Comprehensive Guide to Maternal Nutrition & Care Partners
Evidence-based approaches for improved maternal outcomes and family-centered care
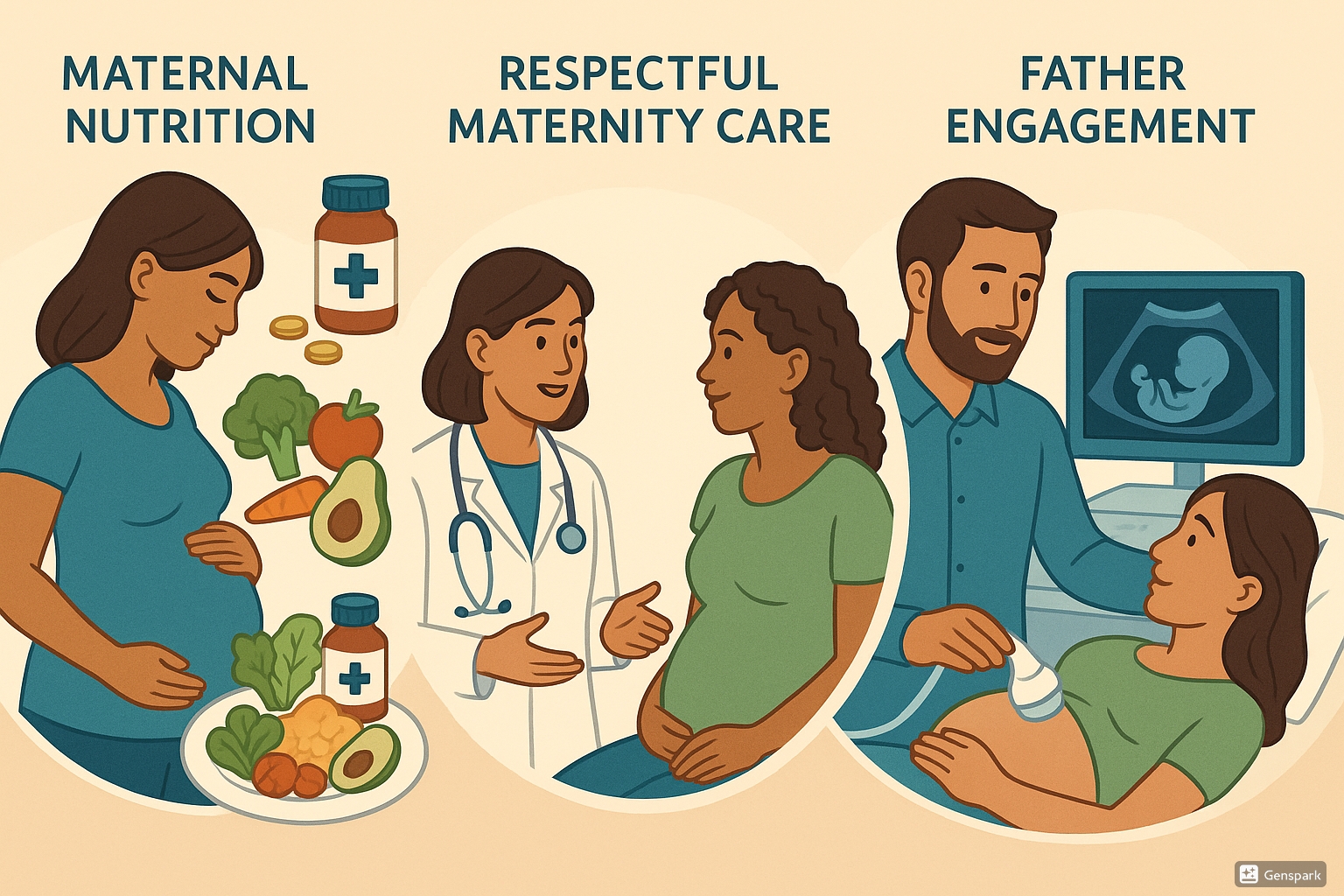
This comprehensive guide provides nursing students with evidence-based knowledge on three interconnected aspects of maternity care: maternal nutrition, respectful maternity care protocols, and father engagement in maternity services. These components work together to create a holistic approach to maternal wellbeing and positive family outcomes.
