Foetal Distress
Comprehensive Nursing Notes
Table of Contents
Definition and Terminology
Foetal distress refers to a condition where the foetus shows signs of compromise due to inadequate oxygen or nutrient supply. This term has been traditionally used to describe when the foetus does not receive adequate amounts of oxygen during pregnancy or labor.
Modern obstetric practice has largely replaced the term “foetal distress” with “non-reassuring foetal status” (NRFS) as it provides a more precise description of the concerning findings without implying a definitive diagnosis of foetal compromise.
Synonyms include:
- Foetal compromise
- Non-reassuring foetal heart rate trace
- Foetal intolerance to labor
Foetal distress represents an emergency condition that requires immediate attention and often intervention to prevent adverse outcomes. The condition can occur during pregnancy, but is most commonly identified during labor and delivery when continuous foetal monitoring is in place.
Pathophysiology
The pathophysiology of foetal distress centers on insufficient oxygen supply to the foetus, which can lead to hypoxia, acidemia, and potentially irreversible damage if prolonged. Understanding the underlying mechanisms is crucial for appropriate nursing assessment and interventions.
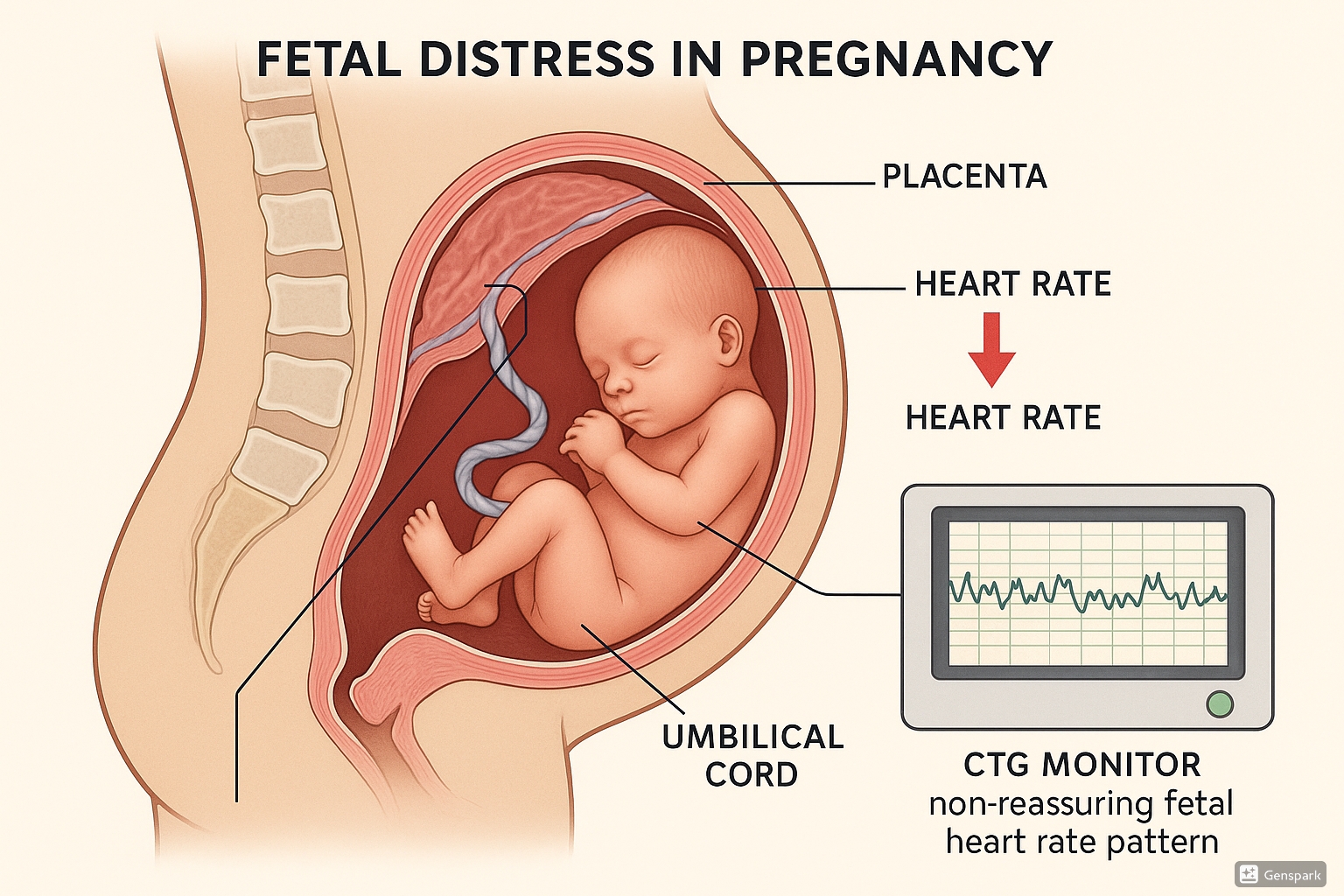
Figure 1: Anatomical representation of foetal distress showing compromised oxygen supply and monitoring
Primary Pathophysiological Mechanisms
1. Uteroplacental Insufficiency
This is the most common cause of antepartum foetal distress, occurring when blood flow through the placenta is compromised, reducing oxygen exchange between maternal and foetal circulation.
