Introduction
In today’s complex healthcare environment, nurses must develop essential leadership skills in conflict management, negotiation, and change implementation. These competencies are critical for delivering safe, high-quality patient care while fostering collaborative professional relationships and adapting to evolving healthcare needs.
This comprehensive guide provides nursing students and professionals with evidence-based strategies and practical tools for managing conflicts, negotiating effectively, and implementing successful change initiatives. By mastering these skills, nurses can enhance workplace satisfaction, improve patient outcomes, and contribute positively to organizational development.
The focus of this guide is on developing practical strategies that can be applied in various healthcare settings. Each section includes relevant theories, real-world applications, visual aids, and memory tools to enhance learning and retention.
1. Conflict Management in Nursing
1.1 Understanding Conflict
Conflict is an inevitable aspect of healthcare environments where diverse professionals collaborate under high-pressure conditions. In nursing, conflict refers to a disagreement or opposition between individuals or groups resulting from differences in values, goals, priorities, or approaches to patient care.
Key Elements of Conflict in Healthcare Settings:
- Perceived incompatible goals: Different priorities in patient care approach
- Resource scarcity: Competition for limited time, staff, equipment, or space
- Interdependence: Need for collaboration despite differences
- Emotional components: Stress, frustration, and other emotions that arise during disagreements
Effective conflict management is not about eliminating conflicts but addressing them constructively to harness their potential for positive change and growth. Understanding that conflict is normal allows nurses to approach disagreements as opportunities to improve communication, clarify roles, and enhance the quality of patient care.
1.2 Types of Conflict in Healthcare
| Conflict Type | Description | Examples in Nursing |
|---|---|---|
| Intrapersonal | Internal conflict within an individual, often involving ethical dilemmas or competing priorities | A nurse feeling torn between following a physician’s order and their own clinical judgment about what’s best for the patient |
| Interpersonal | Conflict between two or more individuals due to personality differences, communication issues, or competing goals | Disagreement between a nurse and physician about patient treatment plans or communication style differences between colleagues |
| Intragroup | Conflict within a team or unit due to role ambiguity, workload distribution, or decision-making processes | Nursing unit conflict over shift assignments, unit protocols, or care priorities |
| Intergroup | Conflict between different departments, units, or professional groups | Tension between the emergency department and inpatient units regarding patient transfers or disagreements between nursing and pharmacy about medication protocols |
| Task-related | Conflict about how work should be performed or distributed | Disagreement about the best way to implement a new bedside handoff procedure |
| Value-related | Conflict arising from differences in beliefs, values, or ethical principles | Differences in opinions about end-of-life care approaches or patient autonomy issues |
Recognizing the type of conflict is the first step in developing an appropriate strategy for resolution. Different conflict types may require different approaches and interventions.
1.3 Stages of Conflict
Conflicts typically progress through predictable stages. Understanding these stages helps nurses recognize conflict early and intervene before escalation occurs.
- Latent Stage: Conditions for conflict exist but are not recognized. Tension begins to build.
- Perceived Stage: Parties become aware of potential conflict, but it has not yet affected the relationship.
- Felt Stage: Emotional responses develop, such as anxiety, frustration, or anger.
- Manifest Stage: Conflict becomes visible through behaviors such as arguments, criticism, or avoidance.
- Aftermath Stage: Resolution occurs, or consequences of unresolved conflict persist.
Clinical Tip:
Early intervention at the latent or perceived stages is most effective. The longer a conflict persists, the more difficult resolution becomes. Developing a strategy for early identification of potential conflicts can prevent escalation and improve resolution outcomes.
1.4 Thomas-Kilmann Conflict Model
The Thomas-Kilmann Conflict Mode Instrument (TKI) identifies five conflict management styles based on two dimensions: assertiveness (concern for self) and cooperativeness (concern for others).

