Fetal Engagement in Late Pregnancy
Comprehensive Nursing Notes
Table of Contents
Introduction to Fetal Engagement
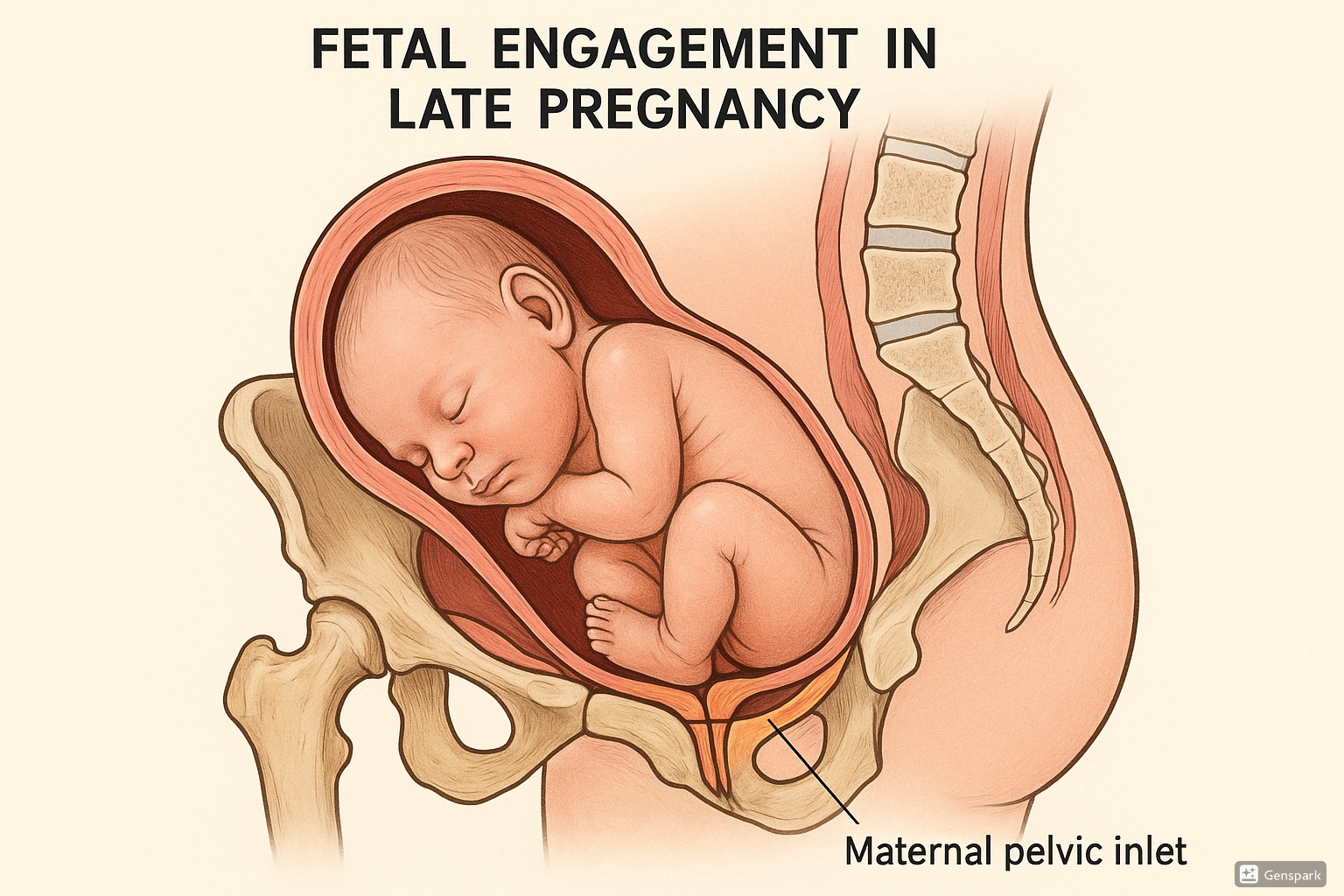
Fetal engagement refers to the descent of the presenting part of the fetus (typically the head) into the maternal pelvis. This critical process usually occurs during the later stages of pregnancy, approximately 2-4 weeks before term in nulliparous women (first-time mothers). In multiparous women (those who have given birth previously), engagement may not occur until labor begins.
