Danger Signs During Pregnancy & Birth Preparedness
A Comprehensive Guide for Nursing Students
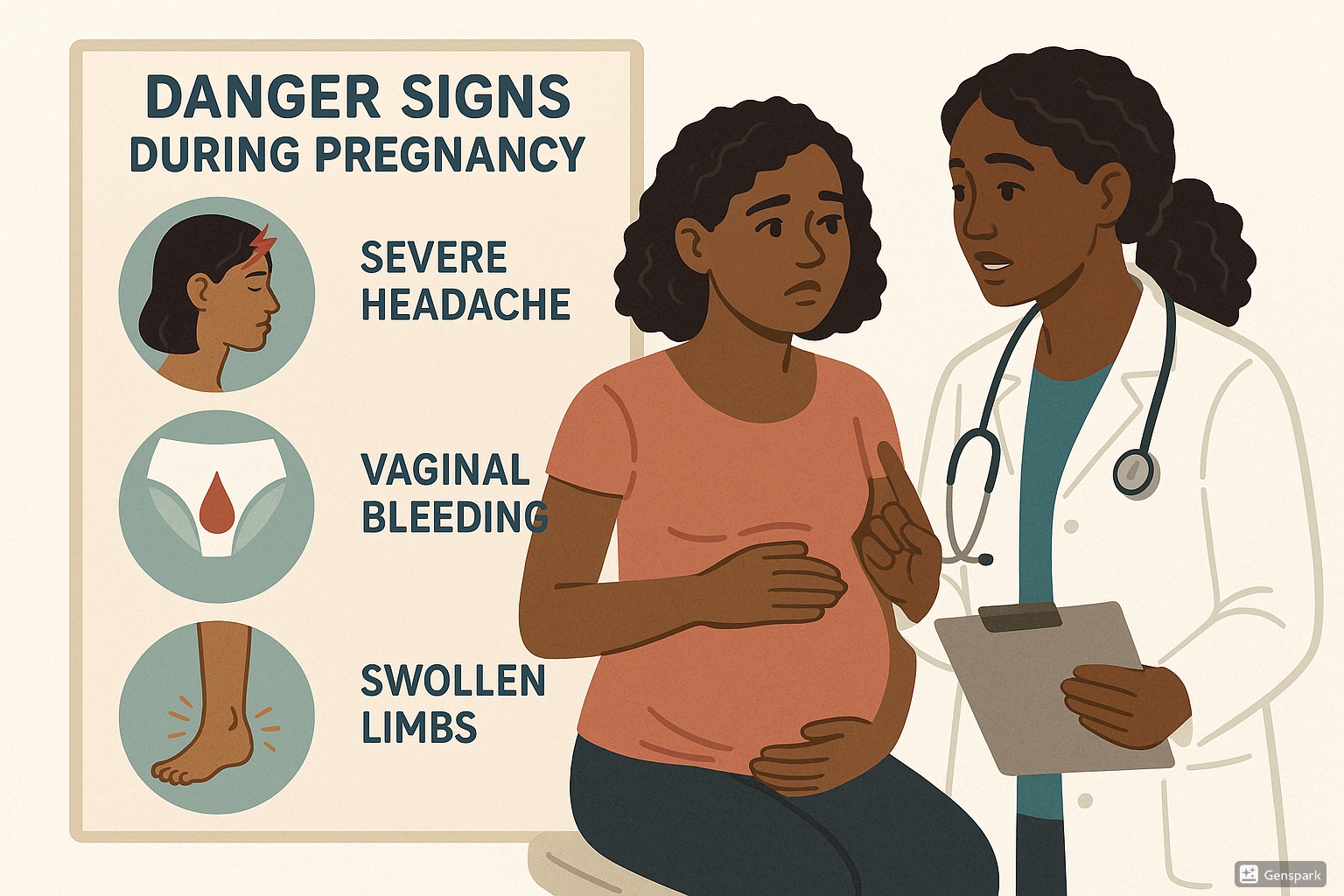
Medical illustration showing danger signs during pregnancy and patient education
Clinical Significance:
Recognizing danger signs during pregnancy is critical for preventing maternal and fetal morbidity and mortality. As nursing professionals, your ability to identify these signs early and facilitate appropriate interventions can be life-saving.
Table of Contents
1. Introduction
Pregnancy is a physiologically complex period requiring vigilant monitoring and care. While most pregnancies progress normally, approximately 15% of pregnant women develop complications that can lead to maternal or fetal morbidity and mortality. Understanding danger signs during pregnancy and ensuring birth preparedness are essential competencies for nursing professionals in maternal health.
