Pediatric Gastroenteritis
Diarrhea & Vomiting in Children
Comprehensive nursing notes for assessment, management, and patient education
Quick Reference Guide
Red Flags
- Severe dehydration (10% body weight loss)
- Bloody diarrhea
- Persistent vomiting (>24 hours)
- Signs of shock
- Altered mental status
- Infants <3 months with fever
Key Interventions
- Oral rehydration therapy (ORT)
- Assess hydration status frequently
- Monitor I/O and vital signs
- Continue age-appropriate nutrition
- Zinc supplementation
Remember
- Don’t restrict diet during diarrhea
- Don’t routinely use anti-diarrheal medications
- ORT is first-line treatment
- Monitor for electrolyte imbalances
- Educate on hand hygiene and food safety
Overview
Gastroenteritis is inflammation of the digestive tract that results in vomiting, diarrhea, or both, and is sometimes accompanied by fever or abdominal cramps. It is a common condition in the pediatric population and a leading cause of morbidity and mortality worldwide.
Key Facts
- Affects 3-5 billion children worldwide annually
- Most common in children under 5 years
- Leading cause of dehydration in pediatric patients
- Typically self-limiting (3-7 days)
- Majority of cases (70-80%) are viral in origin
Epidemiology
- 500,000 deaths/year globally in children <5 years
- In developed countries: ~1.5 million physician visits annually
- Accounts for ~200,000 hospitalizations per year in US
- Seasonal patterns: rotavirus peaks in winter months
- More severe in malnourished children and infants
Diagnostic Criteria for Acute Gastroenteritis
Defined as a diarrheal disease of rapid onset, with or without accompanying symptoms such as nausea, vomiting, fever, or abdominal pain. Criteria include:
- ≥3 loose or watery stools in 24 hours
- Change in stool consistency to looser than normal
- Duration less than 14 days
Pathophysiology
Mechanism of Disease
Gastroenteritis involves inflammation of the gastrointestinal tract mucosa, leading to dysfunction in fluid absorption and secretion. The pathophysiology varies based on the causative agent:
Viral Mechanisms:
- Damages enterocytes at villus tips
- Reduces digestive enzyme production
- Impairs absorptive capacity
- Activates enteric nervous system (causing motility changes)
- NSP4 (rotavirus) acts as viral enterotoxin
Bacterial Mechanisms:
- Enterotoxin production: Stimulates excessive fluid secretion (e.g., E. coli, V. cholerae)
- Cytotoxin production: Damages intestinal cells (e.g., C. difficile)
- Invasion: Direct mucosal invasion and inflammation (e.g., Shigella, Salmonella)
- Adherence: Attaches to mucosa causing damage (e.g., EPEC)
Pathophysiological Consequences
Diarrhea Mechanisms
Diarrhea in gastroenteritis occurs through four main mechanisms:
- Osmotic diarrhea: Unabsorbed solutes draw water into intestinal lumen
- Secretory diarrhea: Active ion secretion leads to water secretion
- Inflammatory diarrhea: Mucosal damage and inflammation
- Motility disorders: Altered intestinal transit time
Vomiting Mechanisms
Vomiting is triggered via:
- Activation of chemoreceptor trigger zone (CTZ)
- Stimulation of vagal afferents in GI tract
- Direct stimulation of vomiting center in medulla
- Inflammatory mediators affecting gut-brain axis
Dehydration Pathophysiology
The primary complication of gastroenteritis:
- Excessive fluid losses exceed intake
- Electrolyte imbalances (Na+, K+, Cl-, HCO3-)
- Metabolic acidosis from bicarbonate loss
- Decreased effective circulating volume
- Compensatory mechanisms: increased ADH, aldosterone

Pathophysiology of infectious gastroenteritis showing how different pathogens affect the intestinal mucosa
Etiology
Gastroenteritis in children has multiple causes, with infectious agents being the most common. Understanding the specific etiology helps guide appropriate treatment and preventive measures.