Table of Contents
Introduction
The health and wellbeing of mothers and their infants are interconnected and foundational to public health. This guide focuses on three critical aspects of maternity care that, when implemented together, can significantly improve outcomes for mothers, infants, and families.
Optimal maternity care requires attention to maternal nutrition, respectful care practices, and meaningful engagement of fathers or partners. This comprehensive approach acknowledges that pregnancy and childbirth are not just physiological events but social, emotional, and familial experiences that can have lasting impact on family dynamics and child development.
As nursing professionals, understanding the evidence behind these practices and implementing them in clinical settings can transform maternity care delivery and improve both short and long-term outcomes for families.
Maternal Nutrition
Proper nutrition during pregnancy is fundamental to both maternal and fetal health, influencing birth outcomes and setting the foundation for lifelong health.
Importance of Maternal Nutrition
Maternal nutrition plays a vital role in pregnancy outcomes and child development. Adequate nutrition before and during pregnancy provides essential nutrients for optimal fetal growth, reduces risks of birth defects, and supports maternal health throughout pregnancy and lactation.
Key Impact Areas of Maternal Nutrition
- Fetal growth and development
- Placental function and health
- Maternal energy levels and wellbeing
- Birth weight and pregnancy outcomes
- Lactation and breastfeeding success
- Long-term child developmental outcomes
- Reduced risk of chronic disease in both mother and child
Nutritional Requirements
Pregnancy increases women’s nutritional needs significantly. Understanding these changes is essential for providing appropriate nutritional counseling.
| Nutrient | Pre-pregnancy Requirement | Pregnancy Requirement | Key Sources | Function |
|---|---|---|---|---|
| Energy | ~2,000 kcal/day | +300 kcal/day (2nd trimester) +300-500 kcal/day (3rd trimester) |
Whole grains, lean proteins, healthy fats | Supports increased metabolic demands and fetal growth |
| Protein | 0.8g/kg/day | 1.1g/kg/day | Lean meats, dairy, legumes, nuts | Tissue development, enzyme production, hormone regulation |
| Iron | 18mg/day | 27mg/day | Red meat, beans, spinach, fortified cereals | Hemoglobin production, oxygen transport, prevents anemia |
| Folate | 400μg/day | 600μg/day | Leafy greens, citrus, beans, fortified grains | Neural tube development, DNA synthesis, cell division |
| Calcium | 1,000mg/day | 1,000mg/day | Dairy products, fortified non-dairy milk, leafy greens | Fetal bone and teeth development, maternal bone health |
| Vitamin D | 15μg/day (600 IU) | 15μg/day (600 IU) | Sunlight, fatty fish, fortified dairy and cereals | Calcium absorption, bone health, immune function |
| Zinc | 8mg/day | 11mg/day | Meat, shellfish, legumes, nuts | Cell division, protein synthesis, immune function |
| Iodine | 150μg/day | 220μg/day | Iodized salt, seafood, dairy | Thyroid function, neurological development |
Mnemonic: “PREGNANT” Nutrients
- P – Protein (increased needs for tissue building)
- R – Red blood cell nutrients (iron, B12, folate)
- E – Energy (additional calories for maternal and fetal needs)
- G – Growth vitamins (A, D, K)
- N – Neurological nutrients (iodine, choline, DHA)
- A – Antioxidants (vitamins C, E, selenium)
- N – Necessary minerals (calcium, magnesium, zinc)
- T – Trace elements (copper, manganese)
Nutrition Assessment & Interventions
Comprehensive nutritional assessment is essential for identifying and addressing nutritional risks during pregnancy.
Assessment Components
- Pre-pregnancy BMI calculation
- Weight gain monitoring
- Dietary recall and food frequency questionnaire
- Biochemical markers (hemoglobin, ferritin, etc.)
