Drugs Used in Labor and Delivery
Comprehensive Guide for Nursing Students
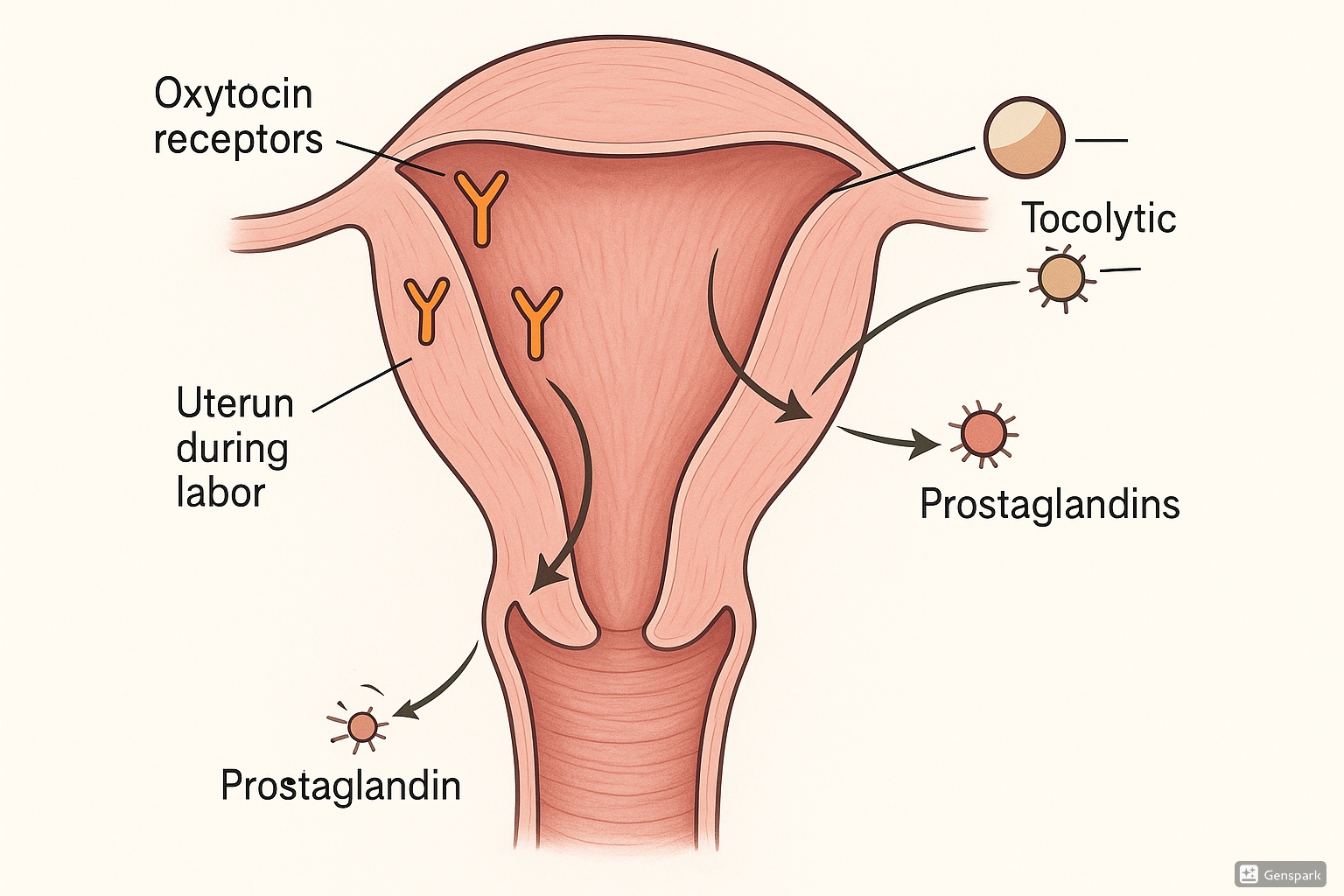
Medical illustration showing drug actions on the uterus during labor
Table of Contents
Introduction to Drugs Used in Labor
Labor and delivery represent critical periods in pregnancy where pharmacological interventions may be necessary to optimize maternal and fetal outcomes. Drugs used during labor and delivery can be broadly categorized based on their intended effects: stimulating uterine contractions (uterotonics), inhibiting contractions (tocolytics), or providing pain relief (analgesics).
