Drug Deaddiction Programs in India: A Community Health Nursing Perspective
Table of Contents
Introduction
Drug addiction represents one of the most pressing public health challenges in India today, affecting individuals across all socioeconomic strata. As nurses working in community health settings, understanding the scope, implementation, and nursing implications of drug deaddiction programs is essential for effective practice. These programs not only address the medical aspects of substance use disorders but also embrace the social, psychological, and cultural dimensions that influence addiction.
The Constitution of India, under Article 47, enjoins that the state shall endeavor to bring about prohibition of the consumption of intoxicating drinks and drugs that are injurious to health. Based on this constitutional mandate, the Government of India has implemented various initiatives to combat drug addiction through a comprehensive approach that includes prevention, treatment, and rehabilitation.
Focus Word: Deaddiction
Throughout these notes, we will be focusing on deaddiction programs – the systematic approaches and interventions designed to help individuals overcome substance dependence and reintegrate into society. Effective deaddiction requires a multidisciplinary approach where community health nurses play a pivotal role in bridging clinical care with community-based support.

Fig. 1: Community health nurse providing counseling to a patient in a deaddiction center
Drug Addiction Statistics in India
Understanding the magnitude of substance abuse in India is crucial for contextualizing the importance of deaddiction programs. Recent data reveals an alarming trend in substance use across the country:
| Substance | Estimated Users (in millions) | Users Requiring Treatment | Treatment Gap |
|---|---|---|---|
| Alcohol | 151.0 | 57.0 million | ≈75% |
| Cannabis | 31.0 | 7.2 million | ≈75% |
| Opioids | 19.0 | 7.7 million | ≈75% |
Table 1: Substance use statistics in India (Source: National Survey on Extent and Pattern of Substance Use in India, 2019)
According to the World Drug Report 2024, the number of people using drugs globally reached 292 million in 2022, representing a 20 percent increase over the past decade. India’s contribution to these statistics is significant, with approximately 7.5 crore individuals suffering from different substance use disorders.
The National Survey on Extent and Pattern of Substance Use in India (2019) reported that alcohol is the most commonly used psychoactive substance, followed by cannabis and opioids. Only about 25% of those who tried to quit received any form of treatment, highlighting a substantial treatment gap that community health nurses must address through deaddiction initiatives.
Drug Deaddiction Programs in India
Historical Development
India’s approach to addressing substance use disorders has evolved significantly over the decades. The initial focus was primarily on punitive measures through legal frameworks like the Narcotic Drugs and Psychotropic Substances (NDPS) Act of 1985. However, recognizing that addiction is a complex health and social issue, the government gradually shifted toward a more comprehensive strategy that balances supply reduction with demand reduction initiatives.
Supply Reduction vs. Demand Reduction
- Supply Reduction: Activities aimed at reducing the availability of illicit drugs within the country (under the purview of the Narcotics Control Bureau and Department of Revenue)
- Demand Reduction: Activities focused on awareness building, treatment, and rehabilitation of individuals with substance use disorders (under the Ministry of Social Justice and Empowerment and Ministry of Health and Family Welfare)
Drug De-addiction Programme (DDAP)
Following recommendations from a Cabinet Sub-Committee, the Drug De-addiction Programme (DDAP) was established in 1988 under the Ministry of Health and Family Welfare, Government of India. DDAP represents one of the earliest systematic approaches to addressing substance use disorders in India through the healthcare system.
DDAP Objectives
- To provide affordable, easily accessible, and evidence-based treatment for all substance use disorders through government healthcare facilities
- To build the capacities of healthcare staff in recognition and management of substance use disorders
- To establish specialized deaddiction centers across the country
- To develop standardized protocols for intervention and treatment
Under DDAP, financial grants are provided for augmenting treatment facilities in selected Central Government Hospitals/Institutions and Government Hospitals/Institutions, particularly in North-Eastern states. The program established the National Drug Dependence Treatment Centre (NDDTC) in Ghaziabad as a national nodal center under the All India Institute of Medical Sciences (AIIMS), New Delhi.
The DDAP has also initiated the Drug Treatment Clinics (DTC) scheme, which has established 27 DTCs across different states. More recently, the program has been expanded to include RML Hospital (New Delhi), AIIMS Bhubaneshwar, and CIP Ranchi.
