Contracted Pelvis and Cephalopelvic Disproportion (CPD)
Comprehensive Nursing Notes for Obstetric Care
Table of Contents
1. Introduction
Contracted pelvis and cephalopelvic disproportion (CPD) remain significant challenges in obstetric practice, particularly in developing countries. These conditions can lead to obstructed labor, which is associated with increased maternal and perinatal morbidity and mortality. Understanding the pathophysiology, diagnosis, and management of contracted pelvis and CPD is essential for nursing professionals to provide optimal care for expectant mothers and their babies.
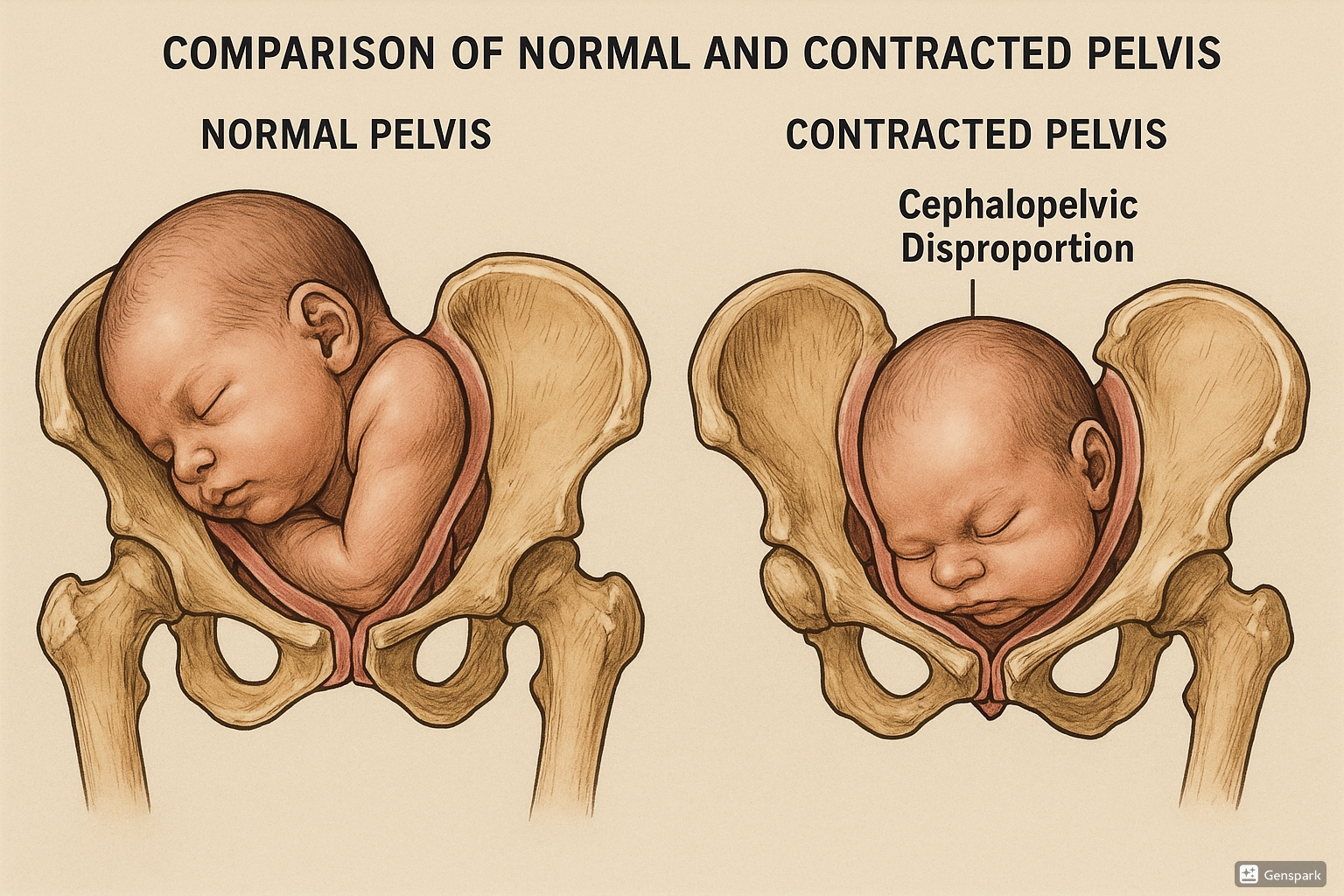
Figure 1: Comparison of normal pelvis and contracted pelvis showing cephalopelvic disproportion during childbirth
2. Definitions
Contracted Pelvis
A contracted pelvis is defined as a pelvis with reduced dimensions or altered shape that is sufficiently abnormal to cause difficulty in the delivery of a normal-sized fetus. It refers to a condition where one or more essential diameters of the pelvis are reduced below normal values, potentially interfering with the normal mechanism of labor.