Key Concept:
Danger signs during pregnancy are symptoms that indicate potential complications that threaten maternal or fetal health, requiring prompt assessment and management.
2. Danger Signs During Pregnancy
The following danger signs warrant immediate attention and should be assessed thoroughly by healthcare providers:
Vaginal Bleeding
Any vaginal bleeding during pregnancy requires evaluation. It may indicate placental problems, threatened abortion, or preterm labor depending on gestational age.
Assessment: Evaluate amount, color, presence of clots, and associated pain.
Severe Headache
Particularly when accompanied by visual disturbances, may indicate preeclampsia, especially in the latter half of pregnancy.
Assessment: Check blood pressure, evaluate for proteinuria, and assess for other signs of preeclampsia.
Edema of Face and Hands
While some edema is normal during pregnancy, sudden or severe swelling of face, hands, or legs may indicate preeclampsia.
Assessment: Evaluate for pitting edema and check blood pressure.
Decreased Fetal Movement
A significant reduction in felt fetal movements (less than 10 movements in 2 hours) may indicate fetal distress.
Assessment: Perform kick counts and consider fetal monitoring if indicated.
High Fever
Fever above 38°C (100.4°F) could indicate infection which may compromise maternal and fetal health.
Assessment: Check for other symptoms of infection and consider appropriate diagnostic tests.
Abdominal Pain
Severe or persistent abdominal pain may indicate placental abruption, preterm labor, or other complications.
Assessment: Evaluate location, intensity, and nature of pain along with associated symptoms.
3. Severe Danger Signs Requiring Immediate Action
The following danger signs during pregnancy require urgent medical intervention:
| Danger Sign | Possible Cause | Required Action |
|---|---|---|
| Convulsions/Seizures | Eclampsia | Immediate hospitalization, magnesium sulfate therapy, blood pressure control |
| Severe headache with visual disturbances | Severe preeclampsia | Urgent blood pressure assessment, proteinuria testing, maternal and fetal evaluation |
| Severe vaginal bleeding | Placental abruption, placenta previa | Emergency transport to hospital, IV access, fluid resuscitation if needed |
| Severe abdominal pain | Abruption, ruptured uterus, appendicitis | Immediate evaluation, possible emergency cesarean section |
| Rapid breathing or difficulty breathing | Pulmonary embolism, amniotic fluid embolism | Emergency oxygen therapy, transfer to critical care |
| High fever with rigors | Sepsis, chorioamnionitis | Blood cultures, broad-spectrum antibiotics, intensive monitoring |
4. Trimester-Specific Danger Signs
First Trimester (Weeks 1-12)
- Severe nausea and vomiting – Hyperemesis gravidarum may lead to dehydration and electrolyte imbalances
- Heavy bleeding with clots – May indicate miscarriage or ectopic pregnancy
- Severe one-sided abdominal/pelvic pain – Possible ectopic pregnancy
Second Trimester (Weeks 13-26)
- Sudden gush of fluid from vagina – Premature rupture of membranes
- Regular or frequent contractions – Threatened preterm labor
- Cervical insufficiency signs – Pressure sensation, spotting
Third Trimester (Weeks 27-40+)
- Decreased fetal movement – Possible fetal distress or placental insufficiency
- Sudden swelling of face, hands, and feet – Preeclampsia concern
- Persistent severe heartburn – May indicate HELLP syndrome when coupled with other signs
- Visual disturbances – Scotomata, flashing lights, or blurred vision may indicate severe preeclampsia
5. Birth Preparedness and Complication Readiness
Birth preparedness and complication readiness (BPCR) is a strategy to promote timely access to skilled maternal and neonatal care. It encourages pregnant women, their families, and communities to plan for normal births and possible complications.
Components of Birth Preparedness Plan
- Identify skilled birth attendant – Arrange for delivery with a qualified healthcare provider
- Identify birthplace location – Decide where the birth will take place
- Save funds for birth-related expenses – Prepare financial resources for normal delivery and possible complications
- Arrange transportation – Plan how to reach the birthplace when labor begins
- Identify blood donors – Identify compatible blood donors in case of emergency
- Identify support person – Arrange for someone to accompany the mother during labor and delivery
- Prepare essential items – Gather necessary supplies for mother and newborn
Nursing Role in Birth Preparedness
Nurses play a crucial role in facilitating birth preparedness by:
- Educating women about danger signs during pregnancy
- Helping create individualized birth plans
- Connecting women with community resources
- Facilitating communication between pregnant women and healthcare providers
- Ensuring regular antenatal assessments
6. Promoting Normalcy During Pregnancy
While vigilance for danger signs is essential, promoting normalcy during pregnancy is equally important for maternal wellbeing. Nurses should emphasize that pregnancy is a natural physiological process while ensuring appropriate monitoring.
