Convulsive Disorders
Comprehensive Nursing Notes for Seizures & Epilepsy
1. Introduction to Convulsive Disorders
Convulsive disorders are neurological conditions characterized by sudden, abnormal electrical discharges in the brain, resulting in changes in behavior, consciousness, movement, or sensation. Seizures are the primary manifestation of these disorders, and when seizures occur recurrently without a clear precipitating cause, the condition is termed epilepsy.
Seizure
A transient occurrence of signs and symptoms resulting from abnormal excessive or synchronous neuronal activity in the brain. A single seizure does not necessarily indicate epilepsy.
Epilepsy
A chronic neurological disorder characterized by recurrent, unprovoked seizures. Diagnosis typically requires at least two unprovoked seizures occurring >24 hours apart.
Clinical Pearl:
Not all seizures represent epilepsy. Seizures can be provoked by metabolic disorders, drug toxicity, alcohol withdrawal, or acute neurological insults. A thorough history is crucial for accurate diagnosis.
2. Pathophysiology of Seizures
Seizures result from an imbalance between excitatory and inhibitory neurotransmission in the brain, leading to synchronized neuronal discharges.
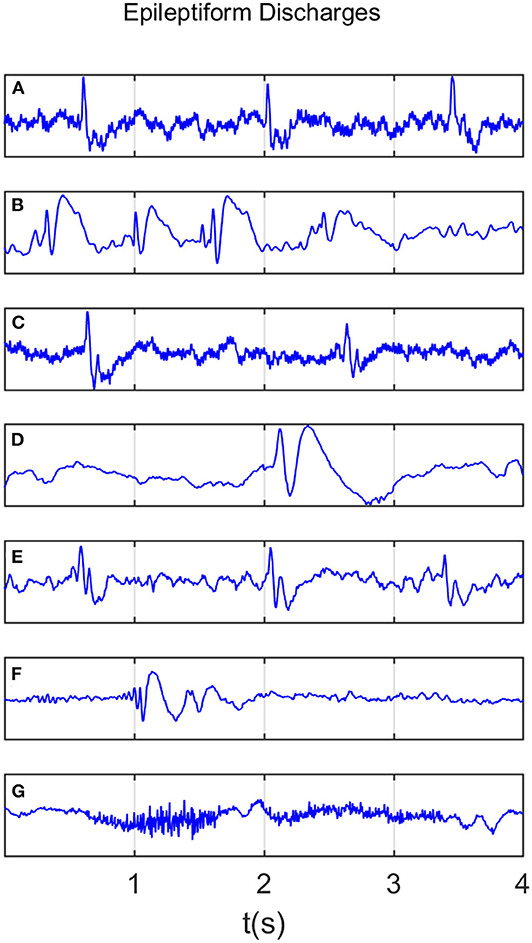
Figure 1: EEG showing typical epileptiform discharges with characteristic spike-wave patterns.
Key Pathophysiological Mechanisms:
Excessive Neuronal Excitability
Caused by increased action of excitatory neurotransmitters (glutamate) or decreased action of inhibitory neurotransmitters (GABA).
Abnormal Neuronal Synchronization
Neurons fire in an abnormally synchronized pattern instead of the typical asynchronous firing.
Ion Channel Dysfunction
Abnormalities in sodium, potassium, or calcium channels affecting membrane stability.
Structural Abnormalities
Brain tumors, cortical dysplasias, scarring, or other lesions creating hyperexcitable foci.