National Action Plan for Drug Demand Reduction (NAPDDR)
The National Action Plan for Drug Demand Reduction (NAPDDR) is a centrally sponsored scheme implemented by the Ministry of Social Justice and Empowerment. It integrates various existing programs related to drug demand reduction and implements them in a holistic manner for greater impact.
Major Objectives of NAPDDR
- Create awareness and educate people about the ill effects of substance abuse
- Develop human resources and build capacity for providing services in deaddiction centers
- Provide for a whole range of community-based services for identification, motivation, counseling, deaddiction treatment, aftercare, and rehabilitation
- Establish and support Integrated Rehabilitation Centres for Addicts (IRCAs)
- Support innovative interventions and pilot projects addressing emerging trends
The Ministry provides financial assistance to Non-Governmental Organizations (NGOs) for setting up and running Integrated Rehabilitation Centre for Addicts (IRCAs). Currently, more than 400 IRCAs are supported by the Ministry across the country.
Nasha Mukt Bharat Abhiyaan (NMBA)
Launched on August 15, 2020, the Nasha Mukt Bharat Abhiyaan (NMBA) or “Addiction-Free India Campaign” represents India’s flagship program for addressing drug addiction. It initially focused on 272 districts identified as most vulnerable in terms of drug usage, based on findings from the Comprehensive National Survey and inputs from the Narcotics Control Bureau.
The NMBA adopts a three-pronged approach:
- Supply Curb: Led by the Narcotics Control Bureau
- Outreach and Awareness: Led by the Ministry of Social Justice and Empowerment
- Treatment: Led by the Ministry of Health and Family Welfare
The campaign emphasizes community participation and leverages local resources to create a mass movement against drug abuse. Educational institutions, particularly schools and colleges, are actively involved in organizing activities such as online seminars, webinars, essay writing, painting competitions, signature campaigns, and oath-taking ceremonies to raise awareness about substance abuse.
Implementation Framework
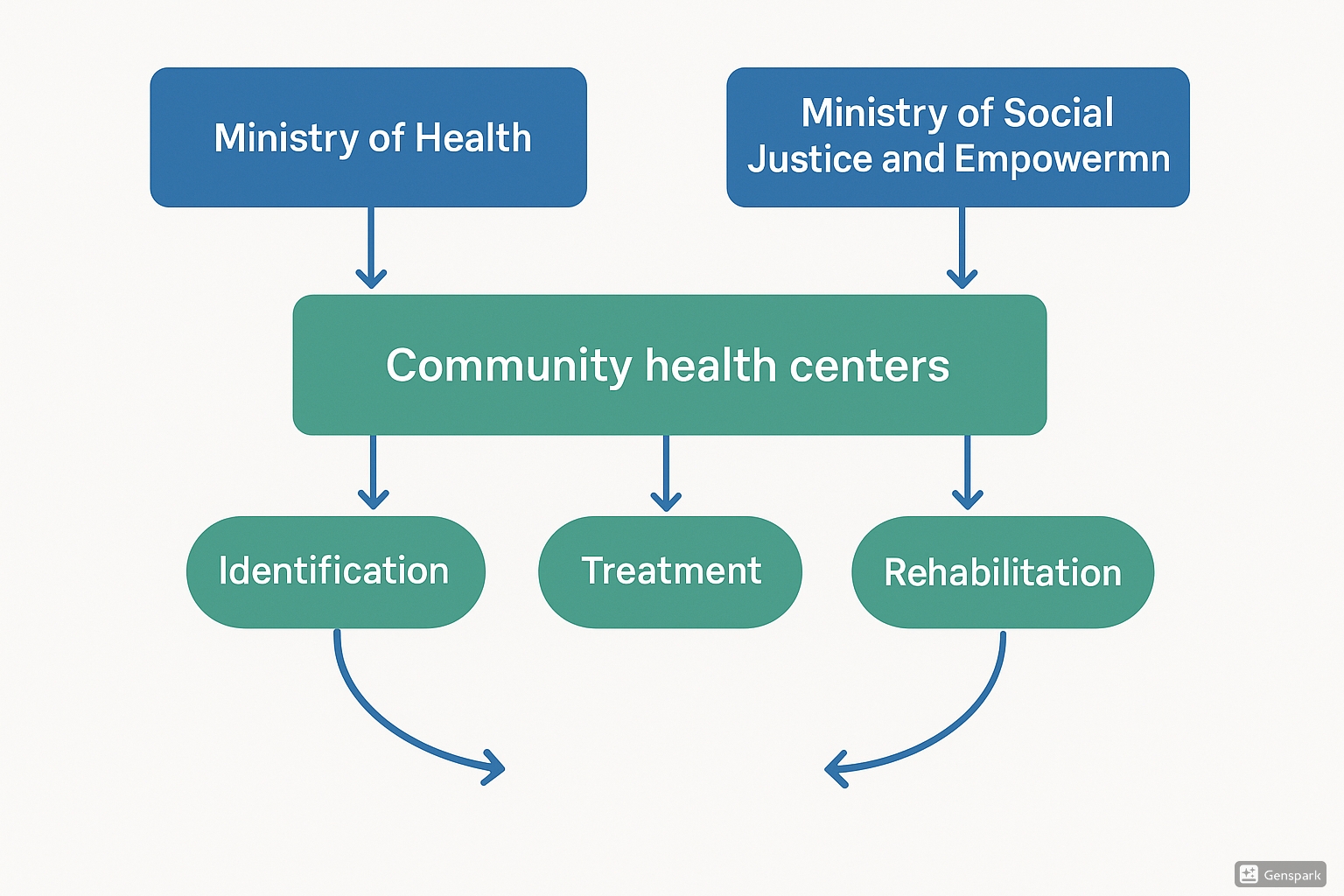
Fig. 2: Drug deaddiction framework in India showing key stakeholders and service flow
The implementation of deaddiction programs in India follows a multi-tiered approach, involving various stakeholders at the national, state, and district levels. Each level has specific responsibilities and mechanisms for coordination:
| Level | Key Stakeholders | Responsibilities |
|---|---|---|
| National Level |
– Ministry of Health and Family Welfare – Ministry of Social Justice and Empowerment – Narcotics Control Bureau – National Drug Dependence Treatment Centre |
– Policy formulation – Resource allocation – Program design – National monitoring |
| State Level |
– State Health Department – Social Welfare Department – State Abhiyaan Committee |
