Fetal Monitoring and First Stage Labor Care
Comprehensive Nursing Notes in Osmosis Style
Table of Contents
Introduction
Fetal monitoring is a crucial aspect of perinatal care that involves assessment and surveillance of fetal health during pregnancy and labor. For nursing students, understanding the principles and techniques of fetal monitoring is essential for providing evidence-based care and ensuring optimal outcomes for both mother and baby. This comprehensive guide focuses on the methods for assessing fetal well-being and providing appropriate nursing care during the first stage of labor.
As a nurse, your ability to properly interpret fetal monitoring data and respond appropriately can significantly impact maternal and neonatal outcomes. This resource aims to provide you with evidence-based knowledge and practical skills needed for effective fetal monitoring and first stage labor management.
Assessing and Monitoring Fetal Well-being
Antenatal Fetal Surveillance
Antenatal fetal surveillance involves various testing modalities to assess fetal well-being before labor begins. These methods are particularly important for high-risk pregnancies but may be utilized in any pregnancy where concerns about fetal health arise.
| Method | Description | Nursing Considerations |
|---|---|---|
| Maternal Perception of Fetal Movement (Kick Counts) | Patient monitors and records fetal movements, typically aiming for at least 10 movements within a 2-hour period | Educate mothers to contact healthcare provider if fewer than 10 movements in 2 hours or significant decrease in movement patterns |
| Nonstress Test (NST) | Electronic monitoring of fetal heart rate response to fetal movement over at least 20 minutes | Reactive NST shows at least two accelerations of 15 beats/min lasting 15 seconds within a 20-minute period |
| Biophysical Profile (BPP) | Combines NST with ultrasound assessment of fetal breathing movements, fetal body/limb movements, fetal tone, and amniotic fluid volume | Score of 8-10/10 is considered normal; scores below 6 may indicate need for delivery |
| Modified BPP | Combines NST with assessment of amniotic fluid volume (deepest vertical pocket) | Simplified version of BPP; normal result includes reactive NST and AFI ≥5 cm |
| Contraction Stress Test (CST) | Evaluates FHR response to uterine contractions to detect late decelerations | Negative CST (no late decelerations) is reassuring; positive CST may indicate uteroplacental insufficiency |
| Umbilical Artery Doppler Velocimetry | Ultrasound assessment of blood flow in umbilical artery | Primarily used in suspected fetal growth restriction; assesses placental function |
Memory Aid: “BANFM” for Antenatal Fetal Assessment
- Biophysical Profile (5 components)
- Amniotic fluid assessment
- Nonstress Test (reactivity)
- Fetal movement counts
- Modified BPP (NST + AFI)
Intrapartum Fetal Monitoring
During labor, fetal monitoring becomes critical for assessing how the fetus is tolerating the stress of contractions and the birth process. There are two primary approaches to intrapartum fetal monitoring:
1. Intermittent Auscultation (IA)
Intermittent auscultation involves periodically listening to the fetal heart rate using a fetoscope, Doppler device, or ultrasound transducer. This method is recommended for low-risk pregnancies by many organizations including the World Health Organization (WHO).