2. Umbilical Cord Compression
Compression of the umbilical cord restricts blood flow to and from the foetus, leading to rapid onset of hypoxemia. When cord compression occurs:
- Initially, the umbilical vein (carrying oxygenated blood to the foetus) is compressed
- This causes decreased foetal preload to the heart
- A baroreceptor-mediated reflex tachycardia occurs
- Subsequently, increased foetal blood pressure in the carotids triggers vagal stimulation
- This vagal response slows the heart rate, causing bradycardia
- When compression is relieved, heart rate typically returns to baseline
3. Head Compression
During labor, compression of the foetal head can trigger a physiological response:
- Increased intracranial pressure (Cushing response)
- Decreased cerebral blood flow
- Vagal activation leading to temporary bradycardia
- This typically corresponds with contractions and resolves as the contraction ends
4. Placental Dysfunction
Various conditions can compromise placental function:
- Placental abruption (premature separation from uterine wall)
- Placenta previa (placenta covering the cervical os)
- Placental insufficiency due to maternal hypertensive disorders
- Maternal vascular disease affecting uteroplacental perfusion
Foetal Response to Hypoxia
When oxygen supply becomes insufficient, the foetus undergoes a series of physiological adaptations:
| Stage | Physiological Response | Clinical Manifestations |
|---|---|---|
| Initial Compensation |
|
|
| Progressive Hypoxemia |
|
|
| Decompensation |
|
|
The progression from compensated to decompensated state can occur rapidly, particularly during labor when the foetus is subjected to additional stressors such as contractions that temporarily reduce uteroplacental blood flow.
Risk Factors
Several maternal, foetal, and placental factors increase the risk of foetal distress. Identifying these risk factors is essential for early detection and prevention.
Maternal Risk Factors
Foetal Risk Factors
Placental and Umbilical Cord Risk Factors
Labor and Delivery Risk Factors
Amniotic Fluid Abnormalities
Clinical Manifestations
Foetal distress manifests through several observable changes that can be detected through clinical assessment and electronic monitoring. Recognizing these signs is crucial for prompt intervention.
Primary Signs of Foetal Distress
| Sign | Description | Clinical Significance |
|---|---|---|
| Abnormal Foetal Heart Rate |
|
Indicates potential foetal hypoxia or acidosis; generally the earliest and most reliable indicator of foetal distress |
| Decreased Foetal Movement | Noticeable reduction in foetal movement over an extended period | May indicate foetal compensation mechanism to conserve energy during hypoxic stress |
| Meconium-Stained Amniotic Fluid |
|
Indicates foetal stress; vagal stimulation causes relaxation of anal sphincter and release of meconium |
| Abnormal Biophysical Profile | Low scores on biophysical profile assessment | Suggests compromised foetal well-being across multiple physiologic parameters |
| Scalp Blood pH Changes | pH <7.20 indicates significant acidosis | Direct measurement of foetal acid-base status indicating degree of hypoxia |
Foetal Heart Rate Patterns in Distress
Characteristic patterns observed on electronic foetal monitoring that suggest foetal distress include:
Gradual decrease in heart rate that begins after contraction onset, reaches its nadir after the peak of contraction, and returns to baseline after the contraction ends.
Significance: Indicates uteroplacental insufficiency and is always concerning.
Abrupt decrease in heart rate with rapid onset and recovery, varying in timing, depth, and duration.