| Category | Causative Agent | Clinical Features | Notes |
|---|---|---|---|
| Viral (Most Common) |
Rotavirus | Watery diarrhea, vomiting, fever; lasts 5-7 days | Most common cause worldwide; winter prevalence; preventable by vaccine |
| Norovirus | More vomiting than diarrhea; lasts 1-3 days | Most common cause in US; highly contagious; year-round | |
| Adenovirus | Mild vomiting with prolonged diarrhea (1-2 weeks) | Common in children <2 years; year-round occurrence | |
| Astrovirus | Similar to mild rotavirus infection | Seasonal in winter; affects infants and young children | |
| Bacterial | Campylobacter | Bloody diarrhea, fever, abdominal pain | Often from contaminated poultry; may develop Guillain-Barré syndrome |
| Salmonella | Diarrhea, fever, abdominal cramps | Associated with eggs, poultry, unpasteurized milk; pet reptiles | |
| Shigella | Bloody, mucoid diarrhea; high fever | Highly contagious; produces Shiga toxin | |
| E. coli (STEC) | Bloody diarrhea; can lead to HUS | Associated with undercooked beef, raw milk; produces Shiga toxin | |
| C. difficile | Watery diarrhea, abdominal pain, fever | Associated with antibiotic use; toxin production | |
| Parasitic | Giardia lamblia | Chronic diarrhea, bloating, fatigue | Contaminated water; day care settings |
| Cryptosporidium | Watery diarrhea, stomach cramps | Swimming pools; severe in immunocompromised | |
| Non-Infectious | Medications | Variable presentation | Antibiotics, antacids, chemotherapy |
| Food Allergies | Diarrhea, vomiting, may have other allergic symptoms | Common allergens: milk, eggs, nuts, wheat | |
| Toxins | Rapid onset vomiting and diarrhea | Heavy metals, pesticides, food toxins |
Common Transmission Routes
Fecal-Oral Transmission
- Direct contact with infected stool
- Contaminated hands, toys, surfaces
- Common in childcare centers
- Inadequate hand hygiene
Food & Water
- Contaminated drinking water
- Undercooked meats or eggs
- Unpasteurized dairy products
- Improperly stored foods
- Cross-contamination during preparation
Age-Related Risk Factors
Infants (<1 year)
- Immature immune system
- Higher body surface to weight ratio
- More rapid dehydration
- Higher metabolic rate
Toddlers (1-3 years)
- Hand-to-mouth behavior
- Daycare exposure
- Incomplete hygiene skills
- Limited communication of symptoms
School-Age (4-12 years)
- Shared facilities
- Group activities
- Variable hygiene practices
- Cafeteria food exposure
Clinical Presentation
The clinical presentation of gastroenteritis varies based on the causative agent, the age of the child, and the degree of dehydration. Recognizing the patterns of symptoms helps in assessment and management.
Diarrhea
- ≥3 loose or watery stools in 24 hours
- May contain mucus (inflammatory)
- May be bloody (bacterial, invasive)
- Duration: 2-14 days (typically)
- Character varies by cause
Vomiting
- Often precedes diarrhea (viral)
- May be projectile in young children
- Usually resolves within 1-2 days
- More prominent in norovirus
- Non-bilious (typically)
Associated Symptoms
- Fever (more common in bacterial)
- Abdominal pain/cramping
- Anorexia (decreased appetite)
- Malaise/fatigue
- Headache (dehydration)
Signs of Dehydration by Severity
| Assessment Parameter | Mild Dehydration (3-5%) |
Moderate Dehydration (6-9%) |
Severe Dehydration (≥10%) |
|---|---|---|---|
| Mental status | Alert, normal | Irritable, fatigued | Lethargic, obtunded |
| Thirst | Slightly increased | Moderately increased | Very thirsty or too lethargic to indicate |
| Heart rate | Normal | Increased | Tachycardia or bradycardia (late) |
| Pulse quality | Normal | Decreased | Weak, thready |
| Breathing | Normal | Normal to fast | Deep, rapid |
| Eyes | Normal | Slightly sunken | Deeply sunken |
| Tears | Present | Decreased | Absent |