– Program implementation – Resource distribution – Monitoring district activities – Providing support and guidance |
| District Level |
– District Collector/Magistrate – Chief Medical Officer – NGOs – District Level Nasha Mukt Committees |
– Direct implementation – Community engagement – Selecting master volunteers – Running deaddiction centers |
| Community Level |
– Community Health Centers – Primary Health Centers – Community Drug Treatment Clinics – Community health workers and nurses |
– Case identification – Referrals – Outpatient services – Follow-up and rehabilitation |
Table 2: Multi-tiered implementation framework for drug deaddiction programs in India
For the Nasha Mukt Bharat Abhiyaan specifically, District Level Nasha Mukt Committees are formed under the chairmanship of the District Commissioner/Magistrate. These committees comprise representatives from stakeholder ministries such as Health, Education, Women & Child Development, as well as the Narcotics Control Bureau, Police, and organizations working in the field of deaddiction.
Role of Community Health Nursing
Community health nurses play a pivotal role in the successful implementation of deaddiction programs. Their position at the interface between healthcare systems and communities makes them ideally placed to address substance use disorders through a public health approach.
Key Responsibilities
| Domain | Responsibilities |
|---|---|
| Prevention |
– Conducting awareness programs in communities, schools, and workplaces – Identifying high-risk individuals and groups – Implementing early intervention strategies – Facilitating health education sessions on substance abuse |
| Screening and Assessment |
– Conducting screenings using standardized tools – Performing comprehensive assessments of individuals with suspected SUDs – Identifying comorbid physical and mental health conditions – Evaluating family and social support systems |
| Treatment and Referral |
– Providing basic counseling and motivational interviewing – Managing mild withdrawal symptoms – Facilitating referrals to specialized deaddiction services – Coordinating care between different service providers |
| Follow-up and Rehabilitation |
– Providing home-based follow-up care – Monitoring treatment adherence and progress – Supporting relapse prevention efforts – Facilitating reintegration into family and community |
| Community Mobilization |
– Building community support for deaddiction initiatives – Engaging community leaders and influencers – Creating supportive environments for recovery – Reducing stigma associated with substance use disorders |
Table 3: Key responsibilities of community health nurses in drug deaddiction programs
Community Assessment for Substance Use
Community health nurses must conduct thorough assessments to understand the patterns and determinants of substance use in their communities. This information is crucial for designing targeted deaddiction interventions.
