Energy Metabolism
Comprehensive Notes for Nursing Students
Learning Objectives
- Understand energy units and their clinical significance
- Master Basal Metabolic Rate (BMR) concepts and calculations
- Identify factors affecting BMR in clinical practice
- Apply energy metabolism knowledge to patient care
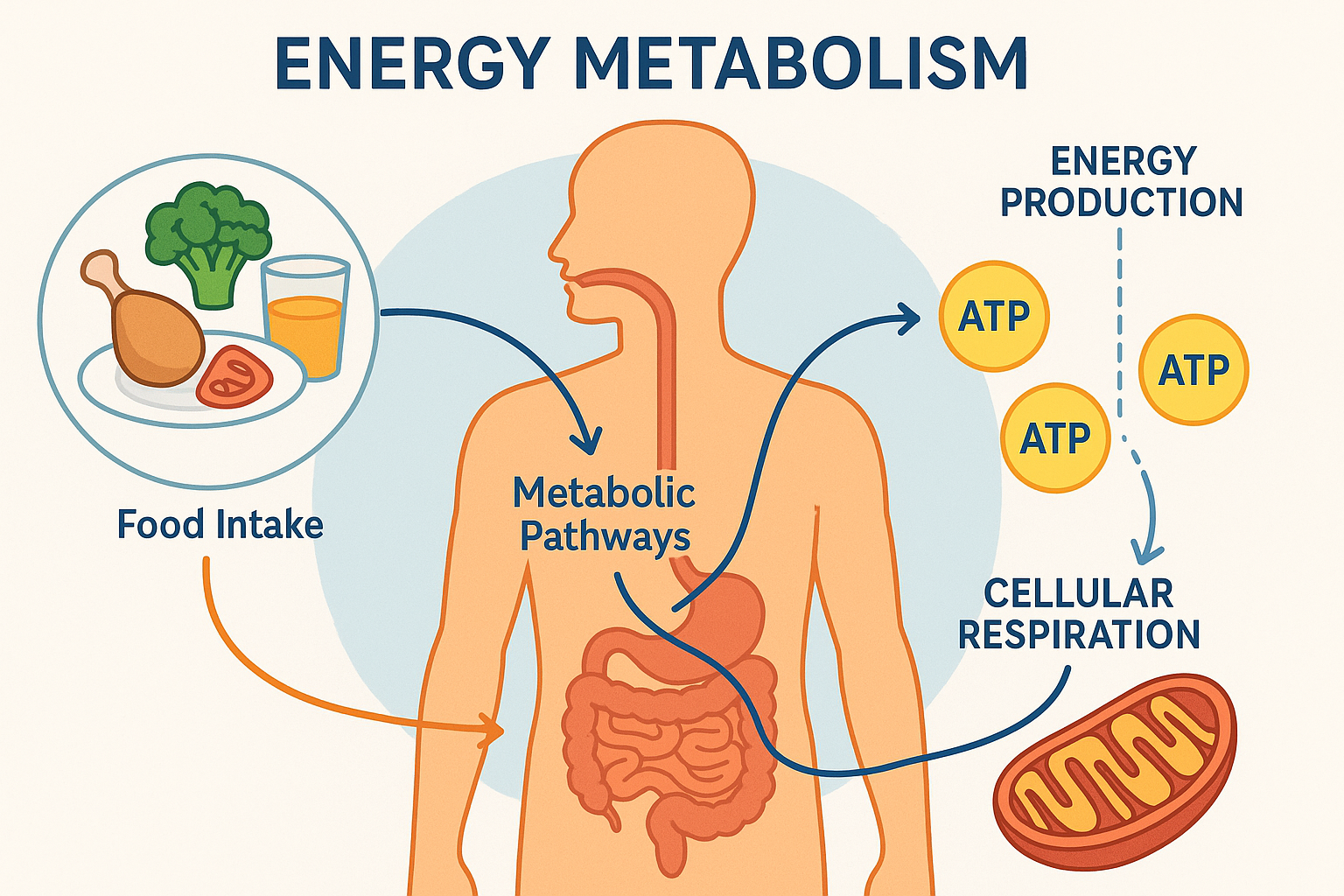
Energy metabolism pathways showing cellular respiration and ATP production
Introduction to Energy Metabolism
Energy metabolism is the cornerstone of human physiology, representing the complex network of biochemical processes that convert nutrients into usable energy. For nursing professionals, understanding energy metabolism is crucial for providing comprehensive patient care, from nutritional assessment to metabolic monitoring in critical care settings.
