Drugs Used in Management of Abnormal Labor
A Comprehensive Guide for Nursing Students
Introduction
Abnormal labor refers to labor that deviates from normal progression, often requiring medical intervention. Pharmacological agents play a critical role in managing various types of labor abnormalities, including induction, augmentation, and inhibition of uterine contractions. This comprehensive guide explores the different drug classes used in managing abnormal labor, their mechanisms of action, indications, contraindications, dosage regimens, side effects, and nursing considerations.
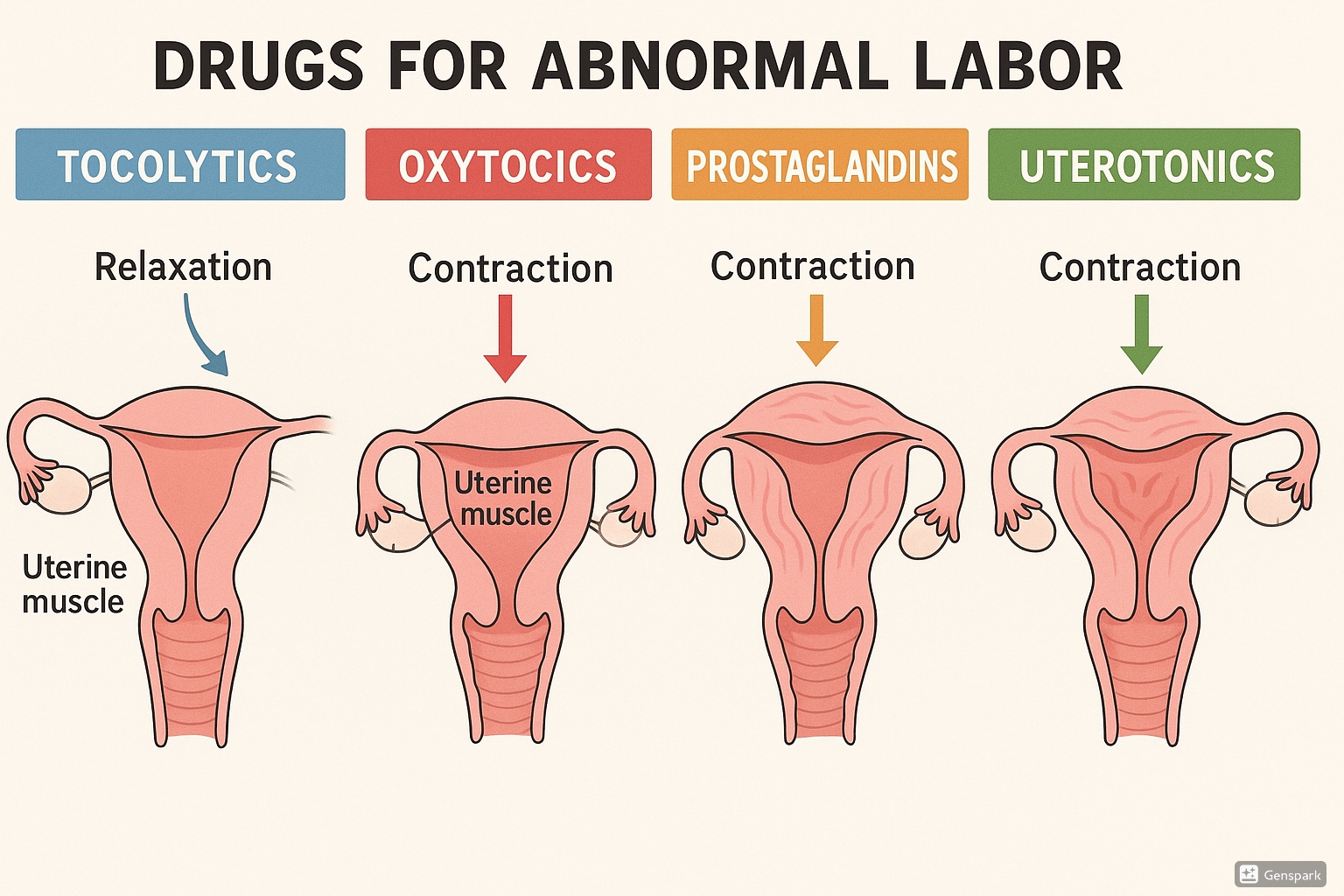
Table of Contents
- 1. Classification of Drugs Used in Abnormal Labor
- 2. Oxytocics for Labor Induction and Augmentation
- 3. Prostaglandins for Cervical Ripening and Labor Induction
- 4. Tocolytics for Inhibition of Preterm Labor
- 5. Drugs for Management of Postpartum Hemorrhage
- 6. Mechanical Methods for Cervical Ripening
- 7. Current Best Practices and Recent Updates
- 8. Clinical Scenarios
- 9. References
1. Classification of Drugs Used in Abnormal Labor
Drugs used in the management of abnormal labor can be broadly classified into the following categories based on their primary effects on uterine activity:
- Uterine Stimulants (Oxytocics): Used for labor induction and augmentation
- Cervical Ripening Agents (Prostaglandins): Used to prepare the cervix for induction
- Uterine Relaxants (Tocolytics): Used to inhibit preterm labor
- Uterotonics: Used to manage postpartum hemorrhage
| Drug Class | Primary Action | Examples | Primary Indications |
|---|---|---|---|
| Oxytocics | Stimulate uterine contractions | Oxytocin (Pitocin), Carbetocin (Duratocin) | Labor induction, augmentation, postpartum hemorrhage |
| Prostaglandins | Cervical ripening, stimulate uterine contractions | Dinoprostone (Cervidil, Prepidil), Misoprostol (Cytotec) | Cervical ripening before induction, labor induction |
| Beta-adrenergic Agonists | Relax uterine smooth muscle | Terbutaline, Ritodrine | Preterm labor inhibition |
| Calcium Channel Blockers | Relax uterine smooth muscle | Nifedipine | Preterm labor inhibition |
| Magnesium Sulfate | Relax uterine smooth muscle, neuroprotection | Magnesium Sulfate | Preterm labor inhibition, preeclampsia/eclampsia |
| NSAIDs | Inhibit prostaglandin synthesis | Indomethacin | Preterm labor inhibition |
| Oxytocin Receptor Antagonists | Block oxytocin receptors | Atosiban | Preterm labor inhibition |
| Ergot Alkaloids | Stimulate sustained uterine contractions | Methylergometrine (Methergine), Ergometrine | Postpartum hemorrhage |
| Prostaglandin F2α Analogs | Stimulate uterine contractions | Carboprost (Hemabate) | Postpartum hemorrhage |
Memory Aid: “COPT Labor Drugs”
- Contraction stimulants: Oxytocin and Ergot alkaloids
- Opening of cervix: Prostaglandins
- Prevention of preterm labor: Tocolytics (Beta-agonists, CCBs, NSAIDs, Mg)
- Termination of bleeding: Uterotonics (Oxytocin, Ergots, Prostaglandins)
2. Oxytocics for Labor Induction and Augmentation
Oxytocics are drugs that stimulate uterine contractions. They are primarily used for labor induction or augmentation when spontaneous labor is inadequate or delayed.