Cephalopelvic Disproportion (CPD)
Cephalopelvic disproportion refers to the mismatch between the size of the fetal head and the maternal pelvis, making vaginal delivery difficult or impossible. CPD occurs when the baby’s head or body is too large to pass safely through the mother’s pelvis. It can result from either a large fetal head (absolute CPD) or abnormal fetal positioning (relative CPD).
Memory Aid – CPD: “Can’t Pass Down”
C = Cranium (baby’s head) too large
P = Pelvis too small or abnormally shaped
D = Disproportion between the two prevents descent
3. Anatomy of the Female Pelvis
Understanding normal pelvic anatomy is crucial for assessing pelvic abnormalities and potential CPD. The female pelvis comprises the sacrum, the coccyx, and two os coxae (each made up of the ischium, ilium, and pubis). Key anatomical landmarks and measurements include:
Key Pelvic Divisions
- False Pelvis: The upper portion above the pelvic brim
- True Pelvis: The lower portion below the pelvic brim
- Pelvic Inlet: The boundary between false and true pelvis
- Pelvic Cavity: The space within the true pelvis
- Pelvic Outlet: The lower boundary of the true pelvis
Critical Pelvic Diameters
- Anteroposterior Diameter (Conjugate): From pubic symphysis to sacral promontory
- Transverse Diameter: Maximum width of pelvic inlet
- Obstetric Conjugate: From sacral promontory to inner pubic symphysis (~10.5 cm normally)
- Diagonal Conjugate: From sacral promontory to lower edge of pubic symphysis (~12.5 cm)
- True Conjugate: From sacral promontory to upper edge of pubic symphysis (~11 cm)
Caldwell-Moloy Pelvic Classification
The female pelvis is typically classified into four basic types according to the Caldwell-Moloy classification:
| Pelvis Type | Characteristics | Frequency | Labor Implications |
|---|---|---|---|
| Gynecoid | Round to slightly oval inlet, well-curved sacrum, adequate dimensions in all planes | ~50% | Most favorable for vaginal delivery |
| Android | Heart-shaped inlet, narrow fore pelvis, flat sacrum, convergent sidewalls | ~20% | Poor for vaginal delivery; high risk for cephalopelvic disproportion |
| Anthropoid | Oval inlet with greater anteroposterior diameter, deep pelvis | ~25% | Acceptable for vaginal delivery |
| Platypelloid | Flat, wide inlet with shorter anteroposterior diameter | ~5% | Associated with transverse arrest and high risk for CPD |
Memory Aid – GAPS: Pelvic Types
G = Gynecoid: “Good” for delivery (round)
A = Android: “Alert” for problems (heart-shaped)
P = Platypelloid: “Problematic” for delivery (flat)
S = anthropoid (S for “Slightly” oval)
4. Types of Contracted Pelvis
Based on Location of Contraction
| Type | Description | Clinical Significance |
|---|---|---|
| Inlet Contraction | Reduced anteroposterior and/or transverse diameter of pelvic inlet | Prevents engagement of fetal head; early labor arrest |
| Mid-Cavity Contraction | Narrowed mid-pelvis with reduced interspinous diameter | Arrest of descent after initial engagement |
| Outlet Contraction | Reduced dimensions of pelvic outlet (intertuberous diameter <8 cm) | Difficulty in final stages of delivery; associated with perineal tears |
| Generally Contracted | All pelvic dimensions uniformly reduced | Highest risk for cephalopelvic disproportion |
Based on Pelvic Architecture and Size
- Small Gynecoid Pelvis (Generally Contracted Pelvis): All diameters uniformly reduced with maintained proportions
- Small Android Pelvis: Heart-shaped inlet with reduced transverse diameter
- Small Anthropoid Pelvis: Oval-shaped with reduced transverse diameter
- Small Platypelloid Pelvis (Simple Flat Pelvis): Reduced anteroposterior diameter with normal or increased transverse diameter
- Rachitic Flat Pelvis: Flattened pelvis due to rickets with reduced anteroposterior diameter
- Robert Pelvis: Extreme narrowing of transverse diameter
- Naegele Pelvis: Oblique distortion due to absence or fusion of one sacral ala
- Kyphotic Pelvis: Increased anteroposterior diameter of inlet with contracted outlet
- Scoliotic Pelvis: Asymmetric due to spinal curvature
- Split Pelvis: Separation of pubic symphysis
5. Causes
Causes of Contracted Pelvis
- Developmental Factors:
- Hereditary or congenital factors
- Racial variations in pelvic architecture
- Small maternal stature
- Nutritional Factors:
- Malnutrition during skeletal development
- Vitamin D deficiency
