
Nursing Care Plan for Diabetes Mellitus
20 Essential NANDA Nursing Diagnoses with Detailed Interventions and Expected Outcomes
Introduction to Diabetes Mellitus Nursing Care
Developing comprehensive nursing care plans for patients with diabetes mellitus is essential for effective management of this chronic metabolic disorder. This guide provides 20 key nursing diagnoses with detailed interventions, rationales, and expected outcomes to help nursing students deliver evidence-based care. Diabetes mellitus nursing care plan.
As nursing professionals, your role in diabetes management extends beyond medication administration to include education, monitoring, prevention of complications, and promotion of self-care. The care plans provided here follow the nursing process and adhere to NANDA-I terminology.
Study Tip:
Throughout this guide, look for visual aids, mnemonics, and flowcharts designed to enhance your comprehension and retention. These learning tools will help you understand the complex relationships between diabetes pathophysiology and nursing interventions.
Table of Contents
- Diabetes Care Mnemonics
- Diabetes Care Flowchart
- Imbalanced Nutrition: More Than Body Requirements
- Risk for Unstable Blood Glucose
- Ineffective Health Management
- Risk for Infection
- Risk for Impaired Skin Integrity
- Deficient Knowledge
- Ineffective Peripheral Tissue Perfusion
- Readiness for Enhanced Self-Health Management
- Impaired Urinary Elimination
- Acute Pain
- Chronic Pain
- Fatigue
- Risk for Disturbed Sensory Perception
- Risk for Falls
- Anxiety
- Risk for Disturbed Body Image
- Powerlessness
- Sexual Dysfunction
- Risk for Impaired Oral Mucous Membrane
- Risk for Diabetic Ketoacidosis
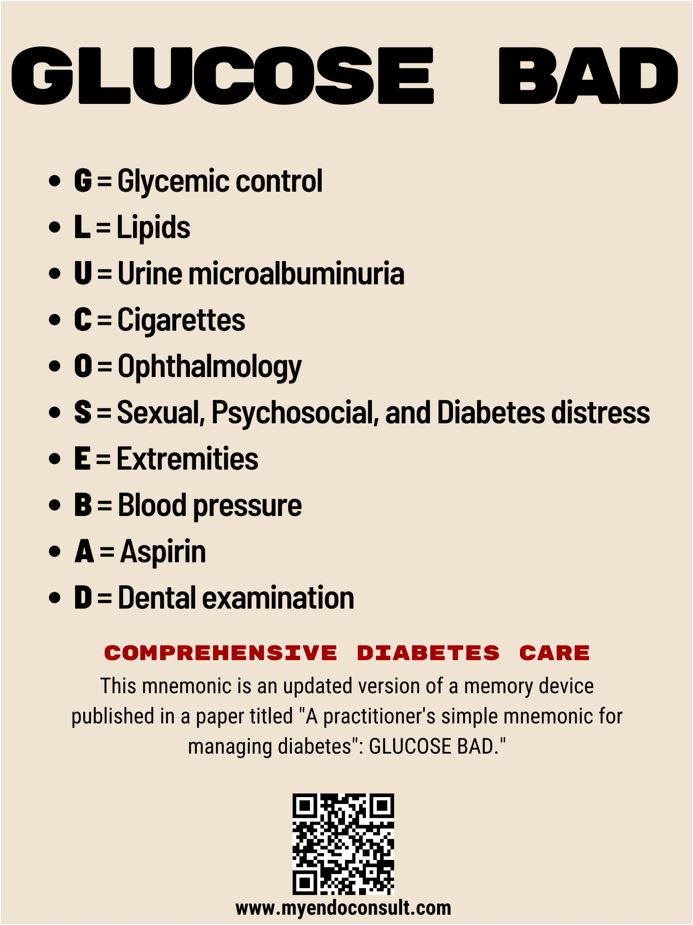
Diabetes Care Mnemonics
GLUCOSE BAD for Diabetes Symptoms
- G – Glycosuria
- L – Lethargy
- U – Urination (frequent)
- C – Compromised immune system
- O – Overeating (polyphagia)
- S – Sweating
- E – Extreme thirst (polydipsia)
- B – Blurred vision
- A – Acidosis
- D – Dehydration
DKA Nursing Intervention Mnemonic: DIABETIC

- D – Determine and monitor vital signs
- I – IV fluids and insulin, observe intake and output
- A – ABG monitoring
- B – Blood glucose monitoring
- E – Electrolyte replacement
- T – Treat the cause
- I – Identify signs of improvement
- C – Continue patient assessment
Insulin Types Mnemonic

Remembering insulin types, onset, peak, and duration is crucial for diabetes nursing care. Use this mnemonic:
Rapid-Acting (R)
- Onset: 10-15 minutes
- Peak: 1-2 hours
- Duration: 3-5 hours
- Examples: Humalog, NovoLog, Apidra
Short-Acting (S)
- Onset: 30 minutes
- Peak: 2-4 hours
- Duration: 5-8 hours
- Examples: Regular insulin (Humulin R)
Intermediate-Acting (I)
- Onset: 1-2 hours
- Peak: 6-10 hours
- Duration: 10-16 hours
- Examples: NPH (Humulin N)
Long-Acting (L)
- Onset: 1-2 hours
- Peak: No peak (steady)
- Duration: 20-24+ hours
- Examples: Lantus, Levemir
Diabetes Nursing Care Flowchart

Flowchart illustrating the nursing care process for diabetes mellitus management