| Conflict Style | Characteristics | When to Use | When to Avoid |
|---|---|---|---|
| Competing (High assertiveness, Low cooperation) |
Pursuing one’s own concerns at the expense of others; power-oriented approach |
|
|
| Accommodating (Low assertiveness, High cooperation) |
Neglecting own concerns to satisfy others; self-sacrificing approach |
|
|
| Avoiding (Low assertiveness, Low cooperation) |
Sidestepping the conflict; not pursuing either party’s concerns |
|
|
| Compromising (Moderate assertiveness, Moderate cooperation) |
Finding an expedient, mutually acceptable solution that partially satisfies both parties |
|
|
| Collaborating (High assertiveness, High cooperation) |
Working to find a solution that fully satisfies all concerns; win-win approach |
|
|
Important Consideration:
There is no single “best” conflict management style. The most effective nurses develop flexibility in applying different styles based on the specific situation, relationship context, and goals. Developing a strategic approach to selecting the appropriate conflict style improves resolution outcomes.
1.5 Conflict Resolution Strategies
Beyond understanding conflict styles, nurses need practical conflict resolution strategies they can apply in clinical settings.
NURSE: A Mnemonic for Conflict Resolution Steps
N – Name the conflict: Clearly identify and acknowledge the specific issue causing tension
U – Understand perspectives: Listen actively to understand all viewpoints involved
R – Respect differences: Demonstrate respect for various opinions and approaches
S – Seek common ground: Identify shared goals and areas of potential agreement
E – Establish solutions: Work together to develop mutually beneficial resolutions
Additional Effective Conflict Resolution Strategies:
- Focus on the issue, not the person: Separate the problem from the people involved
- Use “I” statements: Express feelings without blaming or accusing (e.g., “I feel concerned when…” vs. “You always…”)
- Maintain emotional control: Recognize and manage your emotional responses during conflict
- Identify underlying interests: Look beyond stated positions to understand deeper needs and concerns
- Brainstorm multiple solutions: Generate several options before evaluating and selecting the best approach
- Establish follow-up processes: Create mechanisms to evaluate the effectiveness of solutions and adjust as needed
Implementation Tip:
Practice these strategies in low-stakes situations to build competence before applying them in more challenging conflicts. Regular practice develops conflict resolution as a core nursing skill rather than a reactive response.
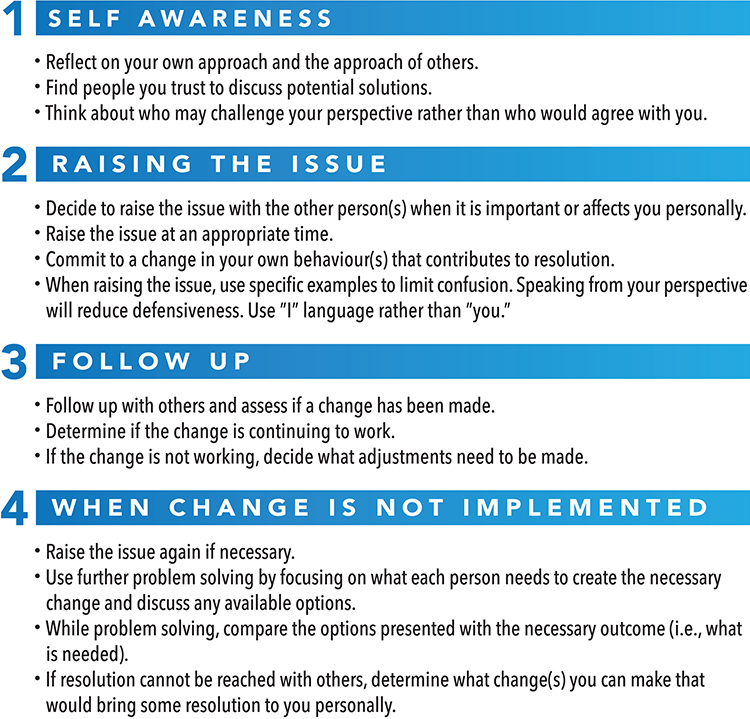
1.6 TALKS Mnemonic for Conflict Communication
The TALKS mnemonic provides a structured approach to communication during conflict situations, particularly when addressing concerns with colleagues or supervisors.
T – Time & place: Choose an appropriate, private setting for the discussion
A – Assertive communication: Express your concerns clearly and confidently while remaining respectful
L – Listen actively: Give full attention to the other person’s perspective without interrupting
K – Keep to the facts: Focus on specific behaviors and situations rather than generalizations or assumptions
S – Seek a solution: Work collaboratively to find a mutually acceptable resolution
Clinical Example:
Situation: A nurse notices a colleague consistently failing to complete documentation on time, creating workflow problems for the next shift.