| Mouth/tongue | Moist | Dry | Very dry |
| Skin fold | Immediately retracts | Retracts in <2 seconds | Retracts in >2 seconds |
| Capillary refill | <2 seconds | 2-3 seconds | >3 seconds |
| Extremities | Warm | Cool | Cold, mottled, cyanotic |
| Urine output | Slightly decreased | Decreased (<1 mL/kg/hr) | Minimal or absent |
| Fontanelle (infants) | Normal | Sunken | Very sunken |
Presentation Differences by Age Group
Infants (<12 months)
- More prone to rapid dehydration
- May have fewer stools but more vomiting
- Irritability or lethargy may be primary sign
- Decreased wet diapers (< 4-6/day)
- Sunken fontanelle is an important sign
- Increased respiratory rate may be present
Toddlers (1-3 years)
- May verbalize abdominal discomfort
- Refusal to drink is common
- Activity level significantly decreased
- May pull at ears (referred pain)
- Often have more pronounced diarrhea
- Can become dehydrated in 6-12 hours
School-Age (4-12 years)
- Better able to describe symptoms
- May complain of dizziness
- Headache more commonly reported
- Better able to maintain hydration
- Muscle cramps may be present
- May have more localized abdominal pain
Warning Signs & Red Flags
Immediate Medical Attention:
- Signs of severe dehydration
- Persistent vomiting (>24 hours)
- Bloody diarrhea
- Severe abdominal pain
- Bilious (green) vomit
Other Concerning Signs:
- High fever (>39°C/102.2°F)
- Altered mental status
- Infants <3 months with fever
- No urine output for >8 hours
- Inability to tolerate oral fluids
Diagnosis
The diagnosis of gastroenteritis in children is primarily clinical, based on history and physical examination. Laboratory tests are not routinely required but may be indicated in certain scenarios.
Clinical Diagnosis
History Taking
- Onset and duration of symptoms
- Frequency of diarrhea and vomiting
- Stool characteristics (watery, bloody, mucus)
- Associated symptoms (fever, pain)
- Oral intake and urine output
- Recent travel, food consumption
- Sick contacts, daycare exposure
- Recent antibiotic use
Physical Examination
- Vital signs: HR, RR, BP, temperature
- Weight (compared to baseline)
- Hydration status assessment
- Abdominal examination
- Skin turgor and mucous membranes
- Mental status and activity level
- Signs of alternate diagnoses
Laboratory Studies
When to Consider Laboratory Testing
- Moderate to severe dehydration
- Prolonged symptoms (>7 days)
- Bloody diarrhea
- Immunocompromised patient
- Recent travel to endemic areas
- Suspected outbreaks
- Severe abdominal pain
- Toxic appearance
Potential Tests
- Serum electrolytes: Assess electrolyte imbalances
- BUN/Creatinine: Evaluate renal function and dehydration
- CBC: Elevated WBC may suggest bacterial infection
- Stool studies:
- Fecal leukocytes/lactoferrin (inflammatory)
- Stool culture (bacterial pathogens)
- Stool PCR panel (multiple pathogens)
- Ova and parasites (parasitic infection)
- C. difficile toxin (antibiotic-associated)
- Urinalysis: Evaluate hydration status
Differential Diagnosis
Gastrointestinal
- Appendicitis
- Intussusception
- Inflammatory bowel disease
- Malabsorption syndromes
- Food poisoning
- Hemolytic uremic syndrome
Systemic Infections
- Urinary tract infection
- Otitis media
- Pneumonia
- Meningitis
- Sepsis
- Viral syndromes
Other Conditions
- Diabetic ketoacidosis
- Food allergies/intolerances
- Medication side effects
- Toxic ingestions
- Functional abdominal pain
- Surgical abdomen
Diagnostic Algorithm

Algorithm for the diagnosis and management of acute gastroenteritis in children
Mnemonic: “DIARRHEA” – Differential Diagnosis for Pediatric Diarrhea
Treatment
The cornerstone of treatment for pediatric gastroenteritis is rehydration and prevention of dehydration. Most cases can be managed with oral rehydration therapy and supportive care.
