Diabetes Mellitus: Community Health Nursing Perspectives
Comprehensive nursing notes on epidemiology, prevention, screening, diagnosis, management, referral, and follow-up
Table of Contents
Introduction to Diabetes
Diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels resulting from defects in insulin production, insulin action, or both. As community health nurses, understanding diabetes is essential for effective prevention, early detection, and management to reduce the burden of this condition in our communities.
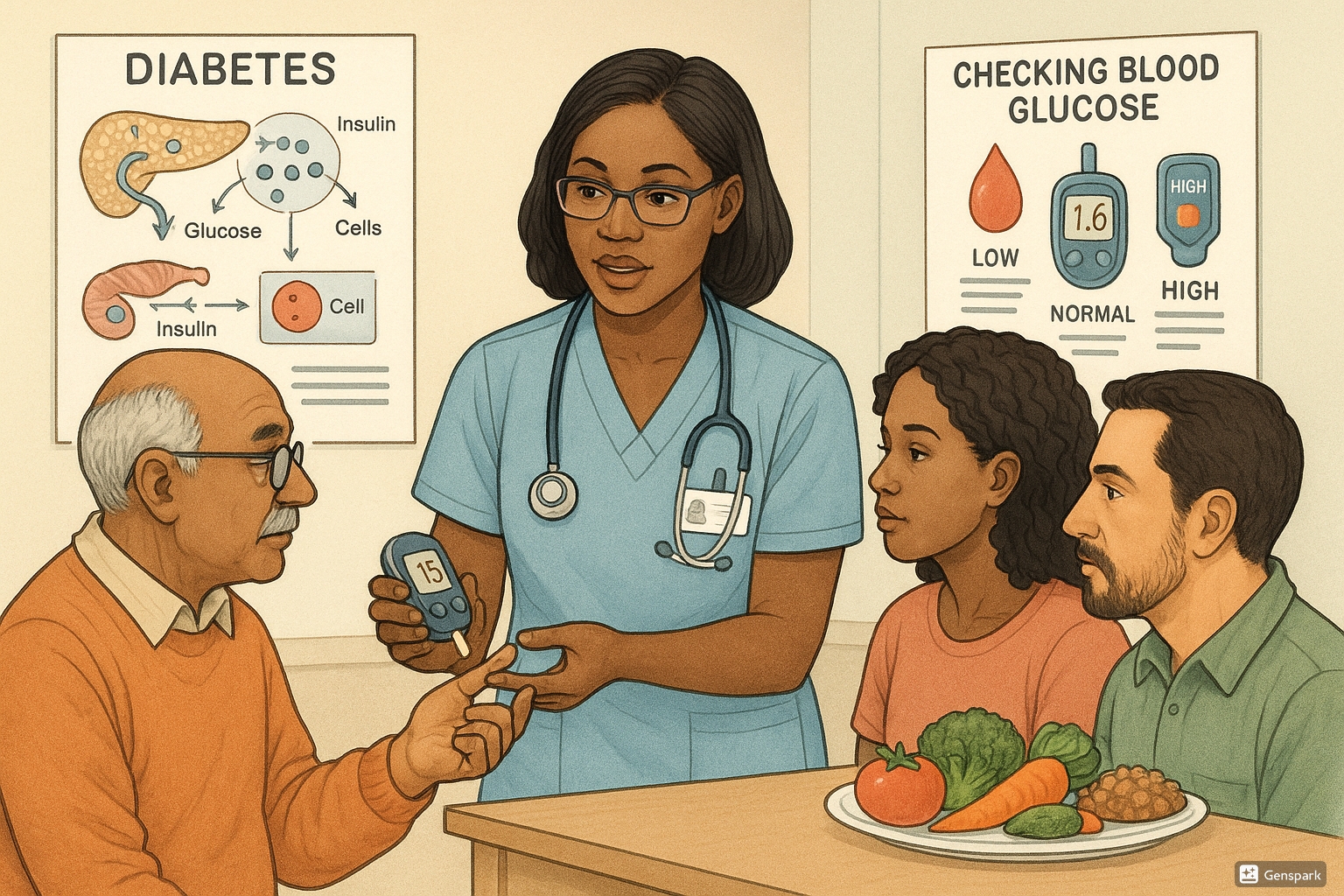
A community health nurse educating patients about diabetes management and blood glucose monitoring
Types of Diabetes
| Type | Key Characteristics | Primary Cause | Community Health Nursing Focus |
|---|---|---|---|
| Type 1 Diabetes | Autoimmune destruction of beta cells leading to absolute insulin deficiency | Autoimmune process, genetic factors | Early diagnosis, insulin management education, preventing complications |
| Type 2 Diabetes | Progressive insulin secretory defect and insulin resistance | Lifestyle factors, genetics, obesity | Prevention strategies, lifestyle modification, screening high-risk populations |
| Gestational Diabetes | Glucose intolerance first recognized during pregnancy | Pregnancy-related insulin resistance | Screening all pregnant women, education, postpartum follow-up |
| Other Specific Types | Diabetes due to genetic defects, diseases of exocrine pancreas, drug-induced | Various specific causes | Identifying specific causes, targeted interventions |
Epidemiology of Diabetes
The global prevalence of diabetes has risen dramatically, making it one of the most significant public health challenges of the 21st century. Community health nurses play a crucial role in understanding and addressing the epidemiological patterns of diabetes within their communities.
Global and Regional Burden
Global Statistics: According to the International Diabetes Federation, approximately 537 million adults (20-79 years) were living with diabetes in 2021. This number is projected to rise to 643 million by 2030 and 783 million by 2045.