Significance: Typically caused by umbilical cord compression. Concerning when severe, prolonged, or recurrent.
Decrease in heart rate of ≥15 bpm lasting between 2-10 minutes.
Significance: May indicate acute events such as cord prolapse, maternal hypotension, or placental abruption.
Fluctuation in heart rate of <5 bpm for extended periods.
Significance: May indicate foetal central nervous system depression from hypoxia or certain medications.
A smooth, undulating waveform with regular cycles, resembling a sine wave.
Significance: Associated with severe foetal anemia, hypoxia, or certain medications; considered an ominous sign.
No single sign should be interpreted in isolation. The clinical picture must consider maternal factors, foetal factors, and the overall progression of labor. Foetal distress is a dynamic condition that requires continuous assessment and re-evaluation.
Diagnosis and Assessment
Accurate diagnosis of foetal distress relies on a combination of clinical assessment, electronic monitoring, and in some cases, invasive testing. Consistent monitoring and proper interpretation are essential for early detection and intervention.
Diagnostic Methods
| Method | Description | Advantages | Limitations |
|---|---|---|---|
| Intermittent Auscultation | Listening to FHR at regular intervals using a fetoscope or handheld Doppler device | Non-invasive, cost-effective, allows maternal mobility | Provides limited information, depends on examiner skill, not continuous |
| Continuous Electronic Foetal Monitoring (CEFM) | Continuous recording of FHR and uterine contractions using external or internal monitors | Provides continuous data, records patterns over time, widely available | Restricts mobility, high false-positive rate, requires interpretation skill |
| Foetal Scalp Blood Sampling | Collection of foetal blood from the presenting part to measure pH or lactate | Direct assessment of acid-base status, confirms acidosis | Invasive, requires cervical dilation, membranes rupture, technical expertise |
| Biophysical Profile (BPP) | Ultrasound assessment of 5 parameters: foetal breathing, movement, tone, amniotic fluid volume, and non-stress test | Comprehensive assessment of foetal wellbeing, non-invasive | Time-consuming, requires specialized equipment and expertise |
| Doppler Velocimetry | Ultrasound assessment of blood flow in foetal vessels (umbilical artery, middle cerebral artery) | Detects abnormal placental resistance, useful for IUGR assessment | Most useful before 34 weeks, requires specialized equipment |
| Non-Stress Test (NST) | Recording of FHR in response to foetal movement | Non-invasive, easily performed, good indicator of current foetal status | Limited predictive value for long-term outcomes, can be time-consuming |
Electronic Foetal Monitoring (EFM) Assessment
When interpreting electronic foetal monitoring traces, healthcare providers assess four key components:
Normal: 110-160 bpm
Tachycardia: >160 bpm
Bradycardia: <110 bpm
Measured between contractions over a 10-minute window; excluding accelerations, decelerations, and periods of marked variability.
Normal (moderate): 6-25 bpm
Minimal: ≤5 bpm
Marked: >25 bpm
Absent: Undetectable
Reflects the interplay between sympathetic and parasympathetic nervous systems.
Transient increases in FHR ≥15 bpm lasting ≥15 seconds
Presence indicates intact foetal CNS and adequate oxygenation; reassuring sign.
Transient decreases in FHR below baseline
Classified as early, late, variable, or prolonged based on timing relative to contractions and waveform characteristics.
This mnemonic helps remember the different types of decelerations and their causes:
- V (Variable decelerations) – C (Cord compression)
- E (Early decelerations) – H (Head compression)
- A (Accelerations) – O (Okay/Oxygen is good)
- L (Late decelerations) – P (Placental insufficiency)
Amniotic Fluid Assessment
The volume and characteristics of amniotic fluid provide important diagnostic information:
- Oligohydramnios: Reduced fluid volume (Amniotic Fluid Index [AFI] <5 cm), associated with foetal distress and placental insufficiency
- Meconium-stained fluid: Categorized as light, moderate, or thick; thick meconium is more concerning and associated with higher rates of meconium aspiration syndrome
While electronic foetal monitoring has a high sensitivity for detecting foetal distress, it has a relatively low specificity, leading to potential false positives. This underscores the importance of correlating EFM findings with the clinical context and, when appropriate, confirming with additional tests like foetal scalp blood sampling before making management decisions.