Community Assessment Framework: ASPECT
- Availability – Assess the types and accessibility of substances in the community
- Social factors – Identify social norms, peer influences, and cultural attitudes toward substance use
- Prevalence – Determine the extent of substance use in different demographic groups
- Environmental factors – Evaluate living conditions, unemployment, and neighborhood characteristics
- Community resources – Map existing services, support systems, and potential partners
- Trends – Monitor changing patterns of substance use over time
Intervention Strategies
Community health nurses employ various evidence-based strategies to address substance use disorders at different levels of prevention:
| Prevention Level | Intervention Strategies | Nursing Activities |
|---|---|---|
| Primary Prevention (Before substance use begins) |
– School-based education programs – Community awareness campaigns – Life skills training – Family-based interventions |
– Conduct educational sessions in schools and colleges – Organize community awareness events – Facilitate life skills workshops – Engage families in prevention efforts |
| Secondary Prevention (Early identification and intervention) |
– Screening programs – Brief interventions – Motivational interviewing – Referrals to specialized services |
– Conduct routine screenings in healthcare settings – Deliver brief interventions for at-risk individuals – Apply motivational interviewing techniques – Make appropriate referrals to deaddiction centers |
| Tertiary Prevention (Treatment and rehabilitation) |
– Deaddiction treatment support – Relapse prevention – Family support and counseling – Social reintegration |
– Support medication adherence – Provide follow-up care in the community – Conduct family counseling sessions – Facilitate access to vocational rehabilitation |
Table 4: Prevention levels and intervention strategies for community health nurses
Treatment Approaches
Community-Based Treatment
Community-based treatment approaches bring deaddiction services closer to patients in their local environment. This model has several advantages over traditional institutional care:
| Advantages | Implementation Aspects |
|---|---|
|
– Greater accessibility for patients – Less disruption to family and work life – Reduced stigma around treatment – Lower costs compared to inpatient care – Integration with existing community resources – Better continuity of care |
– Utilization of existing community spaces – Collaboration with local healthcare providers – Involvement of community leaders and influencers – Leveraging family and social support systems – Creating networks of service providers – Training community volunteers as recovery supporters |
In India, various approaches have been utilized for providing community-based treatment of substance use disorders:
- Community Outreach Clinics: Regular clinics held at community health centers or civil hospitals
- Special Outreach Outpatient Clinics: Services provided in premises arranged by village panchayats
- Camp Approach: Short-term camps (7-10 days) in villages or localities for acute withdrawal management
- Community Drug Treatment Clinics (CDTCs): Specialized clinics providing comprehensive services in high-risk areas
Community Drug Treatment Clinics (CDTCs)
The Community Drug Treatment Clinic model, pioneered by the National Drug Dependence Treatment Centre (NDDTC), AIIMS, represents an effective approach to delivering deaddiction services in community settings.
Key Features of CDTCs
- Location: Established in areas with high prevalence of substance use disorders
- Infrastructure: Utilizes existing community spaces (e.g., community halls, local hospitals)
- Staffing: Operates with minimal staff (doctors visit twice weekly, nursing staff daily)
- Services: Provides both pharmacological and non-pharmacological interventions
- Approach: Follows an open-door policy without requiring appointments
- Integration: Links with other healthcare services in the community
CDTCs shift the focus from long-term inpatient care for a few to low-intensity outpatient treatment for many. This approach helps bridge the substantial treatment gap for substance use disorders in India.
Pharmacological Interventions
Pharmacological treatments are an essential component of comprehensive deaddiction programs. Community health nurses need to understand these medications, their uses, and potential side effects to provide appropriate support and monitoring.