Physical Wellbeing
- Encourage appropriate physical activity based on pre-pregnancy fitness level
- Provide guidance on normal nutritional needs during pregnancy
- Educate about normal physiological changes versus concerning symptoms
- Promote adequate rest and sleep hygiene
Psychosocial Support
- Address anxiety about childbirth through education and preparation
- Encourage participation in childbirth education classes
- Facilitate partner and family involvement in prenatal care
- Screen for perinatal mood disorders and provide resources
Balancing Vigilance and Normalcy
Nurses must skillfully balance vigilance for danger signs while promoting confidence in the natural process of pregnancy. This approach helps reduce unnecessary anxiety while ensuring proper monitoring for potential complications.
7. Best Practices and Recent Updates
Recent Evidence-Based Updates
1. Revised Blood Pressure Thresholds for Hypertensive Disorders
Recent guidelines from the American College of Obstetricians and Gynecologists (ACOG) have updated the diagnostic criteria for hypertensive disorders in pregnancy. Hypertension is now defined as systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg, with severe features defined as systolic BP ≥160 mmHg and/or diastolic BP ≥110 mmHg.
2. Cell-Free DNA Testing for Preeclampsia Risk
Emerging research supports the use of cell-free DNA testing as early as 10-13 weeks of gestation to identify women at high risk for developing preeclampsia. This allows for earlier preventive interventions such as low-dose aspirin therapy.
3. Telehealth Monitoring for High-Risk Pregnancies
Integration of remote monitoring technologies with traditional prenatal care allows for more frequent assessment of high-risk conditions without requiring in-person visits. Home blood pressure monitoring, electronic fetal movement counting applications, and virtual check-ins have shown promising results for early detection of pregnancy complications.
8. Assessment and Interventions
Nursing assessment for danger signs during pregnancy should be systematic and thorough. The following framework provides guidance for assessment and appropriate interventions:
| Assessment Parameter | Normal Finding | Concerning Finding | Nursing Intervention |
|---|---|---|---|
| Blood Pressure | <140/90 mmHg | ≥140/90 mmHg | Recheck in 15 minutes; if elevated, assess for other preeclampsia signs, notify provider |
| Urine Protein | Negative to trace | 1+ or greater | Assess for other preeclampsia signs, monitor BP, notify provider |
| Vaginal Bleeding | None | Any amount | Assess quantity, note color and presence of clots, check vital signs, notify provider immediately |
| Fetal Movement | ≥10 movements in 2 hours | <10 movements in 2 hours | Non-stress test, biophysical profile as ordered, consider emergency evaluation |
| Edema | Mild dependent edema | Facial edema, pitting edema of extremities | Check BP, assess for proteinuria, evaluate for other preeclampsia signs |
Documentation Requirements
Thorough documentation is essential when assessing danger signs. Include:
- Specific symptoms reported by the patient
- Onset, duration, and severity of symptoms
- Objective assessment findings
- Interventions implemented
- Patient response to interventions
- Healthcare provider notifications
- Follow-up plan
9. Resources and References
Clinical References
- American College of Obstetricians and Gynecologists. (2020). Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin No. 222. Obstetrics & Gynecology, 135(6), e237-e260.
- World Health Organization. (2023). WHO recommendations on antenatal care for a positive pregnancy experience.
- Association of Women’s Health, Obstetric and Neonatal Nurses. (2021). Guidelines for Professional Registered Nurse Staffing for Perinatal Units.
- Strategies Toward Ending Preventable Maternal Mortality (EPMM). (2021). World Health Organization.
- Johns Hopkins Evidence-Based Practice in Nursing & Healthcare. (2023). Birth Preparedness and Complication Readiness: A Global Survey.
Patient Education Resources
- American College of Nurse-Midwives: “Share With Women” patient education handouts
- Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN): Patient education materials
- March of Dimes: Pregnancy education resources
- Lamaze International: Birth preparation resources
- Centers for Disease Control and Prevention: Pregnancy complications information
Summary of Key Points
- Danger signs during pregnancy require prompt recognition and intervention by healthcare providers.
- Birth preparedness and complication readiness help ensure timely access to skilled care.
- Balancing vigilance for complications with promoting normalcy during pregnancy optimizes maternal wellbeing.
- Recent updates in practice include revised hypertension thresholds, advanced screening methods, and telehealth monitoring.
- Thorough assessment, documentation, and patient education are essential nursing responsibilities.
“Early recognition of danger signs during pregnancy saves lives. Nursing professionals are uniquely positioned to educate, assess, and intervene.”