- Screening for food insecurity
- Evaluation of nutrition-related symptoms
- Assessment of cultural/religious food practices
Recommended Interventions
- Personalized nutritional counseling
- Prenatal vitamin supplementation
- Iron supplementation (based on hemoglobin levels)
- Dietary modifications for common pregnancy complications
- Referral to dietitian when indicated
- Connection to food assistance programs if needed
- Education on food safety in pregnancy
Recommended Weight Gain During Pregnancy
| Pre-pregnancy BMI Category | BMI Range (kg/m²) | Recommended Weight Gain (kg) | Rate of Weight Gain in 2nd and 3rd Trimesters |
|---|---|---|---|
| Underweight | <18.5 | 12.5-18 | 0.51 kg/week |
| Normal Weight | 18.5-24.9 | 11.5-16 | 0.42 kg/week |
| Overweight | 25.0-29.9 | 7-11.5 | 0.28 kg/week |
| Obese | ≥30.0 | 5-9 | 0.22 kg/week |
| Twin Pregnancy | – | 16-24 | 0.68 kg/week |
Maternal Malnutrition & Outcomes
Malnutrition during pregnancy—whether undernutrition or overnutrition—can have serious consequences for both mother and child.
Consequences of Undernutrition
| Maternal Impact | Fetal/Child Impact |
|---|---|
| Anemia and fatigue | Low birth weight |
| Poor wound healing | Intrauterine growth restriction |
| Increased infection risk | Preterm birth |
| Pregnancy complications | Birth defects |
| Postpartum depression | Developmental delays |
| Reduced breastmilk production | Long-term metabolic programming |
Consequences of Overnutrition
| Maternal Impact | Fetal/Child Impact |
|---|---|
| Gestational diabetes | Macrosomia (large for gestational age) |
| Hypertensive disorders | Birth trauma |
| Increased cesarean delivery | Childhood obesity risk |
| Postpartum hemorrhage | Increased risk of stillbirth |
| Postpartum weight retention | Insulin resistance |
| Increased complications with anesthesia | Neurodevelopmental disorders |
Important Note:
The first 1,000 days (from conception to age 2) represent a critical window for nutrition intervention. Maternal nutrition during this period not only affects immediate outcomes but programs metabolic function and health trajectories throughout the child’s lifespan.
Practical Nutrition Strategies
Nurses play a crucial role in providing practical, evidence-based nutrition guidance to pregnant women.
Dietary Recommendations
- Emphasize dietary diversity
- Encourage 3 meals and 2-3 healthy snacks
- Focus on nutrient-dense whole foods
- Include protein with each meal
- Choose complex carbohydrates
- Include healthy fats
- Stay well hydrated (8-10 cups water daily)
Supplementation Guidance
- Prenatal vitamin with 400-600μg folic acid
- Iron supplementation as indicated
- Calcium supplementation when dietary intake is inadequate
- Consider vitamin D supplementation
- DHA supplementation (200-300mg daily)
- Avoid excessive vitamin A supplementation
- Discuss timing of supplements for optimal absorption
Common Challenges & Solutions
- Nausea: Small, frequent meals; cold foods
- Heartburn: Small meals; avoid lying down after eating
- Constipation: Fiber, water, physical activity
- Food aversions: Alternative nutrient sources
- Cravings: Healthy substitutions
- Limited budget: Cost-effective nutrient-dense foods
- Cultural considerations: Culturally appropriate recommendations
Mnemonic: “NUTRITION” Counseling Approach
- N – Needs assessment (individualize approach)
- U – Understand food preferences and culture
- T – Timing of meals and snacks
- R – Recommended supplements
- I – Intake of key nutrients
- T – Troubleshoot barriers
- I – Individualize advice
- O – Offer practical strategies
- N – Note progress and adjust as needed
Building Partnership Using RMC Protocol
Respectful Maternity Care (RMC) is a human rights approach to care that promotes dignity, respect, and empowerment during maternity care.