Application of TALKS:
- Time & place: “Hi Sarah, do you have a few minutes to talk privately in the break room after handoff?”
- Assertive communication: “I’ve noticed that medication documentation hasn’t been completed before shift change over the past week. This makes it difficult for me to know what’s been administered.”
- Listen actively: “I’d like to understand what might be making timely documentation challenging for you.”
- Keep to the facts: “Yesterday and Monday, the 2 PM and 4 PM medications weren’t charted until after 8 PM according to the system timestamps.”
- Seek a solution: “How can we work together to ensure documentation is completed more promptly? Would it help if we adjusted the medication schedule or implemented a reminder system?”
Using the TALKS framework provides a strategic approach to addressing conflicts professionally while maintaining positive working relationships. This structured communication method helps prevent emotional escalation and focuses the conversation on resolution rather than blame.
2. Negotiation Strategies in Healthcare
2.1 Understanding Negotiation
Negotiation is a strategic dialogue aimed at reaching an agreement when parties have both shared and opposing interests. In healthcare, effective negotiation skills are essential for patient advocacy, interprofessional collaboration, and organizational improvement.
Unlike conflict management, which focuses on resolving disputes, negotiation proactively addresses needs and interests before conflicts arise or as part of the resolution process.
Key Elements of Effective Negotiation:
- Preparation: Gathering information and clarifying objectives before negotiation begins
- Active listening: Understanding others’ perspectives and underlying needs
- Problem-solving orientation: Focusing on mutual gain rather than winning/losing
- Relationship management: Maintaining positive professional relationships throughout the process
- Strategic thinking: Considering long-term implications of negotiated agreements
2.2 Types of Negotiations in Healthcare
| Negotiation Type | Description | Examples in Nursing |
|---|---|---|
| Patient Advocacy | Negotiating on behalf of patients to ensure their needs and preferences are addressed | Discussing treatment options with physicians, arranging accommodations for religious or cultural practices, securing additional resources for patient care |
| Interprofessional | Negotiating with other healthcare professionals to coordinate care and clarify roles | Determining patient care priorities with physicians, coordinating discharge planning with social workers, establishing care protocols with pharmacy |
| Organizational | Negotiating within the healthcare organization for resources, policies, or changes | Advocating for staffing adjustments, negotiating for professional development opportunities, proposing policy changes |
| Workload | Negotiating assignment distribution and responsibilities within a team | Arranging shift trades, balancing patient assignments, distributing unit responsibilities |
| Career | Negotiating terms of employment, advancement, or role development | Discussing salary and benefits, negotiating for flexible scheduling, establishing parameters for a new role |
Each type of negotiation may require different approaches and skills, though all benefit from thoughtful strategy and preparation.
2.3 Essential Negotiation Skills for Nurses
-
Preparation and Research
Gathering relevant information before negotiation begins establishes credibility and enables informed decision-making. This includes understanding policies, collecting data, and anticipating others’ positions.
-
Clear Communication
Articulating needs, concerns, and proposals clearly while avoiding medical jargon when negotiating with patients or non-clinical staff. This includes both verbal and written communication skills.
-
Active Listening
Demonstrating genuine interest in understanding others’ perspectives through attentive listening, clarifying questions, and acknowledging concerns.
-
Emotional Intelligence
Recognizing and managing emotions—both yours and others’—during negotiation processes. This includes maintaining composure during tense discussions and responding appropriately to others’ emotional cues.
-
Creative Problem-Solving
Developing innovative solutions that address multiple interests and overcome apparent deadlocks through divergent thinking.
-
Assertiveness
Advocating effectively for your position while maintaining respect for others. This balance is particularly important for nurses who often need to assert clinical judgments while collaborating with other professionals.
Development Tip:
Record yourself practicing a negotiation scenario with a colleague and review it together. This provides insights into your communication patterns and helps identify areas for improvement in your negotiation strategy.
2.4 ISBAR Communication Tool
The ISBAR (Identify, Situation, Background, Assessment, Recommendation) tool provides a structured format for clear, concise communication during clinical handovers and negotiations with other healthcare professionals.