Prevalence by Region: The highest age-adjusted comparative prevalence of diabetes is observed in the Middle East and North Africa (18.1%), followed by South East Asia (11.3%), and the Western Pacific (9.2%).
Diabetes Epidemiology in Different Populations
| Population Group | Prevalence Characteristics | Community Health Nursing Implications |
|---|---|---|
| Age Groups | Predominantly affects adults aged 40-59 years, but increasing among younger populations | Age-specific screening protocols, prevention education targeted to age groups |
| Socioeconomic Status | Higher burden in low- and middle-income countries and disadvantaged populations | Social determinants assessment, targeted interventions for underserved communities |
| Ethnic/Racial Groups | Higher prevalence among indigenous populations, African Americans, Hispanics, South Asians | Culturally competent care, ethnically tailored prevention strategies |
| Urban vs. Rural | Increasing rapidly in urban areas, but rural areas face barriers to care | Addressing urban lifestyle factors, improving rural access to care |
Epidemiological Transition in Diabetes
The epidemiological pattern of diabetes has undergone significant changes in recent decades:
- Shift from a disease of affluence to affecting all socioeconomic groups
- Increasing prevalence in low- and middle-income countries
- Rising incidence of Type 2 diabetes among children and adolescents
- Growing recognition of regional and population-specific genetic susceptibilities
Economic Burden
The economic impact of diabetes is substantial:
- Global healthcare expenditure on diabetes estimated at $966 billion (2021)
- Direct medical costs (hospitalizations, medications, supplies)
- Indirect costs (lost productivity, disability, premature mortality)
- Intangible costs (reduced quality of life, pain, psychological impacts)
Community Health Nursing Focus
Community health nurses should develop diabetes prevention and management strategies based on local epidemiological data. This includes identifying high-prevalence areas, targeting high-risk groups, and addressing social determinants of health that contribute to diabetes disparities.
Risk Factors for Diabetes
Understanding risk factors is essential for community health nurses to identify individuals at high risk for developing diabetes and implement timely preventive measures. Risk factors vary by diabetes type.
Modifiable vs. Non-modifiable Risk Factors
Non-modifiable Risk Factors
- Age: Risk increases with age, particularly after 45 years
- Family history: First-degree relatives with diabetes
- Ethnicity: Higher risk in specific ethnic groups
- Genetic predisposition: Multiple genetic markers identified
- History of gestational diabetes
- Polycystic ovary syndrome (PCOS)
Modifiable Risk Factors
- Overweight and obesity: Especially central/abdominal obesity
- Physical inactivity: Sedentary lifestyle
- Unhealthy diet: High in processed foods, sugars, saturated fats
- Smoking: Increases insulin resistance
- Hypertension: Blood pressure ≥140/90 mmHg
- Dyslipidemia: Low HDL cholesterol, high triglycerides
- Prediabetes: Impaired fasting glucose or impaired glucose tolerance
Specific Risk Assessment Tools
Community health nurses can use validated risk assessment tools to identify individuals at high risk for developing diabetes:
| Risk Assessment Tool | Key Components | Application in Community Health Nursing |
|---|---|---|
| Finnish Diabetes Risk Score (FINDRISC) | Age, BMI, waist circumference, physical activity, diet, hypertension, history of high blood glucose, family history | Simple non-invasive tool for community-based screening |
| American Diabetes Association Risk Test | Age, sex, history of hypertension, obesity, physical activity, family history | Quick assessment during community health fairs and outreach events |
| Indian Diabetes Risk Score (IDRS) | Age, abdominal obesity, family history, physical activity | Culturally appropriate for South Asian populations |
| QDiabetes | Comprehensive algorithm including multiple risk factors | Detailed risk stratification for targeted interventions |
- D Diet (unhealthy) and Dyslipidemia
- I Inactivity (physical) and Insulin resistance
- A Age (>45 years) and Abdominal obesity
- B Blood pressure (elevated)
- E Ethnicity (high-risk) and Environment
- T Tobacco use
- E Elevated glucose history (prediabetes, gestational diabetes)
- S Stress and Sleep disorders
Pathophysiology of Diabetes Mellitus
Understanding the pathophysiology of diabetes allows community health nurses to provide evidence-based education to individuals and communities and implement appropriate prevention and management strategies.
Type 1 Diabetes Pathophysiology
Autoimmune Process
Type 1 diabetes results from T-cell mediated autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency. The autoimmune process involves:
- Genetic susceptibility (HLA genes)
- Environmental triggers (viral infections, dietary factors)
- Production of autoantibodies (GAD65, IA-2, insulin autoantibodies)
- Progressive beta cell destruction (clinical symptoms appear when approximately 80-90% of beta cells are destroyed)
Type 2 Diabetes Pathophysiology
Multiple Defects
Type 2 diabetes is characterized by a combination of insulin resistance and progressive beta cell dysfunction:
- Insulin Resistance: Diminished tissue response to insulin in muscle, liver, and adipose tissue
- Beta Cell Dysfunction: Initial compensation with hyperinsulinemia, followed by progressive decline in insulin secretion
- Incretin Defect: Reduced GLP-1 effect and resistance to GIP
- Alpha Cell Dysfunction: Inappropriate glucagon secretion
- Renal Glucose Handling: Increased glucose reabsorption
- Brain Insulin Resistance: Altered central regulation of metabolism
Gestational Diabetes Pathophysiology
Gestational diabetes results from insulin resistance and relative insulin deficiency during pregnancy:
- Normal pregnancy is characterized by progressive insulin resistance starting in mid-pregnancy
- Placental hormones (human placental lactogen, progesterone, cortisol) contribute to insulin resistance
- Women who develop gestational diabetes have insufficient beta cell function to compensate for increased insulin demands
- Post-delivery, glucose metabolism typically returns to normal, but these women have increased risk for future type 2 diabetes
Pathophysiological Basis for Clinical Manifestations
| Clinical Manifestation | Underlying Pathophysiology |
|---|---|
| Polyuria (increased urination) | Hyperglycemia exceeds renal threshold, causing osmotic diuresis |
| Polydipsia (increased thirst) | Compensatory response to dehydration from osmotic diuresis |
| Polyphagia (increased hunger) | Cellular starvation despite hyperglycemia due to insulin deficiency/resistance |
| Weight loss (in type 1) | Catabolic state with breakdown of fat and protein for energy |
| Fatigue | Cellular inability to utilize glucose for energy |
| Recurrent infections | Impaired immune function, elevated glucose in tissues supporting microbial growth |
Clinical Manifestations of Diabetes
Community health nurses must recognize the various clinical manifestations of diabetes to facilitate early detection and prompt intervention. The presentation can vary greatly between diabetes types and individuals.
