Child Morbidity & Mortality
Developmental Differences Affecting Response to Illness
Comprehensive notes on pediatric health metrics and how children differ from adults in their physiological, psychological, social, and immunological responses to illness.
Child Morbidity and Mortality Rates
Global Overview
Child mortality remains a significant global health concern despite substantial improvements in recent decades. According to the World Health Organization (WHO) and UNICEF:
- An estimated 4.8 million children died before reaching their fifth birthday in 2023
- This includes 2.3 million newborns who died within the first 28 days of life
- Global under-5 mortality has declined by 61%, from 94 deaths per 1,000 live births in 1990 to 37 in 2023
- Approximately 16,000 children under 15 die every day worldwide
Key Insight:
Most child deaths are preventable with existing interventions such as vaccination, proper nutrition, access to healthcare, clean water, and sanitation.
Child Mortality by Age Group
| Age Group | Terminology | Rate (2023) |
|---|---|---|
| First 24 hours | Immediate neonatal | Highest risk period |
| 0-28 days | Neonatal mortality | 18 per 1,000 live births |
| 29 days-1 year | Post-neonatal infant | 10 per 1,000 live births |
| 0-1 year | Infant mortality | 28 per 1,000 live births |
| 1-4 years | Child mortality | 9 per 1,000 live births |
| 0-5 years | Under-five mortality | 37 per 1,000 live births |
Leading Causes of Child Mortality
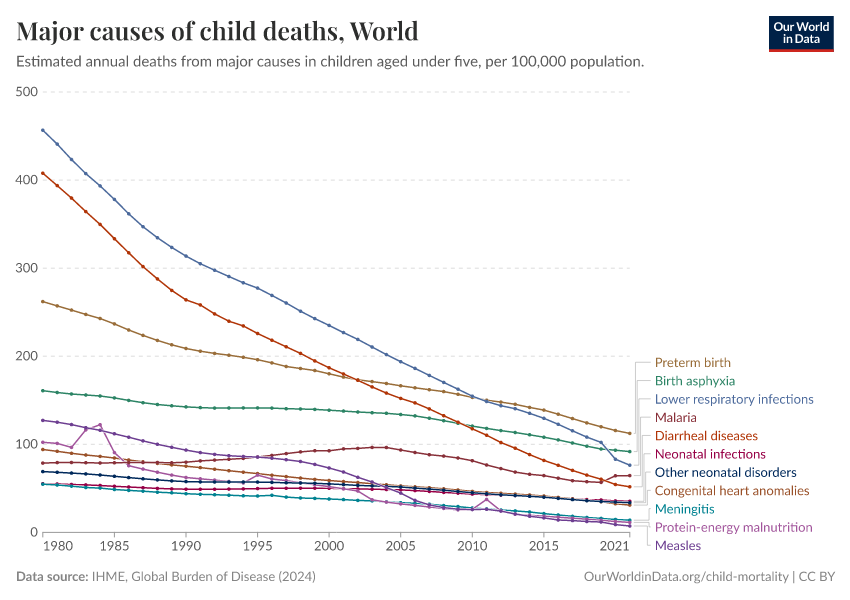
Source: Our World in Data
Neonatal Period (0-28 days)
- Preterm birth complications (35%)
- Intrapartum-related events (birth asphyxia)
- Neonatal infections (sepsis, meningitis, pneumonia)
- Congenital anomalies
- Low birth weight
Post-Neonatal (1-59 months)
- Pneumonia (19%)
- Diarrhea (18%)
- Malaria (8%)
- Measles
- Injuries (accidents, drowning)
- Malnutrition (underlying contributor to ~45% of deaths)
Regional Variations
Child mortality rates vary significantly by region:
- Highest: Sub-Saharan Africa and South Asia (>75% of global child deaths)
- Lowest: High-income countries (typically <5 deaths per 1,000 live births)
- Children in low-income countries are 14 times more likely to die before age five compared to children in high-income countries
Child Morbidity: Common Childhood Illnesses
Infectious Diseases
- Respiratory infections
- Gastroenteritis
- Otitis media
- Meningitis
- Urinary tract infections
- Childhood exanthems (measles, chickenpox)
Non-Infectious Conditions
- Asthma and allergies
- Obesity
- Type 1 diabetes
- Congenital disorders
- Developmental disabilities
- Mental health disorders
Injuries & Accidents
- Falls
- Burns
- Poisoning
- Drowning
- Road traffic accidents
- Sports injuries
Global Progress and Challenges
Progress Made
- Global under-5 mortality rate declined by 61% since 1990
- Expanded immunization programs
- Improved management of childhood illnesses (IMCI)
- Better maternal health services
- Improved nutrition and food security programs
- Enhanced water, sanitation, and hygiene (WASH)
Persistent Challenges
- Inequity in access to healthcare services
- Weak health systems in resource-limited settings
- Antimicrobial resistance
- Conflict and humanitarian crises
- Climate change impacts
- Pandemic disruptions to essential services
Physiological Differences

Source: ResearchGate
Key Principle:
Children are not simply “small adults.” Their anatomical and physiological differences significantly impact how they respond to illness, injury, and treatment.