Key Treatment Principles
- Prevent and treat dehydration – Primary goal of therapy
- Maintain nutrition – Resume normal diet as soon as tolerated
- Avoid unnecessary medications – Most cases are self-limiting
- Prevent spread of infection – Hygiene and isolation measures
- Identify and treat complications – Monitor for clinical deterioration
Rehydration Strategies
Oral Rehydration Therapy (ORT)
First-line treatment for mild to moderate dehydration. ORT solutions contain appropriate amounts of glucose, sodium, potassium, and base to replace losses.
ORT Administration:
- Mild dehydration: 50 mL/kg over 4 hours
- Moderate dehydration: 100 mL/kg over 4 hours
- Plus replacement for ongoing losses (10 mL/kg for each diarrheal stool)
- Give small amounts frequently (5-15 mL every 5-10 minutes)
- Use spoon, syringe, or cup depending on age
Commercial ORT Solutions:
- Pedialyte®, Enfalyte®, Rehydralyte®
- Available as liquids, popsicles, or powder
- Do not dilute commercial preparations
Intravenous Rehydration (IV)
Reserved for severe dehydration or when ORT fails or is contraindicated.
Indications for IV Therapy:
- Severe dehydration (≥10% weight loss)
- Shock or impending shock
- Persistent vomiting despite ORT
- Altered mental status
- Ileus or intestinal obstruction
- Failure of ORT
IV Rehydration Approach:
- Initial bolus: 20 mL/kg isotonic solution (NS or LR)
- Repeat bolus if necessary based on clinical response
- Maintenance: Calculate based on weight plus deficit replacement
- Monitor electrolytes and adjust fluids accordingly
- Transition to oral rehydration when possible
Nutritional Management
Feeding During Gastroenteritis
Recommended Approach:
- Continue breastfeeding throughout illness
- Resume normal diet within 24 hours of starting rehydration
- No need for diluted formula
- Regular, age-appropriate diet is best
- Small, frequent feedings may be better tolerated
- Continue ORT alongside food introduction
Foods to Consider:
- Complex carbohydrates (rice, potatoes, bread)
- Lean meats, yogurt, fruits, vegetables
- Bananas (potassium-rich)
- Cereals, toast
Foods to Avoid:
- High-fat foods
- High-sugar foods and beverages
- Caffeine-containing drinks
- Large amounts of apple or pear juice
Pharmacological Management
| Medication Class | Examples | Indications | Nursing Considerations |
|---|---|---|---|