Classical Signs and Symptoms
- P Polyuria (increased urination)
- O Osmodiuresis (glucose in urine)
- L Loss of weight (especially Type 1)
- Y Yeast infections (recurrent)
- M Malaise and fatigue
- A Acanthosis nigricans (Type 2)
- T Thirst (polydipsia)
- I Increased hunger (polyphagia)
- C Cloudy vision (due to lens changes)
Presentation Differences by Diabetes Type
| Feature | Type 1 Diabetes | Type 2 Diabetes | Gestational Diabetes |
|---|---|---|---|
| Onset | Rapid (days to weeks) | Gradual (months to years) | During pregnancy (typically 24-28 weeks) |
| Typical symptoms | Classic symptoms, often severe | May be asymptomatic or mild symptoms | Usually asymptomatic |
| Body weight | Often normal or underweight with recent weight loss | Often overweight or obese | Variable |
| DKA risk | High | Lower, but possible (especially in stressful conditions) | Very low |
| Detection circumstance | Usually symptomatic presentation | Often discovered during routine screening | Detected through routine pregnancy screening |
Early vs. Late Manifestations
Early Manifestations
- Polyuria (frequent urination)
- Polydipsia (excessive thirst)
- Polyphagia (increased hunger)
- Unexplained weight loss (Type 1)
- Fatigue and weakness
- Blurred vision
- Recurrent infections (UTIs, skin, vaginal)
- Slow-healing wounds
Late/Chronic Manifestations
- Microvascular complications:
- Retinopathy (vision changes)
- Nephropathy (kidney damage)
- Neuropathy (nerve damage)
- Macrovascular complications:
- Coronary artery disease
- Peripheral vascular disease
- Cerebrovascular disease
- Foot problems (ulcers, infections)
- Skin changes
Clinical Presentation in Special Populations
Community health nurses should be aware of unique presentations in specific populations:
| Population | Unique Considerations |
|---|---|
| Children | May present with enuresis (bedwetting), irritability, poor school performance, growth issues |
| Elderly | Often asymptomatic or atypical presentation; may present with falls, confusion, urinary incontinence |
| Pregnant women | Usually asymptomatic; detected through screening; may have increased risk for UTIs, vaginal infections |
| Different ethnic groups | May develop complications at lower BMI thresholds or earlier in disease course |
Community Health Nursing Alert
Be vigilant for diabetes symptoms in individuals with risk factors, even when symptoms are subtle. Type 2 diabetes can remain undiagnosed for years, allowing complications to develop before detection. Community-based screening efforts should target high-risk populations.
Complications of Diabetes Mellitus
Diabetes complications significantly impact quality of life and increase healthcare costs. Community health nurses play a vital role in prevention, early detection, and management of these complications.
Acute Complications
| Complication | Description | Community Health Nursing Intervention |
|---|---|---|
| Diabetic Ketoacidosis (DKA) | Life-threatening condition characterized by hyperglycemia, ketosis, and metabolic acidosis; more common in Type 1 diabetes | Education on sick-day management, regular monitoring, recognition of early warning signs, prompt referral |
| Hyperosmolar Hyperglycemic State (HHS) | Extreme hyperglycemia without significant ketosis; more common in Type 2 diabetes; higher mortality than DKA | Prevention education for elderly and caregivers, ensuring adequate hydration during illness |
| Hypoglycemia | Blood glucose <70 mg/dL; symptoms include sweating, tremors, confusion; can be life-threatening | Education on recognition and treatment, ensuring patients carry glucose sources, involving family members in education |
Chronic Complications
Microvascular Complications
| Complication | Description | Screening and Early Detection | Community Health Nursing Role |
|---|---|---|---|
| Diabetic Retinopathy | Progressive damage to retinal blood vessels; leading cause of blindness in working-age adults | Annual comprehensive dilated eye examination | Ensure regular eye screening, education on importance of glycemic control, facilitating referrals |
| Diabetic Nephropathy | Kidney damage leading to proteinuria and potentially end-stage renal disease | Annual urine albumin-to-creatinine ratio and eGFR monitoring | Blood pressure monitoring, medication adherence support, education on renal protection |
| Diabetic Neuropathy | Nerve damage affecting sensory, motor, and autonomic nervous systems | Regular foot examinations, monofilament testing, autonomic function assessment | Foot care education, regular foot assessments, pain management strategies |
Macrovascular Complications
| Complication | Description | Prevention Focus |
|---|---|---|
| Cardiovascular Disease | Increased risk of coronary artery disease, myocardial infarction, heart failure | Comprehensive cardiovascular risk reduction: lipid management, blood pressure control, smoking cessation, aspirin therapy when indicated |
| Cerebrovascular Disease | Increased risk of stroke and transient ischemic attacks | Blood pressure management, antiplatelet therapy, carotid screening when indicated |
| Peripheral Arterial Disease | Atherosclerosis in peripheral arteries, leading to claudication, tissue loss | Regular pulse checks, ankle-brachial index screening, foot examinations |
Other Complications
- Diabetic Foot Problems: Combination of neuropathy and vascular insufficiency leading to ulcers, infections, and potential amputation
- Skin Conditions: Acanthosis nigricans, necrobiosis lipoidica, diabetic dermopathy
- Dental Problems: Increased risk of periodontal disease, tooth loss
- Psychological Impact: Depression, diabetes distress, anxiety
- Sexual Dysfunction: Erectile dysfunction in men, sexual arousal issues in women
- D Depression and Dental issues
- I Infections (recurrent)
- A Atherosclerosis and Arterial disease
- B Blood pressure problems (hypertension)
- E Eye disease (retinopathy)
- T Tactile sensation loss (neuropathy)
- E Erectile dysfunction
- S Stroke risk increased
- C Cardiovascular disease
- O Osteomyelitis (foot complications)
- S Skin conditions
- T Tissue damage (wounds, ulcers)
- S Sodium/fluid imbalance (nephropathy)
Prevention & Control Measures for Diabetes
Prevention is a cornerstone of diabetes management in community health nursing. Evidence-based prevention strategies can significantly reduce diabetes incidence and delay onset in high-risk individuals.