20 Key Nursing Diagnoses for Diabetes Mellitus
1. Imbalanced Nutrition: More Than Body Requirements
Assessment/Defining Characteristics:
- Weight 20% over ideal body weight for height and frame
- BMI > 25 kg/m²
- Sedentary activity level
- Dysfunctional eating patterns
- Excessive intake compared to metabolic needs
Related Factors:
- Excessive intake in relation to metabolic requirements
- Psychosocial factors affecting eating habits
- Decreased physical activity
- Limited knowledge regarding nutritional needs
Nursing Interventions:
-
1. Perform comprehensive nutritional assessment
Rationale: Establishes baseline nutritional status and identifies specific areas for intervention.
-
2. Collaborate with registered dietitian to develop individualized meal plan
Rationale: Ensures nutritional plan meets specific needs of patient with diabetes while promoting weight management.
-
3. Educate patient on carbohydrate counting and glycemic index
Rationale: Empowers patient to make informed food choices that help maintain stable blood glucose levels.
-
4. Teach portion control techniques using visual aids
Rationale: Visual cues help patients better understand appropriate portion sizes.
-
5. Implement gradual exercise program appropriate for patient’s condition
Rationale: Regular exercise improves insulin sensitivity and helps with weight management.
Expected Outcomes:
- Patient will demonstrate understanding of relationship between diet, exercise, and blood glucose control
- Patient will develop a meal plan with appropriate caloric intake within 1 week
- Patient will show consistent adherence to meal plan as evidenced by food diary
- Patient will demonstrate gradual weight loss of 1-2 pounds per week
- Patient will maintain blood glucose levels within target range
2. Risk for Unstable Blood Glucose
Assessment/Defining Characteristics:
- Fasting blood glucose > 126 mg/dL
- HbA1c > 6.5%
- History of blood glucose fluctuations
- Inadequate blood glucose monitoring
- Altered medication regimen adherence
Risk Factors:
- Insufficient diabetes management knowledge
- Inadequate compliance with diabetes treatment plan
- Medication mismanagement
- Stress and illness
- Dietary inconsistency
- Lack of acceptance of diagnosis
Nursing Interventions:
-
1. Monitor blood glucose levels according to recommended schedule
Rationale: Regular monitoring helps identify patterns and triggers for glucose fluctuations.
-
2. Teach proper blood glucose monitoring technique
Rationale: Ensures accurate results for appropriate treatment decisions.
-
3. Educate about relationship between food intake, physical activity, and blood glucose levels
Rationale: Helps patient understand how different factors affect glycemic control.
-
4. Teach signs/symptoms of hypoglycemia and hyperglycemia and appropriate interventions
Rationale: Early recognition allows timely intervention to prevent serious complications.
-
5. Assist patient in developing a sick-day management plan
Rationale: Illness can significantly impact blood glucose levels; a plan helps maintain control during these periods.