- Frequency:
- First stage (latent phase): Every 30 minutes
- First stage (active phase): Every 15-30 minutes
- Second stage: Every 5-15 minutes
- Assessment timing: Listen before, during, and after a contraction for at least 60 seconds
- Documentation: Record baseline rate, rhythm, and presence of accelerations or decelerations
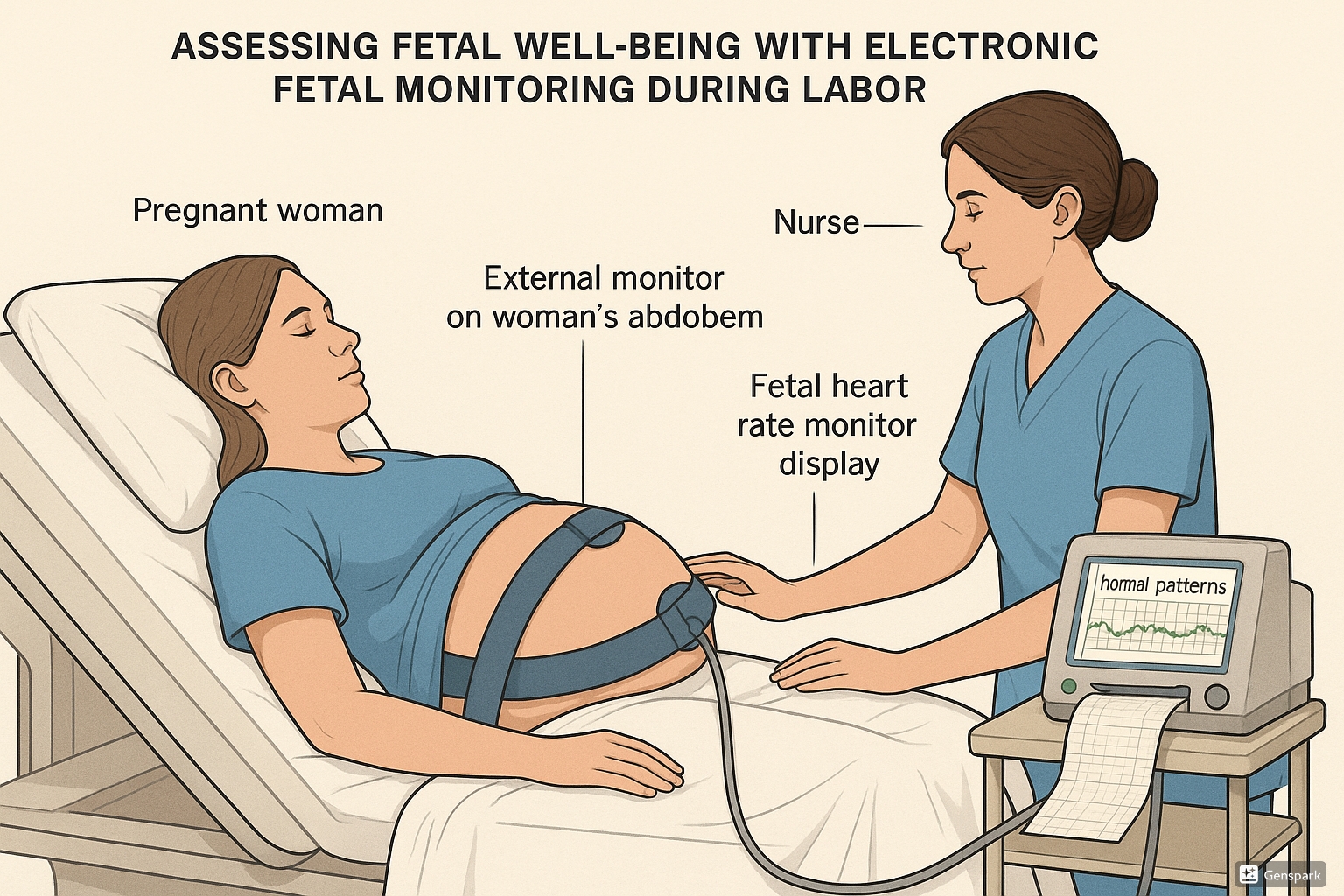
2. Electronic Fetal Monitoring (EFM)
Electronic fetal monitoring, or cardiotocography (CTG), provides continuous recording of both the fetal heart rate and uterine contractions. This approach is commonly used in high-risk pregnancies and in many hospital settings for all laboring women.