| Substance Type | Medication | Purpose | Nursing Considerations |
|---|---|---|---|
| Alcohol | Benzodiazepines | Management of withdrawal symptoms | Monitor for respiratory depression, sedation, and fall risk |
| Disulfiram | Deterrent therapy | Educate about alcohol-disulfiram reaction, ensure compliance | |
| Naltrexone | Reduces cravings | Monitor liver function, assess for side effects | |
| Opioids | Buprenorphine | Opioid substitution therapy | Ensure proper dosing, monitor for misuse |
| Methadone | Opioid substitution therapy | Observe for respiratory depression, monitor QT prolongation | |
| Naltrexone | Prevents euphoric effects | Ensure opioid-free period before starting, monitor compliance | |
| Tobacco | Nicotine replacement therapy, Bupropion, Varenicline | Reduces withdrawal symptoms and cravings | Monitor for neuropsychiatric symptoms, assess effectiveness |
| Cannabis | Symptomatic treatment | Management of withdrawal symptoms | Monitor for sleep disturbances, anxiety, and irritability |
Table 5: Pharmacological interventions in substance use disorder treatment
Challenges and Best Practices
Despite significant efforts in implementing deaddiction programs, several challenges persist in the Indian context. Community health nurses must be aware of these challenges and adopt best practices to overcome them:
| Challenge | Best Practice |
|---|---|
| High treatment gap (75% of individuals with SUDs do not receive treatment) | Implement proactive case-finding in communities and establish easily accessible outpatient services like CDTCs |
| Stigma associated with substance use disorders | Conduct community awareness programs emphasizing that addiction is a health condition, not a moral failing |
| Limited availability of trained healthcare professionals | Leverage task-sharing approaches by training community volunteers and lay counselors to support deaddiction efforts |
| Overemphasis on inpatient treatment models | Promote community-based and outpatient treatment approaches that are more accessible and cost-effective |
| Poor integration with primary healthcare | Incorporate substance use screening and basic interventions into routine primary healthcare services |
| Limited follow-up and aftercare | Establish community-based recovery support systems and use mobile health technologies for follow-up |
| Addressing comorbid conditions | Implement integrated screening and treatment approaches for mental and physical health conditions |
Table 6: Challenges and best practices in drug deaddiction programs
Community health nurses can play a pivotal role in addressing these challenges by serving as advocates for evidence-based approaches, facilitating coordination between different stakeholders, and ensuring continuity of care for individuals with substance use disorders.
Mnemonics for Nursing Practice
Mnemonics can help community health nurses remember key concepts and approaches in substance use deaddiction programs:
SUBSTANCE: Screening Approach for Community Nurses
- Specific substance use patterns (type, frequency, amount)
- Understanding of consequences by the patient
- Behavioral changes associated with use
- Social impact (family, work, legal issues)
- Tolerance and withdrawal symptoms
- Attempts to quit in the past
- Need for treatment (patient’s perception)
- Co-occurring health conditions
- Environment and support system
RECOVERY: Supporting Recovery in Community Settings
- Relationship building with patient and family
- Education about substance use and recovery
- Coping skills development
- Ongoing support and follow-up
- Validation of progress and challenges
- Employment and social reintegration
- Relapse prevention strategies
- Yield positive reinforcement for achievements
DEADDICTION: Nursing Approach to Treatment
- Detoxification support and monitoring
- Education about addiction as a disease
- Assessment of physical and mental health needs
- Development of personalized care plans
- Daily living skills enhancement
- Integration of family in treatment
- Counseling and psychological support
- Treatment adherence promotion
- Identification of triggers and risk factors
- Ongoing recovery maintenance
- Networking with community resources
Case Study: Community Nurse’s Role in Drug Deaddiction
Case Scenario: Community Drug Treatment Clinic in Urban Slum
Background: A community health nurse named Meera works in a Community Drug Treatment Clinic (CDTC) established in an urban slum area with high prevalence of substance use disorders, particularly alcohol and opioids.
Assessment: Meera conducted a community assessment using the ASPECT framework and identified high availability of illicit substances, unemployment as a social factor, high prevalence among young males, cramped living conditions, limited existing services, and increasing opioid use trends.
Intervention: Based on the assessment, Meera developed a multi-level intervention strategy:
- Primary Prevention: Organized awareness programs in local schools and community gatherings
- Secondary Prevention: Established a screening booth at the community health center for early identification
- Tertiary Prevention: Provided home-based follow-up for patients undergoing deaddiction treatment
Implementation: Meera coordinated with the District Level Nasha Mukt Committee to secure resources for the CDTC. She trained community volunteers to serve as “recovery champions” who could support patients in between clinic visits.
Challenges: Meera encountered resistance from local alcohol vendors and stigma among community members. Some patients also faced pressure from peers to continue substance use.
Solutions: Meera engaged community leaders to address resistance, conducted stigma reduction workshops, and established peer support groups for patients to counter negative peer influence.