Expected Outcomes:
- Patient will maintain blood glucose levels within target range (typically 80-130 mg/dL before meals and <180 mg/dL after meals)
- Patient will demonstrate proper blood glucose monitoring technique
- Patient will identify and respond appropriately to episodes of hypoglycemia and hyperglycemia
- Patient will maintain food and activity log with corresponding glucose readings
- Patient will achieve HbA1c within target range (typically <7%)
3. Ineffective Health Management
Assessment/Defining Characteristics:
- Failure to include treatment regimen in daily routines
- Ineffective choices in daily living for meeting health goals
- Verbalization of difficulty following prescribed regimen
- Acceleration of illness symptoms
- Failure to achieve blood glucose targets
Related Factors:
- Complexity of healthcare system
- Complexity of therapeutic regimen
- Insufficient knowledge of management regimen
- Economic difficulties
- Social support deficits
- Perceived barriers to treatment
Nursing Interventions:
-
1. Assess patient’s understanding of diabetes management and identify barriers to compliance
Rationale: Identifies knowledge gaps and specific obstacles to address in the care plan.
-
2. Simplify regimen when possible and integrate into patient’s daily routine
Rationale: Treatment plans that fit into existing routines are more likely to be followed.
-
3. Provide educational materials at appropriate literacy level
Rationale: Ensures patient can understand and utilize provided information.
-
4. Connect patient with community resources and support groups
Rationale: Additional support systems can improve adherence and provide practical solutions.
-
5. Develop a collaborative self-management plan with achievable short-term goals
Rationale: Patient involvement in planning and achieving small successes increases motivation for long-term adherence.
Expected Outcomes:
- Patient will identify specific barriers to diabetes self-management
- Patient will incorporate diabetes management tasks into daily routine
- Patient will demonstrate improved adherence to treatment plan
- Patient will utilize community resources for ongoing diabetes support
- Patient will verbalize increased confidence in managing diabetes
4. Risk for Infection
Assessment/Risk Factors:
- Elevated blood glucose levels
- Compromised immune function
- Poor circulation, especially in extremities
- Decreased sensation due to neuropathy
- Delayed wound healing
- Altered skin integrity
Nursing Interventions:
-
1. Teach proper foot care and daily foot inspection
Rationale: Early detection of skin breaks or injuries allows prompt treatment to prevent infection.
-
2. Monitor for signs and symptoms of infection (fever, increased WBC, redness, warmth, pain, swelling)
Rationale: Early identification allows prompt intervention.
-
3. Maintain glycemic control within target range
Rationale: Hyperglycemia impairs immune function and promotes bacterial growth.
-
4. Teach proper hand hygiene and general infection prevention measures
Rationale: Reduces exposure to pathogens.
-
5. Educate about proper insulin injection technique and site rotation
Rationale: Reduces risk of infection at injection sites and ensures optimal insulin absorption.
Expected Outcomes:
- Patient will remain free of infection
- Patient will demonstrate proper foot care techniques
- Patient will recognize and report early signs of infection
- Patient will maintain blood glucose within target range
- Patient will demonstrate appropriate injection technique
5. Risk for Impaired Skin Integrity
Assessment/Risk Factors:
- Peripheral vascular disease
- Peripheral neuropathy with decreased sensation
- Poor glycemic control
- Altered nutritional status
- Compromised circulation
- History of previous foot ulcers
- Improper footwear
Nursing Interventions:
-
1. Perform comprehensive skin assessment with focus on feet and lower extremities
Rationale: Early identification of skin changes allows prompt intervention.
-
2. Teach proper foot care protocol: daily inspection, gentle cleansing, moisturizing, proper nail care
Rationale: Routine foot care prevents skin breakdown and subsequent complications.
-
3. Educate about proper footwear selection and use
Rationale: Appropriate footwear reduces pressure points and injury risk.
-
4. Teach patient to avoid extreme temperatures on feet (no heating pads, hot water)
Rationale: Decreased sensation may prevent patient from detecting potential burn injuries.
-
5. Recommend regular visits with podiatrist
Rationale: Professional foot care helps prevent complications, especially for high-risk patients.