Levels of Prevention
Primary Prevention
Goal: Prevent diabetes onset
- Community-wide healthy lifestyle promotion
- School-based health education programs
- Workplace wellness initiatives
- Targeted interventions for high-risk groups
- Policy advocacy for environmental changes
Secondary Prevention
Goal: Early detection and intervention
- Screening programs for high-risk populations
- Prediabetes identification and management
- Early diagnosis through community screening events
- Prompt initiation of treatment
- Prevention of early complications
Tertiary Prevention
Goal: Prevent complications
- Optimal diabetes management
- Regular screening for complications
- Self-management education
- Rehabilitation services
- Support groups and mental health services
Evidence-Based Prevention Strategies
| Prevention Strategy | Target Population | Evidence Base | Community Health Nursing Application |
|---|---|---|---|
| Lifestyle Modification Programs | Individuals with prediabetes or high risk for Type 2 diabetes | Diabetes Prevention Program (DPP) showed 58% reduction in diabetes incidence with lifestyle intervention | Facilitate community-based DPP programs, group education sessions, health coaching |
| Weight Management | Overweight/obese individuals | 5-7% weight loss significantly reduces diabetes risk | Community weight management programs, nutrition counseling, physical activity initiatives |
| Physical Activity Promotion | General population, sedentary individuals | 150 minutes/week of moderate activity reduces diabetes risk by 30-50% | Walking groups, exercise classes, environmental advocacy for walkable communities |
| Dietary Interventions | General population, high-risk groups | Mediterranean, DASH, and plant-based diets associated with reduced diabetes risk | Cooking demonstrations, grocery store tours, community gardens, nutrition education |
| Pharmacological Prevention | High-risk individuals with specific indications | Metformin reduces diabetes risk by 31% (most effective in younger, more obese individuals) | Medication management education, adherence support, coordination with primary care |
Community-Based Prevention Programs
Effective diabetes prevention requires coordinated community-based approaches:
- Community Needs Assessment: Identify local diabetes prevalence, risk factors, and resources
- Coalition Building: Partner with stakeholders (healthcare providers, schools, employers, faith-based organizations)
- Public Awareness Campaigns: Increase knowledge about diabetes risk and prevention strategies
- Environmental Interventions: Advocate for policy changes to create healthier food environments and activity-friendly communities
- Culturally Tailored Programs: Develop prevention programs that address specific cultural, linguistic, and social needs
- Evaluation: Measure program outcomes and adjust strategies based on results
Community Health Nursing Focus: “PRIME” Prevention Strategy
- Population screening to identify high-risk individuals
- Risk factor modification through targeted interventions
- Integration of prevention services into primary care
- Multilevel approaches (individual, family, community, policy)
- Evaluation and continuous improvement of prevention programs
Screening Methods for Diabetes
Effective screening is essential for early detection of diabetes, allowing for timely intervention and improved outcomes. Community health nurses play a pivotal role in implementing and promoting screening programs.
Who Should Be Screened?