The selection of appropriate medications requires careful consideration of the clinical context, including gestational age, maternal and fetal status, and specific indications such as labor induction, augmentation, preterm labor, or postpartum hemorrhage prevention.
Clinical Pearl
Most drugs used in labor cross the placenta to some degree. The potential fetal effects should always be considered when selecting medications, particularly when used outside their standard indications.
Uterotonic Drugs
Uterotonic drugs stimulate uterine contractions and are used for labor induction, augmentation of labor, management of postpartum hemorrhage, and control of bleeding after delivery. These medications act on the smooth muscle of the uterus to increase the frequency and strength of contractions.
Oxytocin (Pitocin)
Oxytocin is a peptide hormone naturally produced in the hypothalamus and released by the posterior pituitary gland. Synthetic oxytocin is one of the most commonly used medications in obstetrics.
| Characteristic | Description |
|---|---|
| Mechanism of Action | Binds to oxytocin receptors on uterine myometrial cells, stimulating calcium release and increasing the frequency and force of uterine contractions |
| Indications |
– Labor induction – Labor augmentation – Prevention and treatment of postpartum hemorrhage – Management of incomplete or inevitable abortion |
| Dosage |
Labor induction/augmentation: Initial dose 0.5-2 mU/min IV, increased gradually every 15-60 minutes until adequate labor pattern established. Maximum dose usually 20-40 mU/min. Postpartum hemorrhage: 10-40 units in 1000 mL IV fluid at 125-200 mL/hour |
| Onset & Duration |
Onset: Immediate IV, 3-5 minutes IM Duration: 1 hour after discontinuation |
| Adverse Effects |
– Water intoxication (antidiuretic effect) – Uterine hyperstimulation – Uterine rupture – Fetal distress due to decreased uteroplacental perfusion – Maternal hypertension, tachycardia, arrhythmias – Postpartum hemorrhage (paradoxically) due to uterine atony after prolonged use |
Memory Aid: The “O-X-Y” Rule
O – Only administer with continuous fetal monitoring
X – Xtra caution with grand multiparity (5+ previous births)
Y – Yield (stop) if contractions occur less than 2 minutes apart
Nursing Considerations
- Administer via controlled infusion pump only
- Continuous electronic fetal monitoring required
- Maintain IV access throughout administration
- Monitor vital signs every 15 minutes during active labor
- Document uterine activity and fetal response to contractions
- Have emergency medications available (tocolytics) to reverse uterine hyperstimulation
- Position patient in left lateral position to optimize uteroplacental perfusion
Prostaglandins
Prostaglandins are lipid compounds that have various hormone-like effects. In obstetrics, they are primarily used for cervical ripening and labor induction.
| Agent | Formulation | Dosing | Primary Use |
|---|---|---|---|
| Dinoprostone (PGE2) (Cervidil, Prepidil) |
– Vaginal insert (10 mg) – Endocervical gel (0.5 mg) |
Insert: One 10 mg insert vaginally for up to 12 hours Gel: 0.5 mg intracervically, may repeat every 6 hours up to maximum 1.5 mg/24 hours |
Cervical ripening and labor induction when cervix is unfavorable (low Bishop score) |
| Misoprostol (PGE1) (Cytotec) |
– Oral tablet (100-200 μg) – Vaginal tablet (25-50 μg) |
Vaginal: 25 μg every 3-6 hours Oral: 50-100 μg every 4-6 hours |
– Cervical ripening – Labor induction – Management of postpartum hemorrhage |
Memory Aid: “PRIME” the Cervix
Prostaglandins
Ripen the cervix by
Increasing collagenase
Modifying tissue consistency, and
Effacing before dilation begins
Warning
Prostaglandins are contraindicated in patients with:
- Previous cesarean delivery or major uterine surgery (increased risk of uterine rupture)
- Placenta previa or unexplained vaginal bleeding
- Active herpes infection
- History of hypersensitivity to prostaglandins
Clinical Pearl
Misoprostol (PGE₁) is generally more potent than dinoprostone (PGE₂) and has a higher risk of uterine hyperstimulation. However, it is significantly less expensive and more stable at room temperature, which makes it more accessible in low-resource settings.