| Antimotility Agents | Loperamide (Imodium®) | Generally NOT recommended in children, especially <2 years | Contraindicated in bloody diarrhea, C. difficile infection, can mask signs of dehydration |
| Antiemetics | Ondansetron (Zofran®) | Consider for significant vomiting that prevents ORT; single dose | Monitor for side effects (headache, diarrhea); can prolong QT interval |
| Antibiotics | Azithromycin, Ciprofloxacin, Metronidazole | Only for specific bacterial etiologies when indicated (Shigella, Campylobacter, etc.) | Not routinely recommended; may prolong carrier state in Salmonella; confirm diagnosis before starting |
| Probiotics | Lactobacillus GG, Saccharomyces boulardii | May reduce duration in some cases | Moderate evidence of benefit; most effective when started early; safe |
| Zinc Supplements | Zinc sulfate, zinc acetate | WHO recommends for children in developing countries | 10-20mg/day for 10-14 days; reduces severity and duration; most beneficial in malnourished children |
| Adsorbents | Kaolin-pectin, bismuth subsalicylate | Limited evidence for efficacy | May interfere with absorption of other medications; bismuth can cause black stools |
Oral Rehydration Solution (ORS) Guide
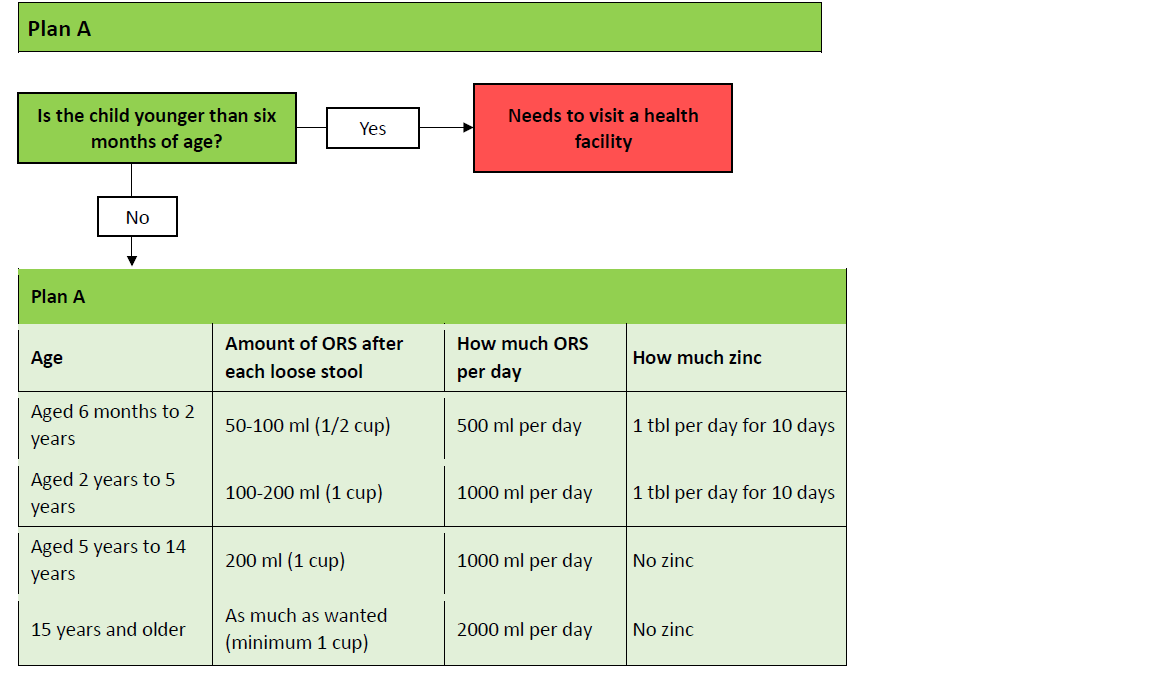
Standard guidelines for oral rehydration therapy in children with gastroenteritis
Home Management
Appropriate for:
- Mild to moderate dehydration
- Reliable caregivers
- Child accepting oral fluids
- No severe symptoms
- Ability to return if worsening
Home Care Instructions:
- ORT administration techniques
- Signs of worsening to monitor
- Proper hand hygiene and cleaning
- Return precautions
- Dietary recommendations
Hospital Management
Indications for Admission:
- Severe dehydration (≥10%)
- Failed oral rehydration
- Intractable vomiting
- Age <2 months with significant symptoms
- Underlying medical conditions
- Social concerns about home management
- Suspected surgical abdomen
- Bloody diarrhea with toxicity
Hospital Interventions:
- IV fluid therapy
- Closer monitoring of electrolytes
- Observation of clinical progress
- Specific pathogen-directed therapy
- Management of complications
Nursing Assessment
Thorough nursing assessment is essential for children with gastroenteritis to identify the severity of illness, guide interventions, and monitor response to treatment.