Expected Outcomes:
- Patient will maintain intact skin integrity
- Patient will demonstrate proper foot inspection and care techniques
- Patient will wear appropriate footwear
- Patient will identify and report early signs of skin breakdown
- Patient will establish regular podiatric care
6. Deficient Knowledge
Assessment/Defining Characteristics:
- Inaccurate follow-through of instructions
- Verbalization of knowledge deficit regarding diabetes management
- Inappropriate or exaggerated behaviors (denial, fear, hostility)
- Frequent questions or misconceptions about diabetes care
- Poor glycemic control despite treatment
Related Factors:
- Recent diagnosis
- Lack of exposure to information
- Information misinterpretation
- Cognitive limitations
- Cultural or language barriers
- Limited interest in learning
Nursing Interventions:
-
1. Assess patient’s current knowledge and learning needs
Rationale: Establishes baseline for developing individualized teaching plan.
-
2. Provide education using multiple teaching methods (visual, verbal, written)
Rationale: Addresses different learning styles for improved comprehension and retention.
-
3. Provide information in manageable segments, prioritizing essential survival skills first
Rationale: Prevents information overload and focuses on critical skills needed for immediate self-care.
-
4. Demonstrate and have patient return-demonstrate skills (insulin administration, glucose monitoring)
Rationale: Hands-on practice reinforces learning and ensures proper technique.
-
5. Provide written materials at appropriate literacy level and in preferred language
Rationale: Enhances understanding and serves as reference after teaching sessions.
Expected Outcomes:
- Patient will verbalize understanding of diabetes pathophysiology, complications, and management
- Patient will demonstrate proper technique for blood glucose monitoring and medication administration
- Patient will correctly interpret blood glucose results and take appropriate actions
- Patient will identify strategies to prevent complications
- Patient will express confidence in performing self-care activities
7. Ineffective Peripheral Tissue Perfusion
Assessment/Defining Characteristics:
- Altered skin characteristics (color, temperature, hair growth)
- Diminished pulses
- Skin color changes when limb is lowered
- Claudication
- Delayed wound healing
- Edema
Related Factors:
- Diabetes mellitus
- Sedentary lifestyle
- Smoking
- Hyperglycemia
- Hypertension
- Hyperlipidemia
Nursing Interventions:
-
1. Assess peripheral pulses, capillary refill, temperature, and color of extremities
Rationale: Establishes baseline circulatory status and aids in early identification of changes.
-
2. Educate about and promote smoking cessation
Rationale: Smoking causes vasoconstriction and further compromises peripheral circulation.
-
3. Teach and encourage regular walking program within patient’s tolerance
Rationale: Exercise improves circulation and collateral blood flow development.
-
4. Instruct to avoid constrictive clothing and crossing legs
Rationale: Prevents further compromise of circulation.
-
5. Monitor and assist with blood pressure, lipid, and glucose control
Rationale: Controlling these factors helps prevent further vascular damage.
Expected Outcomes:
- Patient will demonstrate improved or stable peripheral circulation
- Patient will identify and modify risk factors affecting peripheral circulation
- Patient will participate in regular physical activity to improve circulation
- Patient will maintain blood pressure, glucose, and lipids within target ranges
- Patient will report decreased episodes of claudication or pain
8. Readiness for Enhanced Self-Health Management
Assessment/Defining Characteristics:
- Expresses desire to manage illness and prevent complications
- Seeks information about diabetes management
- Describes reduction of risk factors
- Expresses little difficulty with prescribed regimen
- Makes appropriate choices of daily activities for meeting goals
Nursing Interventions:
-
1. Provide positive reinforcement for self-management efforts
Rationale: Reinforces positive behaviors and motivates continued adherence.
-
2. Help patient set achievable short and long-term goals
Rationale: Clear, attainable goals provide direction and measurable outcomes.
-
3. Provide advanced diabetes education and resources
Rationale: Builds on existing knowledge to enhance self-management capabilities.
-
4. Connect patient with peer support groups and community resources
Rationale: Peer support enhances motivation and provides practical strategies from others’ experiences.
-
5. Encourage patient to become involved in diabetes advocacy or education
Rationale: Helping others reinforces personal knowledge and commitment to self-management.