2.1. Oxytocin (Pitocin)
Mechanism of Action
Oxytocin is a synthetic form of the naturally occurring posterior pituitary hormone. It:
- Binds to oxytocin receptors on uterine myometrial cells
- Increases intracellular calcium concentration
- Stimulates contractions of uterine smooth muscle
- Increases the frequency and force of uterine contractions
- Increases prostaglandin production, which also contributes to uterine contractions
Indications
- Induction of labor
- Augmentation of labor when contractions are inadequate
- Prevention and treatment of postpartum hemorrhage
Contraindications
- Hypersensitivity to oxytocin
- Significant cephalopelvic disproportion
- Unfavorable fetal positions or presentations (e.g., transverse lie)
- Fetal distress where delivery is not imminent
- Placenta previa or vasa previa
- Active genital herpes infection
- Previous classical cesarean section or other significant uterine surgery
- Previous uterine rupture
- Invasive cervical cancer
Dosage and Administration
- For Induction/Augmentation of Labor:
- Low-dose protocol: Start at 0.5-2 mU/min, increase by 1-2 mU/min every 15-40 minutes until adequate contractions achieved. Maximum dose: 40 mU/min.
- High-dose protocol: Start at 6 mU/min, increase by 6 mU/min every 15 minutes until adequate contractions achieved. Maximum dose: 40 mU/min.
- For Prevention of Postpartum Hemorrhage: 10-40 units in 1000 mL of IV fluid, infused at 125 mL/hr after delivery of the placenta
- For Treatment of Postpartum Hemorrhage: 10-40 units in 1000 mL of IV fluid, infused at a rate sufficient to control uterine atony
Adverse Effects
Maternal Effects:
- Uterine hyperstimulation
- Uterine rupture
- Water intoxication (with prolonged infusion)
- Hypotension
- Nausea and vomiting
- Cardiac arrhythmias
- Anaphylaxis (rare)
Fetal Effects:
- Fetal distress due to hyperstimulation
- Fetal hypoxia
- Neonatal jaundice
- Neonatal hyperbilirubinemia
Warning: Uterine Hyperstimulation
Uterine hyperstimulation with oxytocin can lead to:
- Contractions lasting longer than 90 seconds
- Contractions occurring closer than every 2 minutes
- Resting tone > 20 mmHg between contractions
- Fetal heart rate abnormalities
- Potential uterine rupture
Nursing Considerations
- Before administration:
- Verify physician order for oxytocin including dosage, rate of infusion, and parameters
- Assess maternal vital signs, fetal heart rate, and uterine activity as baseline
- Ensure availability of emergency equipment
- Verify adequate IV access
- Ensure patient is on continuous electronic fetal monitoring
- During administration:
- Continuous electronic fetal monitoring
- Monitor frequency, duration, and strength of contractions
- Monitor maternal vital signs every 15-30 minutes
- Monitor fluid intake and output to prevent water intoxication
- Use infusion pump to ensure accurate dosing
- Never administer as IV push or bolus
- Interventions for hyperstimulation:
- Discontinue oxytocin infusion immediately
- Position patient on her left side to improve uteroplacental perfusion
- Administer oxygen at 8-10 L/min via face mask
- Increase IV fluid rate
- Notify physician/midwife
Memory Aid: “CONTRACTILE” for Oxytocin
- Continuous monitoring is essential
- Only use infusion pump
- Never give as IV push
- Titration based on contraction pattern
- Regular assessment of maternal-fetal status
- Avoid hyperstimulation
- Caution with fluid overload
- Turn off if hyperstimulation occurs
- Infusion rate determines action
- Left lateral position if fetal distress
- Emergency equipment nearby
2.2. Carbetocin (Duratocin)
Mechanism of Action
Carbetocin is a long-acting synthetic analog of oxytocin. It:
- Binds to oxytocin receptors on uterine myometrial cells
- Has a longer half-life than oxytocin (approximately 40 minutes vs. 3-5 minutes)
- Provides sustained uterine contractions
- Requires only a single dose versus continuous infusion
Indications
- Prevention of postpartum hemorrhage following cesarean delivery
- Prevention of uterine atony after delivery
Contraindications
- Similar to oxytocin
- Hypersensitivity to carbetocin or oxytocin
- Pregnancy (not for induction or augmentation)
- Liver or kidney disease
- Epilepsy
Dosage and Administration
- Standard dose: 100 mcg as a single IV bolus over 1 minute
- Timing: Administered after delivery of the baby, either before or after delivery of the placenta, depending on institutional protocol
Adverse Effects
- Similar to oxytocin but generally less severe due to single-dose administration
- Headache
- Tremor
- Hypotension
- Flushing
- Nausea and vomiting
- Abdominal pain
- Pruritus
Nursing Considerations
- Administer as a single IV bolus over 1 minute
- Monitor vital signs after administration
- Assess uterine tone after administration
- Monitor for signs of postpartum hemorrhage
- No repeat doses are recommended
Clinical Pearl
Heat-stable carbetocin has been developed for use in low-resource settings where refrigeration is not consistently available. The World Health Organization (WHO) has included heat-stable carbetocin in its recommendations for preventing postpartum hemorrhage.