Initial Nursing Assessment
History Collection
- Onset and duration: When symptoms began and timeline of progression
- Characteristics of vomiting: Frequency, volume, color, contents
- Characteristics of diarrhea: Frequency, volume, consistency, presence of blood/mucus
- Fluid intake: What and how much the child has been drinking
- Urine output: Frequency, volume, color (number of wet diapers)
- Last weight measurement: To calculate potential weight loss
- Exposures: Sick contacts, recent travel, food history
- Home interventions: What has been tried and response
- Other symptoms: Fever, pain, lethargy
- Medical history: Underlying conditions, medications
Physical Assessment
- Vital signs: Temperature, heart rate, respiratory rate, blood pressure
- Weight: Compare to baseline if available
- General appearance: Activity level, responsiveness, irritability
- Mucous membranes: Moisture of lips, tongue, oral cavity
- Eyes: Sunken or not, tear production when crying
- Fontanelles: Sunken or normal in infants
- Skin turgor: Elasticity when pinched, capillary refill
- Extremities: Temperature, color, perfusion
- Abdominal assessment: Distention, tenderness, bowel sounds
- Evaluation of diaper area: Skin integrity, signs of diaper rash
Hydration Assessment Tool for Nurses
| Assessment Parameter | Mild Dehydration (3-5%) | Moderate Dehydration (6-9%) | Severe Dehydration (≥10%) |
|---|---|---|---|
| Weight loss | 3-5% of body weight | 6-9% of body weight | ≥10% of body weight |
| Mental status | Alert, normal | Irritable, fatigued | Lethargic, obtunded |
| Eyes | Normal | Slightly sunken | Deeply sunken |
| Tears | Present | Decreased | Absent |
| Mouth/tongue | Slightly dry | Dry | Very dry, parched |
| Capillary refill | <2 seconds | 2-3 seconds | >3 seconds |
| Skin turgor | Immediate recoil | Slow recoil (<2 sec) | Very delayed recoil (>2 sec) |
| Heart rate | Normal | Increased | Tachycardia or bradycardia |
| Peripheral pulses | Normal, strong | Normal to reduced | Weak, thready, may be impalpable |
| Blood pressure | Normal | Normal to slightly decreased | Decreased, may be undetectable |
| Urine output | Slightly decreased | Oliguria (<1 mL/kg/hr) | Oliguria/anuria |
| Thirst | Slight increase | Moderately increased | Very thirsty or too lethargic to indicate |
Ongoing Assessment
Frequency of Monitoring
- Mild dehydration: Every 2-4 hours
- Moderate dehydration: Every 1-2 hours
- Severe dehydration: Every 15-30 minutes until stable, then hourly
- Inpatient: As per hospital protocol, typically every 4 hours and PRN
- Home care: Instruct caregivers to monitor continuously and reassess based on symptoms
Key Parameters to Reassess
- Intake and output: Document all fluid intake and losses
- Quality and frequency of diarrhea/vomiting: Monitor for improvement
- Hydration indicators: Reassess using hydration assessment tool
- Vital signs: Trend for improvement or deterioration
- Abdominal assessment: Changes in distention or tenderness
- Response to treatment: Improvement or worsening with interventions
- Weight: Daily measurements to track fluid status
Fluid Intake Monitoring Chart
| Time | Type of Fluid | Amount Offered (mL) | Amount Consumed (mL) | Emesis (Y/N) | Diarrhea (Y/N) | Urine Output |
|---|---|---|---|---|---|---|
| 8:00 AM | ||||||
| 9:00 AM | ||||||
| 10:00 AM | ||||||
| 11:00 AM | ||||||
| 12:00 PM | ||||||
| Total | ||||||
Mnemonic: “FLUID” – Focused Assessment for Pediatric Gastroenteritis
Nursing Interventions
Effective nursing interventions for children with gastroenteritis focus on hydration, symptom management, monitoring, and education. These interventions should be tailored to the child’s age and severity of illness.
Priority Nursing Interventions
Hydration Management
- Administer oral rehydration therapy in small, frequent amounts
- Use appropriate administration method (spoon, syringe, cup) based on age
- Document all fluid intake and losses
- Assist with IV therapy if needed
- Monitor for signs of fluid overload or continued dehydration
- Measure weight daily at same time with same scale
- Reassess hydration status frequently
Nutritional Support
- Encourage early reintroduction of appropriate diet
- Support continued breastfeeding if applicable
- Offer small, frequent meals rather than large portions
- Monitor tolerance of food reintroduction
- Document nutritional intake
- Consider culturally appropriate food choices
- Avoid foods high in simple sugars
- Encourage zinc supplementation if indicated
Infection Control
- Implement contact precautions
- Practice and teach proper hand hygiene
- Use appropriate PPE when handling bodily fluids
- Properly dispose of contaminated items
- Clean and disinfect frequently touched surfaces
- Isolate symptomatic patients
- Educate family on prevention of transmission
- Ensure proper diaper changing techniques
Comfort Measures
Symptom Management
For Vomiting:
- Position child sitting upright or on side after feeding
- Administer antiemetics if prescribed
- Provide small, frequent amounts of fluids
- Avoid strong odors that may trigger nausea
- Allow for rest between fluid attempts
For Diarrhea:
- Change diapers promptly
- Apply barrier cream to protect skin
- Clean perineal area gently after each stool
- Position comfortably to avoid pressure on abdomen
- Provide easy access to bathroom for older children
For Abdominal Discomfort:
- Position for comfort
- Apply warm compress to abdomen if tolerated
- Avoid tight clothing around waist
- Assist with frequent position changes
Psychosocial Support
- Provide age-appropriate distraction during rehydration
- Encourage caregiver presence and participation
- Explain procedures at child’s developmental level
- Use therapeutic play for younger children
- Acknowledge and validate both child and caregiver concerns
- Provide quiet environment for rest
- Use positive reinforcement for successful fluid intake
- Allow for normal sleep patterns when possible
- Address caregiver anxiety with education and reassurance
Skin Integrity Management
Frequent diarrhea can quickly lead to perianal skin breakdown. Proper skin care is essential to prevent diaper dermatitis and maintain comfort.