The process of engagement represents an important milestone in pregnancy as it signals that the fetus is properly positioned for delivery and that the maternal pelvis is likely adequate for vaginal birth. Understanding fetal engagement is essential for nursing assessment and care planning in late pregnancy.
Key Point:
Engagement is officially defined as the descent of the widest diameter of the presenting part to a level at or below the plane of the pelvic inlet.
Anatomical Considerations
To properly understand fetal engagement, nurses must be familiar with the relevant anatomy:
Maternal Pelvic Anatomy
| Pelvic Component | Description | Relevance to Engagement |
|---|---|---|
| Pelvic Inlet | The superior opening of the pelvis, bordered by the sacral promontory, linea terminalis, and pubic symphysis | The plane through which initial engagement occurs |
| Pelvic Cavity | The space between the inlet and outlet | Accommodates the fetal head during engagement |
| Ischial Spines | Bony projections that mark the narrowest part of the pelvic cavity | Reference points for assessing fetal station |
| Pelvic Outlet | The inferior opening of the pelvis | The final path for fetal descent during delivery |
Fetal Head Dimensions
The fetal head has several important diameters that influence the engagement process:
- Biparietal Diameter (BPD): The widest transverse diameter of the fetal head, typically 9.5-10.5 cm at term
- Occipitofrontal Diameter: From the occiput to the forehead, typically 12 cm at term
- Suboccipitobregmatic Diameter: From below the occiput to the anterior fontanelle, typically 9.5 cm at term (important in flexed head position)
Clinical Insight:
For successful engagement to occur, the presenting part of the fetus must be able to navigate through the pelvic inlet. The relationship between fetal head dimensions and maternal pelvic measurements is a crucial factor in determining whether engagement can occur naturally.
Mechanism of Engagement
Fetal engagement involves several coordinated processes:
Factors Influencing Engagement
- Fetal Head Flexion: As the fetal head flexes, the smaller suboccipitobregmatic diameter presents to the pelvic inlet, facilitating engagement.
- Uterine Contractions: Even Braxton Hicks contractions in late pregnancy help direct the fetal head toward the pelvis.
- Maternal Pelvic Architecture: The shape and dimensions of the maternal pelvis influence when and how engagement occurs.
- Fetal Position: Occiput anterior positions typically engage more easily than posterior or transverse positions.
- Gravity: Maternal upright positions help the fetal head descend into the pelvis.
The process of engagement is often accompanied by what mothers describe as “lightening” or “dropping” – a sensation that the baby has moved lower in the pelvis, often resulting in reduced pressure on the diaphragm but increased pressure on the bladder.
Engagement Timeline:
In nulliparas (first-time mothers): Typically occurs 2-4 weeks before term
In multiparas (women who have given birth before): May not occur until labor begins
Assessment of Fetal Engagement
Nurses must be proficient in assessing fetal engagement through both abdominal and vaginal examinations. These skills are essential for monitoring the progress of late pregnancy and labor.
Abdominal Examination
The abdominal examination for assessing engagement includes the following techniques:
Pawlik’s Maneuver (Pawlik’s Grip)
- Place hands on either side of the lower maternal abdomen
- Gently attempt to move the presenting part side to side
- If engaged, the presenting part will have limited mobility
- If not engaged, the presenting part will move freely
Fifth Leopold’s Maneuver
- With the patient in a supine position, face the patient’s feet
- Place the first finger of each hand on either side of the midline just above the symphysis pubis
- Press down gently toward the pelvis
- If the fetal head is not engaged, the fingers will readily meet
- If engaged, the fingers will be separated by the fetal head
Vaginal Examination
The most accurate method of assessing engagement is through vaginal examination, which provides information about:
- Station: The relationship of the presenting part to the ischial spines
- Degree of Molding: Overlapping of cranial bones that may indicate engagement against resistance
- Presence of Caput Succedaneum: Soft tissue swelling that may develop during prolonged engagement
Important Nursing Consideration:
Vaginal examinations should be performed only when clinically indicated to reduce the risk of introducing infection. Proper hand hygiene and aseptic technique are essential.
Fetal Stations
Fetal station refers to the relationship between the presenting part (typically the fetal head) and the ischial spines of the maternal pelvis. The station system provides a standardized way to describe the degree of engagement and subsequent descent.
| Station | Description | Clinical Significance |
|---|---|---|
| -5 to -1 | Above the ischial spines | Not fully engaged; may indicate early labor or pre-labor |
| 0 | At the level of the ischial spines | Considered “engaged” in most definitions |
| +1 to +5 | Below the ischial spines | Progressive descent during labor; +3 or more typically indicates imminent delivery |
Definition of Engagement:
In obstetric practice, true engagement is considered to have occurred when the widest diameter of the presenting part has passed through the pelvic inlet. This typically corresponds to station 0 or below.