Classification of Foetal Heart Rate Patterns
The interpretation and classification of foetal heart rate (FHR) patterns are standardized to improve communication among healthcare providers and guide management decisions. Different classification systems exist, but the most widely used is the three-tier system developed by the National Institute of Child Health and Human Development (NICHD).
Three-Tier Classification System
| Category | Description | Features | Management |
|---|---|---|---|
| Category I Normal/Reassuring |
Normal FHR pattern strongly predictive of normal foetal acid-base status at the time of observation |
|
Continue routine monitoring, no specific interventions required |
| Category II Indeterminate |
FHR patterns not predictive of abnormal foetal acid-base status, but with insufficient evidence to classify as Category I or III |
|
|
| Category III Abnormal |
FHR patterns associated with abnormal foetal acid-base status, requiring prompt evaluation and intervention |
|
|
Types of Decelerations
Shape: Uniform, mirror image of contraction
Timing: Onset early in contraction, nadir coincides with peak of contraction, returns to baseline by end of contraction
Cause: Head compression (vagal response)
Significance: Considered physiological and benign
Shape: Uniform, smooth
Timing: Onset delayed after contraction begins, nadir occurs after peak of contraction, slow return to baseline
Cause: Uteroplacental insufficiency
Significance: Always concerning, indicates hypoxemia
Shape: Variable, often “V” or “U” shaped with abrupt onset and recovery
Timing: Inconsistent relationship to contractions
Cause: Umbilical cord compression
Significance: Concerning if deep, prolonged, or recurrent
Shape: Variable
Timing: Deceleration lasting ≥2 minutes but <10 minutes
Cause: Various (maternal hypotension, placental abruption, cord prolapse)
Significance: Requires immediate attention and intervention
Other Classification Systems
NICE Classification (UK): Uses a similar framework but with terminology differences:
- Normal: No concerning features
- Suspicious: One concerning feature present
- Pathological: Two or more concerning features OR one abnormal feature
Classification of FHR patterns should always consider:
- The overall clinical context (maternal condition, labor progress)
- The duration and evolution of patterns over time
- The presence of other risk factors for foetal compromise
- The stage of labor (first or second stage)
Remember that FHR patterns are dynamic and can change rapidly. Continuous reassessment and documentation are essential.
Management and Interventions
Management of foetal distress focuses on resolving the underlying cause, improving foetal oxygenation, and determining the need for expedited delivery. The approach depends on the severity of distress, gestational age, and stage of labor.
Conservative Management (Intrauterine Resuscitation)
When foetal distress is suspected but not severe or when additional time is needed to prepare for delivery, the following interventions may be implemented:
Left lateral position to relieve compression of maternal vena cava and improve uteroplacental perfusion
Rationale: Increases venous return to the heart, cardiac output, and placental perfusion
Supplemental oxygen via face mask at 8-10 L/min
Rationale: Increases maternal oxygen saturation and potentially improves oxygen delivery to the foetus
Note: Evidence for routine use is limited; should be used selectively
Intravenous fluid bolus (typically 500-1000 mL of crystalloid solution)
Rationale: Improves maternal intravascular volume and placental perfusion, particularly in cases of maternal hypotension
Stop oxytocin infusion if in use
Rationale: Reduces frequency and intensity of contractions, allowing improved uteroplacental blood flow between contractions
Short-acting tocolytic agents (e.g., terbutaline 0.25 mg subcutaneously) to temporarily reduce uterine activity
Rationale: Relaxes the uterus to improve placental perfusion, particularly useful in cases of uterine tachysystole or tetanic contractions
Caution: Use with care in patients with cardiac conditions or when contraindicated
The infusion of room temperature saline into the uterine cavity via transcervical catheter.