Mnemonic: “VITAMIN” – Common Causes of Seizures
V – Vascular (stroke, hemorrhage)
I – Infection (meningitis, encephalitis)
T – Trauma (head injury)
A – AV malformation
M – Metabolic disorders
I – Idiopathic/Inherited
N – Neoplasms (tumors)
Remember:
Seizure thresholds vary from person to person. Factors that can lower the seizure threshold include:
- Sleep deprivation
- Alcohol or drug withdrawal
- Stress
- Fever
- Hormonal changes (e.g., menstruation)
- Certain medications
- Flickering lights (photosensitive epilepsy)
3. Classification of Seizure Types
In 2017, the International League Against Epilepsy (ILAE) revised the classification of seizure types. This classification is based on:
- Site of onset in the brain
- Level of awareness during seizure
- Other features (motor vs. non-motor)

Figure 2: ILAE 2017 Classification of Seizure Types (Expanded Version)
Focal Onset Seizures
Begin in one hemisphere of the brain. Can be further classified by awareness level:
Focal Aware (formerly Simple Partial)
- Consciousness preserved
- Patient remains aware and can recall events
- May experience sensory, autonomic, or psychic symptoms
- Can involve motor symptoms in one part of the body
Focal Impaired Awareness (formerly Complex Partial)
- Altered consciousness
- Patient may appear confused or dazed
- Often exhibits automatisms (repetitive movements like lip-smacking, chewing)
- May wander or perform purposeless activities
- Typically lasts 1-2 minutes
Focal to Bilateral Tonic-Clonic (formerly Secondary Generalized)
- Begins as focal seizure then spreads to both hemispheres
- Progresses to tonic-clonic movements involving the entire body
- Complete loss of consciousness
Generalized Onset Seizures
Begin in both hemispheres simultaneously. Always involve impaired awareness. Types include:
Absence (formerly Petit Mal)
- Brief lapses in awareness (typically 5-10 seconds)
- Blank stare, sometimes with minor facial movements
- No postictal confusion
- May occur multiple times daily
- Common in children
Tonic-Clonic (formerly Grand Mal)
- Tonic phase: muscle rigidity/stiffening (10-20 seconds)
- Clonic phase: rhythmic jerking movements (1-3 minutes)
- Complete loss of consciousness
- Often accompanied by:
- Tongue biting
- Urinary incontinence
- Respiratory changes
- Postictal confusion/sleepiness
Myoclonic
- Brief, shock-like muscle jerks
- May involve face, limbs, or entire body
- Consciousness usually preserved
Atonic (Drop Attacks)
- Sudden loss of muscle tone
- May cause falls and injuries
- Brief duration (seconds)
Unknown Onset Seizures
When the onset of a seizure is not clearly identified or observed.
Epileptic Spasms
- Sudden flexion or extension of limbs/trunk
- Occur in clusters
- Common in infants (infantile spasms)
Clinical Pearl:
Always try to classify seizures accurately as it guides treatment decisions. For example, absence seizures respond to ethosuximide, while this drug is ineffective for focal seizures.
4. Clinical Presentation
Phases of a Seizure
1. Prodromal Phase
Occurs hours to days before seizure. Patient may experience:
- Mood changes
- Irritability
- Headache
- Sleep disturbances
- Not all patients experience this phase
2. Ictal Phase
The actual seizure. Manifestations depend on seizure type:
- Altered consciousness
- Motor symptoms
- Sensory changes
- Autonomic symptoms
- Duration: seconds to minutes
3. Postictal Phase
Period following the seizure. May include:
- Confusion
- Fatigue/sleepiness
- Headache
- Muscle soreness
- Memory loss of the event
- Duration: minutes to hours
Mnemonic: “TDOC” – Seizure Documentation
When documenting a seizure, remember to include:
- T – Type (focal, generalized, etc.)
- D – Duration (how long did it last?)
- O – Onset (how did it begin? any triggers?)
- C – Complications (injuries, status epilepticus, etc.)
Mnemonic: “FACT” – Quick History for Seizure Assessment
- F – Focus: generalized vs. local activity
- A – Activity: describe specific movements (tonic-clonic vs. absence)
- C – Color: red, blue, ashen (possible hypoxia)
- T – Time: duration of seizure activity
5. Diagnostic Evaluation
| Diagnostic Test | Purpose | Findings in Seizure Disorders |
|---|---|---|
| Electroencephalogram (EEG) | Records brain’s electrical activity |
|
| Neuroimaging (MRI) | Evaluates brain structure |
|
| CT Scan | Rapid assessment for acute causes |
|
| Laboratory Tests | Rule out metabolic causes |
|
| Lumbar Puncture | Rule out CNS infection |
|

Figure 3: EEG showing epileptiform activity with left temporal spikes.
Important:
A single normal EEG does not rule out epilepsy. Up to 50% of patients with epilepsy may have a normal routine EEG. Consider prolonged or sleep-deprived EEG if clinical suspicion is high.