Energy serves as the fundamental currency of life, driving every cellular process from basic maintenance functions to complex physiological responses. In clinical practice, nurses encounter energy metabolism concepts daily through patient assessments, nutritional planning, wound healing evaluation, and management of metabolic disorders.
Energy Units: Understanding Kilocalories (kcal)
Key Concept
A kilocalorie (kcal) is the amount of energy required to raise the temperature of 1 kilogram of water by 1 degree Celsius. In nutrition and clinical practice, this unit measures the energy content of food and the energy expenditure of the human body.
Fundamental Energy Concepts
Energy cannot be created or destroyed, only transformed from one form to another. This fundamental principle, known as the First Law of Thermodynamics, governs all metabolic processes in the human body. Understanding this concept is essential for nurses working with patients who have metabolic disorders, nutritional deficiencies, or are in critical care situations.
Energy Conversion Formula
1 kcal = 4.184 kJ (kilojoules)
1 kcal = 4,184 J (joules)
Memory Aid: “HEAT”
H – Heat energy to warm water
E – Energy unit for nutrition
A – Assessment tool for metabolism
T – Temperature change measurement
Energy Content of Macronutrients
Carbohydrates
4 kcal/g
Primary energy source for brain and muscles
Proteins
4 kcal/g
Building blocks for tissue repair and maintenance
Fats
9 kcal/g
Concentrated energy storage and insulation
Clinical Nursing Application
When calculating nutritional needs for patients, remember that fats provide more than twice the energy per gram compared to carbohydrates and proteins. This is crucial for patients with limited intake capacity or those requiring high-calorie supplementation.
Energy Metabolism at the Cellular Level
At the cellular level, energy metabolism involves the conversion of chemical energy from food into adenosine triphosphate (ATP), the universal energy currency of cells. This process occurs through three main pathways: glycolysis, the citric acid cycle (Krebs cycle), and oxidative phosphorylation.
Cellular Energy Production Pathway
Cytoplasm • 2 ATP
Mitochondria • 2 ATP
Mitochondria • 32 ATP
Clinical Relevance: Energy Units in Practice
- Nutritional Assessment: Calculate daily caloric needs for patients
- Wound Healing: Increased energy demands require 1.5-2x normal intake
- Critical Care: Monitor energy expenditure in mechanically ventilated patients
- Diabetes Management: Carbohydrate counting and insulin dosing
- Weight Management: Energy balance for therapeutic interventions
Basal Metabolic Rate (BMR)
Key Concept
Basal Metabolic Rate (BMR) represents the minimum energy expenditure required to maintain vital physiological functions at rest. It accounts for 60-75% of total daily energy expenditure in healthy adults and serves as the foundation for all metabolic calculations in clinical practice.
Understanding BMR Fundamentals
BMR reflects the energy cost of maintaining essential cellular functions including protein synthesis, membrane transport, cardiovascular function, respiratory mechanics, and neurological activity. This measurement is obtained under standardized conditions: post-absorptive state (12-hour fast), thermoneutral environment, physical and emotional rest, and supine position.