Nursing Considerations
- Store dinoprostone refrigerated until just before use
- Monitor fetal heart rate and uterine activity continuously during administration
- Dinoprostone insert can be removed quickly if hyperstimulation occurs
- Have emergency tocolytics available
- Monitor for fever, which can be a side effect of prostaglandins
- Assess cervical change according to facility protocol
Ergot Alkaloids
Ergot alkaloids are primarily used for the prevention and treatment of postpartum hemorrhage due to their potent and sustained uterotonic effects.
| Agent | Mechanism | Dosing | Key Features |
|---|---|---|---|
| Methylergonovine (Methergine) |
Direct stimulation of smooth muscle causing sustained tetanic contraction of the uterus |
IM: 0.2 mg after delivery of placenta, can repeat every 2-4 hours Oral: 0.2 mg every 6-8 hours for up to 7 days |
– Causes sustained uterine contraction – Also causes vasoconstriction – Not used for labor induction/augmentation – Only for postpartum use |
Warning
Ergot alkaloids are contraindicated in patients with:
- Hypertension
- Preeclampsia/eclampsia
- Cardiovascular disease
- Before delivery of placenta
Memory Aid: “ERGOT = AFTER”
Ergot alkaloids
Restricted until
Giving birth is complete
Only appropriate
To prevent postpartum bleeding
Nursing Considerations
- Monitor blood pressure every 15 minutes for 2 hours after administration
- Observe for signs of peripheral vasospasm or ischemia
- Check uterine firmness and vaginal bleeding
- NEVER administer IV (severe hypertension can result)
- Store protected from light
Tocolytic Drugs
Tocolytic drugs inhibit uterine contractions and are used to delay preterm birth. The primary goal is to allow time for corticosteroid administration to enhance fetal lung maturity and/or transfer the mother to a facility equipped for preterm neonatal care.
Clinical Pearl
Tocolytics typically delay delivery by only 48-72 hours, which is sufficient for corticosteroid administration but rarely alters long-term neonatal outcomes. They’re most effective between 24-34 weeks of gestation.
Beta-Agonists
Beta-agonists relax uterine smooth muscle by stimulating β₂-adrenergic receptors, increasing intracellular cAMP.
| Agent | Dosing | Adverse Effects |
|---|---|---|
| Terbutaline |
Acute tocolysis: 0.25 mg SC every 3-4 hours as needed IV: 2.5-10 μg/min, titrated to effect |
– Maternal tachycardia – Pulmonary edema – Hyperglycemia – Hypokalemia – Tremors – Chest pain/palpitations – Fetal tachycardia |
| Ritodrine (No longer available in US) |
IV: Initial 50 μg/min, increase by 50 μg/min every 10 min up to 350 μg/min max |
– Similar to terbutaline – Myocardial ischemia – Maternal death (rare) |
Warning
The FDA has issued warnings against long-term use of terbutaline for prevention of preterm labor due to potential for serious maternal heart problems and death. It should not be used for more than 48-72 hours.
Nursing Considerations
- Monitor maternal vital signs, especially heart rate and respiratory rate
- Monitor fetal heart rate continuously during IV administration
- Check maternal blood glucose levels
- Monitor fluid balance carefully to prevent pulmonary edema
- Assess for chest pain, dyspnea, or palpitations
- Have cardioselective beta-blockers available (e.g., esmolol) for severe tachycardia
Calcium Channel Blockers
Calcium channel blockers inhibit calcium influx into smooth muscle cells, reducing uterine contractility. Nifedipine is the most commonly used agent in this class for tocolysis.
| Agent | Dosing | Adverse Effects |
|---|---|---|
| Nifedipine |
Loading dose: 10-20 mg PO, then 10-20 mg every 4-6 hours Maintenance: Extended-release 30-60 mg daily |
– Hypotension – Headache – Facial flushing – Dizziness – Peripheral edema – Transient decrease in fetal heart rate variability |
Memory Aid: “CALM the Uterus”
Calcium channel blockers
Arrest contractions by
Limiting calcium entry
Maintaining uterine relaxation
Clinical Pearl
Compared to beta-agonists, nifedipine has fewer maternal side effects and appears to have better neonatal outcomes. It has largely replaced beta-agonists as a first-line tocolytic in many institutions.