Outcomes: After one year, the CDTC had registered 150 patients, with 60% showing significant reduction in substance use. Community awareness had increased, and more families were seeking help for their members with SUDs.
Learning Points:
- Community engagement is crucial for successful deaddiction programs
- Addressing environmental and social factors is as important as individual treatment
- Training community resources (volunteers) can extend the reach of professional services
- Continuous follow-up is essential for maintaining treatment gains
Additional Resources
Government Portals and Programs
- Ministry of Social Justice and Empowerment: https://socialjustice.gov.in
- Ministry of Health and Family Welfare: https://mohfw.gov.in
- Nasha Mukt Bharat Abhiyaan: https://nmba.dosje.gov.in
- National Drug Dependence Treatment Centre: https://nddtc.aiims.edu
Training Resources for Community Health Nurses
- Screening, Brief Intervention and Referral to Treatment (SBIRT) training
- Motivational Interviewing techniques for substance use disorders
- Community-based rehabilitation approaches for addiction
- Family counseling for substance use disorders
Assessment Tools
- AUDIT (Alcohol Use Disorders Identification Test): Screening tool for alcohol use disorders
- DAST (Drug Abuse Screening Test): Screening tool for drug use disorders
- ASSIST (Alcohol, Smoking and Substance Involvement Screening Test): WHO-developed tool for screening various substances
- CRAFFT: Screening tool specifically designed for adolescents
Conclusion
Drug deaddiction programs in India represent a comprehensive approach to addressing substance use disorders through prevention, treatment, and rehabilitation. The evolution of these programs from primarily institutional models to community-based approaches reflects a growing recognition of addiction as a complex health and social issue requiring multifaceted interventions.
Community health nurses are integral to the success of these deaddiction programs, serving as bridges between healthcare systems and communities. Their roles span across prevention, screening, treatment support, and rehabilitation, making them uniquely positioned to address the substantial treatment gap for substance use disorders in India.
The community-based approach to deaddiction, exemplified by models like Community Drug Treatment Clinics, offers a promising strategy for expanding access to evidence-based treatment. By leveraging existing community resources, engaging families and communities, and providing services closer to where people live, these approaches can help overcome barriers related to accessibility, affordability, and stigma.
As India continues to strengthen its response to substance use disorders through initiatives like the Nasha Mukt Bharat Abhiyaan, community health nurses must equip themselves with the knowledge, skills, and attitudes needed to effectively contribute to these efforts. By understanding the complex nature of addiction, employing evidence-based approaches, and engaging communities as partners in prevention and treatment, nurses can play a transformative role in creating a healthier, addiction-free society.
References
- Ministry of Health and Family Welfare. (n.d.). Drug De-Addiction Programme (DDAP). https://mohfw.gov.in/sites/default/files/drugs%20deaddiction%20programme.pdf
- Ministry of Social Justice and Empowerment. (2024). National Action Plan for Drug Demand Reduction. https://socialjustice.gov.in/schemes/42
- Nasha Mukt Bharat Abhiyaan. (n.d.). About Us. https://nmba.dosje.gov.in/content/about-us
- Ambekar, A., Agrawal, A., Rao, R., et al. (2019). Magnitude of Substance Use in India. New Delhi: Ministry of Social Justice and Empowerment, Government of India.
- World Health Organization. (2024). World Drug Report 2024. United Nations Office on Drugs and Crime.
- Dhawan, A., Rao, R., Ambekar, A., et al. (2017). Treatment of substance use disorders through the government health facilities: Developments in the Drug De-addiction Programme of Ministry of Health and Family Welfare, Government of India. Indian Journal of Psychiatry, 59(3), 380-384.
- Rao, R., Varshney, M., Singh, S., Agrawal, A., & Ambekar, A. (2021). Improving Treatment of Substance Use Disorders through Community-based Drug Treatment Clinics. Indian Journal of Community Medicine, 46(3), 401-404.
- Murthy, P., Manjunatha, N., Subodh, B. N., Chand, P. K., & Benegal, V. (2010). Substance use and addiction research in India. Indian Journal of Psychiatry, 52(Suppl1), S189-S199.
- Chavan, B. S., & Gupta, N. (2004). Camp approach: A community-based treatment for substance dependence. American Journal on Addictions, 13, 324-325.
- Prevention of substance use disorders in the community and workplace settings. (2018). Indian Journal of Social Psychiatry, 34(5), S36-S45.