I – Identify: Introduce yourself and the patient/situation you’re discussing
S – Situation: Briefly state the current situation or issue requiring attention
B – Background: Provide relevant contextual information about the situation
A – Assessment: Share your analysis of the situation, including concerns
R – Recommendation: State what you need or propose should happen
Application in Negotiation:
While ISBAR was developed for clinical handovers, it provides an excellent framework for structuring negotiations with other healthcare professionals because it:
- Organizes information logically and comprehensively
- Provides a professional framework that enhances credibility
- Ensures all relevant information is communicated
- Concludes with a clear action request or recommendation
Example: Using ISBAR in Negotiation
Scenario: A nurse needs to negotiate for additional staff support due to increasing patient acuity on the unit.
Application of ISBAR:
- Identify: “Hi Susan, I’m Jordan Chen, the charge nurse on 4-West today.”
- Situation: “We’ve had three patient admissions in the past hour, and two of our current patients have become unstable, requiring more intensive monitoring.”
- Background: “Our unit currently has eight patients requiring hourly assessments, and our nurse-to-patient ratio is now 1:6, which exceeds our standard safety guidelines of 1:4 for high-acuity patients.”
- Assessment: “I’m concerned about our ability to provide safe care with current staffing levels. The increased monitoring requirements and complex medication regimens create a high-risk situation.”
- Recommendation: “We need at least one additional RN for the next eight hours to restore appropriate ratios. If that’s not possible, I recommend transferring our two stable patients to the stepdown unit to reduce our load.”
Using the ISBAR framework in negotiations helps nurses communicate professionally and effectively while emphasizing patient safety and quality care as the central focus of the discussion. This structured approach strengthens the nurse’s negotiating position through clear, evidence-based communication.
2.5 Effective Negotiation Strategies
WIN Strategy for Healthcare Negotiations
W – What matters: Identify core interests and priorities
I – Investigate options: Explore multiple potential solutions
N – Navigate to agreement: Work collaboratively toward consensus
Key Negotiation Strategies for Nursing Practice:
-
Focus on Interests, Not Positions
Look beyond stated positions to understand underlying interests and needs. For example, instead of arguing about whether a patient should be transferred (positions), explore why each party believes their preferred approach is best (interests).
-
Use Objective Criteria
Base negotiations on standards independent of either party’s will, such as evidence-based practice guidelines, institutional policies, or patient outcomes data. This shifts the focus from personal preferences to objective quality measures.
-
Generate Multiple Options
Develop several possible solutions before selecting one, which expands the possibilities beyond win-lose scenarios. Brainstorming without immediate evaluation encourages creative problem-solving.
-
Build Relationships Before Negotiating
Invest in professional relationships proactively, not just when you need something. Strong collegial relationships create a foundation of trust that facilitates more productive negotiations.
-
Frame Around Patient Outcomes
Present requests and proposals in terms of benefits to patient care and safety. This creates common ground and emphasizes shared healthcare values.
-
Know Your BATNA
Determine your Best Alternative To a Negotiated Agreement—what you’ll do if negotiation fails. This establishes your “walk away” point and prevents accepting unfavorable terms.
Common Pitfalls to Avoid:
- Failing to prepare: Entering negotiations without clear objectives or sufficient information
- Emotional reactivity: Allowing frustration or anger to derail productive discussion
- Binary thinking: Viewing the situation as having only two possible outcomes
- Premature compromise: Settling quickly before exploring better alternatives
- Ignoring relationship impact: Focusing solely on immediate outcomes without considering long-term working relationships
Developing sophisticated negotiation strategies enables nurses to advocate effectively for patients, improve working conditions, and contribute to organizational improvement. These skills represent a critical dimension of nursing leadership in contemporary healthcare environments.
3. Implementing Planned Change
3.1 Understanding Planned Change
Planned change is a deliberate, structured process of moving from a current state to a desired future state. In nursing, planned change is essential for quality improvement, evidence-based practice implementation, and organizational development.
Key Characteristics of Effective Planned Change:
- Purposeful: Driven by clearly defined goals and expected outcomes
- Structured: Following a systematic process rather than random interventions
- Evidence-based: Grounded in research, best practices, and relevant theory
- Collaborative: Involving stakeholders throughout the process
- Iterative: Incorporating feedback and evaluation for continuous improvement
Successful implementation of planned change requires a strategic approach that addresses both the technical aspects of the change and the human factors that influence adoption and sustainability.