BMR Memory Aid: “VITAL”
V – Vital organ function maintenance
I – Ion transport and cellular processes
T – Temperature regulation
A – ATP production for basic metabolism
L – Life-sustaining physiological processes
BMR vs. Related Concepts
Basal Metabolic Rate (BMR)
Measured under strict laboratory conditions
- • 12-hour fast
- • Supine position
- • Thermoneutral environment
- • Complete rest
Resting Energy Expenditure (REE)
Practical measurement in clinical settings
- • 4-6 hour fast
- • Seated or supine
- • Comfortable temperature
- • Quiet environment
BMR Calculation Methods
Harris-Benedict Equation (Original 1909)
Men: BMR = 66.47 + (13.75 × weight in kg) + (5.003 × height in cm) – (6.755 × age in years)
Women: BMR = 655.1 + (9.563 × weight in kg) + (1.850 × height in cm) – (4.676 × age in years)
Mifflin-St Jeor Equation (More Accurate)
Men: BMR = (10 × weight in kg) + (6.25 × height in cm) – (5 × age in years) + 5
Women: BMR = (10 × weight in kg) + (6.25 × height in cm) – (5 × age in years) – 161
BMR Distribution by Body System
Clinical Applications of BMR
In clinical practice, BMR calculations form the foundation for nutritional assessment, energy requirement estimation, and metabolic monitoring. Healthcare providers use BMR to develop individualized nutrition plans, assess metabolic dysfunction, and monitor treatment responses in various patient populations.
Nursing Practice Application
When using BMR calculations, multiply by activity factors: sedentary (1.2), lightly active (1.375), moderately active (1.55), very active (1.725), or extremely active (1.9). For hospitalized patients, consider stress factors for illness, surgery, or infection.
BMR Assessment Process
Step 1: Patient Assessment
- • Measure height and weight
- • Record age and gender
- • Note medical conditions
- • Assess activity level
Step 2: BMR Calculation
- • Apply appropriate equation
- • Consider body composition
- • Adjust for medications
- • Factor in disease states
Step 3: Activity Adjustment
- • Multiply by activity factor
- • Consider occupational demands
- • Account for exercise routine
- • Adjust for physical limitations
Step 4: Clinical Application
- • Develop nutrition plan
- • Monitor weight changes
- • Assess metabolic health
- • Adjust interventions
Clinical Scenarios: BMR Applications
Critical Care Patient
A 45-year-old male patient in ICU with sepsis requires 1.5-2.0x BMR due to increased metabolic demands from systemic inflammation and healing processes.
Geriatric Patient
An 80-year-old female with decreased muscle mass shows BMR reduction of 20-30% compared to younger adults, requiring adjusted nutritional planning.
Pediatric Patient
A 10-year-old child has BMR per kg body weight 2-3x higher than adults due to growth and development requirements.
Factors Affecting Basal Metabolic Rate
Key Concept
BMR is influenced by multiple intrinsic and extrinsic factors that can increase or decrease metabolic rate by 10-40%. Understanding these factors is crucial for accurate metabolic assessment and personalized patient care planning.
BMR Factors Mnemonic: “SHAPES”
S – Size and body composition
H – Hormones and health status
A – Age and gender
P – Physical activity and environment
E – Emotional state and medications
S – Sleep patterns and circadian rhythms
Intrinsic Factors
Body Size and Composition
Lean body mass is the strongest predictor of BMR, accounting for 60-70% of individual variation. Muscle tissue has high metabolic activity (13 kcal/kg/day) compared to adipose tissue (4.5 kcal/kg/day).
Clinical Implications:
- • Athletes with higher muscle mass have elevated BMR
- • Obesity may have proportionally lower BMR per kg body weight
- • Sarcopenia in elderly reduces BMR significantly
- • Body surface area correlates with heat production
Age and Gender
BMR decreases approximately 2-3% per decade after age 30, primarily due to loss of lean muscle mass and changes in organ function. Men typically have 10-15% higher BMR than women due to greater muscle mass and testosterone levels.
Age-Related Changes:
- • Infants: Highest BMR per kg (50-60 kcal/kg/day)
- • Children: Elevated BMR for growth and development
- • Adults: Peak BMR in 20s-30s, gradual decline
- • Elderly: 20-30% reduction due to sarcopenia
Genetics and Ethnicity
Genetic factors account for 25-40% of BMR variation between individuals. Ethnic differences in muscle fiber composition, enzyme activity, and metabolic efficiency contribute to BMR variations.
Genetic Influences:
- • Mitochondrial DNA variants affect energy production
- • Thyroid hormone receptor polymorphisms
- • Uncoupling protein gene variations
- • Familial clustering of metabolic rates
Hormonal Factors
Thyroid Hormones
Thyroid hormones (T3 and T4) are the primary regulators of BMR. Hyperthyroidism can increase BMR by 50-100%, while hypothyroidism can decrease it by 30-50%.