Indications: Variable decelerations due to cord compression, particularly with oligohydramnios
Rationale: Creates an artificial cushion around the cord to prevent compression
Important Note: Currently not routinely recommended in the UK for intrauterine foetal resuscitation; only undertaken under special arrangements including audit and research
Delivery Interventions
When conservative measures fail to resolve foetal distress or in cases of severe, acute distress, expedited delivery is necessary:
| Intervention | Indications | Considerations |
|---|---|---|
| Assisted Vaginal Delivery (Forceps/Vacuum) |
|
|
| Emergency Caesarean Section |
|
|
Antepartum Management
When foetal distress is detected during pregnancy (before labor):
- Enhanced foetal monitoring (BPP, Doppler studies)
- Treatment of underlying maternal conditions (hypertension, diabetes)
- Steroid administration for foetal lung maturity if preterm
- Timing delivery based on gestational age and severity of distress
- Consider in-utero transfer to higher-level facility if necessary
For preterm foetuses with suspected distress, there is a balance between the risks of prematurity versus the risks of continued intrauterine hypoxia. Decision-making should involve:
- Neonatology consultation
- Assessment of neonatal intensive care capabilities
- Consideration of steroid administration for lung maturity
- Magnesium sulfate for neuroprotection if <32 weeks
- Weighing the risks and benefits of expectant management versus delivery
Nursing Care and Interventions
Nurses play a critical role in prevention, early detection, and management of foetal distress. Skilled nursing assessment and interventions are essential components of effective care.
This useful nursing mnemonic outlines the key interventions for managing foetal distress:
- S – STOP oxytocin infusion
- M – Mom turned on side (preferably left lateral)
- O – O₂ administration
- A – Assess baby and mom to see if changes occurred
- N – Notify Provider
Nursing Assessment
- Evaluate baseline FHR, variability, accelerations, and decelerations
- Recognize patterns consistent with foetal distress
- Interpret FHR in context of uterine contraction pattern
- Document findings appropriately
- Ensure monitoring equipment is functioning properly
- Monitor vital signs, especially blood pressure
- Assess hydration status and urine output
- Evaluate contraction pattern (frequency, duration, intensity)
- Check for signs of placental abruption (vaginal bleeding, abdominal pain)
- Assess for maternal hypotension following regional anesthesia
Nursing Interventions
1. Preventive Interventions
- Position the laboring woman to optimize uteroplacental perfusion (left lateral position)
- Ensure adequate hydration (oral or IV)
- Monitor and document maternal vital signs and FHR according to protocols
- Educate the woman about position changes and their importance
- Avoid supine position, especially in late pregnancy
2. Interventions for Suspected Foetal Distress
| Intervention | Nursing Actions | Rationale |
|---|---|---|
| Position Change |
|
Relieves pressure on vena cava, improves venous return and cardiac output, enhances uteroplacental perfusion |
| Oxytocin Management |
|
Reduces uterine activity, allows for improved uteroplacental blood flow between contractions |
| Oxygen Administration |
|
Increases maternal oxygen saturation, may improve foetal oxygenation in cases of hypoxemia |
| Hydration |
|
Improves maternal circulating volume, enhances perfusion to placenta, treats or prevents dehydration |
| Continuous Assessment |
|
Determines effectiveness of interventions, identifies need for additional measures or expedited delivery |
3. Preparation for Emergency Delivery
- Alert the healthcare team according to protocol
- Prepare equipment for potential resuscitation
- Document all assessments, interventions, and responses
- Support and inform the woman and her partner
- Prepare for transfer to operating room if caesarean section indicated
- Assist with preparations for assisted vaginal delivery if appropriate
Nursing Diagnosis Related to Foetal Distress
Key nursing diagnoses that may apply in cases of foetal distress include:
- Risk for Altered Foetal Perfusion related to maternal position, contraction pattern, or maternal conditions
- Risk for Impaired Gas Exchange (foetal) related to altered placental perfusion or cord compression
- Anxiety related to concerns about foetal wellbeing and emergency interventions
- Deficient Knowledge related to understanding of foetal monitoring and interventions
- Acute Pain related to labor process and interventions
Thorough documentation is essential and should include:
- Detailed description of FHR patterns and changes
- Timing of pattern recognition and interventions
- Notification of healthcare providers
- Response to interventions
- Maternal and foetal condition throughout the event
- Communications with healthcare team and the woman/family
In cases of litigation related to birth injuries, documentation of timely recognition and appropriate interventions is critically important.
Complications
Foetal distress, if not promptly recognized and appropriately managed, can lead to serious complications for both the foetus/newborn and the mother. Understanding these potential complications is essential for anticipating care needs and communicating risks.