Types of Engagement
Fetal engagement can occur in different patterns, each with clinical implications:
| Type of Engagement | Description | Clinical Implications |
|---|---|---|
| Early Engagement | Occurs weeks before due date (common in nulliparas) |
– May indicate favorable pelvic architecture – Often results in early lightening symptoms – Generally a positive sign for labor progression |
| Late Engagement | Occurs during early labor (common in multiparas) |
– Normal variation in multiparous women – May delay recognition of true labor – Can lead to rapid labor once engagement occurs |
| Deep Engagement | Head descends well below the ischial spines before labor |
– May lead to increased bladder pressure and discomfort – Generally indicates good pelvic adequacy – Can result in shorter first stage of labor |
| Non-engagement | Failure of the presenting part to engage by term or early labor |
– May indicate cephalopelvic disproportion – Could suggest malpresentation – May necessitate cesarean delivery – Requires careful monitoring |
Clinical Note:
The pattern and timing of engagement provide valuable clinical information about potential labor progression and possible complications. Nurses should document engagement status during each assessment in late pregnancy and labor.
Clinical Significance of Fetal Engagement
Understanding fetal engagement has several important clinical applications:
Maternal Signs and Symptoms Related to Engagement
- Lightening: Descent of the uterus, leading to easier breathing but increased urinary frequency
- Increased Pelvic Pressure: Pressure sensations in the lower back, pelvis, and perineum
- Wadding Gait: Changes in walking pattern due to pressure on pelvic ligaments
- Increased Urinary Frequency: Due to greater pressure on the bladder
- Improved Respiratory Function: As pressure on the diaphragm decreases
- Leg Edema or Varicosities: May worsen due to increased pelvic pressure
Prognostic Value
Fetal engagement provides important information about:
- Labor Readiness: Engagement often indicates the body is preparing for labor
- Pelvic Adequacy: Successful engagement suggests the pelvis is likely adequate for vaginal birth
- Labor Duration: Early engagement in nulliparas often correlates with shorter first stage of labor
- Need for Intervention: Non-engagement at term may indicate the need for closer monitoring or intervention
Nursing Pearl:
When a nulliparous patient reports relief from shortness of breath but complains of increased urinary frequency around 36-38 weeks, suspect engagement has occurred. This is an ideal time to review signs of labor and preparation for birth.
Potential Complications Related to Fetal Engagement
While engagement is a normal physiological process, several complications can occur:
Delayed or Failed Engagement
Possible causes include:
- Cephalopelvic Disproportion (CPD): Mismatch between fetal head size and maternal pelvis
- Fetal Malpresentation: Such as breech, face, or brow presentation
- Placenta Previa: Low-lying placenta blocking the birth canal
- Uterine Abnormalities: Such as fibroids or uterine anomalies
- Multiple Gestation: Twins or higher-order multiples
- Polyhydramnios: Excessive amniotic fluid reducing descent
Complications of Abnormal Engagement
| Condition | Description | Nursing Implications |
|---|---|---|
| Asynclitism | Lateral tilting of the fetal head, causing one parietal bone to present first |
– May delay engagement or cause arrest of descent – Requires careful monitoring during labor – May benefit from position changes |
| Persistent Occiput Posterior | Fetal head engages with occiput facing maternal sacrum |
– Associated with prolonged labor and back pain – Increased risk of operative delivery – Position changes may help rotation |
| Deep Transverse Arrest | Fetal head engages but becomes stuck in transverse position |
– Often requires instrumental delivery or cesarean – May indicate anthropoid pelvis – Close monitoring for fetal distress |
| Cord Prolapse Risk | Higher risk when presenting part not well engaged |
– Caution with amniotomy if head high – Emergency preparedness – Vigilance during labor |
Critical Assessment:
Non-engagement at 40 weeks in a nulliparous woman should prompt thorough evaluation for potential cephalopelvic disproportion or malpresentation. Advanced maternal age, history of pelvic injury, and maternal short stature are risk factors that warrant particular attention.