Preventive Measures:
- Change diapers immediately after soiling
- Gently cleanse perianal area with warm water
- Avoid harsh wipes containing alcohol or fragrance
- Pat skin dry rather than rubbing
- Apply zinc oxide barrier cream with each diaper change
- Expose area to air when possible
If Irritation Occurs:
- Apply thicker layer of protective barrier
- Consider antifungal cream if candidal infection suspected
- Use soft, absorbent diapers
- Increase frequency of diaper changes
- Document skin condition and interventions
- Consider hydrocolloid dressings for severe cases
Key Nursing Procedures
Supplies Needed:
- Oral rehydration solution
- Spoon, syringe, medicine cup, or small cup
- Clean towel or bib
- Documentation form
Procedure Steps:
- Wash hands thoroughly
- Explain procedure to child and caregiver
- Position child upright or semi-reclined
- Measure appropriate amount of ORS based on age:
- Infants: 5-10 mL every 5-10 minutes
- Toddlers: 10-15 mL every 5-10 minutes
- Older children: 15-30 mL every 5-10 minutes
- Administer slowly to prevent vomiting
- Allow child to rest between sips
- Gradually increase volume as tolerated
- Document amount consumed and tolerance
Supplies Needed:
- IV administration set
- Prescribed IV fluid
- Infusion pump
- IV site care supplies
- Documentation form
Procedure Steps:
- Verify physician order for IV fluid
- Check fluid type, rate, and patient identification
- Assess IV site for patency and signs of infiltration
- Regulate flow rate according to order
- Monitor vital signs per protocol
- Assess for signs of fluid overload:
- Increased respiratory rate or effort
- Periorbital edema
- Crackles in lungs
- Document IV site condition, fluid amount, and child’s response
- Transition to oral rehydration when appropriate
Electrolyte Imbalance Management
| Electrolyte Imbalance | Signs & Symptoms | Nursing Interventions |
|---|---|---|
| Hyponatremia (Low Sodium) |
|
|
| Hypokalemia (Low Potassium) |
|
|
| Metabolic Acidosis (Bicarbonate Loss) |
|
|
Age-Specific Nursing Interventions
Infants (0-12 months):
- Use syringe or spoon for ORT administration
- Continue breastfeeding if applicable
- Monitor fontanelles for sunkenness
- Count wet diapers (goal: 4-6/day)
- Position to prevent aspiration
- More frequent skin care
Toddlers (1-3 years):
- Offer ORT in small colorful cups
- Freeze ORT into popsicles
- Use play techniques for hydration
- Involve in comfort measures
- Praise successful fluid intake
- Clear explanation of procedures
School-Age (4-12 years):
- Explain rationale for fluids
- Allow choices when possible
- Teach self-monitoring of symptoms
- Provide privacy for toileting
- Involve in goal-setting for fluid intake
- Provide age-appropriate activities
Patient Education
Effective patient education is essential for managing gastroenteritis in children. Parents and caregivers need clear instructions for home care, recognition of warning signs, and prevention of future episodes.