3. Prostaglandins for Cervical Ripening and Labor Induction
Prostaglandins are used for cervical ripening before labor induction. They soften the cervix and can initiate uterine contractions, making them valuable for patients with an unfavorable cervix (low Bishop score).
3.1. Dinoprostone (Cervidil, Prepidil)
Mechanism of Action
Dinoprostone is a synthetic form of prostaglandin E2 (PGE2). It:
- Increases the production of collagenase in the cervix
- Decreases collagen content of the cervix
- Softens the cervix and increases cervical compliance
- Stimulates uterine contractions
- Relaxes cervical smooth muscle
Indications
- Cervical ripening in patients with an unfavorable Bishop score who require labor induction
- Induction of labor in patients at or near term gestation
Contraindications
- Hypersensitivity to prostaglandins
- Situations where vaginal delivery is contraindicated
- Unexplained vaginal bleeding during pregnancy
- Placenta previa or vasa previa
- Previous cesarean section or major uterine surgery
- Active genital herpes infection
- Pelvic structural abnormalities
- Fetal distress
- Grand multiparity (≥6 previous deliveries)
- Regular, progressive uterine contractions
Dosage and Administration
- Cervidil (vaginal insert): 10 mg insert placed transversely in the posterior fornix of the vagina. Remains in place for up to 12 hours.
- Prepidil (cervical gel): 0.5 mg applied intracervically. May repeat every 6 hours if needed. Maximum total dose: 1.5 mg (3 doses in 24 hours).
Adverse Effects
- Uterine hyperstimulation with or without fetal distress
- Nausea and vomiting
- Diarrhea
- Fever
- Headache
- Backache
- Warm feeling in vagina
- Uterine rupture (rare)
Nursing Considerations
- Before administration:
- Assess baseline fetal heart rate and uterine activity
- Confirm Bishop score and indication for cervical ripening
- Verify no contraindications exist
- During and after administration:
- Continuous electronic fetal monitoring
- Monitor for uterine hyperstimulation
- Maintain patient in recumbent position for 30 minutes after insertion
- Have patient avoid ambulation for 2 hours after insertion
- Cervidil can be easily removed if hyperstimulation occurs
- Do not start oxytocin until at least 30 minutes after Cervidil removal or 6-12 hours after Prepidil application
Memory Aid: “CERVICAL” for Dinoprostone
- Cervical ripening is primary effect
- Examine Bishop score before use
- Remove if hyperstimulation occurs
- Vaginal placement (posterior fornix)
- Increases collagenase in cervix
- Continuous monitoring required
- Avoid oxytocin for 6-12 hours after use
- Low Bishop score is indication
3.2. Misoprostol (Cytotec)
Mechanism of Action
Misoprostol is a synthetic prostaglandin E1 (PGE1) analog. It:
- Softens the cervix by promoting breakdown of collagen fibers
- Increases water content in cervical tissue
- Stimulates uterine contractions by increasing calcium influx into myometrial cells
- Results in cervical effacement and dilation
Indications
- Cervical ripening and labor induction in viable pregnancies
- Management of postpartum hemorrhage (off-label)
- Management of incomplete abortion or miscarriage
Important Note
Misoprostol is FDA approved for prevention of NSAID-induced gastric ulcers. Its use for cervical ripening and labor induction is off-label but widely practiced and supported by clinical evidence and guidelines.
Contraindications
- Similar to dinoprostone
- Previous cesarean delivery or major uterine surgery (represents a significant risk of uterine rupture)
- Hypersensitivity to prostaglandins
- Active labor or ruptured membranes
Dosage and Administration
- Vaginal route: 25 mcg every 3-6 hours (maximum of 4 doses in 24 hours)
- Oral route: 50-100 mcg every 4-6 hours
- Sublingual route: 25-50 mcg every 4-6 hours
- Buccal route: 25-50 mcg every 4-6 hours
Warning: Uterine Rupture Risk
Misoprostol significantly increases the risk of uterine rupture in patients with previous uterine scars, particularly from cesarean deliveries. The use of misoprostol in these patients is contraindicated.
Adverse Effects
- Uterine hyperstimulation
- Uterine rupture
- Nausea and vomiting
- Diarrhea
- Fever and shivering
- Headache
- Fetal distress secondary to hyperstimulation
Nursing Considerations
- Before administration:
- Confirm gestational age and absence of contraindications
- Perform baseline assessment of maternal vital signs and fetal heart rate
- Review Bishop score
- During and after administration:
- Continuous electronic fetal monitoring
- Monitor for uterine hyperstimulation
- Monitor temperature (due to risk of fever)
- Provide antiemetics if needed for nausea
- Tocolytic agents should be available if hyperstimulation occurs
- Patient education:
- Inform patient about expected effects (contractions)
- Explain potential side effects
- Instruct to report excessive cramping or bleeding
Clinical Pearl
According to recent studies from 2025, vaginal misoprostol achieves vaginal delivery rates similar to oral misoprostol while significantly reducing the need for oxytocin augmentation. The vaginal route may be preferred when aiming to reduce additional interventions during labor.
Memory Aid: “MISO-P” for Misoprostol
- Multiple routes of administration (vaginal, oral, sublingual, buccal)
- Increases uterine contractions
- Scar from previous C-section is a contraindication
- Off-label use but evidence-based
- Prostaglandin E1 analog that causes cervical ripening
Comparing Prostaglandins
Recent studies indicate that while both dinoprostone and misoprostol are effective for cervical ripening and labor induction, misoprostol tends to be more effective at achieving vaginal delivery within 24 hours and is more cost-effective. However, misoprostol may have a slightly higher risk of uterine hyperstimulation. The choice between agents should consider individual patient factors, institutional protocols, and availability.
