Food Classification and Origin
Comprehensive Nursing Notes
Introduction to Food Science in Nursing
Food is a fundamental component of human health and plays a crucial role in disease prevention, recovery, and overall well-being. As nursing professionals, understanding food classification, nutritional content, and origins is essential for providing comprehensive patient care, dietary counseling, and health promotion.
This comprehensive guide explores the classification systems of foods, their origins, and practical applications in nursing practice. Understanding these concepts enables nurses to make informed decisions about patient nutrition, therapeutic diets, and health education.
Visual Overview: Food Groups and Nutrients
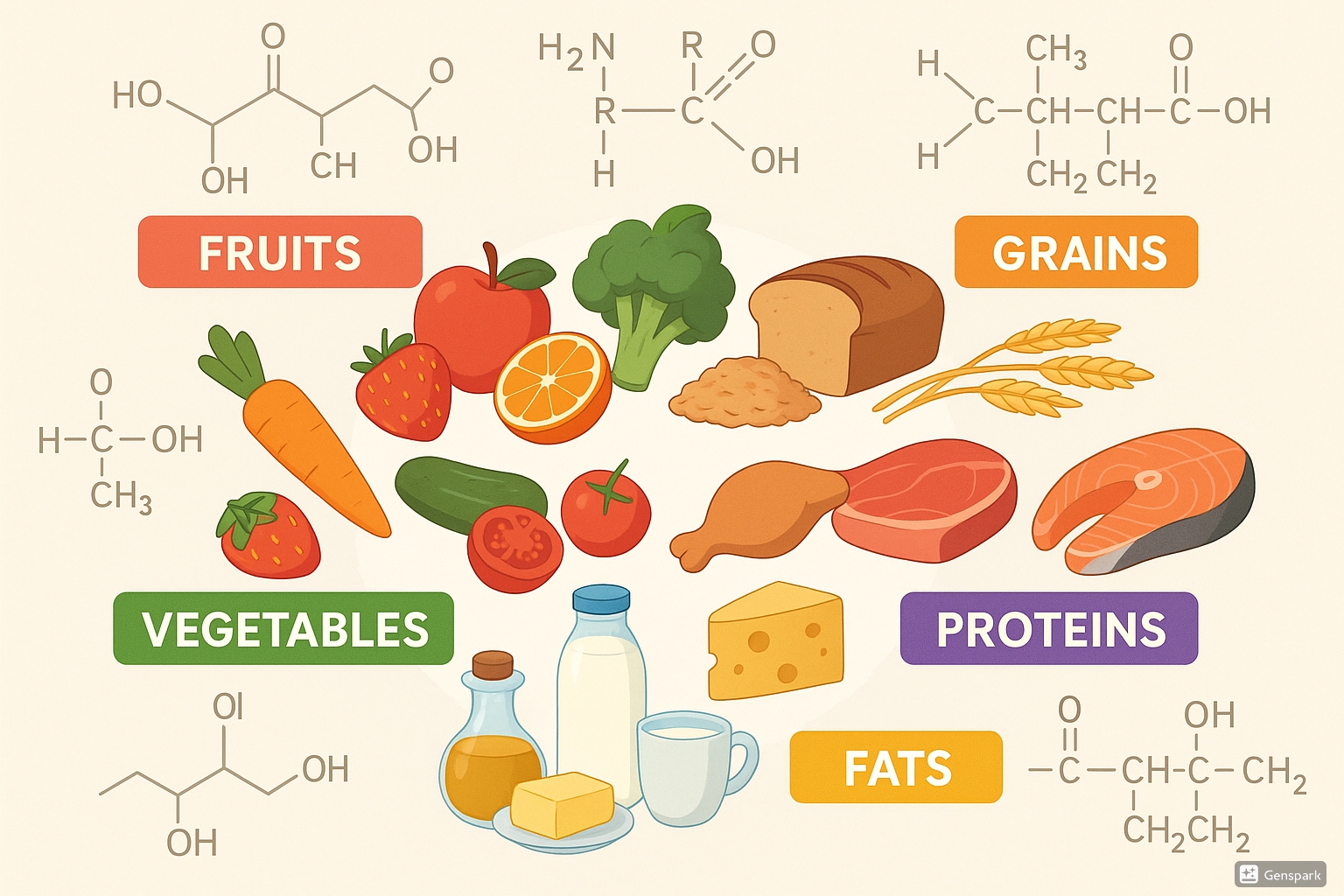
Comprehensive illustration showing the six major food groups and their molecular structures
Food Classification Systems
Nutrient-Based Classification
Carbohydrates
Primary energy source
Proteins
Building blocks
Fats
Energy storage
Vitamins
Metabolic regulators
Minerals
Structural components
Water
Essential medium
Memory Aid: CPF-VAN
C-P-F + V-A-N
- Carbohydrates – Carbs give you energy to Care
- Proteins – Proteins help you grow and Play
- Fats – Fats keep you Full and warm
- Vitamins – Vitamins keep you Vibrant
- Ash/Minerals – Ash builds your Architecture
- Nutrients in water – Water is Never optional
Functional Classification
Energy-Giving Foods
- • Rice, wheat, oats, barley
- • Potatoes, sweet potatoes
- • Oils, butter, nuts
- • Sugar, honey, jaggery
Function: Provide calories for daily activities
Body-Building Foods
- • Meat, fish, eggs
- • Milk, cheese, yogurt
- • Beans, lentils, peas
- • Nuts and seeds
Function: Growth and repair of tissues
Protective Foods
- • Fruits: citrus, berries, melons
- • Vegetables: leafy greens, carrots
- • Whole grains
- • Liver, fish oils
Function: Prevent diseases, boost immunity, regulate body functions
MyPlate Food Groups (USDA)
Vegetables
5 subgroups:
- • Dark green (spinach, kale)
- • Red/orange (tomatoes, carrots)
- • Starchy (potatoes, corn)
- • Beans/peas (legumes)
- • Other (onions, celery)
Fruits
Fresh, frozen, canned, dried:
- • Citrus fruits (oranges, lemons)
- • Berries (strawberries, blueberries)
- • Stone fruits (peaches, apricots)
- • Tropical fruits (mango, pineapple)
- • Melons (watermelon, cantaloupe)
Grains
Whole vs. refined:
- • Whole grains (brown rice, oats)
- • Refined grains (white bread, pasta)
- • Cereals and crackers
- • Quinoa, barley, bulgur
- • Fortified grain products
Protein Foods
Animal and plant sources:
- • Meat, poultry, seafood
- • Eggs and egg products
- • Nuts, seeds, nut butters
- • Beans, peas, lentils
- • Soy products (tofu, tempeh)
Dairy
Calcium-rich foods:
- • Milk (low-fat, skim)
- • Cheese (natural, processed)
- • Yogurt (plain, flavored)
- • Fortified soy beverages
- • Calcium-fortified alternatives
Oils & Fats
Essential fatty acids:
- • Vegetable oils (olive, canola)
- • Nuts and seeds
- • Avocados
- • Fish oils
- • Limit saturated fats
MyPlate Memory Aid: “Very Fit Guys Play Dancing”
Food Origins and Sources
Plant-Based Food Origins
Tree and Shrub Sources
Herbaceous Plant Sources
Animal-Based Food Origins
Land Animals
Aquatic Animals
Alternative Sources
Geographical Food Origins
Major Crop Origins
Climate-Specific Foods
Food Processing and Preparation Origins
Minimally Processed