Foetal and Neonatal Complications
| Complication | Description | Potential Long-term Consequences |
|---|---|---|
| Birth Asphyxia | Oxygen deprivation at birth leading to impaired function of multiple organ systems | Hypoxic-ischemic encephalopathy, multi-organ dysfunction syndrome, death |
| Meconium Aspiration Syndrome | Inhalation of meconium-stained amniotic fluid into the lungs before or during delivery | Respiratory distress, pneumonia, persistent pulmonary hypertension, chronic lung disease |
| Hypoxic-Ischemic Encephalopathy (HIE) | Brain injury resulting from oxygen deprivation and limited blood flow to the brain | Cerebral palsy, intellectual disability, seizure disorders, developmental delay |
| Acidosis | Buildup of acid in the blood due to inadequate oxygen supply | Organ dysfunction, particularly affecting brain, heart, and kidneys |
| Persistent Pulmonary Hypertension | Failure of normal circulatory transition at birth | Chronic respiratory issues, neurodevelopmental impairment |
| Stillbirth | Foetal death occurring after 20 weeks gestation | Profound psychological impact on family, implications for future pregnancies |
Maternal Complications
While foetal distress primarily affects the foetus, there can be associated maternal complications:
- Emergency Delivery Complications: Increased risk of trauma associated with urgent operative delivery (caesarean section or instrumental vaginal delivery)
- Psychological Impact: Increased risk of postpartum depression, post-traumatic stress disorder, and anxiety related to the emergency situation and concerns about the baby’s well-being
- Prolonged Hospital Stay: Both mother and baby may require extended hospitalization for monitoring and treatment
Factors Affecting Outcomes
The severity of complications depends on several factors:
- Duration and severity of hypoxia: Longer and more severe oxygen deprivation increases risk of adverse outcomes
- Gestational age: Preterm infants are more vulnerable to complications
- Pre-existing conditions: Foetal growth restriction or other anomalies may reduce foetal reserves
- Time to intervention: Prompt recognition and appropriate management improves outcomes
- Quality of neonatal resuscitation: Skilled resuscitation can mitigate effects of intrapartum asphyxia
- Access to therapeutic hypothermia: For HIE, cooling therapy initiated within 6 hours of birth can improve neurological outcomes
While foetal distress and birth asphyxia have traditionally been associated with cerebral palsy, current research indicates that the vast majority of cerebral palsy cases (approximately 70-80%) are not related to intrapartum events but rather to prenatal or genetic factors. Only a small percentage of cerebral palsy cases can be attributed solely to events during labor and delivery.
For intrapartum hypoxia to be considered the cause of cerebral palsy, specific criteria must be met, including:
- Evidence of metabolic acidosis in umbilical cord arterial blood (pH < 7.0 and base deficit ≥ 12 mmol/L)
- Early onset of severe or moderate neonatal encephalopathy
- Cerebral palsy of the spastic quadriplegic or dyskinetic type
- Exclusion of other identifiable causes
Prevention
While not all cases of foetal distress can be prevented, several strategies can reduce the risk or allow for earlier detection and intervention, improving outcomes.
Antepartum Preventive Measures
- Thorough prenatal history and physical examination
- Identification of high-risk pregnancies
- Appropriate referral for specialized care when indicated
- Regular reassessment of risk status throughout pregnancy
- Teaching foetal movement monitoring (kick counts)
- Instructions on when to seek medical attention
- Education about signs of complications
- Importance of keeping prenatal appointments
- Optimal control of diabetes, hypertension, and other medical conditions
- Treatment of infections
- Smoking cessation counseling
- Substance abuse treatment when applicable
- Appropriate use of non-stress testing
- Biophysical profiles when indicated
- Doppler studies for high-risk pregnancies
- Proper interpretation and follow-up of abnormal results
Intrapartum Preventive Measures
- Appropriate Foetal Monitoring: Use of continuous electronic foetal monitoring for high-risk pregnancies and intermittent auscultation for low-risk pregnancies according to guidelines
- Interpretation Skills: Ensuring all staff are trained in correct interpretation of foetal heart rate patterns and appropriate response
- Labor Management: Judicious use of oxytocin, avoiding uterine tachysystole
- Maternal Positioning: Encouraging positions that optimize uteroplacental perfusion
- Hydration: Maintaining adequate maternal hydration
- Regular Reassessment: Ongoing evaluation of the labor progress and foetal wellbeing
- Prompt Response to Abnormalities: Timely implementation of intrauterine resuscitation measures when indicated
System-Level Preventive Strategies