Understanding Respectful Maternity Care
Respectful Maternity Care is an approach to care that emphasizes the fundamental rights of women, newborns, and families, promoting equitable access to evidence-based care while recognizing unique needs and preferences.
Respectful maternity care (RMC) is a well-described, rational approach for improving person-centered and equitable intrapartum and postpartum care. RMC is now considered the fifth “R” in the Alliance for Innovation on Maternal Health (AIM) Maternal Safety Bundle, alongside Readiness, Recognition, Response, and Reporting.
The concept of RMC emerged from a recognition that disrespectful care, mistreatment, and abuse during childbirth contribute to poor maternal outcomes and deter women from seeking facility-based care. RMC seeks to transform care delivery to be more woman-centered, dignified, and culturally appropriate.
Key Components of RMC
The RMC protocol encompasses several interconnected components that collectively create a respectful care environment.
Fundamental Principles of RMC
- Person-centered care: Placing women’s needs, values, and preferences at the center of care
- Dignity and respect: Treating all women with dignity regardless of age, ethnicity, socioeconomic status, or other factors
- Privacy and confidentiality: Maintaining physical privacy and information confidentiality
- Informed consent: Ensuring women receive complete information and freely consent to procedures
- Continuous support: Allowing women to have the support person of their choice during labor and birth
- Effective communication: Clear, respectful communication between providers and women
- Non-discrimination: Equitable care free from discrimination
- Access to healthcare: Ensuring all women have access to timely, appropriate care
- Autonomy: Respecting women’s right to make decisions about their care
- Quality of physical environment: Ensuring clean, safe, and comfortable care facilities
Validated Measurement Tools for RMC
Several validated tools have been developed to measure aspects of respectful maternity care:
| Tool | Purpose |
|---|---|
| MADM (Mothers Autonomy in Decision Making) | Measures women’s autonomy and role in decision-making during maternity care |
| MOR (Mothers on Respect) Index | Assesses women’s experiences of respectful care during pregnancy and childbirth |
| MIST (Mistreatment Index) | Identifies instances of mistreatment or disrespectful care during childbirth |
| PCMC (Person-Centered Maternity Care) Scale | Evaluates person-centered care across multiple domains |
| RMC-Q (RMC Questionnaire) | Assesses respectful maternity care practices in facilities |
Mnemonic: “RESPECT” Framework for Maternity Care
- R – Recognize individual needs and preferences
- E – Ensure privacy and confidentiality
- S – Support informed decision-making
- P – Promote continuous support during labor
- E – Engage in effective, compassionate communication
- C – Create a supportive, non-discriminatory environment
- T – Treat every woman with dignity
Implementing RMC in Practice
Implementing respectful maternity care requires both systemic changes and individual provider commitment to woman-centered principles.
Institutional Strategies
- Develop clear RMC policies
- Conduct staff training on RMC
- Create physical environments that support privacy
- Establish mechanisms for feedback from women
- Implement transparent accountability systems
- Involve women in designing maternity services
- Ensure adequate staffing and resources
Provider Practices
- Use respectful, non-judgmental language
- Obtain informed consent for all procedures
- Respect cultural preferences when possible
- Provide continuous updates on progress
- Include women in all care decisions
- Address pain management proactively
- Practice shared decision-making
- Recognize and address implicit bias
Community Engagement
- Partner with community organizations
- Create maternity care advisory groups
- Conduct community education on rights in childbirth
- Establish doula and peer support programs
- Develop culturally appropriate resources
- Foster community-facility dialogue
- Engage community leaders as advocates
Steps for Building Partnership Using RMC
- Establish rapport: Create a welcoming environment and introduce yourself
- Assess needs and preferences: Ask open-ended questions about care preferences and expectations
- Provide information: Share complete, accurate information in understandable language
- Facilitate choice: Present options and support informed decision-making
- Respect decisions: Honor women’s choices even when they differ from provider preferences
- Support continuous communication: Check in regularly and update as situations change
- Include support network: Recognize the role of partners, family members, or doulas
- Reflect and improve: Seek feedback and continuously improve care practices
Addressing Challenges in RMC
Despite growing recognition of its importance, implementing respectful maternity care faces several challenges that must be addressed.