3.2 Lewin’s Change Theory
Kurt Lewin’s Three-Step Model of Change provides a foundational framework for understanding and implementing change in nursing practice. This model conceptualizes change as a dynamic process moving through three distinct stages.
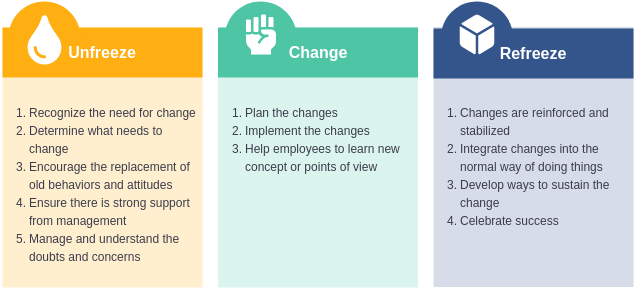
Stage 1: Unfreezing
The unfreezing stage involves creating readiness for change by disrupting the existing equilibrium and helping stakeholders recognize the need for change.
Key Unfreezing Strategies:
- Create dissatisfaction with the current state by highlighting problems or gaps
- Present compelling data that demonstrates the need for change
- Connect the change to core values and organizational mission
- Address fears and concerns openly and honestly
- Build a coalition of supporters who champion the change
Stage 2: Moving/Changing
The moving stage involves implementing the actual change through new processes, behaviors, or systems. This phase requires detailed planning, resource allocation, and ongoing support.
Key Moving Strategies:
- Provide clear direction about what is changing and why
- Offer comprehensive training in new skills or processes
- Create opportunities for involvement to increase ownership
- Address resistance constructively and empathetically
- Celebrate early successes to maintain momentum
- Communicate consistently throughout the process
Stage 3: Refreezing
The refreezing stage involves stabilizing and institutionalizing the change as the new norm. This ensures the change becomes embedded in the organizational culture and daily practice.
Key Refreezing Strategies:
- Reinforce the change through policies, procedures, and systems
- Recognize and reward adoption of new practices
- Provide ongoing support and resources
- Integrate the change into orientation and training for new staff
- Monitor compliance and address drift or regression
- Document the benefits achieved through the change
Application Tip:
Create a specific implementation plan for each stage of Lewin’s model, identifying key activities, responsible parties, and timeline. This structured approach enhances the likelihood of successful change implementation. Having clear strategies for each phase helps anticipate and address challenges proactively.
3.3 Kotter’s 8-Step Change Model
John Kotter’s 8-Step Change Model expands on Lewin’s framework by providing a more detailed roadmap for implementing organizational change. This model is particularly useful for complex changes that require significant cultural or behavioral adjustments.

Step 1: Create a Sense of Urgency
Help stakeholders recognize why change is necessary and why it must happen now, not later.
Nursing Example: Sharing patient safety incident data and benchmarking against other units or facilities to demonstrate the immediate need for a new medication administration protocol.
Step 2: Build a Guiding Coalition
Assemble a group with enough power, expertise, and credibility to lead the change effort.
Nursing Example: Forming a team that includes frontline nurses, nurse managers, pharmacists, physicians, and IT specialists to implement a barcode medication administration system.
Step 3: Form a Strategic Vision and Initiatives
Develop a clear vision of what the change aims to achieve and specific initiatives to realize that vision.
Nursing Example: Creating a vision statement like “Zero preventable medication errors through technology-enhanced verification processes” with supporting initiatives for each phase of implementation.
Step 4: Enlist a Volunteer Army
Communicate the vision broadly and enlist a large number of people who are committed to driving change.
Nursing Example: Training nurse champions on each shift who volunteer to support colleagues in adopting new practices and troubleshooting issues.
Step 5: Enable Action by Removing Barriers
Remove obstacles to change, modify systems that undermine the vision, and encourage risk-taking and innovation.
Nursing Example: Adjusting staffing patterns temporarily during implementation, streamlining documentation requirements, or providing additional technical support.
Step 6: Generate Short-Term Wins
Plan for and create visible improvements that can be celebrated to maintain momentum.
Nursing Example: Highlighting a 20% reduction in medication scanning errors after the first month and recognizing teams that achieve high compliance rates.
Step 7: Sustain Acceleration
Use increased credibility from early wins to change systems, structures, and policies that don’t align with the vision.