General Screening Recommendations
- Adults of any age who are overweight/obese (BMI ≥25 kg/m² or ≥23 kg/m² in Asian Americans) and have one or more additional risk factors:
- First-degree relative with diabetes
- High-risk race/ethnicity (African American, Latino, Native American, Asian American, Pacific Islander)
- History of cardiovascular disease
- Hypertension (≥140/90 mmHg or on therapy)
- HDL cholesterol <35 mg/dL and/or triglycerides >250 mg/dL
- Physical inactivity
- Women with polycystic ovary syndrome
- A1C ≥5.7%, impaired glucose tolerance, or impaired fasting glucose on previous testing
- All adults starting at age 45 years, regardless of weight
- Women with history of gestational diabetes, screen every 1-3 years throughout their lifetimes
- For all individuals, testing should be repeated at minimum of 3-year intervals
Screening Tests for Diabetes
| Screening Test | Methodology | Diagnostic Criteria | Advantages | Limitations |
|---|---|---|---|---|
| Fasting Plasma Glucose (FPG) | Blood glucose measurement after at least 8 hours of fasting | Normal: <100 mg/dL Prediabetes: 100-125 mg/dL Diabetes: ≥126 mg/dL |
Relatively inexpensive, widely available, standardized test | Requires fasting, single point measurement, day-to-day variability |
| Oral Glucose Tolerance Test (OGTT) | Blood glucose measurement 2 hours after consuming 75g glucose load | Normal: <140 mg/dL Prediabetes: 140-199 mg/dL Diabetes: ≥200 mg/dL |
More sensitive than FPG, detects more cases | Time-consuming (2+ hours), more expensive, less convenient, requires preparation |
| Hemoglobin A1C | Measures average blood glucose over prior 2-3 months | Normal: <5.7% Prediabetes: 5.7-6.4% Diabetes: ≥6.5% |
No fasting required, less day-to-day variability, standardized measurement | More expensive, less available in some settings, affected by hemoglobinopathies and anemia |
| Random Plasma Glucose | Blood glucose measured regardless of when last meal was consumed | Diabetes: ≥200 mg/dL with classic symptoms | Convenient, no preparation needed | Less sensitive, must be confirmed with FPG or A1C |
Community-Based Screening Programs
Community health nurses can implement effective diabetes screening programs using the following approaches:
- Opportunistic Screening: Incorporate diabetes screening into routine healthcare visits and other health screenings
- Targeted Screening Events: Organize screening activities in locations where high-risk populations gather (community centers, places of worship, workplaces)
- Mobile Screening Units: Bring screening services to underserved areas and rural communities
- Two-Step Screening Process: Use risk assessment tools first, followed by blood tests for those identified as high-risk
- Integration with Other Health Programs: Combine diabetes screening with hypertension, cholesterol, and other chronic disease screenings
Community Health Nursing Strategy: SCREEN Approach
- Strategic targeting of high-risk populations
- Comprehensive risk assessment using validated tools
- Rapid testing with point-of-care devices when appropriate
- Education provided during screening about risk factors and prevention
- Effective referral systems for those with abnormal results
- Navigation assistance to ensure follow-up care
Screening in Special Populations
| Population | Special Considerations |
|---|---|
| Children and Adolescents | Screen overweight/obese children (BMI >85th percentile) with risk factors beginning at age 10 or onset of puberty. Test every 3 years using FPG, A1C, or OGTT. |
| Pregnant Women | Screen all pregnant women at 24-28 weeks using OGTT. Screen high-risk women at first prenatal visit. For gestational diabetes: fasting glucose ≥92 mg/dL, 1-hour ≥180 mg/dL, or 2-hour ≥153 mg/dL. |
| Elderly | Consider comorbidities and life expectancy when screening. Adjust A1C interpretation (may be slightly higher in older adults without diabetes). |
| High-Risk Ethnic Groups | Consider screening at lower BMI thresholds (≥23 kg/m²) for Asian Americans. More frequent screening may be warranted for other high-risk ethnic groups. |
Diagnosis of Diabetes Mellitus
Accurate diagnosis of diabetes is essential for appropriate management and prevention of complications. Community health nurses must understand diagnostic criteria and be able to explain them to individuals and families.
Diagnostic Criteria
Diagnostic Criteria for Diabetes Mellitus
Diabetes can be diagnosed based on any of the following criteria:
- Fasting plasma glucose (FPG) ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 hours.
- 2-hour plasma glucose ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test (OGTT) using a 75g glucose load.
- Hemoglobin A1C ≥6.5% (48 mmol/mol).
- Random plasma glucose ≥200 mg/dL (11.1 mmol/L) in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis.
Note: In the absence of unequivocal hyperglycemia, results should be confirmed by repeat testing. When two different tests are available and results are discordant, the test with a result above the diagnostic threshold should be repeated.
Prediabetes Criteria
| Category | Fasting Plasma Glucose | 2-hour OGTT | A1C |
|---|---|---|---|
| Normal | <100 mg/dL (5.6 mmol/L) | <140 mg/dL (7.8 mmol/L) | <5.7% (39 mmol/mol) |
| Prediabetes | 100-125 mg/dL (5.6-6.9 mmol/L) [Impaired Fasting Glucose] | 140-199 mg/dL (7.8-11.0 mmol/L) [Impaired Glucose Tolerance] | 5.7-6.4% (39-47 mmol/mol) |
| Diabetes | ≥126 mg/dL (7.0 mmol/L) | ≥200 mg/dL (11.1 mmol/L) | ≥6.5% (48 mmol/mol) |
Diagnostic Process in Community Settings
Community health nurses should follow a structured approach to diabetes diagnosis:
- Risk Assessment: Identify individuals at high risk using validated tools (FINDRISC, ADA Risk Test)
- Initial Testing: Choose appropriate test based on setting and resources (A1C, FPG)
- Confirmation: Repeat testing if initial results are abnormal
- Classification: Determine diabetes type based on clinical presentation, age, body habitus, and other factors
- Additional Testing: Consider autoantibody testing for suspected Type 1 diabetes or specific genetic testing when appropriate
- Initial Evaluation: Assess for complications and comorbidities
Differential Diagnosis
Community health nurses should be aware of conditions that may mimic or complicate the diagnosis of diabetes:
- Gestational diabetes: Hyperglycemia first recognized during pregnancy
- Monogenic diabetes syndromes: MODY (Maturity Onset Diabetes of the Young), neonatal diabetes
- Secondary diabetes: Due to pancreatic diseases, medications (glucocorticoids, antipsychotics), endocrinopathies, infections
- Stress hyperglycemia: Transient elevation during acute illness
- Factitious hyperglycemia: Due to laboratory errors or interfering substances
- D Detect risk factors (family history, obesity, ethnicity)
- I Interpret symptoms (classic 3 P’s: polyuria, polydipsia, polyphagia)
- A Assess using appropriate tests (FPG, OGTT, A1C)
- G Gather confirmatory tests (repeat abnormal results)
- N Note type classification (Type 1, Type 2, other)
- O Organize initial evaluation (complications screening)
- S Start education and management planning
- E Ensure proper follow-up and referrals
Challenges in Community-Based Diagnosis
| Challenge | Community Health Nursing Strategy |
|---|---|
| Limited resources for testing | Use risk assessment tools to prioritize testing; partner with local laboratories for discounted services; utilize point-of-care testing when appropriate |
| Patient barriers to follow-up testing | Implement reminder systems; provide transportation assistance; offer testing at convenient times and locations |
| Cultural perceptions about diagnosis | Provide culturally sensitive education; involve community leaders; use cultural brokers |
| Confusion about diagnostic thresholds | Develop clear educational materials; use visual aids to explain test results; train community health workers on diagnostic criteria |
Primary Management of Diabetes
Effective diabetes management in community settings requires a comprehensive approach that addresses glycemic control, cardiovascular risk reduction, and lifestyle modification. Community health nurses play a vital role in supporting self-management and coordinating care.