4. Tocolytics for Inhibition of Preterm Labor
Tocolytics are drugs that inhibit uterine contractions and are used to delay delivery in women with preterm labor. They provide time for administration of antenatal corticosteroids, magnesium for fetal neuroprotection, and maternal transport to a tertiary care center if needed.
Important Information
Tocolytics typically delay delivery for only 48-72 hours but can provide critical time for interventions that improve neonatal outcomes. They are not used to prevent preterm delivery over the long term.
4.1. Beta-Adrenergic Agonists
4.1.1. Terbutaline
Mechanism of Action
Terbutaline is a beta-2 adrenergic receptor agonist. It:
- Stimulates beta-2 adrenergic receptors in uterine smooth muscle
- Increases intracellular cyclic AMP
- Decreases intracellular calcium concentration
- Inhibits myosin light-chain kinase activity
- Results in uterine muscle relaxation
Indications
- Acute tocolysis for preterm labor
- Short-term delay of delivery (48-72 hours) to allow for:
- Administration of antenatal corticosteroids
- Maternal transfer to a facility with neonatal intensive care
- Administration of magnesium sulfate for fetal neuroprotection
Contraindications
- Maternal cardiac disease
- Pulmonary edema
- Maternal hyperthyroidism
- Poorly controlled diabetes mellitus
- Eclampsia or severe preeclampsia
- Maternal hemodynamic instability
- Chorioamnionitis
- Advanced cervical dilation (>4-5 cm)
- Significant vaginal bleeding
- Fetal anomalies incompatible with life
- Intrauterine fetal demise
- Placental abruption
Dosage and Administration
- Subcutaneous: 0.25 mg every 20 minutes to 3-4 hours as needed, maximum of 5 mg in 24 hours
- Intravenous (rarely used): Initial loading dose of 2.5-10 mcg/min, increased by 2.5-5 mcg/min every 20 minutes until contractions cease or side effects occur. Maximum dose: 25 mcg/min
- Oral (maintenance): 2.5-5 mg every 4-6 hours (no longer recommended by FDA for maintenance)
Adverse Effects
Maternal Effects:
- Tachycardia
- Palpitations
- Tremor
- Nervousness
- Headache
- Nausea
- Vomiting
- Hyperglycemia
- Hypokalemia
- Pulmonary edema (rare)
- Chest pain
- Myocardial ischemia (rare)
Fetal Effects:
- Fetal tachycardia
- Neonatal hypoglycemia
- Neonatal hypocalcemia
- Ileus
- Hyperbilirubinemia
FDA Warning
The FDA has issued a black box warning against the prolonged use (beyond 48-72 hours) of terbutaline for prevention of preterm labor or maintenance tocolysis due to the risk of serious maternal cardiac events and death.
Nursing Considerations
- Before administration:
- Assess maternal cardiac status and vital signs
- Obtain baseline maternal electrolytes, especially potassium
- Monitor blood glucose, especially in diabetic patients
- Check fetal heart rate and uterine contractions
- During administration:
- Monitor maternal vital signs every 15 minutes during initial dosing, then every 1-4 hours
- Monitor maternal pulse continuously; maintain below 120 bpm
- Monitor for signs of pulmonary edema (dyspnea, crackles)
- Monitor maternal ECG if possible
- Monitor uterine contractions
- Monitor fetal heart rate continuously
- Maintain strict intake and output
- Monitor electrolytes, especially potassium
- Monitor blood glucose
Memory Aid: “BETA-BLOCK” for Beta-Agonist Tocolytics
- Blood glucose rises
- Electrolyte imbalance (hypokalemia)
- Tachycardia is common
- Avoid in cardiac disease
- Brief use only (48-72 hours)
- Limits contractions by relaxing uterine muscle
- Ongoing assessment of maternal vitals
- Cardiac side effects are serious risks
- Keep monitoring pulmonary status
4.1.2. Ritodrine
Ritodrine is no longer available in the United States but is used in some countries for tocolysis. It has a mechanism of action similar to terbutaline and similar side effect profile.
Mechanism of Action
Similar to terbutaline, ritodrine is a beta-2 adrenergic agonist that relaxes uterine smooth muscle.
Dosage and Administration
- Intravenous: Initial dose of 50-100 mcg/min, increased by 50 mcg/min every 10 minutes until contractions cease or side effects occur. Maximum dose: 350 mcg/min.
- Oral (maintenance): 10-20 mg every 4-6 hours
4.2. Calcium Channel Blockers
4.2.1. Nifedipine
Mechanism of Action
Nifedipine is a calcium channel blocker. It:
- Blocks L-type calcium channels in smooth muscle cell membranes
- Decreases intracellular calcium concentration
- Inhibits calcium-dependent myosin light-chain kinase activation
- Prevents actin-myosin interaction
- Results in uterine smooth muscle relaxation
Indications
- First-line tocolytic for acute preterm labor (in many institutions)
- Delay of delivery for 48-72 hours to allow for:
- Administration of antenatal corticosteroids
- Transfer to a facility with neonatal intensive care
- Administration of magnesium sulfate for fetal neuroprotection
Contraindications
- Hypersensitivity to nifedipine
- Severe maternal hypotension
- Advanced liver disease
- Concurrent use with magnesium sulfate (potential for severe hypotension)
- Aortic stenosis
- Congestive heart failure
- Same contraindications for tocolysis as with beta-agonists
Dosage and Administration
- Loading dose: 10-20 mg orally, may repeat in 30 minutes if contractions persist
- Maintenance dose: 10-20 mg orally every 4-6 hours for 48-72 hours
- Alternative regimen: Extended-release 30-60 mg daily
Note: Do not administer sublingually due to risk of precipitous hypotension.