Nursing Example: Expanding the initiative to include additional medication safety components or extending the project to other units based on initial success.
Step 8: Institute Change
Anchor new approaches in the organizational culture by connecting them to organizational success.
Nursing Example: Incorporating barcode scanning compliance into unit performance metrics, new staff orientation, and annual competency validation.
Implementation Consideration:
While Kotter’s model presents steps sequentially, real-world implementation often involves overlapping phases and circular movement between steps. Flexibility in applying the model while maintaining its core principles is essential for successful change management. A strategy that adapts to emerging challenges while maintaining focus on the vision typically yields the best results.
3.4 Managing Resistance to Change
Resistance to change is a natural human response that must be anticipated and addressed constructively for successful implementation. Understanding the types and sources of resistance enables more effective change management strategies.
| Type of Resistance | Characteristics | Management Strategies |
|---|---|---|
| Rational Resistance | Based on logical disagreement with the change approach, timeline, or evidence base |
|
| Emotional Resistance | Based on feelings of fear, loss, or uncertainty about how the change will affect individuals personally |
|
| Political Resistance | Based on perceived threats to influence, status, or resource allocation |
|
| Practical Resistance | Based on genuine operational barriers or resource constraints |
|
SHIFT Mnemonic for Addressing Resistance:
S – Specify the resistance by identifying its exact nature
H – Hear concerns completely without interrupting
I – Investigate underlying causes beyond what’s initially expressed
F – Find common ground and shared goals
T – Target responses to address specific concerns
Viewing resistance as valuable feedback rather than opposition creates opportunities to improve change initiatives. Often, those resisting change have important insights about potential challenges or unintended consequences that can be addressed proactively.
3.5 The Nurse’s Role in Change Implementation
Nurses play multiple critical roles in the change implementation process, regardless of their formal position within the organization. Understanding these roles helps nurses maximize their impact on successful change initiatives.
Key Nursing Roles in Change Implementation:
-
Change Agent
Nurses often initiate and lead change efforts based on their direct observation of patient care needs and system inefficiencies. As change agents, nurses identify opportunities for improvement, build support for change, and guide implementation processes.
Example Activities: Identifying practice gaps, researching evidence-based alternatives, developing implementation proposals, securing leadership support.
-
Early Adopter
By embracing new practices early and demonstrating their effectiveness, nurses can model the change for peers and help overcome initial resistance. Early adopters provide practical feedback that improves implementation.
Example Activities: Volunteering for pilot testing, providing constructive feedback on processes, sharing positive experiences with colleagues.
-
Change Champion
Change champions actively promote the initiative among peers, provide informal leadership, and help colleagues navigate challenges during implementation. They translate the change vision into practical application.
Example Activities: Providing peer-to-peer support, troubleshooting issues, celebrating successes, maintaining enthusiasm during setbacks.
-
Expert Resource
Nurses with specialized knowledge related to the change serve as resources for others, providing guidance, education, and support throughout the implementation process.
Example Activities: Developing educational materials, conducting training sessions, answering questions, demonstrating techniques.
-
Data Collector/Evaluator
Nurses gather and analyze data to document baseline performance, monitor progress, and evaluate outcomes of change initiatives. This provides evidence to support continuation or modification of the change.
Example Activities: Conducting audits, tracking quality indicators, collecting feedback, analyzing trends, reporting results.
Essential Skills for Nurse Change Leaders:
- Systems thinking: Understanding how changes affect various components of care delivery
- Project management: Planning, organizing, and coordinating change activities
- Influence without authority: Persuading colleagues without formal power
- Adaptive leadership: Adjusting approaches based on emerging challenges
- Resilience: Persisting despite setbacks and maintaining positive focus
Nurses at all levels can contribute meaningfully to change implementation by understanding these roles and developing the associated skills. Effective nurse change leaders recognize that successful implementation requires both technical expertise and interpersonal strategies for engagement and influence.
3.6 Case Study: Implementing Change in Nursing Practice
Case Scenario: Implementing Bedside Shift Report
Background: A 30-bed medical-surgical unit decides to implement bedside shift reporting to improve patient satisfaction, reduce communication errors, and increase patient involvement in care planning. Currently, shift handoffs occur at the nurses’ station without patient involvement.