Goals of Diabetes Management
| Parameter | General Target | Considerations for Target Adjustment |
|---|---|---|
| Glycemic Control (A1C) | <7.0% | More stringent (e.g., <6.5%) for selected patients with short disease duration, long life expectancy, no significant CVD Less stringent (e.g., <8.0%) for patients with history of severe hypoglycemia, limited life expectancy, advanced complications |
| Preprandial Capillary Plasma Glucose | 80-130 mg/dL | Individualize based on hypoglycemia risk, pregnancy status, age |
| Postprandial Capillary Plasma Glucose | <180 mg/dL | May target <140 mg/dL for selected patients if achievable without hypoglycemia |
| Blood Pressure | <140/90 mmHg | Lower targets (<130/80 mmHg) may be appropriate for individuals at high risk for CVD |
| Lipids (LDL) | With ASCVD: <70 mg/dL Without ASCVD: <100 mg/dL |
Intensity of therapy based on individual cardiovascular risk assessment |
The Diabetes Management Triad
Nutrition Therapy
Key Principles:
- Individualized approach based on preferences and goals
- Focus on whole, unprocessed foods
- Carbohydrate awareness and consistency
- Portion control and meal timing
- Mindful eating practices
Recommended Patterns:
- Mediterranean diet
- DASH diet
- Plant-based approaches
- Low-carbohydrate patterns
Physical Activity
Recommendations:
- 150+ minutes/week moderate-intensity aerobic activity
- Resistance training 2-3 times/week
- Flexibility and balance exercises
- Break up prolonged sitting every 30 minutes
Benefits:
- Improves insulin sensitivity
- Aids weight management
- Reduces cardiovascular risk
- Improves well-being
Pharmacotherapy
Type 1 Diabetes:
- Multiple daily injections or insulin pump
- Basal-bolus insulin regimen
- Carbohydrate counting
Type 2 Diabetes:
- Metformin as first-line therapy
- Additional agents based on comorbidities
- Cardiovascular and renal benefits of newer agents
- Insulin when indicated
Pharmacological Management
| Medication Class | Mechanism of Action | Main Benefits | Key Nursing Considerations |
|---|---|---|---|
| Biguanides (Metformin) | Decreases hepatic glucose production; improves insulin sensitivity | Weight neutral/loss; cardiovascular benefits; low hypoglycemia risk | Take with meals; GI side effects; vitamin B12 monitoring; renal function monitoring |
| Sulfonylureas | Stimulates insulin secretion from pancreatic beta cells | Rapid glucose-lowering effect; inexpensive | Hypoglycemia risk; weight gain; take with meals; diminishing effect over time |
| DPP-4 Inhibitors | Increases incretin levels, increasing insulin secretion and decreasing glucagon | Weight neutral; low hypoglycemia risk | Dose adjustment for renal impairment; joint pain monitoring |
| SGLT-2 Inhibitors | Blocks glucose reabsorption in kidneys, increasing urinary glucose excretion | Weight loss; BP reduction; cardiovascular and renal protection | Genital mycotic infections; euglycemic DKA risk; adequate hydration; foot care |
| GLP-1 Receptor Agonists | Increases insulin secretion; decreases glucagon; slows gastric emptying; promotes satiety | Weight loss; cardiovascular benefits; low hypoglycemia risk | Injection technique education; nausea management; pancreatitis monitoring |
| Insulin | Replaces endogenous insulin | Most effective glucose-lowering agent; no dose limit | Injection technique; hypoglycemia management; storage instructions; dose adjustment |
Diabetes Self-Management Education and Support (DSMES)
DSMES is a cornerstone of diabetes care and should be facilitated by community health nurses:
- E Eating plan and nutrition education
- D Drug therapy management and administration skills
- U Understanding blood glucose monitoring
- C Cardiovascular risk reduction strategies
- A Activity planning and exercise effects
- T Treatment of acute complications (hypo/hyperglycemia)
- E Emotional health and coping skills
Community Health Nursing Approaches to Diabetes Management
- Group-Based Education Programs: Structured group sessions covering essential diabetes management topics
- Home Visits: Individualized support in the person’s environment to address specific barriers
- Telehealth Services: Remote monitoring, virtual education, and support for individuals with access barriers
- Community Health Worker Models: Trained community members providing culturally appropriate support and navigation
- Peer Support Programs: Connecting individuals with others who have successfully managed diabetes
- Medication Management: Simplifying regimens, addressing adherence barriers, monitoring for side effects
- Problem-Solving Support: Helping individuals develop strategies to overcome daily management challenges
Special Considerations
Community health nurses should pay special attention to diabetes management in:
- Elderly patients: Fall risk, cognitive function, medication burden
- Pregnant women: Tighter glycemic targets, increased monitoring, medication safety
- Children and adolescents: Growth and development, school management, family dynamics
- Low literacy populations: Simplified education materials, teach-back methods
- Food insecure individuals: Practical meal planning, resource connection
Referral Guidelines for Diabetes
Timely and appropriate referrals are essential for comprehensive diabetes care. Community health nurses must know when and where to refer individuals with diabetes for specialized care and support services.