| Challenge | Impact | Solutions |
|---|---|---|
| Staff shortages and burnout | Reduced time for respectful care; compassion fatigue | Adequate staffing; provider wellbeing initiatives; work environment improvements |
| Hierarchical medical culture | Power imbalances; diminished patient autonomy | Interprofessional education; flattened hierarchy models; team-based care approaches |
| Implicit bias and discrimination | Disparities in care quality; adverse outcomes | Bias training; equity frameworks; diverse staffing; accountability measures |
| Limited resources and infrastructure | Overcrowding; lack of privacy; inadequate facilities | Creative use of existing space; privacy screens; advocacy for improved facilities |
| Time constraints | Rushed interactions; limited opportunities for shared decision-making | Efficient workflows; delegation of non-clinical tasks; prioritization of communication |
| Lack of metrics and accountability | Difficulty measuring and improving respectful care | Implementation of validated tools; regular assessment; transparency in reporting |
| Cultural and language barriers | Miscommunication; cultural insensitivity | Interpreter services; cultural competence training; diverse workforce |
Important Note:
Respectful maternity care is not a luxury but a fundamental human right. Research shows that RMC is associated with improved clinical outcomes, higher satisfaction, increased facility births, and reduced maternal mortality and morbidity. Special attention should be given to marginalized populations who face the greatest risk of disrespectful care, including racial/ethnic minorities, adolescents, unmarried women, those with low socioeconomic status, and women with disabilities.
Father Engagement in Maternity Care
Meaningful engagement of fathers during pregnancy, childbirth, and early parenthood contributes significantly to maternal wellbeing and positive family outcomes.
Importance of Father Engagement
Father engagement in maternity care represents a paradigm shift from seeing pregnancy and childbirth as exclusively women’s experiences to recognizing them as family experiences that shape family formation and dynamics.
Research shows that early father involvement is associated with improved cognitive and socio-emotional development in children. Conversely, absent fathers have been linked to poorer educational, behavioral, and developmental outcomes in children. This impact occurs through both direct effects on child behavior and indirect effects via partner relationship problems, reduced social support, and increased maternal stress.
Despite growing evidence of its importance, father engagement is often overlooked in maternity care settings, with services primarily designed for mothers and babies, inadvertently excluding fathers or treating them as secondary participants.
Benefits of Father Involvement
Evidence demonstrates multiple benefits when fathers are actively engaged during pregnancy, childbirth, and the postpartum period.
Benefits for Mothers
- Earlier initiation of prenatal care
- Increased attendance at antenatal visits
- Reduced maternal stress and anxiety
- Improved health behaviors during pregnancy
- Enhanced maternal satisfaction with birth experience
- Lower rates of postpartum depression
- Reduced physical symptoms postpartum
- Improved breastfeeding initiation and duration
- Better overall maternal health at 3 months postpartum
Benefits for Children
- Higher birth weights
- Reduced infant mortality
- Better cognitive development
- Enhanced socio-emotional skills
- Stronger father-child attachment
- Improved language development
- Lower risks of behavioral problems
- Higher academic achievement
- Positive impact on child health practices
Benefits for Fathers
- Stronger paternal identity development
- Increased confidence in parenting abilities
- Greater satisfaction with fatherhood role
- Enhanced relationship with partner
- Improved health behaviors
- Stronger commitment to family
- Increased paternal competence
- More positive work-family balance
- Psychological wellbeing and purpose
Key Research Findings on Father Engagement
- Most fathers report positive feelings about their partner’s pregnancy and want to be involved
- Almost all fathers attend pregnancy ultrasound examinations when permitted
- Greater paternal engagement is positively associated with first contact with health professionals before 12 weeks gestation
- Women with more engaged partners report more positive experiences during labor and birth
- In the postnatal period, most engaged fathers help with infant care, including diaper changing, bathing, and feeding
- Where paternal involvement is highest, women report significantly better overall health and fewer psychological symptoms postpartum
- Women with engaged partners are more likely to initiate breastfeeding and breastfeed for longer durations
- Taking paternity leave is strongly associated with improved maternal wellbeing at three months postpartum
Strategies for Promoting Father Engagement
Healthcare providers can implement specific strategies to increase father engagement throughout the perinatal period.