Application of Lewin’s Change Theory
| Stage | Activities | Challenges | Solutions |
|---|---|---|---|
| Unfreezing |
|
|
|
| Moving |
|
|
|
| Refreezing |
|
|
|
Outcomes and Lessons Learned
Outcomes:
- Patient satisfaction scores related to communication increased by 22%
- Medication errors decreased by 15% in the six months following implementation
- Nurse satisfaction with handoff quality improved by 35%
- After initial adjustment period, average handoff time decreased by 2 minutes compared to pre-implementation
Key Lessons:
- Early involvement of frontline staff in planning was crucial for acceptance
- Addressing practical concerns concretely (e.g., time management, privacy protocols) reduced resistance
- Phased implementation allowed for adaptation before full-scale rollout
- Continuous monitoring and feedback prevented drift back to previous practices
- Connecting the change to tangible patient and staff benefits maintained motivation
This case study demonstrates how applying change theory with thoughtful strategies for each phase can lead to successful implementation despite initial challenges. The systematic approach to planning, execution, and sustainment created lasting improvement in communication practices and patient outcomes.
4. Conclusion
Conflict management, negotiation, and change implementation are essential competencies for nursing practice in today’s complex healthcare environment. By developing expertise in these areas, nurses can enhance patient care, improve workplace relationships, and contribute meaningfully to organizational improvement.
Key takeaways from this comprehensive guide include:
- Conflict is inevitable but manageable: Understanding conflict types, stages, and resolution approaches enables nurses to transform potential disruptions into opportunities for improvement.
- Effective negotiation requires both skill and strategy: By mastering negotiation fundamentals and using structured communication tools like ISBAR, nurses can advocate successfully for patients, colleagues, and themselves.
- Change implementation follows predictable patterns: Applying established frameworks such as Lewin’s and Kotter’s models provides a roadmap for navigating the complex process of planned change.
- Resistance is valuable feedback: Rather than viewing resistance as an obstacle, skilled change leaders use it as a source of information to improve implementation approaches.
- Nurses have multiple roles in the change process: From initiating change to supporting implementation to evaluating outcomes, nurses contribute at every stage of organizational improvement.
The mnemonics and frameworks presented throughout this guide provide practical tools that nurses can apply immediately in their practice settings. By developing competence in conflict management, negotiation, and change implementation, nurses position themselves as effective leaders who can influence healthcare quality and work environment positively.
As healthcare continues to evolve, these leadership competencies will become increasingly valuable. Nurses who develop and apply these skills strategically will be well-equipped to navigate challenges, seize opportunities, and make meaningful contributions to healthcare improvement.
5. References
- American Nurses Association. (2023). Conflict resolution in nursing. https://www.nursingworld.org/content-hub/resources/nursing-leadership/conflict-resolution-in-nursing/
- British Journal of Nursing. (2019). Communicating effectively using the TALKS mnemonic. https://www.britishjournalofnursing.com/content/clinical/communicating-effectively-using-the-talks-mnemonic/
- Harvard Program on Negotiation. (2023). High stakes negotiations in the healthcare industry. https://www.pon.harvard.edu/daily/teaching-negotiation-daily/negotiate-the-healthcare-industry/
- Kilmann Diagnostics. (2024). Overview of the Thomas-Kilmann Conflict Mode Instrument (TKI). https://kilmanndiagnostics.com/overview-thomas-kilmann-conflict-mode-instrument-tki/
- Kotter, J. (2023). The 8-step process for leading change. https://www.kotterinc.com/methodology/8-steps/
- Lewin, K. (1951). Field theory in social science: Selected theoretical papers. Harper & Row.
- National Center for Biotechnology Information. (2023). Change management in health care. https://www.ncbi.nlm.nih.gov/books/NBK459380/
- National Center for Biotechnology Information. (2024). ISBAR: A handover nursing strategy in emergency departments. https://pmc.ncbi.nlm.nih.gov/articles/PMC10855820/
- Nursing Management Journal. (2023). Conflict management styles of nurse managers. https://journals.lww.com/jinm/fulltext/2023/05040/conflict_management_styles_of_nurse_managers_and.5.aspx
- OJIN: The Online Journal of Issues in Nursing. (2016). Integrating Lewin’s theory with Lean’s system approach for change. https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-21-2016/No2-May-2016/Integrating-Lewins-Theory-with-Leans-System-Approach.html