Adverse Effects
- Maternal hypotension
- Reflex tachycardia
- Headache
- Flushing
- Dizziness
- Peripheral edema
- Nausea
- Transient hypoxemia (rare)
- Elevated liver enzymes (with prolonged use)
Nursing Considerations
- Before administration:
- Assess baseline maternal blood pressure and heart rate
- Ensure patient is not taking other medications that could interact with nifedipine
- Verify patient is not receiving concurrent magnesium sulfate
- Assess fetal heart rate and uterine contractions
- During administration:
- Monitor maternal blood pressure and pulse every 15-30 minutes for first 2 hours, then every 2-4 hours
- Assess for symptoms of hypotension (dizziness, lightheadedness)
- Monitor for headache and provide analgesia as needed
- Monitor fetal heart rate
- Monitor uterine contractions
- Patient education:
- Report dizziness, severe headache, or chest pain immediately
- Change positions slowly to minimize orthostatic hypotension
- Maintain adequate hydration
Clinical Pearl
According to recent systematic reviews, nifedipine appears to have better efficacy and fewer maternal side effects compared to beta-agonists for tocolysis. It has become the first-line tocolytic in many institutions.
Memory Aid: “CALCIUM BLOCK” for Nifedipine
- Carefully monitor blood pressure
- Avoid sublingual administration
- Likely to cause headaches
- Caution with magnesium sulfate (interaction)
- Immediate release for loading dose
- Uterine relaxation via calcium channel blockade
- Maintenance with extended release possible
- Blood pressure drops common
- Limits uterine contractions effectively
- Oral administration only
- Changes in position should be slow
- Keep patient well-hydrated
4.3. Magnesium Sulfate
Mechanism of Action
As a tocolytic, magnesium sulfate:
- Acts as a calcium antagonist
- Competes with calcium for entry into cells
- Decreases intracellular calcium concentration
- Inhibits myosin light-chain kinase activity
- Reduces actin-myosin interaction
- Results in uterine muscle relaxation
As a neuroprotective agent, it:
- Blocks N-methyl-D-aspartate (NMDA) receptors
- Reduces cerebral injury from hypoxia/ischemia
- Decreases inflammatory cytokines
- Stabilizes cell membranes
Indications
- Tocolysis for preterm labor (though recent evidence suggests limited effectiveness)
- Fetal neuroprotection when delivery is anticipated before 32 weeks’ gestation
- Treatment and prevention of seizures in preeclampsia/eclampsia
Contraindications
- Myasthenia gravis
- Heart block or significant cardiac disease
- Renal failure
- Myocardial damage
- Hepatitis
- Same contraindications for tocolysis as with other agents
Dosage and Administration
- For tocolysis:
- Loading dose: 4-6 g IV over 20-30 minutes
- Maintenance dose: 2-4 g/hour continuous IV infusion for 12-24 hours
- For fetal neuroprotection:
- Loading dose: 4 g IV over 30 minutes
- Maintenance dose: 1 g/hour continuous IV infusion until delivery or for a maximum of 24 hours
- Therapeutic serum levels:
- Tocolysis: 5-8 mEq/L (6-10 mg/dL)
- Preeclampsia: 4-7 mEq/L (4.8-8.4 mg/dL)
Adverse Effects
Maternal Effects:
- Flushing
- Feeling of warmth
- Diaphoresis
- Nausea and vomiting
- Headache
- Visual disturbances
- Lethargy
- Pulmonary edema
- Respiratory depression
- Hypotension
- Decreased deep tendon reflexes
- Cardiac arrest (at very high levels)
Fetal/Neonatal Effects:
- Decreased fetal heart rate variability
- Lethargy at birth
- Hypotonia
- Respiratory depression
- Lower Apgar scores
Warning: Magnesium Toxicity
Signs of magnesium toxicity by serum levels:
- Loss of patellar reflexes: 8-12 mg/dL
- Respiratory depression: 12-15 mg/dL
- Cardiac arrest: >25 mg/dL
Antidote: Calcium gluconate 1 g IV (10 mL of 10% solution) over 2-3 minutes
Nursing Considerations
- Before administration:
- Assess baseline vital signs, deep tendon reflexes, and level of consciousness
- Check baseline renal function
- Ensure IV access with large-bore catheter
- Verify appropriate infusion pump settings
- Check availability of calcium gluconate as antidote
- During administration:
- Monitor maternal vital signs every 15-30 minutes during loading dose, then every 1-2 hours
- Assess deep tendon reflexes hourly
- Monitor respiratory rate (keep >12 breaths/min)
- Monitor urine output (maintain >30 mL/hr)
- Monitor magnesium levels every 4-6 hours
- Assess for signs of toxicity
- Monitor fetal heart rate continuously
Memory Aid: “MAGNESIUM”
- Monitor reflexes frequently
- Assess respiratory rate (keep >12/min)
- Guard against toxicity
- Neuromuscular function affected
- Ensure adequate urine output
- Serum levels guide therapy (5-8 mEq/L for tocolysis)
- Infusion rate determines effect
- Use infusion pump for administration
- Maintain calcium gluconate at bedside
4.4. NSAIDs
4.4.1. Indomethacin
Mechanism of Action
Indomethacin is a non-steroidal anti-inflammatory drug (NSAID). It:
- Inhibits cyclooxygenase (COX) enzymes
- Decreases prostaglandin synthesis
- Reduces prostaglandin-mediated uterine contractions
- May also decrease intracellular calcium levels
Indications
- Acute tocolysis for preterm labor before 32 weeks’ gestation
- Particularly useful in polyhydramnios-associated preterm labor
Contraindications
- Gestational age >32 weeks (due to risk of premature closure of ductus arteriosus)
- Renal or hepatic dysfunction
- Active peptic ulcer disease
- Platelet dysfunction or coagulopathy
- Significant heart disease
- Intrauterine growth restriction
- Oligohydramnios
- Maternal hypertension
- Same contraindications for tocolysis as with other agents
Dosage and Administration
- Loading dose: 50-100 mg orally or rectally
- Maintenance dose: 25-50 mg orally every 6 hours or 100 mg rectally every 12 hours
- Duration: Usually limited to 48-72 hours; maximum cumulative duration should not exceed 72 hours
Adverse Effects
Maternal Effects:
- Nausea, vomiting, dyspepsia
- Gastric irritation, ulceration
- Platelet dysfunction
- Increased bleeding time
- Fluid retention
- Renal dysfunction
- Headache
- Dizziness
Fetal/Neonatal Effects:
- Premature closure of ductus arteriosus
- Pulmonary hypertension
- Decreased renal function
- Oligohydramnios
- Necrotizing enterocolitis (potentially)
- Intraventricular hemorrhage (potentially)
Warning: Fetal Risks
Due to the risk of premature closure of the ductus arteriosus, indomethacin should not be used beyond 32 weeks gestation and should be limited to 48-72 hours of treatment.