- Calcium deficiency during growth
- Metabolic Disorders:
- Rickets
- Osteomalacia
- Osteoporosis
- Trauma/Injury:
- Pelvic fractures
- Previous pelvic surgeries
- Radiation therapy to pelvis
- Spinal Deformities:
- Kyphosis
- Scoliosis
- Spondylolisthesis
- Lower Limb Abnormalities:
- Unilateral or bilateral hip dislocation
- Poliomyelitis with limb atrophy
- Lower limb inequalities
Causes of Cephalopelvic Disproportion
CPD results from a mismatch between fetal size and maternal pelvis. Causes include:
Fetal Factors
- Fetal macrosomia (>4000g)
- Post-term pregnancy
- Hydrocephaly
- Malpresentation (brow, face, or shoulder)
- Multiple pregnancy
- Congenital anomalies
Maternal Factors
- Contracted pelvis (any type)
- Maternal diabetes or gestational diabetes
- Excessive maternal weight gain
- Advanced maternal age
- Maternal short stature
- History of pelvic trauma
- Adolescent pregnancy (when pelvis is not fully developed)
- Previous difficult deliveries or cesarean sections
Memory Aid – FETAL CPD Causes:
F = Family history of large babies
E = Excessive maternal weight gain
T = Term exceeded (post-dates)
A = Abnormal presentation
L = Large for gestational age
6. Diagnosis and Assessment
Clinical Assessment
- History Taking:
- Previous difficult deliveries
- History of CPD or cesarean sections
- Previous birth weights
- History of pelvic trauma or metabolic disorders
- Family history of difficult deliveries
- Abdominal Examination:
- Assessment of fetal size (Leopold’s maneuvers)
- Evaluation of engagement
- Pendulous abdomen in primigravida (suggestive of CPD)
- Assessment of malpresentations
- Pelvimetry (Clinical):
- External pelvimetry – measuring external landmarks
- Internal pelvimetry – vaginal examination to assess pelvic dimensions
- Dynamic pelvimetry – evaluating pelvic capacity during labor
Radiological Assessment
- X-ray Pelvimetry: Traditional method, but limited due to radiation exposure
- CT Pelvimetry: Provides accurate measurements but involves radiation
- MRI Pelvimetry: Excellent soft tissue visualization without radiation; measures both bony pelvis and fetal size
- Ultrasound: Estimates fetal weight and head circumference; assesses fetal presentation and position
Diagnostic Indicators of Cephalopelvic Disproportion
- Failure to progress in labor despite adequate contractions
- Non-engagement of fetal head at term in primigravida
- Molding and caput formation without descent
- Abnormal labor curve (prolonged latent or active phase)
- Contracted pelvic measurements (obstetric conjugate <10 cm)
- Estimated fetal weight >4000g with maternal pelvic measurements suggesting inadequate capacity
Memory Aid – PROGRESS to Diagnose CPD:
P = Protracted labor despite good contractions
R = Reduced pelvic measurements
O = Obstetric history suggestive of past difficulties
G = Greater than normal fetal size
R = Relative disproportion assessment (trial of labor)
E = Engagement failure at term (primigravida)
S = Signs of obstructed labor
S = Significant molding without descent
7. Degrees of Pelvic Contraction
The severity of contracted pelvis is typically classified based on the measurement of the true conjugate (anteroposterior diameter of the pelvic inlet):
| Degree of Contraction | True Conjugate Measurement | Degree of Disproportion | Management Approach |
|---|---|---|---|
| Minor | 9-10 cm | Minor disproportion | Trial of labor; vaginal delivery usually possible |
| Moderate | 8-9 cm | Moderate disproportion | Trial of labor with close monitoring; cesarean if failed |
| Severe | 6-8 cm | Marked disproportion | Elective cesarean section usually indicated |
| Extreme | <6 cm | Absolute disproportion | Cesarean section mandatory |
Clinical Correlation with Fetal Weight
The significance of pelvic measurements must be correlated with estimated fetal weight:
| Obstetric Conjugate | Maximum Safe Fetal Weight | Risk of CPD |
|---|---|---|
| >11 cm | Any weight | Minimal |
| 10-11 cm | ~4000g | Low |
| 9-10 cm | ~3500g | Moderate |
| 8-9 cm | ~3000g | High |
| <8 cm | <2500g | Very high |
8. Clinical Features
Antepartum Signs
- Primigravida:
- Non-engagement of the presenting part at term
- Pendulous abdomen (fetus lies unusually anterior)
- Fundal height greater than gestational age
- Abnormal lie or presentation
- Multigravida:
- History of previous difficult deliveries
- Previous cesarean for CPD
- History of prolonged labor