Respiratory System Differences
| Feature | Children | Adults | Clinical Implication |
|---|---|---|---|
| Airway diameter | Smaller | Larger | Higher resistance to airflow; minor edema can cause significant obstruction |
| Tongue | Relatively larger | Proportional | More prone to airway obstruction |
| Larynx position | Higher (C3-C4) | Lower (C5-C6) | Different intubation technique required |
| Trachea | Shorter, narrower | Longer, wider | Easier right mainstem intubation |
| Cricoid ring | Narrowest part | Glottis is narrowest | Uncuffed ET tubes often used in young children |
| Chest wall | More cartilaginous | More ossified | More compliant; less protection for organs |
| Respiratory rate | Higher | Lower | Different normal ranges by age |
Clinical Implications
- Respiratory distress: Children develop respiratory distress more quickly due to:
- Higher metabolic rates and oxygen consumption
- Smaller functional residual capacity
- Less respiratory reserve
- Immature respiratory muscles that fatigue faster
- Infection susceptibility: Higher risk of severe presentations with respiratory infections like bronchiolitis, croup, and pneumonia
- Airway management: Different approach needed for pediatric airway management during emergencies
Remember!
In young children, respiratory arrest often precedes cardiac arrest, unlike in adults where the reverse is more common.
Cardiovascular System Differences
Structural Differences
- Heart positioned more horizontally in chest
- Thinner ventricular walls
- Less myocardial contractile mass
- Limited ability to increase stroke volume
- Higher resting heart rates
Functional Differences
- Cardiac output depends more on heart rate than stroke volume
- Faster circulation time
- Higher cardiac output per kg body weight
- More sensitive to volume changes
- Less vascular tone reserve
Clinical Implications
- Tachycardia is primary compensatory mechanism
- Bradycardia is an ominous sign of decompensation
- Hypotension is a late sign of shock
- Blood pressure increases with age
- Greater susceptibility to fluid overload
Normal Heart Rate Ranges by Age
| Age | Awake Rate (bpm) | Sleeping Rate (bpm) |
|---|---|---|
| Neonate (<28 days) | 100-205 | 90-160 |
| Infant (1-12 months) | 100-180 | 80-160 |
| Toddler (1-2 years) | 98-140 | 80-120 |
| Preschooler (3-5 years) | 80-120 | 65-100 |
| School-age (6-11 years) | 75-118 | 58-90 |
| Adolescent (12-15 years) | 60-100 | 50-90 |
| Adult | 60-100 | 40-60 |
Renal System Differences
Developmental Differences
- Newborns: Kidneys are anatomically and functionally immature
- Lower glomerular filtration rate (GFR)
- Reduced concentrating ability
- Impaired sodium conservation
- Less acidification capacity
- Maturation:
- GFR reaches adult levels by 1-2 years
- Tubular function matures more slowly
- Full concentrating ability by school age
Clinical Implications
- Fluid balance:
- Higher total body water percentage
- Higher water requirements per kg
- Greater susceptibility to dehydration
- More rapid development of electrolyte imbalances
- Medication handling:
- Reduced drug clearance in infants
- Dosage adjustments needed for renally excreted drugs