Indications for Referral
| Clinical Situation | Referral Type | Urgency |
|---|---|---|
| Newly diagnosed Type 1 diabetes | Endocrinologist | Immediate (same day) |
| Diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS) | Emergency department | Immediate (emergency) |
| Severe hypoglycemia requiring assistance | Emergency department | Immediate (emergency) |
| Newly diagnosed Type 2 diabetes | Primary care provider; diabetes education program | Within 1-2 weeks |
| Persistent hyperglycemia despite treatment adherence | Endocrinologist | Within 2-4 weeks |
| Gestational diabetes | High-risk obstetrics; diabetes education | Within 1 week |
| New or worsening retinopathy symptoms | Ophthalmologist | Within 1-4 weeks (depending on symptoms) |
| Foot ulcers or infections | Podiatrist; wound care specialist | Within 1-7 days (depending on severity) |
| Chronic kidney disease (eGFR <60 ml/min) | Nephrologist | Within 2-4 weeks |
| Painful neuropathy | Neurology | Within 2-4 weeks |
| Diabetes distress, depression, anxiety | Mental health provider | Within 2-4 weeks |
Multidisciplinary Diabetes Care Team
Community health nurses coordinate care across a multidisciplinary team for comprehensive diabetes management:
Core Team Members
- Primary Care Provider: Overall medical management, coordination of care
- Endocrinologist: Specialized diabetes management, complex cases
- Diabetes Educator: Self-management education, skills training
- Registered Dietitian: Medical nutrition therapy, meal planning
- Community Health Nurse: Home-based support, case management, navigation
- Pharmacist: Medication management, adherence support
Extended Team Members
- Ophthalmologist/Optometrist: Eye examinations, retinopathy management
- Podiatrist: Foot care, ulcer management
- Nephrologist: Kidney disease management
- Cardiologist: Cardiovascular disease management
- Mental Health Provider: Psychological support, behavioral strategies
- Social Worker: Resource coordination, social determinants
- Exercise Physiologist: Physical activity prescription
Referral Process in Community Settings
- R Recognize indication for referral
- E Evaluate urgency and appropriate provider
- F Facilitate appointment scheduling and transportation
- E Educate patient about referral purpose and expectations
- R Review outcomes and ensure information flow back to primary team
Overcoming Referral Barriers
Community health nurses should address barriers to successful diabetes referrals:
| Barrier | Community Health Nursing Strategies |
|---|---|
| Geographic distance to specialists | Telehealth options; mobile specialist clinics; transportation assistance; community-based care |
| Financial constraints | Insurance navigation; sliding-scale services; medication assistance programs; community resources |
| Long wait times for appointments | Established referral pathways; urgent care protocols; interim management support |
| Health literacy challenges | Clear referral instructions; teach-back method; appointment reminders; follow-up support |
| Cultural/language barriers | Cultural brokers; interpreter services; culturally concordant providers when possible |
| Poor information exchange between providers | Standardized referral forms; care coordination systems; follow-up communication |
Community Health Nursing Focus
Community health nurses can develop a diabetes referral resource directory specific to their community. This should include:
- Specialist contact information and referral procedures
- Insurance acceptance and payment options
- Typical wait times and urgent referral protocols
- Transportation resources
- Language services available
- Community-based support services
Follow-up Care for Diabetes
Consistent follow-up care is essential for successful long-term diabetes management. Community health nurses play a critical role in ensuring appropriate monitoring, preventing complications, and supporting ongoing self-management.