Expected Outcomes:
- Patient will achieve personal health goals related to diabetes management
- Patient will demonstrate advanced understanding of diabetes self-management strategies
- Patient will participate in diabetes support community
- Patient will maintain optimal health indicators (HbA1c, lipids, blood pressure)
- Patient will independently troubleshoot and solve problems related to diabetes management
9. Impaired Urinary Elimination
Assessment/Defining Characteristics:
- Frequency, urgency, and/or nocturia
- Polyuria (excessive urine output)
- Changes in urinary pattern
- Urinary tract infections
- Difficulty initiating voiding
Related Factors:
- Diabetes-related autonomic neuropathy affecting bladder function
- Hyperglycemia causing osmotic diuresis
- Urinary tract infections
- Diabetic nephropathy
Nursing Interventions:
-
1. Monitor intake and output and urinary patterns
Rationale: Provides objective data about urinary function and helps identify abnormalities.
-
2. Test urine for glucose, ketones, protein, and signs of infection as indicated
Rationale: Helps identify causes of urinary symptoms and detect complications.
-
3. Maintain glycemic control to reduce polyuria
Rationale: Hyperglycemia causes osmotic diuresis; controlling blood glucose helps normalize urine output.
-
4. Teach patient about adequate hydration while balancing fluid restrictions if present
Rationale: Proper hydration helps prevent urinary tract infections while respecting cardiac or renal limitations.
-
5. Educate about urinary hygiene and infection prevention
Rationale: People with diabetes are at increased risk for UTIs; proper hygiene helps prevent infection.
Expected Outcomes:
- Patient will demonstrate normalized urinary patterns
- Patient will maintain adequate hydration
- Patient will remain free from urinary tract infections
- Patient will maintain blood glucose within target range to reduce polyuria
- Patient will verbalize understanding of relationship between diabetes and urinary function
10. Acute Pain
Assessment/Defining Characteristics:
- Verbal reports of pain (burning, tingling, electric shock-like)
- Guarding or protective behavior
- Changes in appetite or sleep
- Facial expressions of pain
- Focus on pain
- Altered vital signs during painful episodes
Related Factors:
- Diabetic neuropathy
- Peripheral vascular disease
- Infection or inflammation
- Musculoskeletal complications (frozen shoulder, carpal tunnel syndrome)
Nursing Interventions:
-
1. Perform comprehensive pain assessment using standardized scale
Rationale: Establishes baseline and allows evaluation of interventions.
-
2. Administer prescribed analgesics or neuropathic pain medications
Rationale: Pharmacological management is often first-line treatment for neuropathic pain.
-
3. Teach non-pharmacological pain management techniques (relaxation, distraction, positioning)
Rationale: Complementary approaches can enhance pain control and reduce medication dependence.
-
4. Maintain glycemic control within target range
Rationale: Improved glucose control can reduce neuropathic symptoms over time.
-
5. Monitor for medication side effects and effectiveness
Rationale: Ensures optimal pain management while minimizing adverse effects.
Expected Outcomes:
- Patient will report reduced pain intensity (decrease of at least 2 points on pain scale)
- Patient will demonstrate use of effective pain management strategies
- Patient will maintain functional abilities despite pain
- Patient will verbalize understanding of pain management plan
- Patient will maintain adequate rest and sleep patterns
11. Chronic Pain
Assessment/Defining Characteristics:
- Reports of persistent pain for >3 months
- Changes in ability to perform activities of daily living
- Depression or irritability related to pain
- Altered sleep pattern
- Social withdrawal
- Decreased quality of life
Related Factors:
- Diabetic peripheral neuropathy
- Long-term peripheral vascular disease
- Charcot joint
- Long-standing diabetic amyotrophy
Nursing Interventions:
-
1. Conduct comprehensive pain assessment including impact on function and quality of life
Rationale: Chronic pain affects multiple dimensions of life and requires holistic assessment.
-
2. Develop multimodal pain management plan with patient
Rationale: Combined approaches typically work better than single modalities for chronic pain.
-
3. Facilitate referrals to pain specialists, physical therapy, occupational therapy as appropriate
Rationale: Multidisciplinary approach provides comprehensive management.
-
4. Screen for and address depression and anxiety
Rationale: Psychological factors significantly impact chronic pain perception and management.
-
5. Educate about pacing activities and energy conservation techniques
Rationale: Helps maintain function while managing pain and preventing exacerbations.