- Standardized Protocols: Implementation of evidence-based protocols for monitoring and managing foetal distress
- Regular Training: Simulation drills and team training for emergency response to foetal distress
- Clear Communication Tools: Structured communication methods (e.g., SBAR – Situation, Background, Assessment, Recommendation) for handoffs and escalation of concerns
- Quality Improvement: Regular case reviews and continuous quality improvement activities focused on foetal monitoring practices
- Appropriate Staffing: Ensuring adequate nurse-to-patient ratios in labor and delivery units
- Access to Technology: Availability of appropriate monitoring equipment and interpretation tools
Several global initiatives have shown promise in reducing complications related to foetal distress:
- MOREOB (Managing Obstetrical Risk Efficiently): A comprehensive patient safety, professional development, and performance improvement program for caregivers in labor and delivery units
- PROMPT (PRactical Obstetric Multi-Professional Training): An evidence-based multi-professional obstetric emergency training course demonstrating improvements in perinatal outcomes
- Electronic Foetal Monitoring Certification Programs: Standardized training and certification in interpretation of foetal monitoring has been associated with improved outcomes
- Baby-Friendly Hospital Initiative: While primarily focused on breastfeeding, this WHO initiative promotes practices that support optimal maternal-infant care including appropriate monitoring practices
Summary and Key Points
Definition and Terminology
- Foetal distress refers to a condition where the foetus shows signs of compromise due to inadequate oxygen or nutrient supply.
- Modern obstetric practice has moved toward the term “non-reassuring foetal status” for more precise description.
Pathophysiology
- Primary mechanisms include uteroplacental insufficiency, umbilical cord compression, head compression, and placental dysfunction.
- Foetal response to hypoxia progresses from initial compensation to progressive hypoxemia and eventually decompensation if not resolved.
Risk Factors
- Maternal factors include advanced age, hypertensive disorders, diabetes, and chronic medical conditions.
- Foetal factors include growth restriction, multiple pregnancy, and post-term gestation.
- Placental and cord factors include abruption, previa, and cord compression events.
Clinical Manifestations
- Abnormal foetal heart rate patterns (tachycardia, bradycardia, decreased variability, decelerations)
- Decreased foetal movement
- Meconium-stained amniotic fluid
- Abnormal biophysical profile or Doppler studies
Diagnosis
- Electronic foetal monitoring is the primary diagnostic tool during labor.
- Three-tier classification system categorizes FHR patterns as Category I (normal), II (indeterminate), or III (abnormal).
- Additional diagnostic methods include foetal scalp blood sampling, biophysical profile, and Doppler studies.
Management
- Conservative measures (intrauterine resuscitation): maternal positioning, oxygen administration, hydration, and discontinuation of oxytocin.
- Expedited delivery via assisted vaginal delivery or cesarean section when conservative measures fail or in acute, severe distress.
Nursing Interventions
- STOP MOAN mnemonic: Stop oxytocin, Mom on side, Oxygen administration, Assess response, Notify provider.
- Continuous assessment of foetal and maternal status.
- Implementation of intrauterine resuscitation measures.
- Preparation for potential emergency delivery.
- Documentation of assessments, interventions, and responses.
Complications
- Foetal/neonatal: birth asphyxia, meconium aspiration syndrome, hypoxic-ischemic encephalopathy, acidosis.
- Maternal: complications related to emergency delivery, psychological impact.
Prevention
- Risk assessment and appropriate prenatal care.
- Management of maternal medical conditions.
- Appropriate foetal monitoring during labor.
- Staff training in recognition and management of foetal distress.
- System-level strategies including standardized protocols and regular drills.
As a nursing student and future nurse, remember these key points when caring for patients with potential foetal distress:
- Foetal distress requires prompt recognition and action – minutes matter.
- Develop proficiency in interpreting foetal heart rate patterns and understanding their clinical significance.
- Know your facility’s protocols for escalation and emergency response.
- Document thoroughly all assessments, interventions, and responses.
- Communication with the healthcare team and the laboring woman/family is essential.
- Prevention through careful monitoring and risk assessment is the best approach.
With proper knowledge, skills, and teamwork, many adverse outcomes related to foetal distress can be prevented or mitigated.
These notes are intended for educational purposes only and should be used alongside clinical instruction and current evidence-based guidelines.
© 2025 Nursing Educational Resources