- Higher risk of drug toxicity
- Acid-base balance: Less capacity to compensate for acidosis
Normal Urine Output by Age
- Newborn: 1-3 ml/kg/hr
- Infant: 2 ml/kg/hr
- Child: 1-2 ml/kg/hr
- Adolescent/Adult: 0.5-1 ml/kg/hr
Neurological System Differences
Structural & Developmental
- Brain growth:
- Brain reaches 80% of adult size by age 2
- Continues developing through adolescence
- Higher metabolic demands in children
- Skull/fontanelles:
- Open fontanelles in infants (anterior closes by 18 months)
- Thinner skull provides less protection
- More flexible/elastic skull bones
- Myelination:
- Incomplete at birth
- Progresses in cephalocaudal pattern
- Continues through adolescence
Clinical Implications
- Increased vulnerability:
- Higher cerebral blood flow requirements
- Less tolerance to hypoxia and hypoglycemia
- Brain injury patterns differ from adults
- Intracranial pressure (ICP):
- Fontanelles allow for expansion in infants
- Bulging fontanelle indicates raised ICP
- Different signs of increased ICP by age
- Seizure threshold:
- Lower seizure threshold in children
- More susceptible to febrile seizures
- Different seizure presentations by age
Metabolic Differences
Energy Requirements
- Higher basal metabolic rate per kg body weight
- Greater caloric requirements per kg
- Faster metabolism of drugs and toxins
- Limited glycogen stores in young children
- More susceptible to hypoglycemia during illness
Thermoregulation
- Higher surface area to body mass ratio
- Greater heat loss potential
- Less developed temperature control mechanisms
- More susceptible to hypothermia
- More prone to rapid temperature elevation
Body Composition Differences
| Component | Children | Adults | Clinical Implication |
|---|---|---|---|
| Total body water | Higher percentage (70-80% in newborns) | Lower percentage (50-60%) | Greater fluid requirements; faster dehydration |
| Extracellular fluid | Higher percentage | Lower percentage | Different distribution of water-soluble drugs |
| Body fat | Lower percentage | Higher percentage | Different distribution of lipid-soluble drugs |
| Muscle mass | Lower percentage | Higher percentage | Different energy reserves |
Pharmacokinetic Differences
Absorption, Distribution & Metabolism
- Absorption:
- Variable gastric pH and emptying time
- Irregular intestinal motility
- Greater skin permeability in infants
- Distribution:
- Higher volume of distribution for water-soluble drugs
- Lower plasma protein levels in neonates
- Immature blood-brain barrier
- Metabolism:
- Immature hepatic enzyme systems at birth
- Phase I enzymes develop at different rates
- Faster metabolism in children vs. adults for some drugs
Excretion & Clinical Implications
- Excretion:
- Reduced glomerular filtration in neonates
- Immature tubular secretion and reabsorption
- GFR reaches adult values by 1-2 years
- Clinical considerations:
- Weight-based dosing required
- Different dosing intervals may be needed
- Different therapeutic ranges
- Greater susceptibility to adverse effects
- Certain medications contraindicated in children
Remember:
“Children are not small adults” applies especially to pharmacotherapy!