Nursing Interventions Related to Fetal Engagement
Nurses play a crucial role in assessment, education, and care related to fetal engagement:
Assessment Interventions
- Perform regular abdominal examinations to track engagement progression
- Document station accurately during vaginal examinations
- Monitor maternal vital signs and fetal heart rate patterns
- Assess for signs of labor onset in relation to engagement status
- Evaluate maternal comfort and address increasing pressure symptoms
Patient Education
- Explain the meaning of lightening and increased pelvic pressure
- Teach positions that may facilitate engagement (forward leaning, squatting)
- Review signs of labor in relation to engagement status
- Provide guidance on managing increased urinary frequency
- Explain the significance of engagement in the birth process
- Discuss when to contact healthcare providers based on symptoms
Supportive Interventions
| Maternal Symptom | Nursing Intervention |
|---|---|
| Increased pelvic pressure |
– Recommend pelvic support belt – Suggest periods of rest with elevated legs – Teach pelvic tilt exercises – Recommend warm baths |
| Urinary frequency |
– Encourage adequate hydration despite frequency – Suggest voiding on schedule rather than waiting – Teach pelvic floor exercises – Monitor for signs of urinary tract infection |
| Lower back pain |
– Demonstrate safe stretching exercises – Recommend heat/cold therapy – Suggest side-lying position for rest – Teach partner massage techniques |
| Sleep disturbance |
– Recommend supportive pillows – Suggest left lateral positioning – Teach relaxation techniques – Address anxiety about impending labor |
Nursing Consideration:
For patients showing signs of engagement but experiencing significant discomfort, maternal positioning can make a significant difference. Side-lying with pillows between the knees, gentle pelvic rocking, and prenatal yoga poses can help redistribute pressure.
Helpful Mnemonics for Fetal Engagement
Mnemonics can aid in remembering key concepts related to fetal engagement:
ENGAGED
E – Examine abdominal contour for lightening
N – Note the presenting part in relation to ischial spines
G – Gauge mobility using Pawlik’s grip
A – Assess maternal symptoms (breathing ease, urinary frequency)
G – Guide patients on expected symptoms and self-care
E – Evaluate for potential complications
D – Document findings accurately
STATION
S – Spines (ischial) are the reference point (station 0)
T – Tracking descent is critical for labor progress
A – Above spines: negative numbers (-1 to -5)
T – True engagement occurs at station 0 or below
I – Increments of centimeters measure station
O – Occiput position affects engagement pattern
N – Nulliparas typically engage before labor
PELVIS
P – Presenting part must fit through the inlet
E – Engagement status provides clues about adequacy
L – Landmarks (ischial spines) guide assessment
V – Variations in pelvic types affect engagement
I – Inlet diameter must accommodate fetal head
S – Shape matters: gynecoid is most favorable
Global Practices Related to Fetal Engagement
Different cultures and healthcare systems have various approaches to monitoring and promoting fetal engagement:
Traditional Practices
- Japanese Maternity Belt (Sarashi): Traditional abdominal binding believed to support proper fetal positioning
- Mayan Abdominal Massage: External manipulation technique aimed at optimizing fetal position
- Traditional Indian Squatting: Regular squatting in late pregnancy to facilitate engagement through gravity and pelvic opening
- African Birth Stools: Designed to facilitate gravity-assisted engagement and descent
Contemporary Global Approaches
| Practice/Region | Description | Evidence/Considerations |
|---|---|---|
| UK Midwifery Practices | Less emphasis on numerical stations; focus on “fifths palpable” abdominal assessment |
– Reduces vaginal examinations – Promotes non-invasive monitoring – Based on extensive midwifery tradition |
| Dutch Home Birth Model | Emphasizes maternal positioning and movement to facilitate natural engagement |
– High rate of successful home births – Focus on physiological processes – Careful risk assessment |
| Scandinavian Approach | Integration of physiotherapy techniques to optimize pelvic biomechanics |
– Includes pelvic floor preparation – Addresses pelvic alignment – Multidisciplinary collaboration |
| Brazilian Rebozo Technique | Gentle rhythmic movements using a traditional scarf to relax pelvic muscles and facilitate optimal fetal positioning |
– Non-invasive intervention – Growing anecdotal support – Limited formal research |
Evidence-Based Practice:
While various cultural practices exist to promote engagement, research consistently supports that maternal position changes, especially those that utilize gravity and pelvic mobility, can facilitate engagement. Implementing these practices in nursing care can promote physiological birth processes.