Nursing Considerations
- Monitor blood pressure regularly
- Do not administer sublingual nifedipine for tocolysis (risk of severe hypotension)
- Avoid concurrent use with magnesium sulfate (increased risk of hypotension)
- Check compatibility with other medications
- Position patient in left lateral position if hypotension occurs
Magnesium Sulfate
Magnesium sulfate acts as a calcium antagonist and reduces uterine contractility. It is also the drug of choice for seizure prophylaxis in preeclampsia and eclampsia.
| Indication | Dosing | Monitoring |
|---|---|---|
| Tocolysis |
Loading dose: 4-6 g IV over 20-30 minutes Maintenance: 1-4 g/hour IV continuous infusion |
– Therapeutic serum level: 4-8 mEq/L (tocolysis) – Therapeutic serum level: 4-7 mEq/L (preeclampsia) – Loss of patellar reflexes: 8-12 mEq/L – Respiratory depression: >12 mEq/L – Cardiac arrest: >25 mEq/L |
| Preeclampsia/ Eclampsia |
Loading dose: 4-6 g IV over 15-20 minutes Maintenance: 1-2 g/hour IV continuous infusion |
|
| Fetal Neuroprotection |
Loading dose: 4 g IV over 30 minutes Maintenance: 1 g/hour IV until delivery |
– Most effective when given at least 4 hours before anticipated delivery – Used between 24-32 weeks gestation |
Memory Aid: “MAGS Monitoring”
Magnesium levels >12 = respiratory arrest
Absent reflexes around 8-10
Good therapeutic range = 4-8
Seizure control at 4-7
Clinical Pearl
Beyond its tocolytic effects, magnesium sulfate has been shown to have neuroprotective effects for the fetus when given before extremely preterm birth, reducing the risk of cerebral palsy.
Warning
The FDA recommends against using magnesium sulfate for more than 5-7 days to stop preterm labor due to risk of low calcium levels and bone problems in the developing fetus.
Nursing Considerations
- Assess deep tendon reflexes, respiratory rate, and urine output hourly
- Keep calcium gluconate ready as antidote (1 g IV)
- Monitor serum magnesium levels every 4-6 hours
- Adjust dosage based on serum levels and clinical assessment
- Caution with concurrent CNS depressants
- Reduce dose in patients with renal impairment
Prostaglandin Inhibitors (NSAIDs)
NSAIDs inhibit cyclooxygenase enzymes, reducing prostaglandin synthesis that is necessary for uterine contractions.
| Agent | Dosing | Considerations |
|---|---|---|
| Indomethacin |
Loading dose: 50-100 mg PO or PR Maintenance: 25-50 mg PO every 6 hours for up to 48 hours |
– Most effective <32 weeks gestation – Use limited to 48-72 hours – Risk of premature closure of ductus arteriosus (>32 weeks) – Risk of oligohydramnios with prolonged use – Contraindicated in patients with renal disease, asthma, coagulation disorders |
Memory Aid: “INDO-NO-GO after 32”
Remember that indomethacin is generally avoided after 32 weeks gestation due to increased risk of premature closure of the ductus arteriosus.
Nursing Considerations
- Monitor amniotic fluid volume (AFI) daily
- Discontinue if oligohydramnios develops
- Monitor fetal cardiac function and ductus arteriosus by ultrasound if available
- Assess for GI distress; administer with food if possible
- Monitor for maternal edema or decreased urine output
Oxytocin Antagonists
Oxytocin antagonists competitively block oxytocin receptors in the myometrium, reducing uterine contractions.
| Agent | Dosing | Comments |
|---|---|---|
| Atosiban (Not available in US) |
Loading: 6.75 mg IV bolus Maintenance: 18 mg/hour for 3 hours, then 6 mg/hour for up to 45 hours |
– Commonly used in Europe – Fewer cardiovascular side effects than beta-agonists – Limited to 48 hours total treatment – Mainly hepatic elimination |
Clinical Pearl
Atosiban has a more favorable side effect profile than beta-agonists, but it is no more effective in delaying delivery or improving neonatal outcomes. It remains unavailable in the US but is widely used in Europe and other regions.
Labor Analgesia & Anesthesia
Pain management during labor can be achieved through various pharmacological methods. The choice depends on the stage of labor, maternal preferences, and maternal-fetal conditions.