Psychological Differences

Source: Responsive Classroom
Cognitive Development & Illness Understanding
| Age Group | Cognitive Stage (Piaget) | Understanding of Illness | Clinical Considerations |
|---|---|---|---|
| Infants (0-1 year) |
Sensorimotor | No understanding of illness; responds to physical discomfort and separation anxiety |
|
| Toddlers (1-3 years) |
Preoperational (early) | Magical thinking; illness may be seen as punishment; limited understanding of cause and effect |
|
| Preschoolers (3-6 years) |
Preoperational | Illness understood as specific symptoms; believes in “contagion” but not logical causation; fear of bodily harm |
|
| School-age (6-12 years) |
Concrete operational | Understands simple physiological explanations; can relate cause and effect; concerned with bodily integrity |
|
| Adolescents (12-18 years) |
Formal operational | Can understand complex explanations; concerns about body image, independence, peer relationships |
|
| Adults | Formal operational | Full understanding of complex disease processes; able to weigh risks and benefits; concerns about roles and responsibilities |
|
Emotional Responses to Illness
Children
- Regression: May revert to earlier developmental behaviors
- Separation anxiety: Heightened fear of separation from caregivers
- Limited coping mechanisms: Fewer strategies to manage stress and anxiety
- Concrete expressions: May express distress through behavior rather than verbalization
- Fantasies and fears: May develop unrealistic fears about procedures or outcomes
- Bodily concerns: More immediate focus on pain and discomfort
- Time perception: Limited understanding of time, making waiting periods particularly difficult
Adults
- Rational processing: Better able to understand and rationalize the illness experience
- Complex concerns: Worry about broader implications (financial, occupational, family responsibilities)
- Established coping: More developed coping strategies and defense mechanisms
- Abstract thinking: Can contemplate long-term consequences and mortality
- Verbal expression: More likely to verbalize fears and concerns
- Control issues: May struggle with loss of control and independence
- Identity challenges: Illness may challenge established self-concept and roles
Communication Differences
Communication With Children
Developmental Considerations:
- Limited vocabulary and abstract thinking
- Shorter attention span
- Non-verbal communication more significant
- Difficulty expressing symptoms precisely
Effective Approaches:
- Use age-appropriate language
- Employ visual aids and demonstrations
- Include play and storytelling
- Speak at eye level
- Allow for questions and expression
- Involve parents in communication
Communication With Adults
Developmental Considerations:
- Full vocabulary and abstract reasoning
- Longer attention span
- Verbal communication predominant
- Ability to describe symptoms in detail
Effective Approaches:
- Provide detailed information
- Address both immediate and long-term concerns
- Use professional language with explanations
- Acknowledge expertise about their own body
- Discuss treatment options and preferences
- Respect privacy and autonomy
Psychological Response to Hospitalization
Children’s Response
Children may experience the following stages of adjustment to hospitalization:
- Protest: Crying, clinging to parents, rejecting hospital staff
- Despair: Withdrawal, decreased interaction, apathy
- Detachment/Adjustment: Gradual adaptation to hospital environment
Risk Factors for Psychological Distress:
- Young age (6 months to 4 years most vulnerable)
- Previous negative healthcare experiences
- Sudden, emergency admissions
- Limited preparation
- Separation from parents/caregivers
- Painful procedures
- Unclear explanations about illness or treatment
Interventions to Minimize Distress