Expected Outcomes:
- Patient will report improved pain management with reduced impact on daily activities
- Patient will demonstrate effective use of multiple pain management strategies
- Patient will maintain optimal level of physical and social functioning
- Patient will demonstrate healthy coping mechanisms for dealing with chronic pain
- Patient will report improved quality of life despite chronic pain
12. Fatigue
Assessment/Defining Characteristics:
- Verbalization of overwhelming lack of energy
- Inability to maintain usual routines
- Decreased performance
- Lethargy or listlessness
- Increased physical complaints
- Emotional lability
Related Factors:
- Blood glucose fluctuations
- Sleep disturbance
- Increased metabolic energy expenditure
- Chronic disease state
- Anemia
- Depression
Nursing Interventions:
-
1. Assess for underlying causes of fatigue (poor glycemic control, anemia, sleep apnea, depression)
Rationale: Identifying and addressing specific causes provides targeted management.
-
2. Optimize blood glucose management
Rationale: Both hyperglycemia and hypoglycemia contribute to fatigue.
-
3. Teach energy conservation techniques and activity pacing
Rationale: Helps patient manage limited energy resources effectively.
-
4. Develop graduated exercise program
Rationale: Regular physical activity paradoxically helps reduce fatigue over time.
-
5. Promote good sleep hygiene practices
Rationale: Quality sleep reduces fatigue; diabetes can disrupt sleep patterns.
Expected Outcomes:
- Patient will identify factors that contribute to fatigue
- Patient will demonstrate improved energy level as evidenced by increased activity tolerance
- Patient will maintain blood glucose within target range
- Patient will implement energy conservation techniques in daily activities
- Patient will report improved sleep quality
13. Risk for Disturbed Sensory Perception
Assessment/Risk Factors:
- Diabetic peripheral neuropathy
- Decreased sensitivity to heat, cold, pressure, or pain
- Altered proprioception
- Diabetic retinopathy
- Visual changes
- Biochemical imbalances affecting neural function
Nursing Interventions:
-
1. Assess sensory function regularly (monofilament testing, vibration perception, visual acuity)
Rationale: Early detection of sensory changes allows prompt intervention.
-
2. Teach compensatory strategies for sensory deficits
Rationale: Visual inspection can compensate for loss of tactile sensation.
-
3. Educate about safety measures to prevent injury
Rationale: Decreased sensation increases risk of undetected injury.
-
4. Encourage regular eye examinations
Rationale: Early detection and treatment of retinopathy helps prevent vision loss.
-
5. Maintain optimal glycemic control
Rationale: Reduces progression of neuropathy and retinopathy.
Expected Outcomes:
- Patient will remain free from injury related to sensory deficits
- Patient will demonstrate safety measures to compensate for sensory deficits
- Patient will maintain optimal blood glucose control to slow progression of neuropathy
- Patient will obtain recommended eye examinations
- Patient will report any new sensory changes promptly
14. Risk for Falls
Assessment/Risk Factors:
- Peripheral neuropathy with decreased proprioception
- Visual impairment due to retinopathy
- Orthostatic hypotension
- Episodes of hypoglycemia
- Altered gait or balance
- Diabetic foot problems
Nursing Interventions:
-
1. Perform fall risk assessment using standardized tool
Rationale: Identifies specific risk factors to address in prevention plan.
-
2. Assess home environment and recommend modifications
Rationale: Environmental adaptations reduce fall hazards.
-
3. Teach patient to monitor for and prevent hypoglycemic episodes
Rationale: Hypoglycemia can cause dizziness, confusion, and falls.
-
4. Refer for physical therapy to improve balance, strength, and gait
Rationale: Exercise interventions can improve physical function and reduce fall risk.
-
5. Recommend appropriate footwear and assistive devices if needed
Rationale: Proper footwear and mobility aids improve stability and safety.
Expected Outcomes:
- Patient will remain free from falls
- Patient will identify personal fall risk factors
- Patient will implement environmental modifications to reduce fall hazards
- Patient will use appropriate assistive devices and footwear
- Patient will maintain blood glucose within target range to prevent hypoglycemia
15. Anxiety
Assessment/Defining Characteristics:
- Expressed concerns regarding diabetes diagnosis or complications
- Apprehensive affect or behavior
- Increased tension
- Poor concentration
- Insomnia
- Expressed fear of hypoglycemic episodes
Related Factors:
- New diagnosis of chronic illness
- Threat of complications
- Situational crisis related to disease management
- Fear of hypoglycemia
- Stress of lifestyle changes
- Financial concerns related to treatment costs
Nursing Interventions:
-
1. Provide opportunities for patient to express fears and concerns
Rationale: Verbalization helps identify specific anxieties and is first step in addressing them.