- Prior instrumental deliveries
Physical Findings
- Short stature (often <150 cm)
- Skeletal deformities (kyphosis, scoliosis)
- Limb abnormalities (polio, rickets)
- Palpably contracted pelvis on examination
- Reduced pelvic measurements
Intrapartum Signs of Cephalopelvic Disproportion
- First Stage:
- Prolonged latent phase (>20 hours in primigravida)
- Slow cervical dilation (<1 cm/hour in active phase)
- Early rupture of membranes
- Poor descent despite good contractions
- Second Stage:
- Prolonged duration (>2 hours in primigravida)
- Arrest of descent
- Formation of large caput succedaneum
- Excessive molding of fetal head
- Maternal exhaustion
- Obstructed Labor Signs:
- Bandl’s ring formation (pathological retraction ring)
- Maternal tachycardia and dehydration
- Fetal distress
- Meconium-stained liquor
Memory Aid – MOLDING signs of CPD in labor:
M = Meconium staining as fetus becomes distressed
O = Obstructed progress despite good contractions
L = Large caput formation
D = Descent arrested
I = Increased molding
N = Non-engagement persists
G = Greater than normal length of labor
9. Complications
Maternal Complications
- Short-term:
- Obstructed labor
- Uterine rupture
- Postpartum hemorrhage
- Genital tract injuries (cervical/vaginal tears)
- Urinary tract injuries (fistula formation)
- Wound infections (after cesarean section)
- Sepsis
- Maternal exhaustion and dehydration
- Long-term:
- Vesicovaginal or rectovaginal fistula
- Pelvic floor dysfunction
- Urinary/fecal incontinence
- Secondary infertility
- Psychological trauma
- Increased risk in future pregnancies
Fetal/Neonatal Complications
- Immediate:
- Birth asphyxia
- Intracranial hemorrhage
- Cerebral palsy
- Brachial plexus injuries
- Fractures (skull, clavicle)
- Facial nerve palsy
- Cephalohematoma
- Fetal death
- Long-term:
- Developmental delays
- Neurological impairment
- Cognitive disabilities
- Physical disabilities
Warning Signs of Severe CPD:
- Bandl’s ring (pathological retraction ring)
- Severe molding with no descent
- Fetal bradycardia or late decelerations
- Maternal exhaustion with rising pulse
- Prolonged second stage (>3 hours with epidural)
10. Management Approaches
Antenatal Management
- Early Detection:
- Thorough evaluation of maternal pelvis during prenatal care
- Serial ultrasound estimation of fetal weight
- Identification of risk factors for CPD
- Early referral for specialized care if suspected
- Management of Risk Factors:
- Control of gestational diabetes to prevent macrosomia
- Appropriate weight gain counseling
- Monitoring fetal growth
- Delivery planning based on risk assessment
- Decision Making:
- Planned cesarean section for severe/extreme pelvic contraction
- Trial of labor for minor/moderate contraction
- Multidisciplinary approach involving obstetricians, midwives, and anesthesiologists
Intrapartum Management
Management Based on Degree of Contraction:
| Degree of Contraction | Management Approach | Considerations |
|---|---|---|
| Minor Degree (True conjugate 9-10 cm) |
Trial of labor with close monitoring | Good prognosis for vaginal delivery, especially with average-sized fetus |
| Moderate Degree (True conjugate 8-9 cm) |
Trial of labor if favorable factors; otherwise planned cesarean | Consider fetal weight, presentation, maternal parity, and pelvic architecture |
| Severe Degree (True conjugate 6-8 cm) |
Elective cesarean section generally indicated | Trial of labor only in very selected cases with very small fetus |
| Extreme Degree (True conjugate <6 cm) |
Mandatory cesarean section | Vaginal delivery not possible; high risk of maternal and fetal complications |
Trial of Labor Protocol:
- Continuous electronic fetal monitoring
- Regular assessment of labor progress (cervicograph)
- Adequate pain management
- Maintenance of hydration and nutrition
- Vigilance for signs of obstructed labor
- Readiness for emergency cesarean section
- Assessment of descent and rotation of the presenting part
Indications for Cesarean Section:
- Failure to progress despite adequate contractions
- Fetal distress during trial of labor
- Severe/extreme pelvic contraction
- Previous cesarean section with recurrent indication
- Malpresentation with cephalopelvic disproportion
Advanced Management Options
- Positional Interventions: Various maternal positions during labor can sometimes optimize pelvic dimensions and fetal descent