6. Nursing Assessment
History Taking
- Detailed seizure description (from patient and witnesses)
- Age at onset and frequency of seizures
- Triggers (sleep deprivation, stress, alcohol)
- Presence of aura
- Family history of seizures
- History of head trauma, CNS infections
- Developmental history (for pediatric patients)
- Current medications and compliance
- Substance use (alcohol, recreational drugs)
Physical Assessment
- Vital signs including temperature
- Neurological examination
- Level of consciousness
- Signs of trauma (tongue biting, injuries)
- Assess for postictal state
- Signs of metabolic disorders
- Signs of infection
- Evidence of other medical conditions
Seizure Observation and Documentation
Accurately document the following:
- Time of onset and duration
- Body parts involved initially and progression
- Level of consciousness
- Eye movements/deviation
- Color changes
- Presence of automatisms
- Incontinence
- Postictal behavior and duration
- Response to interventions
- Possible precipitating factors
7. Nursing Care and Interventions
Care During a Seizure
Mnemonic: “The Three S’s” of Seizure First Aid
STAY
Stay with the person until they are fully conscious and aware.
SAFE
Keep the person safe by removing harmful objects and protecting their head.
SIDE
Turn the person onto their side if possible to maintain airway patency.
DO
- Time the seizure
- Protect from injury (remove dangerous objects)
- Loosen tight clothing around neck
- Place something soft under the head if possible
- Turn to recovery position after convulsions stop
- Stay with patient until fully recovered
- Reassure and reorient after seizure
- Document seizure characteristics
DO NOT
- Restrain movements
- Put anything in the mouth
- Try to stop the seizure
- Give food, drink, or medications by mouth until fully alert
- Move the person unless in danger
Ongoing Nursing Care
Safety Interventions
- Implement seizure precautions
- Padded side rails if hospitalized
- Bed in low position
- Avoid restraints
- Supervise ambulation as needed
- Fall risk assessment
Medication Management
- Administer antiepileptic drugs as prescribed
- Monitor for therapeutic effects
- Assess for adverse effects
- Monitor drug levels when indicated
- Educate about importance of adherence
- Check for drug interactions
Education & Support
- Teach seizure recognition and first aid
- Discuss safety measures
- Lifestyle modifications to reduce triggers
- Medication education
- Support for psychological impact
- Resources for patients and families
Clinical Pearl:
The psychological impact of seizure disorders can be significant. Patients may experience anxiety, depression, stigma, and fear of having seizures in public. Holistic nursing care should address these psychosocial aspects alongside physical care.
8. Pharmacological Management
Antiepileptic drugs (AEDs), also called antiseizure medications (ASMs), are the mainstay of epilepsy treatment. Selection is based on seizure type, patient characteristics, side effects, and comorbidities.
Nursing Considerations for AEDs:
- Many AEDs require gradual titration when starting or stopping
- Abrupt discontinuation can precipitate seizures or status epilepticus
- Monitor for drug-specific adverse effects
- Many AEDs have significant drug interactions
- Some require therapeutic drug monitoring (phenytoin, carbamazepine, valproate)
- Special considerations for pregnancy (teratogenic potential)
AED Side Effect Mnemonics
Phenytoin: “Some People Have Crazy Noggin Diseases”
Valproic Acid: “WATCH”
9. Status Epilepticus
Definition
Status epilepticus (SE) is a medical emergency defined as:
- Seizure activity lasting ≥5 minutes, OR
- Two or more seizures without full recovery of consciousness between them
Types of Status Epilepticus
- Convulsive Status Epilepticus: Most common and dangerous form with continuous tonic-clonic movements
- Non-convulsive Status Epilepticus: Prolonged altered mental status without obvious convulsive movements
- Focal Status Epilepticus: Continuous focal seizure activity
- Absence Status Epilepticus: Prolonged confusion with minimal motor manifestations
Complications
- Neuronal damage/death
- Cerebral edema
- Hypoxic brain injury
- Metabolic acidosis
- Hyperthermia
- Rhabdomyolysis
- Aspiration pneumonia
- Cardiac arrhythmias
- Respiratory failure
- Death
Management of Status Epilepticus
| Time | Steps | Nursing Considerations |
|---|---|---|
| 0-5 minutes |
|
|
| 5-20 minutes |
|
|
| 20-40 minutes |
|
|
| 40+ minutes |
|
|
Critical Nursing Alert!