Evidence-Based Practice: When to Use Continuous EFM
According to current guidelines, continuous electronic fetal monitoring is recommended for pregnancies with:
- Previous cesarean delivery
- Preeclampsia or hypertension
- Intrauterine growth restriction
- Preterm labor
- Multiple gestation
- Meconium-stained amniotic fluid
- Abnormalities detected during intermittent auscultation
- Induction or augmentation of labor
External vs. Internal Fetal Monitoring
| Feature | External Monitoring | Internal Monitoring |
|---|---|---|
| Method | Ultrasound transducer placed on maternal abdomen | Fetal scalp electrode attached directly to fetal scalp |
| Requirements | No specific prerequisites | Requires ruptured membranes and cervical dilation |
| Accuracy | May lose contact with movement; can confuse maternal and fetal heart rates | More accurate and continuous signal; direct fetal ECG |
| Invasiveness | Non-invasive | Invasive; small risk of infection or scalp injury |
| Mobility | Allows more mobility; wireless options available | Restricts mobility |
| Best for | Early labor, intact membranes, maternal obesity | When external monitoring is inadequate or precise data is needed |
Memory Aid: “FACE” Comparing External vs. Internal Monitoring
- Flexibility: External offers more
- Accuracy: Internal provides greater precision
- Conditions: Internal requires ruptured membranes
- Easiness: External is easier to apply and non-invasive
Fetal Heart Rate Interpretation
Proper interpretation of fetal heart rate patterns is crucial for assessing fetal well-being during labor. The NICHD (National Institute of Child Health and Human Development) terminology is used to standardize FHR interpretation.
Key Components of FHR Assessment:
- Baseline Rate: The average FHR rounded to increments of 5 beats per minute during a 10-minute window
- Normal: 110-160 beats per minute (bpm)
- Tachycardia: >160 bpm
- Bradycardia: <110 bpm
- Baseline Variability: Fluctuations in the baseline FHR
- Absent: Undetectable
- Minimal: ≤5 bpm
- Moderate (normal): 6-25 bpm
- Marked: >25 bpm
- Accelerations: Transient increases in FHR
- ≥15 bpm above baseline for ≥15 seconds
- Reassuring sign of fetal well-being
- Decelerations: Transient decreases in FHR
- Early: Uniform, gradual decrease with onset and return that mirrors contraction timing
- Late: Gradual decrease with onset, lowest point, and recovery occurring after the beginning, peak, and end of contraction
- Variable: Abrupt decrease with rapid onset and return; variable in duration and timing
- Prolonged: Decrease from baseline for >2 minutes but <10 minutes
| FHR Category | Characteristics | Management Implications |
|---|---|---|
| Category I (Normal) |
|
Routine monitoring; no specific action needed |
| Category II (Indeterminate) |
|
Continued observation, evaluation, and surveillance; consider corrective measures |
| Category III (Abnormal) |
|
Prompt evaluation and intervention; prepare for possible rapid delivery if pattern doesn’t resolve |
Memory Aid: “VAIL” for FHR Assessment Components
- Variability: Fluctuations in baseline
- Accelerations: Transient increases in FHR
- Initial baseline rate: Normal (110-160 bpm)
- Lows (Decelerations): Early, late, variable, prolonged
Critical Considerations in FHR Interpretation
Remember that FHR patterns must be interpreted in the context of the clinical situation, including:
- Gestational age
- Medication effects (e.g., opioids, regional anesthesia)
- Maternal fever or infection
- Maternal position
- Stage and phase of labor
- Previous FHR patterns
Care During First Stage of Labor
Phases of First Stage Labor
The first stage of labor begins with the onset of regular uterine contractions that cause cervical change and ends with full cervical dilation to 10 cm. This stage is divided into two phases:
| Phase | Cervical Dilation | Characteristics | Duration |
|---|---|---|---|
| Latent Phase | 0 cm to 6 cm |
|
|
| Active Phase | 6 cm to 10 cm |
|
|
Memory Aid: “6-1-2” Rule for Active Labor
Active labor begins at 6 cm dilation, with expected progression of 1 cm/hr for nulliparous women and 2 cm/hr for multiparous women.
Nursing Interventions During First Stage Labor
The nurse’s role during the first stage of labor is multifaceted, including assessment, monitoring, support, and documentation.