Home Care Instructions
Fluid Replacement
- Offer oral rehydration solution (ORS) in small amounts frequently:
- Infants: 5-10 mL every 5-10 minutes
- Toddlers: 10-15 mL every 5-10 minutes
- Older children: 15-30 mL every 5-10 minutes
- Increase amount gradually as tolerated
- Replace fluid lost with each diarrheal stool or vomiting episode
- Continue breastfeeding if applicable
- Avoid sugary drinks, juices, sports drinks, and sodas
- Freeze ORS into popsicles for older children
- Track fluid intake and output
Diet Management
- Resume normal diet within 24 hours
- Start with easily digestible foods:
- Rice, toast, crackers, bananas
- Plain pasta, potatoes
- Lean meats, yogurt
- Cooked vegetables
- Avoid high-fat or sugary foods
- Offer small, frequent meals rather than large portions
- Do not restrict food unnecessarily
- Continue formula at full strength for infants
- Avoid milk products only if they worsen symptoms
Hygiene & Skin Care
- Change diapers promptly after soiling
- Clean perianal area gently with warm water
- Apply barrier cream with each diaper change
- Pat skin dry rather than rubbing
- Allow diaper-free time when possible
- Practice thorough hand hygiene after diaper changes
- Disinfect changing surfaces
- Keep child’s hands clean
Managing Symptoms
- For fever:
- Use acetaminophen or ibuprofen as directed
- Dress in light clothing
- Keep room temperature comfortable
- For vomiting:
- Wait 30-60 minutes after vomiting before offering fluids
- Position upright or on side after feeding
- Avoid strong odors that trigger nausea
- For abdominal discomfort:
- Position for comfort
- Warm compress if tolerated
- Gentle abdominal massage
When to Seek Medical Attention
Instruct parents to call or return to healthcare provider immediately if any of these develop:
- Unable to keep down small amounts of fluid for 24 hours
- Decreased urination (fewer than 4-6 wet diapers in 24 hours)
- Blood in vomit or stool
- Green-colored (bilious) vomit
- Signs of severe dehydration:
- Extreme lethargy or unresponsiveness
- Sunken eyes or fontanelle
- No tears when crying
- Dry mouth
- Skin that stays pinched when released
- High fever (>101.5°F or 38.6°C)
- Persistent severe abdominal pain
- Swollen or distended abdomen
- Symptoms worsen or do not improve after 24-48 hours
- Irritability or excessive sleepiness
- Symptoms in infant under 3 months
- Child with underlying medical conditions
Preventing Future Episodes
Hand Hygiene
- Wash hands with soap and water for at least 20 seconds:
- After using the bathroom
- Before preparing or eating food
- After changing diapers
- After cleaning up vomit or diarrhea
- After touching animals
- Use hand sanitizer when soap is not available
- Teach proper handwashing technique to children
- Supervise young children’s handwashing
Food & Water Safety
- Cook foods thoroughly, especially meats
- Keep hot foods hot and cold foods cold
- Refrigerate leftovers promptly
- Wash fruits and vegetables thoroughly
- Use separate cutting boards for meat and produce
- Avoid unpasteurized milk and juices
- Drink clean, treated water
- Be cautious with food when traveling
Home Environment
- Clean and disinfect frequently touched surfaces
- Use bleach solution (1:10 dilution) for cleaning contaminated areas
- Wash soiled linens and clothes in hot water
- Dispose of diapers properly
- Keep bathroom areas clean, especially toilets
- Avoid sharing personal items
- Isolate sick family members when possible
- Keep children home from school/daycare until 24-48 hours after symptoms resolve
Educational Resources for Families
Recommended Resources:
- American Academy of Pediatrics: HealthyChildren.org
- CDC: Handwashing in Childcare Settings
- KidsHealth: Information on Dehydration and Gastroenteritis
- WHO: Oral Rehydration Salts (ORS)
- Family-friendly videos on handwashing and food safety
When to Schedule Follow-up:
- Symptoms persist beyond 7 days
- Child required IV hydration
- Weight loss not regained within 1-2 weeks
- Child has underlying medical conditions
- Recurrent episodes of gastroenteritis
- Delayed return to normal activity