Status epilepticus is a medical emergency with a significant mortality rate. For every minute seizure activity continues, the chance of stopping it decreases. Prompt recognition and intervention are essential to prevent neurological damage.
10. Febrile Seizures
Overview
Febrile seizures are convulsions that occur in children between 6 months and 5 years of age, associated with fever (temperature ≥100.4°F/38°C) without evidence of intracranial infection or defined cause.
Key Points:
- Most common seizure disorder in childhood (2-5% of children)
- Peak incidence: 12-18 months of age
- More common in males
- Family history is often present
- Typically benign with excellent prognosis
- Low risk (2-7%) of developing epilepsy later in life
Types of Febrile Seizures
Simple Febrile Seizures:
- Brief (less than 15 minutes)
- Generalized (not focal)
- Occur once in a 24-hour period
- No neurological abnormalities afterward
- Excellent prognosis
Complex Febrile Seizures:
- Prolonged (>15 minutes)
- Focal features
- Recur within 24 hours
- May have postictal neurological abnormalities
- Higher risk of subsequent epilepsy
Nursing Management of Febrile Seizures
During Seizure:
- Ensure airway patency
- Position child on side
- Do not restrain
- Remove objects that could cause injury
- Time the seizure
- Observe and document seizure characteristics
After Seizure:
- Assess vital signs
- Check temperature
- Administer antipyretics as prescribed
- Tepid sponging if appropriate
- Maintain hydration
- Identify and treat the source of fever
Parent Education:
- Reassurance about benign nature of most febrile seizures
- First aid measures for seizures
- Fever management techniques
- When to seek emergency care:
- Seizure lasting >5 minutes
- Difficulty breathing
- Bluish discoloration
- Repeated seizures
- Adherence to follow-up appointments
Clinical Pearl:
Simple febrile seizures do not require routine neuroimaging, EEG, or anticonvulsant prophylaxis. The primary focus should be on identifying and treating the underlying cause of fever and providing parental education and support.
11. Patient and Family Education
Seizure Management
- Recognition of seizure warning signs (aura)
- First aid measures for seizures
- When to seek emergency care
- Importance of keeping a seizure diary
- Tracking potential triggers
- Safety precautions at home
Medication Teaching
- Importance of medication adherence
- Taking medications at scheduled times
- Never abruptly stopping medications
- Side effects to monitor
- Potential drug interactions
- What to do if a dose is missed
Lifestyle Modifications
- Adequate sleep hygiene
- Stress management techniques
- Regular exercise
- Avoiding alcohol and recreational drugs
- Maintaining regular meals
- Avoiding known triggers
Special Considerations:
Pregnancy Planning:
- Preconception counseling
- Medication adjustments (some AEDs are teratogenic)
- Folate supplementation
- Close monitoring during pregnancy
Driving Regulations:
- Varies by location/country
- Typically seizure-free period required (often 3-12 months)
- Legal reporting requirements
- Alternative transportation options
Community Resources and Support
- Epilepsy Foundation and local support groups
- Financial assistance programs for medications
- Vocational rehabilitation services
- School accommodations (504 plans, IEPs)
- Medical alert identification
- Seizure response dogs
Mind Map: Convulsive Disorders

Figure 4: Mind Map of Epilepsy Classification according to ILAE 2017 guidelines.
Key Takeaways
Clinical Assessment
- Accurate seizure classification guides treatment
- Detailed seizure description is crucial (TDOC)
- Distinguish epileptic from non-epileptic events
- EEG and neuroimaging are key diagnostic tools
- Always consider underlying causes (VITAMIN)
Nursing Management
- Patient safety is the priority during seizures
- The Three S’s: Stay, Safe, Side
- Status epilepticus requires urgent intervention
- Medication management and adherence are critical
- Address psychological and social aspects of care
Final Clinical Pearl:
Seizure disorders are much more than just the seizures themselves. They impact all aspects of a patient’s life including relationships, employment, self-esteem, and independence. Holistic nursing care should address not just the management of seizures but the person as a whole, providing education, emotional support, and advocacy to improve quality of life.