-
2. Provide accurate information about diabetes and its management
Rationale: Knowledge helps reduce fears based on misconceptions.
-
3. Teach relaxation techniques (deep breathing, progressive muscle relaxation)
Rationale: Provides coping strategies to manage anxiety symptoms.
-
4. Refer to support groups or mental health services if indicated
Rationale: Peer support and professional counseling provide additional resources for managing anxiety.
-
5. Help develop step-by-step approach to diabetes self-management
Rationale: Breaking tasks into manageable steps reduces feeling of being overwhelmed.
Expected Outcomes:
- Patient will verbalize decreased anxiety about diabetes management
- Patient will demonstrate relaxation techniques to manage anxiety
- Patient will identify specific concerns and develop coping strategies
- Patient will participate in diabetes management without excessive worry
- Patient will utilize support systems when feeling anxious
16. Risk for Disturbed Body Image
Assessment/Risk Factors:
- Need for insulin injections or insulin pump
- Weight changes related to diabetes
- Presence of diabetes-related complications
- Need for continuous glucose monitoring devices
- Foot deformities or amputations
- Altered functionality due to complications
Nursing Interventions:
-
1. Assess patient’s perception of body image and impact of diabetes
Rationale: Establishes baseline and identifies specific concerns to address.
-
2. Provide opportunities to discuss feelings about body changes
Rationale: Acknowledging feelings is first step in developing healthy adaptation.
-
3. Connect with others who successfully manage diabetes and technology
Rationale: Peer role models demonstrate positive adaptation and provide practical strategies.
-
4. Teach strategies for managing visible diabetes equipment discreetly when desired
Rationale: Gives patient control over disclosure and visibility of diabetes management.
-
5. Focus on abilities rather than limitations
Rationale: Promotes positive self-concept by emphasizing strengths.
Expected Outcomes:
- Patient will express positive adaptation to body changes
- Patient will incorporate diabetes management tools into self-concept
- Patient will demonstrate confidence in managing diabetes in social situations
- Patient will verbalize acceptance of physical changes
- Patient will maintain positive self-concept
17. Powerlessness
Assessment/Defining Characteristics:
- Expressed frustration over inability to manage diabetes
- Depression about disease progression despite adherence to regimen
- Apathy about self-care
- Expressed lack of control over health outcomes
- Anxiety about disease complications
- Passive approach to care decisions
Related Factors:
- Chronic nature of diabetes
- Unpredictable blood glucose fluctuations despite adherence
- Complex healthcare system
- Development of complications despite good control
- Healthcare treatment regimen
Nursing Interventions:
-
1. Involve patient in decision-making about care plan
Rationale: Participation in care decisions increases sense of control.
-
2. Help identify aspects of care over which patient has control
Rationale: Focusing on controllable factors reduces feelings of helplessness.
-
3. Provide realistic information about diabetes management
Rationale: Understanding that blood glucose variability is normal helps reduce frustration when fluctuations occur despite adherence.
-
4. Set achievable short-term goals to build confidence
Rationale: Small successes help restore sense of control and efficacy.
-
5. Provide positive reinforcement for self-care efforts
Rationale: Recognition of efforts helps maintain motivation even when results are variable.
Expected Outcomes:
- Patient will verbalize increased sense of control over diabetes management
- Patient will actively participate in treatment decisions
- Patient will identify aspects of care within their control
- Patient will express realistic expectations about diabetes management
- Patient will demonstrate initiative in self-care activities
18. Sexual Dysfunction
Assessment/Defining Characteristics:
- Reports of changes in sexual function or satisfaction
- Erectile dysfunction in males
- Decreased libido
- Vaginal dryness in females
- Altered sexual response
- Expressed concerns about sexual performance
Related Factors:
- Diabetic autonomic neuropathy
- Vascular changes
- Medication side effects
- Psychosocial factors (depression, anxiety)
- Altered hormone levels
Nursing Interventions:
-
1. Provide private, comfortable environment to discuss sexual concerns
Rationale: Privacy and non-judgmental approach encourage open communication about sensitive topic.