Nursing Considerations
- Before administration:
- Verify gestational age is <32 weeks
- Assess baseline maternal renal and hepatic function
- Check for history of GI disorders
- Assess amniotic fluid volume
- During administration:
- Monitor for signs of GI irritation
- Monitor uterine contractions
- Monitor fetal heart rate
- Assess amniotic fluid volume daily
- Monitor for signs of bleeding or bruising
- Patient education:
- Take with food to minimize GI effects
- Report any unusual bleeding or bruising
- Report severe headache or visual disturbances
Clinical Pearl
Indomethacin may be particularly effective in cases of preterm labor associated with polyhydramnios because it can reduce fetal urine production and subsequently decrease amniotic fluid volume, which may help alleviate uterine distention.
4.5. Oxytocin Receptor Antagonists
4.5.1. Atosiban
Important Note
Atosiban is not FDA-approved in the United States but is widely used in Europe and other countries for tocolysis.
Mechanism of Action
Atosiban is a competitive oxytocin receptor antagonist. It:
- Competes with oxytocin for binding to the oxytocin receptors in the myometrium
- Blocks oxytocin-mediated release of inositol trisphosphate from myometrial cell membranes
- Prevents the increase in intracellular calcium induced by oxytocin
- Inhibits uterine contractions
Indications
- Tocolysis for preterm labor between 24 and 33 weeks’ gestation
Contraindications
- Gestational age <24 weeks or >33 weeks
- Preterm premature rupture of membranes >30 weeks
- Intrauterine growth restriction with abnormal fetal heart rate
- Antepartum hemorrhage requiring immediate delivery
- Intrauterine infection
- Placenta previa
- Abruptio placentae
- Same contraindications for tocolysis as with other agents
Dosage and Administration
- Initial bolus: 6.75 mg IV over 1 minute
- Loading infusion: 18 mg/hour for 3 hours
- Maintenance infusion: 6 mg/hour for up to 45 hours
- Maximum duration: 48 hours
- Maximum cumulative dose: 330 mg
Adverse Effects
Atosiban has a favorable safety profile compared to other tocolytics, with fewer maternal cardiovascular side effects.
- Nausea
- Vomiting
- Headache
- Dizziness
- Hot flushes
- Tachycardia
- Hypotension
- Hyperglycemia (less common)
- Injection site reactions
Nursing Considerations
- Before administration:
- Verify gestational age is between 24-33 weeks
- Assess maternal vital signs
- Assess fetal heart rate and uterine contractions
- During administration:
- Monitor maternal vital signs
- Monitor blood glucose levels, especially in diabetic patients
- Assess uterine contractions
- Monitor fetal heart rate
- Observe for injection site reactions
Clinical Pearl
Atosiban has fewer cardiovascular side effects compared to beta-agonists and may be preferred in patients with cardiac conditions. Recent studies also suggest it may have anti-inflammatory properties that could provide additional benefits in managing preterm labor.
Comparative Efficacy of Tocolytics
According to the most recent meta-analyses and systematic reviews, calcium channel blockers (particularly nifedipine) and oxytocin receptor antagonists (atosiban) appear to have the best balance of efficacy and safety for acute tocolysis. Beta-agonists are effective but associated with more maternal side effects. Magnesium sulfate has limited evidence supporting its effectiveness as a tocolytic but remains important for fetal neuroprotection. NSAIDs can be effective for short-term use before 32 weeks.
5. Drugs for Management of Postpartum Hemorrhage
Postpartum hemorrhage (PPH) is a leading cause of maternal mortality worldwide. Pharmacological agents used to manage PPH primarily act by increasing uterine muscle tone and contractions.
5.1. Ergot Alkaloids
5.1.1. Methylergometrine (Methergine)
Mechanism of Action
Methylergometrine is a semisynthetic ergot alkaloid. It:
- Directly stimulates alpha-adrenergic and serotonin receptors in uterine smooth muscle
- Produces strong, sustained tetanic uterine contractions
- Reduces uterine blood flow
- Causes generalized vasoconstriction
Indications
- Prevention and treatment of postpartum hemorrhage due to uterine atony
- Management of subinvolution of the uterus
Contraindications
- Hypertension
- Preeclampsia or eclampsia
- Coronary artery disease
- Peripheral vascular disease
- Hepatic or renal impairment
- During pregnancy or labor (before delivery of the placenta)
- Hypersensitivity to ergot alkaloids
Dosage and Administration
- Intramuscular: 0.2 mg after delivery of placenta or as needed to control uterine atony
- Intravenous: 0.2 mg slowly over 1 minute for emergency control of hemorrhage (use with caution)
- Oral: 0.2 mg every 6-8 hours for 2-7 days
Note: Intravenous administration should be used only in emergencies when other routes are not feasible.