Prenatal Period Strategies
| Strategy | Implementation |
|---|---|
| Direct invitation | Explicitly invite and welcome fathers to prenatal appointments |
| Flexible scheduling | Offer evening or weekend appointments to accommodate work schedules |
| Father-inclusive language | Use language that acknowledges fathers as co-parents, not visitors |
| Educational materials for fathers | Provide resources specifically designed for fathers’ needs and questions |
| Father-focused classes | Offer prenatal classes that include father-specific content |
| Direct engagement | Address questions and information to fathers as well as mothers |
| Father-to-father peer support | Connect expectant fathers with experienced fathers for mentoring |
Labor, Delivery & Postpartum Strategies
| Strategy | Implementation |
|---|---|
| Labor support education | Teach fathers specific techniques to support mothers during labor |
| Active inclusion in decision-making | Include fathers in discussions about care options and decisions |
| Normalize father presence | Create an environment where fathers are expected participants |
| Early skin-to-skin opportunities | Facilitate father-infant skin-to-skin contact when mother is unable |
| Hands-on teaching | Directly teach infant care skills to fathers before discharge |
| Father-inclusive postpartum visits | Schedule follow-up visits when fathers can attend |
| Father mental health screening | Screen for paternal depression and anxiety postpartum |
Three Phases of Father Involvement in Pregnancy
Research identifies three distinct phases that fathers experience during pregnancy:
-
The Announcement Phase
Initial reaction to pregnancy news, characterized by a range of emotions from joy to shock or concern. This is a critical time for healthcare providers to establish connection with fathers.
-
The Moratorium Phase
A period when the pregnancy doesn’t feel “real” to many fathers, as they can’t directly experience physical changes. Ultrasound appointments are particularly important during this phase as they help fathers visualize and connect with their unborn child.
-
The Focusing Phase
Later in pregnancy when fathers begin actively preparing for their new role, attending classes, preparing the home, and developing more concrete ideas about fatherhood. This is an ideal time for education and skills development.
Mnemonic: “FATHERS” Engagement Approach
- F – Focus on both parents as clients
- A – Acknowledge father’s role and importance
- T – Teach skills directly to fathers
- H – Help fathers understand their unique contribution
- E – Encourage questions and participation
- R – Recognize different learning styles
- S – Schedule services to include fathers
Addressing Barriers to Father Involvement
Despite growing recognition of the importance of father involvement, multiple barriers can prevent their full engagement in maternity care.
| Barrier | Description | Solutions |
|---|---|---|
| Institutional barriers | Facility policies that limit father participation; physical spaces not accommodating fathers | Policy review and revision; environment modifications; father-friendly facilities |
| Provider attitudes | Healthcare providers who view fathers as peripheral or even disruptive | Staff training on father engagement; challenging stereotypes; highlighting benefits |
| Work-related constraints | Inflexible work schedules; limited or no paternity leave | Flexible appointment times; telehealth options; advocacy for paternity leave policies |
| Knowledge and confidence | Fathers’ lack of knowledge about pregnancy, birth, and infant care | Father-specific education; hands-on skills training; peer mentoring |
| Cultural expectations | Cultural norms that define pregnancy and childbirth as women’s domains | Culturally sensitive approaches; community engagement; role models |
| Maternal gatekeeping | Mothers who may consciously or unconsciously limit father involvement | Education about benefits of father involvement; facilitation of co-parenting |
| Complex family structures | Non-traditional partnerships; separated parents; blended families | Flexible definitions of family; inclusive policies; individualized approaches |
Important Note:
When encouraging father engagement, it’s essential to recognize domestic violence situations where father involvement may not be safe or appropriate. All maternity services should include domestic violence screening and have protocols for managing disclosure safely.