For Children:
- Encourage parental rooming-in when possible
- Maintain familiar routines
- Allow comfort objects (blankets, toys)
- Use child life specialists for preparation and support
- Provide age-appropriate activities and distraction
- Minimize painful procedures and use pain management strategies
Differences from Adult Approach:
- Focus on family-centered care vs. patient-centered care
- Greater emphasis on maintaining development
- More attention to non-verbal cues
- Use of play therapy and expressive techniques
- Parent education and involvement in care
- Creation of child-friendly environment
Immunological Differences
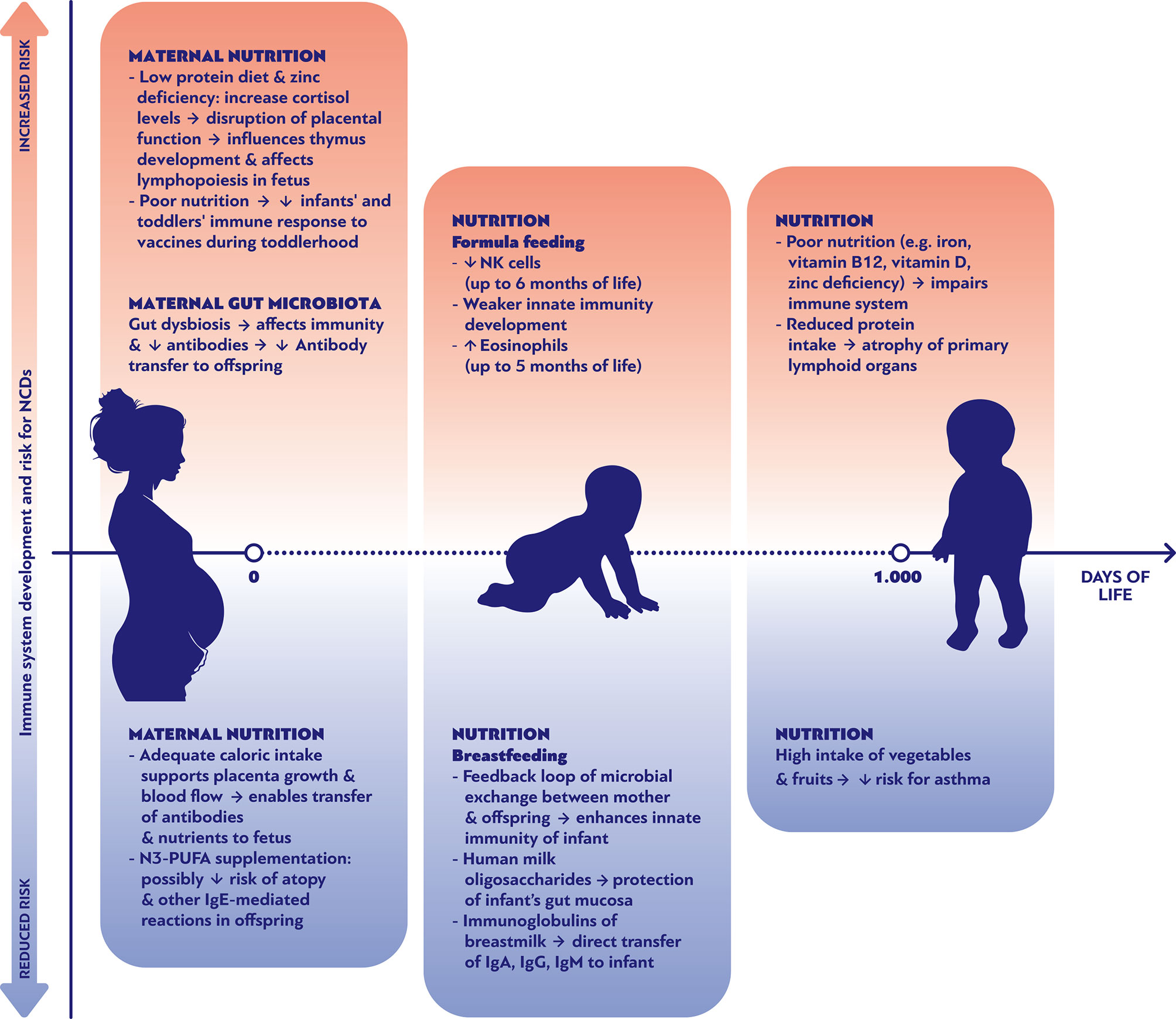
Source: Frontiers in Immunology
Key Concept:
The immune system undergoes significant development from birth through adolescence, with important differences from adult immunity that affect disease susceptibility, presentation, and treatment response.
Developmental Immunology
Immune System Maturation Timeline
| Age Period | Innate Immunity | Adaptive Immunity | Clinical Implications |
|---|---|---|---|
| Neonatal (Birth-28 days) |
|
|
|
| Infancy (1-12 months) |
|
|
|
| Early Childhood (1-5 years) |
|
|
|
| School Age (6-12 years) |
|
|
|
| Adolescence (12-18 years) |
|
|
|
| Adult |
|
|
|
Key Immunological Differences
Innate Immune System
Children vs Adults:
- Neutrophil function:
- Children: Reduced chemotaxis, phagocytosis, and pathogen killing in early years
- Adults: Fully functional neutrophil responses
- Natural Killer (NK) cells:
- Children: Lower cytotoxic activity in infancy and early childhood
- Adults: Optimal NK cell function against viruses and tumor cells
- Toll-like receptors (TLRs):
- Children: Altered TLR expression and response patterns
- Adults: More balanced TLR responses to pathogens
- Inflammatory response:
- Children: Often dampened in neonates, potentially excessive in older children
- Adults: More regulated inflammatory response
Adaptive Immune System
Children vs Adults:
- B cells and antibodies:
- Children: Limited antibody diversity and quantity, especially IgG2 subclass
- Adults: Full antibody repertoire with robust responses
- T cell responses:
- Children: Biased toward Th2 responses (allergy-prone), naive T cell predominance
- Adults: Balanced Th1/Th2 responses, more memory T cells
- Immune memory:
- Children: Developing memory, may require multiple exposures
- Adults: Established immunological memory from prior exposures
- Mucosal immunity:
- Children: Gradual maturation of mucosal defenses, lower IgA levels
- Adults: Well-established mucosal defenses
Clinical Manifestations of Immunological Differences
Infection Patterns
- Children:
- Higher frequency of infections
- Increased susceptibility to encapsulated bacteria
- More severe presentations of some viral infections
- Age-specific pathogens (RSV, rotavirus)
- Often first exposure to common pathogens
- Adults:
- Lower infection frequency
- Established immunity to common pathogens
- Reactivation of latent infections more common
- Occupational or lifestyle-related exposures
- Comorbidities influence infection risk
Inflammatory Responses
- Children:
- Neonates: limited inflammation
- Young children: rapid fever development
- Higher risk of febrile seizures
- Robust acute phase responses
- Kawasaki disease and MIS-C unique to children
- Adults:
- More modulated fever response
- Higher risk of cytokine storms in some infections
- Chronic inflammation more common
- Adult-onset inflammatory disorders
- Inflammatory response affected by comorbidities
Immune Dysregulation
- Children:
- Higher incidence of food allergies
- More common atopic conditions
- Early-onset autoimmunity has distinct patterns
- Primary immunodeficiencies typically present in childhood
- Th2-skewed responses promote allergies
- Adults:
- Different spectrum of autoimmune diseases
- Secondary immunodeficiencies more common
- Age-related immune senescence
- Higher risk of immune-related malignancies
- Occupational allergies more frequent
Therapeutic Considerations
Vaccination Differences
- Schedule timing:
- Children: Primary series timed to developing immune system, window of vulnerability
- Adults: Boosters and specific risk-based vaccines
- Immune responses:
- Children: May require multiple doses to establish immunity
- Adults: Generally more robust responses to single doses
- Adjuvant requirements:
- Children: May need different adjuvants for optimal response
- Adults: Standard adjuvants generally effective
Antimicrobial Treatment
- Pathogen coverage:
- Children: Different pathogen prevalence by age
- Adults: Different empiric coverage considerations
- Dosing considerations:
- Children: Weight-based dosing, developmental pharmacokinetics
- Adults: Standard dosing with organ function adjustments
- Adverse reactions:
- Children: Different adverse event profiles (e.g., antibiotic rashes more common)
- Adults: Age and comorbidity-related toxicity concerns
Immunomodulatory Therapies
- Children often require adjusted dosing beyond simple weight-based calculations
- Long-term immunosuppression has different risk profiles in developing vs. mature immune systems
- Growth and development must be considered with immunomodulatory treatments in children
- Different risk-benefit considerations for biologic therapies
- Immune reconstitution occurs differently in children vs. adults
Clinical Mnemonics
ABCD-P: Physiological Differences in Children
-
A
Airway
Smaller airway diameter, higher larynx, proportionally larger tongue, funnel-shaped airway
-
B
Breathing
Higher respiratory rate, greater oxygen consumption, less respiratory reserve, diaphragmatic breathing
-
C
Circulation
Higher heart rate, cardiac output dependent on rate not stroke volume, faster circulation time
-
D
Development/Drugs
Developing organ systems, different pharmacokinetics, weight-based dosing needed
-
P
Proportions
Larger head-to-body ratio, higher surface area to mass ratio, higher total body water percentage
SCALES: Major Causes of Child Mortality
-
S
Sepsis/Severe infection
Including neonatal sepsis, pneumonia, and bloodstream infections
-
C
Complications of prematurity
Leading cause of neonatal mortality worldwide
-
A
Asphyxia and birth trauma
Including intrapartum-related events and birth complications
-
L
Lung/Lower respiratory infections
Particularly pneumonia as a leading cause in under-5s
-
E
Enteric diseases
Diarrheal illnesses remain a major cause of child mortality
-
S
Severely malnourished
Underlying contributor to nearly half of all child deaths
CHILD vs ADULT: Psychological Response to Illness
-
C
Cognitive limitations
Children have developing cognitive abilities that affect illness understanding
-
H
Heightened fears
More concrete fears about pain, bodily harm, separation
-
I
Immediate focus
Present-oriented rather than future consequences
-
L
Limited coping strategies
Fewer developed psychological defense mechanisms
-
D
Dependent on others
Rely on caregivers for support and interpretation of experience
-
A
Abstract thinking
Adults can understand complex disease processes
-
D
Diverse concerns
Worry about roles, finances, and future implications
-
U
Understanding of mortality
Greater awareness of potential fatal outcomes
-
L
Long-term perspective
Consider future consequences and chronic implications
-
T
Tried coping mechanisms
Established defense mechanisms and coping strategies
IMMATURE: Pediatric Immune System Characteristics
-
I
Inefficient neutrophil function
Reduced chemotaxis and phagocytosis in early life
-
M
Maternal antibodies temporary
Initial protection gradually wanes over first year
-
M
Memory responses developing