Adverse Effects
- Hypertension (sometimes severe)
- Nausea and vomiting
- Headache
- Dizziness
- Chest pain
- Dyspnea
- Peripheral vasospasm
- Seizures
- Stroke (rare)
- Myocardial infarction (rare)
Nursing Considerations
- Before administration:
- Verify blood pressure is within normal limits
- Ensure placenta has been delivered
- Assess for contraindications
- During administration:
- Monitor blood pressure and pulse every 15 minutes for at least 1 hour after parenteral administration
- Assess for signs of hypertension or vasospasm
- Assess uterine tone frequently
- Evaluate lochia for excessive bleeding
- Patient education:
- Report severe headache or chest pain immediately
- Watch for signs of peripheral vasospasm (cold or numb extremities)
- Take oral doses with food to minimize GI effects
Memory Aid: “ERGOTS”
- Elevated blood pressure (monitor closely)
- Rigid, tetanic uterine contractions
- Generalized vasoconstriction
- Only after placental delivery
- Take vital signs frequently
- Strong contraindication in hypertension
5.1.2. Ergometrine
Ergometrine is similar to methylergometrine but may have a more rapid onset and shorter duration of action. It is used similarly for management of postpartum hemorrhage and has comparable contraindications, side effects, and nursing considerations.
Dosage and Administration
- Intramuscular: 0.2-0.5 mg
- Intravenous: 0.1-0.5 mg (for emergency use only)
- Oral: 0.2-0.5 mg every 6-8 hours for up to 48 hours
5.2. Prostaglandins for PPH
5.2.1. Carboprost (Hemabate)
Mechanism of Action
Carboprost is a synthetic 15-methyl analog of prostaglandin F2α. It:
- Stimulates myometrial contractions by increasing myometrial calcium levels
- Produces sustained uterine contractions
- Causes vasoconstriction
- Is effective when other uterotonics fail (typically used as a second-line agent)
Indications
- Treatment of postpartum hemorrhage due to uterine atony that has not responded to conventional methods
- Second-line treatment for refractory postpartum bleeding
Contraindications
- Active cardiac, pulmonary, renal, or hepatic disease
- Acute pelvic inflammatory disease
- Hypersensitivity to prostaglandins
Dosage and Administration
- Standard dose: 250 mcg (0.25 mg) intramuscular
- Repeat dose: May be repeated every 15-90 minutes as needed
- Maximum dose: 2 mg total (8 doses)
Adverse Effects
- Diarrhea (most common)
- Nausea and vomiting
- Fever
- Headache
- Chills
- Flushing
- Hypertension
- Bronchospasm (use with caution in asthmatic patients)
Nursing Considerations
- Before administration:
- Review patient history for contraindications
- Verify adequate first-line interventions have been attempted
- Assess baseline vital signs
- During administration:
- Monitor vital signs
- Assess uterine tone
- Evaluate lochia
- Monitor for diarrhea and provide appropriate interventions
- Monitor temperature for fever
- Assess for respiratory distress, especially in asthmatic patients
Memory Aid: “CARBOPROST”
- Contractions are strong and sustained
- Asthma is a relative contraindication
- Repeatable every 15-90 minutes
- Bronchospasm is a potential side effect
- Only intramuscular administration
- Prostaglandin F2α derivative
- Refractory uterine atony is main indication
- Onset is rapid (usually within minutes)
- Second-line agent after oxytocin/ergot alkaloids
- Temperature may increase (fever is common)
Stepwise Approach to Postpartum Hemorrhage Management
Current guidelines recommend a stepwise approach to pharmacological management of postpartum hemorrhage:
- First-line: Oxytocin (IV bolus followed by infusion)
- Second-line: Ergot alkaloids (methylergometrine/ergometrine) or Prostaglandins (carboprost or misoprostol)
- Third-line: Additional prostaglandins if not already used
- Adjuncts: Tranexamic acid (an antifibrinolytic) is now recommended within the first 3 hours of bleeding onset
6. Mechanical Methods for Cervical Ripening
Although the focus of this guide is on pharmacological agents, mechanical methods are important alternatives or adjuncts to drugs for cervical ripening and labor induction.
| Method | Description | Mechanism | Advantages | Disadvantages |
|---|---|---|---|---|
| Foley Catheter | Insertion of a balloon catheter through the cervical os and inflation with 30-60 mL of fluid | Mechanical pressure causes cervical dilation and stimulates release of endogenous prostaglandins | Low cost, reduced risk of uterine hyperstimulation, can be used with previous cesarean | Potential increased risk of infection, discomfort during placement |
| Double Balloon Catheter | Device with two balloons, one placed above internal os and one below external os | Direct pressure on cervix from both sides | May be more effective than single balloon, can be used with previous cesarean | Higher cost, potential discomfort |
| Laminaria/Dilapan | Hygroscopic dilators placed in cervical canal | Absorb moisture and gradually expand, causing cervical dilation | Gradual cervical ripening, reduced risk of hyperstimulation | Slower action, risk of infection |
| Amniotomy | Artificial rupture of membranes | Release of prostaglandins from membranes and stimulation of contractions | Immediate impact, can be combined with other methods | Requires some cervical dilation already, risk of cord prolapse, committed to delivery |
Bishop Score
The Bishop score assesses cervical readiness for induction by evaluating:
- Cervical dilation
- Cervical effacement
- Cervical consistency
- Cervical position
- Fetal station
Scores ≤ 5 indicate an unfavorable cervix that may benefit from ripening methods before oxytocin induction.
Clinical Pearl
Recent evidence suggests that mechanical methods are as effective as pharmacological methods for cervical ripening and may be associated with a lower risk of uterine hyperstimulation. Combined methods (mechanical + pharmacological) may be more effective than either alone for reducing time to delivery, particularly in nulliparous women with unfavorable cervices.
7. Current Best Practices and Recent Updates
Best Practice #1: Oxytocin Protocol Standardization
ACOG recommends institutions develop and implement standardized oxytocin protocols for induction and augmentation of labor. Standardized protocols have been shown to:
- Reduce the incidence of uterine hyperstimulation
- Decrease cesarean delivery rates
- Improve maternal and fetal outcomes
- Enhance communication among the healthcare team
These protocols should include clear criteria for initiation, dosing regimens, monitoring parameters, and management of adverse events.