Conclusion
Maternal nutrition, respectful maternity care, and father engagement represent three interconnected pillars of comprehensive, family-centered maternity care. When implemented together, these evidence-based approaches can transform pregnancy, birth, and early parenting experiences while improving outcomes for mothers, infants, and families.
Optimal maternal nutrition supports maternal and fetal health, preventing complications and establishing the foundation for lifelong wellness. Respectful maternity care ensures that women receive dignified, person-centered care that respects their autonomy and preferences. Father engagement acknowledges the important role that fathers play and actively involves them as partners in maternity care and early parenting.
As nursing professionals, we have a unique opportunity to integrate these approaches into practice, advocating for systemic changes while implementing individual-level strategies that support families. By addressing maternal nutrition, implementing respectful care protocols, and actively engaging fathers, we can improve both clinical outcomes and the lived experience of maternity care for families.
Global Best Practices
Several global initiatives demonstrate successful integration of these three areas:
- Sweden’s Family-Centered Maternity Care Model: Emphasizes father involvement from pregnancy through postpartum, with generous parental leave policies for both parents and specialized father education programs.
- New Zealand’s Midwifery Model: Integrates RMC principles through continuity of care, cultural sensitivity (especially for Māori families), and nutritional support tailored to cultural food preferences.
- Canada’s Indigenous Doula Programs: Address nutritional needs through traditional foods, incorporate cultural birth practices, and include extended family in the birth process.
- Netherlands’ Kraamzorg System: Provides in-home postpartum care that supports maternal nutrition, breastfeeding, and father skill-building in the first week after birth.
- Rwanda’s Fathers’ Clubs: Community-based approach to engaging fathers in maternal nutrition, birth preparation, and postpartum support, with measurable improvements in antenatal care attendance and facility births.
References
- UNICEF. (2021). UNICEF Programming Guidance: Maternal Nutrition. Prevention of malnutrition in women before and during pregnancy and while breastfeeding. https://www.unicef.org/media/114561/file/Maternal%20Nutrition%20Programming%20Guidance.pdf
- Redshaw, M., & Henderson, J. (2013). Fathers’ engagement in pregnancy and childbirth: evidence from a national survey. BMC pregnancy and childbirth, 13(1), 1-15. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-13-70
- Agency for Healthcare Research and Quality. (2024). Respectful Maternity Care: Dissemination and Implementation of Perinatal Safety Culture to Improve Equitable Maternal Healthcare Delivery and Outcomes. https://effectivehealthcare.ahrq.gov/sites/default/files/product/pdf/respectful-maternity-care-protocol.pdf
- World Health Organization. (2016). WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization.
- Shakibazadeh, E., Namadian, M., Bohren, M. A., et al. (2018). Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG: An International Journal of Obstetrics & Gynaecology, 125(8), 932-942.
- Institute of Medicine. (2009). Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press.
- American College of Obstetricians and Gynecologists. (2021). Optimizing support for breastfeeding as part of obstetric practice. ACOG Committee Opinion No. 821. Obstetrics & Gynecology, 137, e54-65.
- Association of Women’s Health, Obstetric and Neonatal Nurses. (2022). Respectful Maternity Care Framework and Implementation Strategy. Journal of Obstetric, Gynecologic & Neonatal Nursing, 51(2), 167-176.
- Burgess, A., & Goldman, R. (2021). Fatherhood in the first 1,000 days: The impact of father involvement on child nutrition outcomes. London: Promundo Global.
- Kwambai, T. K., Dellicour, S., Desai, M., et al. (2013). Perspectives of men on antenatal and delivery care service utilisation in rural western Kenya: a qualitative study. BMC pregnancy and childbirth, 13(1), 1-10.