-
2. Educate about relationship between diabetes and sexual function
Rationale: Understanding physiological basis helps reduce guilt and anxiety about sexual changes.
-
3. Optimize blood glucose management
Rationale: Improved glycemic control may help prevent or minimize sexual dysfunction.
-
4. Refer to appropriate specialists (urologist, gynecologist, sex therapist)
Rationale: Specialized treatment may be needed to address specific sexual concerns.
-
5. Discuss alternative expressions of intimacy and sexuality
Rationale: Expanding definition of sexual expression helps maintain intimacy despite changes in function.
Expected Outcomes:
- Patient will verbalize understanding of relationship between diabetes and sexual function
- Patient will discuss sexual concerns with healthcare provider or appropriate specialist
- Patient will identify strategies to address sexual dysfunction
- Patient will report improved sexual satisfaction
- Patient will maintain intimate relationship despite changes in sexual function
19. Risk for Impaired Oral Mucous Membrane
Assessment/Risk Factors:
- Hyperglycemia
- Decreased salivary flow (xerostomia)
- Poor oral hygiene
- Immunosuppression related to diabetes
- Medication side effects
- Dehydration
Nursing Interventions:
-
1. Assess oral cavity regularly for signs of inflammation, infection, or dryness
Rationale: Early identification allows prompt intervention.
-
2. Teach proper oral hygiene techniques
Rationale: Good oral hygiene prevents infection and complications.
-
3. Encourage adequate hydration
Rationale: Helps prevent dry mouth and promotes overall oral health.
-
4. Recommend regular dental check-ups
Rationale: Professional dental care is essential for preventing and managing complications.
-
5. Maintain optimal glycemic control
Rationale: Hyperglycemia increases risk of oral infections and impairs healing.
Expected Outcomes:
- Patient will maintain intact and healthy oral mucous membranes
- Patient will demonstrate proper oral hygiene techniques
- Patient will seek regular dental care
- Patient will maintain adequate hydration
- Patient will maintain blood glucose within target range
20. Risk for Diabetic Ketoacidosis
Assessment/Risk Factors:
- Illness or infection
- Omission of insulin doses
- New diagnosis of Type 1 diabetes
- Medication non-adherence
- Psychological stress
- Inadequate blood glucose monitoring
- Poor knowledge of sick-day management
Nursing Interventions:
-
1. Educate about signs and symptoms of DKA (polyuria, polydipsia, nausea, vomiting, abdominal pain, fruity breath)
Rationale: Early recognition allows prompt intervention before severe acidosis develops.
-
2. Develop sick-day management plan with patient
Rationale: Illness increases insulin requirements; having a plan prevents omission of insulin during illness.
-
3. Teach blood glucose and ketone monitoring during illness
Rationale: Allows early detection of developing ketosis and appropriate intervention.
-
4. Educate about importance of insulin during illness
Rationale: Common misconception that reduced food intake requires reduced insulin; during illness, insulin needs often increase despite reduced intake.
-
5. Instruct when to seek medical attention
Rationale: Establishes clear guidelines for when home management is insufficient.
Expected Outcomes:
- Patient will remain free from diabetic ketoacidosis
- Patient will identify early signs and symptoms of DKA
- Patient will demonstrate appropriate sick-day management
- Patient will maintain insulin administration during illness
- Patient will seek timely medical attention when appropriate
Summary and Key Points
Effective nursing care for patients with diabetes mellitus requires comprehensive assessment and individualized interventions addressing multiple dimensions of health. The 20 nursing diagnoses outlined in this guide cover physical, psychological, and educational aspects of diabetes care.
Remember these key principles when implementing diabetes nursing care plans:
- Glycemic control is fundamental to preventing complications
- Patient education is essential for self-management success
- Regular assessment for early complications allows prompt intervention
- Psychological support is as important as physical care
- Individualize care plans based on patient’s specific needs and situation
By addressing these nursing diagnoses systematically, you can help patients with diabetes achieve optimal health outcomes and quality of life despite living with a chronic condition.