Limited immunological memory, especially in infancy
-
A
Antibody production limited
Especially IgG2 subclass important for bacterial defenses
-
T
T-cell bias toward Th2
Predisposition to allergic responses rather than Th1
-
U
Underdeveloped mucosal immunity
Lower IgA levels at mucosal surfaces
-
R
Reduced NK cell activity
Diminished natural killer cell function early in life
-
E
Evolving progressively
Gradual maturation through childhood and adolescence
Mind Maps
Child vs Adult: Differences That Affect Illness Response
Physiological
- Smaller airway diameter
- Higher metabolic rate
- Greater body surface area ratio
- Higher water percentage
- Heart rate dependent cardiac output
- Immature renal function
- Less respiratory reserve
- Developing organ systems
- Different pharmacokinetics
- Vulnerable temperature regulation
Psychological
- Developing cognitive abilities
- Limited understanding of illness
- Concrete vs abstract thinking
- Magical thinking in young children
- Fear of separation from caregivers
- Fewer coping mechanisms
- Play as communication
- Different time perception
- Limited vocabulary for symptoms
- Regression during illness
Social
- Dependency on caregivers
- Family-centered identity
- Developmental focus vs. role focus
- School disruption impact
- Different healthcare delivery models
- Limited decision-making authority
- Peer relationship importance
- Special legal protections
- Parent interpretation of symptoms
- Family dynamics influence
Immunological
- Developing immune system
- Limited antibody diversity
- Reduced neutrophil function early
- Th2-biased responses
- Maternal antibody protection wanes
- Developing memory responses
- Different vaccine requirements
- Age-specific pathogens
- Different inflammatory patterns
- Unique pediatric immune disorders
Child Mortality: Major Causes & Interventions
Neonatal Causes
- Preterm birth complications
- Birth asphyxia
- Neonatal sepsis
- Congenital anomalies
- Low birth weight
Key Interventions
- Skilled birth attendance
- Prenatal care
- Neonatal resuscitation
- Kangaroo mother care
- Clean cord care
Infectious Diseases
- Pneumonia
- Diarrheal diseases
- Malaria
- HIV/AIDS
- Measles
Key Interventions
- Immunization
- Antibiotics for pneumonia
- ORS for diarrhea
- Insecticide-treated bed nets
- PMTCT for HIV
Other Causes
- Malnutrition (underlying)
- Injuries/Accidents
- Drowning
- Burns
- Poisoning
Key Interventions
- Nutritional supplementation
- Breastfeeding promotion
- Safety education
- Childproofing
- Supervision
Cross-Cutting Interventions
Healthcare Systems
- Universal health coverage
- Trained health workers
- Integrated services
Social Determinants
- Education for girls
- Poverty reduction
- Clean water & sanitation
Policy Level
- Child protection laws
- Maternal leave policies
- Food security programs
References
Child Mortality and Morbidity
- World Health Organization. (2024). Child mortality and causes of death. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/child-mortality-and-causes-of-death
- UNICEF. (2025). Under-five mortality – Child survival. https://data.unicef.org/topic/child-survival/under-five-mortality/
- Our World in Data. (2023). Child and Infant Mortality. https://ourworldindata.org/child-mortality
- WHO & Maternal and Child Epidemiology Estimation Group. (2023). Causes of child mortality, 2000-2019. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/child-mortality-causes-of-death

Social Differences
Role & Dependency Differences
Children’s Social Context
Adults’ Social Context
Impact of Illness on Social Functioning
Children
Adults
Social Determinants of Health
Social determinants of health affect both children and adults, but with important differences in how they manifest and impact health outcomes:
Healthcare System Interactions
Pediatric Healthcare Model
Adult Healthcare Model