Thyroid Function and BMR:
- • T3 increases mitochondrial respiration
- • Stimulates Na+/K+ ATPase activity
- • Enhances protein synthesis and degradation
- • Affects cardiovascular and respiratory function
Other Hormones
Multiple hormones influence BMR through various mechanisms affecting cellular metabolism, protein synthesis, and energy utilization.
Hormonal Effects:
- • Growth Hormone: Increases BMR by 15-20%
- • Cortisol: Chronic elevation increases BMR
- • Insulin: Affects glucose metabolism efficiency
- • Catecholamines: Acute BMR increase (20-30%)
Environmental and Lifestyle Factors
Temperature
Environmental temperature significantly affects BMR through thermogenesis. Cold exposure increases BMR by 10-15%, while heat exposure can increase it by 5-10%.
Temperature Effects:
- • Shivering thermogenesis: immediate BMR increase
- • Non-shivering thermogenesis: brown fat activation
- • Vasoconstriction/vasodilation energy costs
- • Seasonal BMR variations (5-10% higher in winter)
Nutritional Status
Nutritional intake and status profoundly affect BMR. Caloric restriction can reduce BMR by 15-25%, while overfeeding can increase it by 10-15%.
Nutritional Influences:
- • Thermic effect of food: 8-10% of total energy expenditure
- • Starvation: BMR reduction as survival mechanism
- • Protein intake: Higher thermic effect than carbs/fats
- • Caffeine: Temporary BMR increase (5-10%)
Pathological Factors
Disease States
Various pathological conditions alter BMR through inflammatory responses, increased metabolic demands, and changes in organ function.
Disease Effects on BMR:
- • Fever: 13% increase per °C temperature rise
- • Cancer: 20-30% increase due to tumor metabolism
- • Sepsis: 50-100% increase from inflammatory response
- • COPD: 15-25% increase from work of breathing
BMR Variation by Age and Gender
Nursing Assessment: BMR Factors
When assessing patients, systematically evaluate factors affecting BMR:
- Measure height, weight, and body composition
- Review medication list for metabolic effects
- Assess thyroid function and hormone levels
- Consider environmental factors and stress levels
- Evaluate nutritional status and dietary patterns
Clinical Applications in Nursing Practice
Nutritional Assessment Protocol
Initial Assessment
- • Calculate BMR using appropriate equation
- • Assess activity level and stress factors
- • Review medical history and medications
- • Evaluate nutritional risk factors
Ongoing Monitoring
- • Monitor weight trends and body composition
- • Assess energy intake vs. expenditure
- • Evaluate metabolic response to interventions
- • Adjust nutritional plan based on outcomes
Special Populations
Critical Care Patients
Use indirect calorimetry when available. Apply stress factors: mild stress (1.2), moderate stress (1.3), severe stress (1.5), severe burns (2.0).
Geriatric Patients
Consider age-related BMR decline, medication effects, and comorbidities. Focus on maintaining muscle mass and preventing malnutrition.
Bariatric Patients
Use adjusted body weight calculations. Monitor for metabolic changes post-surgery and adjust nutritional support accordingly.
Key Takeaways for Nursing Practice
Essential Concepts
- Energy is measured in kilocalories (kcal)
- BMR represents minimum energy needs at rest
- Multiple factors influence individual BMR
- Clinical assessment requires systematic evaluation
Clinical Applications
- Nutritional assessment and planning
- Metabolic monitoring in acute care
- Patient education and counseling
- Interdisciplinary care coordination
References and Further Reading
• Cleveland Clinic. (2025). BMR (Basal Metabolic Rate): What It Is & How To Calculate It. https://my.clevelandclinic.org/health/body/basal-metabolic-rate-bmr
• NCBI. (2024). Factors Affecting Energy Expenditure and Requirements. https://www.ncbi.nlm.nih.gov/books/NBK591031/
• Osmosis. (2025). Cellular Respiration: Steps, Process, and Stages. https://www.osmosis.org/answers/cellular-respiration
• StatPearls. (2024). Physiology, Adenosine Triphosphate. https://www.ncbi.nlm.nih.gov/books/NBK553175/