- Instrumental Delivery: In cases of minor disproportion with the head at +2 station or below
- External Cephalic Version: For breech presentations to reduce the risk of CPD
- Induction Considerations: Generally avoided with suspected CPD but may be considered in minor cases with favorable factors
Memory Aid – DECIDE Management of CPD:
D = Determine degree of disproportion
E = Evaluate fetal size and presentation
C = Consider maternal parity and history
I = Identify need for cesarean vs. trial of labor
D = Document progress carefully during labor
E = Emergency preparedness at all times
11. Nursing Care Plan for Contracted Pelvis and CPD
Nursing Assessment
- Maternal Assessment:
- Vital signs monitoring, especially during labor
- Abdominal examination to assess fetal position and engagement
- Evaluation of uterine contractions (frequency, duration, intensity)
- Assessment of maternal pain level and comfort
- Monitoring for signs of maternal distress or exhaustion
- Evaluation of bladder distension
- Fetal Assessment:
- Continuous electronic fetal monitoring
- Evaluation of fetal heart rate patterns
- Assessment of fetal descent using station reference
- Monitoring for signs of fetal distress
- Evaluation of amniotic fluid characteristics
- Labor Progress:
- Evaluation of cervical dilation and effacement
- Assessment of presentation and position
- Documentation of labor progress using partogram
- Monitoring for signs of failure to progress or obstructed labor
Nursing Diagnoses
| Nursing Diagnosis | Related Factors | Defining Characteristics |
|---|---|---|
| Risk for Ineffective Tissue Perfusion | Prolonged labor, uterine hyperstimulation | Maternal hypertension, tachycardia, decreased urine output |
| Risk for Ineffective Fetal Gas Exchange | Fetal compression, cord compression | Non-reassuring fetal heart patterns, meconium |
| Risk for Maternal Injury | Uterine rupture, instrumental delivery | Severe abdominal pain, vaginal bleeding |
| Acute Pain | Labor process, intervention procedures | Verbal reports, facial expressions, guarding |
| Anxiety | Uncertainty, fear of complications | Expressed concern, restlessness, increased questioning |
| Deficient Knowledge | Lack of exposure to information | Questions, misconceptions about cephalopelvic disproportion |
Nursing Interventions
Interventions During Labor:
- Positioning and Mobility:
- Assist with position changes to optimize pelvic dimensions
- Encourage upright positions when appropriate
- Support hands-and-knees position to facilitate rotation
- Implement side-lying positions to relieve pressure
- Pain Management:
- Provide non-pharmacological comfort measures
- Assist with epidural analgesia as ordered
- Implement breathing and relaxation techniques
- Apply heat therapy or massage as appropriate
- Monitoring and Assessment:
- Perform continuous electronic fetal monitoring
- Document labor progress regularly
- Monitor vital signs every 1-2 hours
- Assess bladder fullness and encourage voiding
- Evaluate signs of progress or complications
- Supportive Care:
- Provide emotional support and reassurance
- Offer clear explanations of procedures
- Support partner involvement in care
- Maintain a calm, supportive environment
- Preparation for Cesarean:
- Prepare patient for potential cesarean delivery
- Implement pre-operative protocols as needed
- Ensure informed consent is obtained
- Facilitate rapid preparation if emergency arises
Postpartum Interventions:
- Monitor for postpartum hemorrhage, especially after prolonged labor
- Assess for signs of genital tract trauma
- Monitor vital signs and uterine tone
- Provide pain management for cesarean or instrumental delivery
- Promote early bonding between mother and baby
- Support breastfeeding initiation
- Monitor for signs of infection
- Provide psychosocial support and education
Memory Aid – CARE for CPD:
C = Continuous monitoring (maternal and fetal)
A = Alert for warning signs
R = Ready for emergency intervention
E = Emotional support and education
12. Best Practices & Recent Updates
Recent Updates in CPD Management
- Dynamic Pelvimetry: New approaches to pelvimetry focus on evaluating the pelvis with the woman in different positions, recognizing that pelvic dimensions can change with movement. This can help identify cases where position changes may facilitate delivery despite apparent CPD.