Initial Assessment and Admission
- Obstetric Triage: Obtain presenting symptoms, vital signs, FHR, and contraction patterns
- Review Prenatal Record: Medical, surgical, obstetric history and laboratory results
- Admission History: Complete thorough assessment including medical, surgical, obstetric/gynecologic, and psychosocial history
- Physical Examination:
- General survey and vital signs
- Heart, lung, and extremity assessment
- Obstetric examination: FHR, contractions, membrane status
- Vaginal examination: cervical dilation, effacement, position, station, and presenting part
Ongoing Monitoring During First Stage
| Assessment Parameter | Frequency (Latent Phase) | Frequency (Active Phase) |
|---|---|---|
| Maternal Vital Signs | Every 60 minutes | Every 30-60 minutes |
| Fetal Heart Rate (Intermittent) | Every 30 minutes | Every 15-30 minutes |
| Fetal Heart Rate (Continuous) | Continuous with evaluation every 30 minutes | Continuous with evaluation every 15 minutes |
| Contraction Pattern | Every 30-60 minutes | Every 15-30 minutes |
| Cervical Examination | As indicated by labor progress | Every 2-4 hours or as indicated |
| Pain Assessment | Hourly or as needed | Every 30 minutes or as needed |
| Bladder Status | Every 2 hours | Every 1-2 hours |
Documentation Requirements
- Maternal vital signs and condition
- FHR baseline, variability, accelerations, and decelerations
- Contraction frequency, duration, and intensity
- Cervical changes and fetal descent
- Interventions and patient response
- Pain level and comfort measures provided
- Intake and output
- Medications administered
Comfort Measures During First Stage Labor
Providing comfort during the first stage of labor is essential for promoting a positive birth experience and supporting physiologic birth processes.
Non-Pharmacological Pain Management
- Breathing Techniques: Patterned breathing helps with relaxation and distraction from pain
- Hydrotherapy: Shower or bath can reduce pain perception and promote relaxation
- Massage: Counter-pressure on the sacrum can alleviate back pain during contractions
- Heat/Cold Therapy: Warm compresses for back pain, cool cloths for face/neck
- Relaxation Techniques: Guided imagery, music therapy, or meditation
- Birthing Ball: Promotes optimal fetal positioning and relieves pressure
- TENS (Transcutaneous Electrical Nerve Stimulation): May reduce pain perception in early labor
- Sterile Water Injections: For severe back pain, can provide 60-90 minutes of relief
Pharmacological Pain Management
- Systemic Analgesics: Opioids like fentanyl or morphine for short-term relief
- Nitrous Oxide: Self-administered 50/50 mixture with oxygen
- Regional Anesthesia:
- Epidural: Most common method; continuous infusion of local anesthetic
- Combined Spinal-Epidural: Faster onset than epidural alone
Memory Aid: “COMFORT” for Labor Support Interventions
- Communication: Clear, supportive information
- Options: Provide choices for pain management
- Mobility: Encourage position changes
- Fluids and nutrition: Maintain hydration and energy
- Ongoing assessment: Regular evaluation of pain and coping
- Relaxation techniques: Breathing, visualization
- Therapeutic touch: Massage, counter-pressure
Position Changes and Mobility
Promoting mobility and frequent position changes during the first stage of labor has numerous benefits including enhanced comfort, improved maternal-fetal circulation, and more efficient labor progress.
Benefits of Upright Positions and Mobility
- Uses gravity to assist fetal descent
- Reduces pain perception
- Improves uterine blood flow
- Increases intensity and efficiency of contractions
- May shorten first stage labor duration
- Reduces need for augmentation
- Facilitates fetal rotation through pelvis
Recommended Positions During First Stage
- Walking/Standing: Uses gravity; can lean on partner or wall during contractions
- Sitting: On birthing ball, chair, or bed; promotes relaxation between contractions
- Hands and Knees: Relieves back pain; aids rotation of occiput posterior positions
- Side-lying: Promotes rest while maintaining good uterine perfusion
- Semi-sitting: Comfortable position that still uses some gravity advantage
- Leaning Forward: Standing or kneeling while leaning on bed/partner reduces back pain
- Squatting: Increases pelvic diameter; may be used intermittently
Evidence-Based Practice: Position Changes
Research shows that changing positions every 30 minutes during the first stage of labor can:
- Reduce labor duration by approximately 20-30 minutes
- Improve maternal comfort and satisfaction
- Reduce abnormal fetal heart rate patterns
- Decrease need for augmentation
Even with regional anesthesia, position changes should be facilitated every 1-2 hours.