| Category | Agents | Comments |
|---|---|---|
| Systemic Opioids |
– Fentanyl (25-50 μg IV) – Morphine (2-5 mg IV) – Butorphanol (1-2 mg IV) – Nalbuphine (10 mg IV/IM) – Remifentanil (PCA) |
– Moderate pain relief – Can cause maternal sedation, nausea – Risk of neonatal respiratory depression – Shorter-acting agents (fentanyl) preferred for late labor – Avoid within 1-2 hours of anticipated delivery |
| Regional Analgesia |
Epidural: – Bupivacaine 0.0625-0.125% – Ropivacaine 0.08-0.2% + Fentanyl 1-2 μg/mL Combined Spinal-Epidural: – Intrathecal fentanyl 10-25 μg – Followed by epidural infusion |
– Gold standard for labor pain relief – Minimal systemic effects – Allows patient to remain alert – May prolong second stage of labor – May cause hypotension, requiring fluid preloading – Potential for motor block with higher concentrations – Patient-controlled epidural analgesia (PCEA) increasingly used |
| Inhalational Analgesia |
– Nitrous oxide 50% with oxygen 50% (Entonox) |
– Self-administered – Rapid onset and offset – Less effective than regional anesthesia – Minimal effect on labor progress – May cause dizziness, nausea – Commonly used outside US |
| Local Anesthetics |
Pudendal Block: – Lidocaine 1%, 10 mL per side Perineal Infiltration: – Lidocaine 1-2% |
– Used for episiotomy or repair – Pudendal block helpful for outlet forceps/vacuum – No effect on uterine contractions – Minimal systemic effects – Limited area of anesthesia |
Memory Aid: “4 P’s of Pain Management”
Parenteral (systemic) opioids – Good for early labor
Pudendal block – Good for delivery/episiotomy
Perineal infiltration – Good for repair of lacerations
Pipe through the back (epidural) – Best for active labor
Nursing Considerations for Labor Analgesia
- Monitor maternal vital signs and FHR before and after administration
- Position patient in left lateral position after epidural placement to prevent aortocaval compression
- Assess level of sensory and motor block with epidural anesthesia
- Have emergency equipment and reversal agents available
- Maintain IV access throughout labor
- Monitor maternal temperature (epidural can mask fever)
- Assess for urinary retention with regional anesthesia
Best Practices & Recent Updates
Best Practice #1: Oxytocin Administration
Recent evidence supports the use of lower starting doses (0.5-1 mU/min) and slower incremental increases (every 30-60 minutes) during oxytocin administration for labor induction. This “low and slow” approach has been associated with decreased rates of uterine tachysystole and abnormal fetal heart rate patterns while maintaining efficacy.
Update: The use of standardized oxytocin protocols and checklists has been shown to reduce the incidence of adverse events related to oxytocin administration. Many institutions now use “unit-standard” dosing regimens rather than provider-specific orders.
Best Practice #2: Magnesium Sulfate for Fetal Neuroprotection
Magnesium sulfate administration to women at risk of preterm birth before 32 weeks’ gestation is now recommended for fetal neuroprotection. This practice has been associated with a 30-40% reduction in the risk of cerebral palsy in surviving infants.
Update: The optimal timing appears to be administration at least 4 hours before anticipated delivery, with neuroprotective effects diminishing after 24 hours. Re-treatment may be considered if delivery has not occurred after 24 hours and is still imminent.
Best Practice #3: Enhanced Recovery After Cesarean (ERAC)
Enhanced recovery protocols for cesarean delivery now incorporate multimodal analgesia strategies to minimize opioid use. These typically include scheduled doses of acetaminophen and NSAIDs, with neuraxial morphine for primary analgesia.
Update: The addition of TAP (transversus abdominis plane) blocks or wound infiltration with long-acting local anesthetics like liposomal bupivacaine can further reduce opioid consumption and improve maternal satisfaction with pain control.
References
1. American College of Obstetricians and Gynecologists. (2021). ACOG Practice Bulletin No. 222: Gestational Hypertension and Preeclampsia. Obstetrics & Gynecology, 135(6), e237-e260.
2. American College of Obstetricians and Gynecologists. (2019). ACOG Practice Bulletin No. 171: Management of Preterm Labor. Obstetrics & Gynecology, 133(1), e1-e14.
3. Society for Maternal-Fetal Medicine Publications Committee. (2014). The role of magnesium sulfate in the prevention and management of low birth weight and preterm birth. American Journal of Obstetrics and Gynecology, 214(6), 734-744.
4. National Institute for Health and Care Excellence. (2022). Inducing labour. NICE guideline [NG207].
5. World Health Organization. (2021). WHO recommendations: induction of labour at or beyond term.
6. Society for Obstetric Anesthesia and Perinatology. (2023). Enhanced Recovery After Cesarean (ERAC) Consensus Statement.
7. U.S. Food and Drug Administration. (2013). FDA Drug Safety Communication: FDA recommends against prolonged use of magnesium sulfate to stop pre-term labor.
8. Royal College of Obstetricians and Gynaecologists. (2022). Tocolysis for Women in Preterm Labour. Green-top Guideline No. 1b.