- MRI Pelvimetry: Advanced imaging techniques using MRI provide more accurate assessment of both maternal pelvic dimensions and fetal size without radiation exposure, allowing for better prediction of CPD.
- Individualized Birth Plans: Moving away from strict cutoffs based solely on measurements toward more individualized management that considers multiple factors including maternal birthing history, pelvic architecture, fetal size and position.
Best Practices in Nursing Care
- Early Identification: Screening high-risk women during prenatal care can help identify potential CPD before labor begins.
- Informed Consent: Ensuring women understand the risks, benefits, and alternatives for management of suspected CPD.
- Positions in Labor: Utilizing evidence-based positioning during labor to optimize pelvic dimensions and fetal descent.
- Avoiding Iatrogenic Complications: Preventing unnecessary interventions that may complicate labor in cases of minor pelvic contraction.
- Interdisciplinary Collaboration: Working closely with obstetricians, midwives, anesthesiologists, and pediatricians for optimal outcomes.
Evidence-Based Recommendations
3 Key Practice Updates:
- Trial of Labor Assessment: Recent evidence supports allowing adequate time for labor progress before diagnosing failure to progress in suspected mild CPD cases. The latest guidelines suggest waiting for 6 hours of adequate contractions with no cervical change before diagnosing arrest of active phase.
- Physiotherapy Interventions: Growing evidence supports the use of specific physiotherapy interventions during pregnancy for women with minor pelvic contraction to optimize pelvic dimensions. Postural exercises and pelvic tilts may help prepare the pelvis for delivery.
- Prevention Strategies: New approaches to preventing cephalopelvic disproportion focus on better diabetic control during pregnancy, appropriate weight gain counseling, and timely induction at 39-40 weeks for suspected macrosomia to prevent excessive fetal growth.
Prevention of CPD in Future Pregnancies
- Preconception counseling for women with history of CPD
- Early pregnancy registration and regular antenatal care
- Control of gestational diabetes mellitus
- Appropriate weight gain monitoring
- Serial growth scans to detect macrosomia
- Planned delivery mode based on previous experience
- Adequate birth spacing to allow pelvic recovery
13. References
- Cleveland Clinic. (2022). Cephalopelvic Disproportion: What It Is & Treatment. https://my.clevelandclinic.org/health/diseases/24466-cephalopelvic-disproportion
- American Pregnancy Association. (n.d.). Cephalopelvic Disproportion (CPD). https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/cephalopelvic-disproportion/
- Physiopedia. (n.d.). Contracted Pelvis. https://www.physio-pedia.com/Contracted_Pelvis
- Made For Medical. (2024). Nursing Care Plan For Obstructed Labour. https://www.madeformedical.com/nursing-care-plan-for-obstructed-labour/
- TopLine MD. (2024). Everything You Should Know About Cephalopelvic Disproportion. https://www.toplinemd.com/myobgynspecialists/everything-you-should-know-about-cephalopelvic-disproportion/
- Salk, I., Cetin, M., Salk, S., & Cetin, A. (2016). Determining the incidence of gynecoid pelvis using three-dimensional computed tomography in nonpregnant multiparous women. Medical Principles and Practice, 25(1), 40-48.
- Siccardi, M., Valle, C., & Di Matteo, F. (2021). Dynamic external pelvimetry test in third trimester pregnant women: shifting positions affect pelvic biomechanics and create more room in obstetric diameters. Cureus, 13(3).
- Taffel, S. M., Placek, P. J., & Liss, T. (1987). Trends in the United States cesarean section rate and reasons for the 1980-85 rise. American Journal of Public Health, 77(8), 955-959.
- ACOG Practice Bulletin No. 205: Vaginal Birth After Cesarean Delivery. (2019). Obstetrics & Gynecology, 133(2), e110-e127.
- Pelvimetry for fetal cephalic presentations at or near term for deciding on mode of delivery. (2017). Cochrane Database of Systematic Reviews.