Best Practices and Recent Updates in Fetal Monitoring
1. Intermittent Auscultation for Low-Risk Labors
The latest research and guidelines from organizations including WHO, ACOG, and NICE support intermittent auscultation as the preferred monitoring method for low-risk labors. This approach is associated with reduced intervention rates (including cesarean deliveries) while maintaining equivalent neonatal outcomes compared with continuous electronic monitoring.
Key implementation: Develop standardized protocols and training programs for intermittent auscultation to ensure consistent application and interpretation.
2. Computerized FHR Interpretation Systems
Newer technological advances include computerized analysis systems for electronic fetal monitoring that apply algorithms to identify concerning patterns and reduce inter-observer variability in interpretation. These systems can provide decision support to clinicians but should not replace clinical judgment.
Key implementation: When available, use computerized systems as an adjunct to, not a replacement for, trained clinical assessment. Ensure all users understand the limitations of automated interpretation.
3. Standardized Approach to Category II FHR Patterns
Recent updates emphasize standardized approaches to the management of Category II FHR patterns, which comprise approximately 80% of all tracings. Evidence-based algorithms now include:
- Maternal repositioning (especially left lateral)
- Intravenous fluid bolus
- Reducing or discontinuing oxytocin if being administered
- Amnioinfusion for variable decelerations with suspected cord compression
- Consideration of tocolytics for tetanic contractions
- Oxygen administration only if indicated by maternal hypoxemia
Key implementation: Develop unit-specific protocols for Category II management with defined escalation pathways.
Memory Aids for Fetal Monitoring and Labor Care
“DR C BRAVADO” for FHR Assessment
- Determine risk factors
- Rate baseline
- Calculate variability
- Bradycardia or tachycardia present?
- Reassuring accelerations?
- Absent accelerations?
- Variable decelerations?
- Average variability?
- Decelerations (late)?
- Overall impression
“ABCDE” Response to Abnormal FHR Patterns
- Alter maternal position (usually left lateral)
- Bolus with IV fluids
- Cease oxytocin if running
- Determine cause and document
- Evaluate oxygen administration (if indicated)
“SBAR” for Communication About Concerning FHR Patterns
- Situation: Briefly state the current issue with the FHR
- Background: Provide relevant patient history and labor progress
- Assessment: Your analysis of the FHR pattern and clinical situation
- Recommendation: Suggest action steps based on protocol
“4 P’s” for Labor Progress Assessment
- Powers: Strength, frequency, and duration of contractions
- Passage: Maternal pelvic capacity and dimensions
- Passenger: Fetal size, presentation, and position
- Psyche: Maternal psychological status and coping
References
- American College of Obstetricians and Gynecologists. (2021). Antepartum Fetal Surveillance. ACOG Practice Bulletin No. 229. Obstetrics & Gynecology, 137(6), e177-e197.
- American College of Obstetricians and Gynecologists. (2020). Intrapartum Fetal Heart Rate Monitoring: Nomenclature, Interpretation, and General Management Principles. ACOG Practice Bulletin No. 207. Obstetrics & Gynecology, 135(5), e112-e126.
- National Institute for Health and Care Excellence. (2023). Fetal monitoring in labour. NICE Guideline 229.
- World Health Organization. (2018). WHO recommendations: intrapartum care for a positive childbirth experience. World Health Organization.
- Miller, L.A., Miller, D.A., & Cypher, R.L. (2022). Mosby’s pocket guide to fetal monitoring: A multidisciplinary approach (9th ed.). Elsevier.
- Freeman, R.K., Garite, T.J., Nageotte, M.P., & Miller, L.A. (2021). Fetal heart rate monitoring (5th ed.). Wolters Kluwer Health.
- Lawrence, A., Lewis, L., Hofmeyr, G. J., & Styles, C. (2013). Maternal positions and mobility during first stage labour. Cochrane Database of Systematic Reviews, (10), CD003934.
- Alfirevic, Z., Devane, D., Gyte, G. M., & Cuthbert, A. (2017). Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database of Systematic Reviews, (2), CD006066.