Best Practice #2: Individualized Approach to Labor Dystocia
Recent guidelines from ACOG (2024) emphasize the importance of individualized management of abnormal labor patterns rather than strict adherence to time limits. Key recommendations include:
- Careful assessment of labor progression considering multiple factors (e.g., parity, epidural use, maternal BMI)
- Recognition that the active phase of labor may not begin until 6 cm dilation
- Allowing additional time before diagnosing arrest of dilation (≥4 hours with adequate contractions or ≥6 hours with inadequate contractions requiring oxytocin)
- Judicious use of oxytocin augmentation with consideration of maternal and fetal status
Best Practice #3: Prevention of Primary Cesarean Delivery
Current guidelines emphasize strategies to safely reduce the rate of primary cesarean deliveries, including:
- Allowing adequate time for the latent and active phases of labor
- Encouraging the use of amniotomy and oxytocin augmentation before considering cesarean for arrest disorders
- Using standardized definitions of abnormal labor progression based on contemporary labor curves
- Considering operative vaginal delivery as an alternative to cesarean when appropriate
- Supporting effective labor management techniques such as continuous support, position changes, and ambulation
Recent Updates (2023-2025)
Updated Labor Curves
The most recent ACOG guidelines (2024) have adopted contemporary labor curves that account for modern obstetric populations and practices. These curves demonstrate slower labor progression than previously accepted norms and provide guidance for more patient-specific approaches to diagnosing abnormal labor patterns.
Tocolytic Selection
Current evidence supports calcium channel blockers (nifedipine) as first-line tocolytic agents due to their favorable efficacy and side effect profile. The combination of tocolytic therapy with antenatal corticosteroids and magnesium sulfate for neuroprotection has become standard practice for management of threatened preterm labor before 32 weeks.
Carbetocin for PPH Prevention
Heat-stable carbetocin has been included in WHO recommendations for prevention of postpartum hemorrhage, particularly in settings where cold-chain storage is challenging. It provides similar efficacy to oxytocin with the advantage of a single dose and longer duration of action.
Combined Approaches to Cervical Ripening
Recent studies support the use of combined mechanical and pharmacological methods for cervical ripening in certain situations. The combination may reduce the time to delivery and lower the total dose of pharmacological agents required.
Tranexamic Acid for PPH
Tranexamic acid, an antifibrinolytic agent, is now recommended by WHO and ACOG for use in the management of postpartum hemorrhage. It should be administered within 3 hours of birth for women with PPH, regardless of the cause.
Misoprostol Route Update
Recent research from 2025 indicates that vaginal misoprostol achieves similar vaginal delivery rates as oral administration while significantly reducing the need for oxytocin augmentation, providing a potential advantage in labor induction protocols.
8. Clinical Scenarios
Scenario 1: Labor Induction with Unfavorable Cervix
Patient: 39-year-old G2P1, 41 weeks gestation with Bishop score of 3, scheduled for labor induction.
Pharmacological Approach
- Initial cervical ripening: Dinoprostone vaginal insert (Cervidil) 10 mg placed in posterior fornix for up to 12 hours
- Reassessment: Evaluate Bishop score after 12 hours (or sooner if regular contractions develop)
- Secondary cervical ripening: If Bishop score remains unfavorable, consider misoprostol 25 mcg vaginally every 4-6 hours (up to 4 doses)
- Labor induction: Once Bishop score is favorable (≥6) or after adequate ripening, begin oxytocin infusion
- Starting dose: 1-2 mU/min
- Increase by 1-2 mU/min every 30 minutes
- Continue titration until adequate contractions achieved
- Artificial rupture of membranes: Consider when cervical dilation is ≥3 cm to enhance labor progress
Nursing Considerations
- Perform continuous electronic fetal monitoring throughout the induction process
- Assess and document maternal vital signs per protocol
- Monitor for signs of uterine hyperstimulation (contractions lasting >90 seconds or occurring more frequently than every 2 minutes)
- Remove dinoprostone immediately if hyperstimulation occurs
- Wait 30 minutes after removal of dinoprostone before starting oxytocin
- Use an infusion pump for oxytocin administration
- Monitor fluid intake and output
- Provide emotional support and education about the induction process
Scenario 2: Preterm Labor at 28 Weeks
Patient: 25-year-old G1P0 at 28 weeks gestation presenting with regular contractions every 4-5 minutes, cervix 2 cm dilated and 50% effaced.
Pharmacological Approach
- Tocolytic therapy: Nifedipine 20 mg orally, then 10-20 mg every 4-6 hours for 48 hours
- Alternative: Indomethacin 50 mg loading dose, then 25 mg every 6 hours for 48 hours (if <32 weeks and no contraindications)
- Antenatal corticosteroids: Betamethasone 12 mg IM, repeated in 24 hours
- Magnesium sulfate for neuroprotection: 4 g IV loading dose over 30 minutes, followed by 1 g/hour maintenance
- Antibiotic prophylaxis: If indicated based on Group B Streptococcus status or rupture of membranes
Nursing Considerations
- Monitor maternal vital signs closely, particularly blood pressure if using nifedipine
- Perform continuous electronic fetal monitoring
- Monitor for magnesium toxicity (assess deep tendon reflexes hourly, respiratory rate, level of consciousness)
- Monitor contraction frequency and duration
- Maintain strict intake and output records
- Administer betamethasone as scheduled
- Prepare for possible transfer to a facility with a NICU if not available
- Provide emotional support and education about preterm labor management
Scenario 3: Postpartum Hemorrhage Management
Patient: 32-year-old G3P3 who has delivered vaginally 20 minutes ago and is now experiencing heavy bleeding with a boggy uterus. Estimated blood loss: 800 mL.
Pharmacological Approach
- First-line: Oxytocin 10-40 units in 1000 mL of IV fluid, infused at 125-200 mL/hr
- Second-line (if bleeding continues): Methylergometrine (Methergine) 0.2 mg IM (if no hypertension or preeclampsia)
- Third-line (if bleeding continues): Carboprost
