
- Remote/rural communities: Mobile outreach, radio messaging, community health worker training
- Migrant populations: Culturally appropriate education, accessing through employers
Intersectoral Collaboration
Effective Chikungunya prevention requires collaboration across sectors:
- Healthcare sector: Case management, surveillance, health education
- Municipal authorities: Waste management, water supply improvements
- Education sector: School-based education, school premises vector control
- Housing and urban planning: Improved housing design, drainage systems
- Private sector: Workplace prevention programs, sponsorship of campaigns
- Media: Public awareness campaigns, accurate reporting of outbreaks
- NGOs and community organizations: Community mobilization, volunteer coordination
Global Best Practices
Various regions have developed effective approaches to Chikungunya prevention and control that can inform nursing practice:
Singapore’s Integrated Approach
Singapore has implemented a comprehensive vector control program that includes:
- Legal framework with penalties for harboring breeding sites
- “Mozzie Wipeout” campaign focusing on systematic household inspection
- Detailed breeding site mapping using GIS technology
- Inter-agency coordination through the National Environment Agency
- Community ownership through volunteer “Dengue Prevention Volunteers”
Application: Community health nurses can adopt the systematic inspection approach and use of technology for mapping high-risk areas.
Cuba’s Community Participation Model
Cuba’s successful approach includes:
- Integration of vector control into the primary healthcare system
- Family physician and nurse teams conducting regular household inspections
- Community Working Groups for active participation
- Weekly fumigation schedules during high-risk seasons
- School-based “Pioneer” movement for youth involvement
Application: The integration of vector control into routine primary healthcare services and strong community involvement structure can be adapted to many settings.
India’s NVBDCP Approach
India’s National Vector Borne Disease Control Programme features:
- Integrated vector management approach
- ASHA workers (community health volunteers) as first-line responders
- Biological control with larvivorous fish in appropriate water bodies
- Special drive “Dry Day” once weekly for container inspection
- Epidemic preparedness and rapid response teams at district level
Application: The use of community health volunteers and simple, consistent messaging like “Dry Day” can be effective in resource-limited settings.
Innovative Approaches
Emerging technologies and approaches show promise for enhanced Chikungunya control:
- Wolbachia-infected mosquitoes: Reducing vector competence for Chikungunya transmission
- Genetically modified mosquitoes: Reducing mosquito populations through sterile male release
- Spatial repellent technologies: Such as transfluthrin-treated materials for household protection
- Mobile health applications: For surveillance, education, and reporting of breeding sites
- Remote sensing and predictive modeling: To forecast outbreaks based on environmental conditions
- Community-based trap systems: Such as lethal ovitraps for vector monitoring and control
Adapting Global Practices Locally
When adapting global best practices, community health nurses should consider:
- Local vector ecology and breeding preferences
- Cultural beliefs and practices related to disease and prevention
- Existing healthcare infrastructure and resources
- Seasonal patterns and climate factors
- Community leadership structures and decision-making processes
- Legislative and policy environment for vector control
Resources for Nurses
Community health nurses can utilize these resources for further information and professional development regarding Chikungunya:
Clinical Guidelines and Protocols
- World Health Organization (WHO): Chikungunya Fact Sheet
- Pan American Health Organization (PAHO): Chikungunya Guidelines for Patient Care
- CDC: Information for Healthcare Providers
- National Vector Borne Disease Control Programme (India): Clinical Management Guidelines
Educational Materials
- CDC Chikungunya Communication Resources: Educational Materials for Patients
- WHO Training Materials on Vector-Borne Diseases: Training Module on Chikungunya
- Nursing Center CE Articles: Continuing Education on Arboviral Diseases
Professional Development
- Tropical Nursing Certificate Programs through universities and online platforms
- WHO Global Learning Laboratory for Quality Universal Health Coverage: Learning Opportunities
- Global Outbreak Alert and Response Network (GOARN) Training: Outbreak Response Training
Community Tools and Resources
- PAHO Toolkit for Community Engagement: Aedes aegypti Control
- WHO Handbook for Integrated Vector Management: IVM Guidelines
- CDC’s ArboNET: Surveillance Resources
Nursing Professional Organizations with Vector-Borne Disease Resources
- International Council of Nurses (ICN): Position Statements on Infectious Diseases
- Association of Community Health Nursing Educators (ACHNE): Community Health Resources
- American Public Health Association (APHA): Public Health Nursing Section
- Transcultural Nursing Society: Cultural Considerations in Care
References
- World Health Organization. (2023). Chikungunya. https://www.who.int/news-room/fact-sheets/detail/chikungunya
- Centers for Disease Control and Prevention. (2023). Chikungunya Virus: Information for Healthcare Providers. https://www.cdc.gov/chikungunya/hc/index.html
- Pan American Health Organization. (2023). Chikungunya. https://www.paho.org/en/topics/chikungunya
- Staples, J. E., Breiman, R. F., & Powers, A. M. (2009). Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clinical infectious diseases, 49(6), 942-948.
- Javelle, E., Ribera, A., Degasne, I., Gaüzère, B. A., Marimoutou, C., & Simon, F. (2015). Specific management of post-chikungunya rheumatic disorders: a retrospective study of 159 cases in Reunion Island from 2006-2012. PLoS neglected tropical diseases, 9(3), e0003603.
- Weaver, S. C., & Lecuit, M. (2015). Chikungunya virus and the global spread of a mosquito-borne disease. New England Journal of Medicine, 372(13), 1231-1239.
- Simon, F., Javelle, E., Cabie, A., Bouquillard, E., Troisgros, O., Gentile, G., … & Société de pathologie infectieuse de langue française. (2015). French guidelines for the management of chikungunya (acute and persistent presentations). Médecine et Maladies Infectieuses, 45(7), 243-263.
- Elsinga, J., Gerstenbluth, I., van der Ploeg, S., Halabi, Y., Lourents, N. T., Burgerhof, J. G., … & Tami, A. (2017). Long-term chikungunya sequelae in Curaçao: burden, determinants, and a novel classification tool. Journal of Infectious Diseases, 216(5), 573-581.
- Vijayakumar, K. P., Nair Anish, T. S., George, B., Lawrence, T., Muthukkutty, S. C., & Ramachandran, R. (2011). Clinical profile of chikungunya patients during the epidemic of 2007 in Kerala, India. Journal of global infectious diseases, 3(3), 221.
- Kantor, I. N. (2016). Dengue, Zika and Chikungunya. Medicina, 76(2), 93-97.