Recommended Follow-up Schedule
| Parameter | Frequency | Community Health Nursing Role |
|---|---|---|
| Hemoglobin A1C | Every 3-6 months (depending on control and stability) | Ensure testing appointments; help interpret results; adjust management plan as needed |
| Blood pressure | Every routine visit (at least quarterly) | Home BP monitoring education; lifestyle counseling for hypertension; medication adherence support |
| Lipid profile | Annually (more frequently if abnormal or on lipid-lowering therapy) | Lipid management education; dietary counseling; medication adherence |
| Comprehensive foot examination | Annually (more frequently for high-risk feet) | Basic foot assessments; foot care education; prompt referral for abnormalities |
| Comprehensive eye examination | Annually (less frequently after normal exams; more for retinopathy) | Ensure appointments are scheduled; address barriers to attendance; follow up on findings |
| Nephropathy screening | Annually (urine albumin-to-creatinine ratio and eGFR) | Education on kidney protection; ensure testing completion; medication review |
| Self-management education review | Annually and with any treatment changes | Assess knowledge gaps; provide ongoing education; address barriers to self-care |
| Influenza vaccination | Annually | Ensure vaccination; address vaccine concerns; provide vaccine education |
| Psychological assessment | Periodically, at least annually | Screen for diabetes distress, depression, anxiety; provide support; refer as needed |
Components of Effective Follow-up
Clinical Monitoring
- Glycemic control assessment: A1C, glucose patterns, hypoglycemia episodes
- Medication review: Effectiveness, side effects, adherence, affordability
- Complication screening: Early detection of microvascular and macrovascular complications
- Weight and BMI monitoring: Trends and impact on control
- Comorbidity management: Hypertension, dyslipidemia, cardiovascular disease
Self-Management Support
- Self-monitoring review: Blood glucose patterns, technique, equipment
- Dietary adherence: Meal planning challenges, problem-solving
- Physical activity: Progress, barriers, adjustments
- Problem-solving skills: Managing sick days, travel, special occasions
- Psychological support: Coping strategies, stress management, support systems
Follow-up Methods in Community Settings
Community health nurses can use various approaches to ensure effective diabetes follow-up:
- Home Visits: Direct observation of living environment, medication management, and self-care practices
- Telephone Follow-up: Regular check-ins for medication adherence, symptom monitoring, and problem-solving
- Group Follow-up Sessions: Peer support and education in community settings
- Telehealth Visits: Video consultations for those with transportation or mobility challenges
- Mobile Health Applications: Digital tools for remote monitoring and communication
- Community Health Worker Outreach: Cultural bridging and support in underserved communities
- Nurse-led Clinics: Specialized diabetes follow-up services in community settings
- F Frequency of monitoring appropriate to individual needs
- O Outcomes tracking (clinical measures, quality of life)
- L Lifestyle management support (diet, activity, stress)
- L Laboratory monitoring on schedule
- O Ongoing complication screening
- W Wellness promotion (vaccination, mental health)
Strategies for Improving Follow-up Adherence
| Challenge | Community Health Nursing Strategy |
|---|---|
| Missed appointments | Reminder systems (calls, texts, postcards); appointment tracking; follow-up for missed visits; flexible scheduling options |
| Transportation barriers | Home-based follow-up; telehealth options; transportation assistance programs; community-based follow-up locations |
| Low health literacy | Simplified follow-up instructions; pictorial schedules; teach-back method; involve family members |
| Multiple providers/fragmented care | Care coordination; centralized follow-up planning; shared records; communication facilitation |
| Financial constraints | Link to assistance programs; sliding scale services; bundled follow-up visits; cost-effective testing options |
Red Flags Requiring Immediate Follow-up
Community health nurses should ensure immediate follow-up for these diabetes-related concerns:
- Severe or frequent hypoglycemia episodes
- Significantly elevated blood glucose (>300 mg/dL) persisting despite treatment
- New foot ulcers or infections
- Sudden vision changes
- Chest pain or cardiovascular symptoms
- Symptoms of diabetic ketoacidosis (vomiting, abdominal pain, rapid breathing)
- Acute illness affecting diabetes control
Global Best Practices in Diabetes Management
Examining global approaches to diabetes management can provide valuable insights for community health nursing practice. These innovative models can be adapted to local contexts to improve diabetes outcomes.
Innovative Country-Specific Approaches
| Country/Region | Model/Approach | Key Elements | Outcomes |
|---|---|---|---|
| Finland | North Karelia Project / DEHKO National Diabetes Prevention Program | Community-wide lifestyle intervention; policy changes; food industry partnerships; primary care integration | Significant reduction in Type 2 diabetes incidence; decreased cardiovascular mortality |
| Singapore | “War on Diabetes” National Initiative | School-based prevention; workplace health; public education campaigns; early screening; subsidized care | Improved screening rates; increased public awareness; enhanced care accessibility |
| Mexico | MIDE Program (Integral Diabetes Management) | Group-based care; community health workers; simplified treatment algorithms; patient empowerment focus | Improved glycemic control; reduced complications; increased self-management skills |
| Australia | Integrated Diabetes Care for Indigenous Communities | Cultural adaptation; indigenous health workers; community ownership; outreach services | Increased engagement; improved care continuity; culturally appropriate management |
| United Kingdom | DESMOND Program (Diabetes Education and Self-Management for Ongoing and Newly Diagnosed) | Structured education program; philosophy of patient empowerment; standardized curriculum; quality assurance | Improved knowledge; weight reduction; smoking cessation; psychological well-being |
Translating Global Practices to Local Settings
Community health nurses can adapt global best practices for diabetes management to their local communities by following these principles:
Assessment and Adaptation
- Conduct a community needs assessment to identify specific diabetes challenges
- Evaluate local resources, infrastructure, and cultural contexts
- Select promising global models that align with local needs
- Adapt interventions to account for cultural preferences, health beliefs, and social norms
- Develop implementation plans with community input and stakeholder engagement
Implementation Strategies
- Start with pilot implementation in receptive communities
- Leverage existing community structures and relationships
- Train local champions and build capacity within the community
- Incorporate regular feedback and continuous quality improvement
- Document outcomes and share learnings to build evidence for broader implementation
Universal Elements of Successful Diabetes Programs
Across different global contexts, successful diabetes management programs share these common elements:
- Patient-Centered Approach: Tailoring care to individual needs, preferences, and circumstances
- Multidisciplinary Team Care: Coordinated services across healthcare providers
- Community Engagement: Active participation of community members in program design and implementation
- Cultural Competence: Respect for and integration of cultural beliefs and practices
- Self-Management Support: Empowering individuals with knowledge and skills
- Health System Integration: Connecting community programs with formal healthcare services
- Technology Utilization: Appropriate use of technology to extend reach and effectiveness
- Policy Advocacy: Addressing social determinants through policy change
Global Learning, Local Action
Community health nurses can contribute to global diabetes knowledge exchange by:
- Documenting and publishing successful local adaptations
- Participating in international nursing networks focused on diabetes care
- Contributing to international diabetes registries and databases
- Engaging in collaborative research with international partners
- Advocating for evidence-based policies informed by global best practices