Cleaned, cut, frozen fresh foods
Processed
Bread, cheese, canned vegetables
Highly Processed
Ready meals, snacks, sodas
Ultra-Processed
Artificial additives, preservatives
Nursing Implementation and Clinical Applications
Nutritional Assessment and Planning
Assessment Components
- Dietary History: Food preferences, cultural practices, allergies
- Anthropometric Data: Height, weight, BMI, waist circumference
- Biochemical Markers: Blood glucose, lipids, albumin, hemoglobin
- Clinical Signs: Skin condition, wound healing, energy levels
Planning Considerations
- Individual Needs: Age, gender, activity level, medical conditions
- Cultural Factors: Religious restrictions, ethnic preferences
- Economic Factors: Food security, budget constraints
- Therapeutic Needs: Disease-specific dietary modifications
Disease-Specific Nutritional Interventions
Cardiovascular Disease
Promote: Omega-3 fatty acids, fiber, antioxidants
Limit: Saturated fats, sodium, trans fats
Foods: Fish, whole grains, fruits, vegetables
Avoid: Processed meats, excessive salt, fried foods
Diabetes Mellitus
Promote: Complex carbohydrates, fiber, lean proteins
Limit: Simple sugars, refined carbohydrates
Foods: Whole grains, non-starchy vegetables, lean meats
Avoid: Sugary drinks, white bread, processed snacks
Osteoporosis
Promote: Calcium, vitamin D, magnesium
Limit: Excessive caffeine, alcohol, sodium
Foods: Dairy products, leafy greens, fortified foods
Avoid: Excessive phosphorus, high-sodium foods
Cancer
Promote: Antioxidants, phytochemicals, adequate protein
Limit: Processed meats, excessive alcohol
Foods: Colorful fruits/vegetables, whole grains, lean proteins
Avoid: Charred meats, excessive red meat, refined sugars
Patient Education Strategies
Visual Aids
- • MyPlate diagrams
- • Portion size demonstrations
- • Food label reading guides
- • Meal planning templates
- • Grocery shopping lists
Hands-On Learning
- • Cooking demonstrations
- • Food preparation techniques
- • Measuring and portioning
- • Menu planning exercises
- • Grocery store tours
Technology Integration
- • Nutrition tracking apps
- • Recipe sharing platforms
- • Telehealth consultations
- • Educational videos
- • Virtual reality experiences
Monitoring and Evaluation
Evaluation Metrics
Objective Measures
- • Weight changes and BMI trends
- • Laboratory values (glucose, lipids)
- • Blood pressure measurements
- • Wound healing progression
- • Medication effectiveness
Subjective Measures
- • Energy levels and fatigue
- • Appetite and food satisfaction
- • Quality of life scores
- • Adherence to dietary plans
- • Patient confidence levels
Special Population Considerations
Pediatric Populations
- • Growth and development requirements
- • Age-appropriate food textures
- • Preventing childhood obesity
- • Food allergies and intolerances
- • Family involvement in nutrition
Geriatric Populations
- • Decreased appetite and taste changes
- • Swallowing difficulties (dysphagia)
- • Medication-nutrient interactions
- • Social isolation and meal preparation
- • Preventing malnutrition
Nursing Process Flowchart: Nutritional Care
ASSESSMENT
Gather nutritional history, physical data, laboratory values, and cultural preferences
DIAGNOSIS
Identify nutritional problems: imbalanced nutrition, knowledge deficit, risk for complications
PLANNING
Set realistic goals, develop individualized meal plans, and establish measurable outcomes
IMPLEMENTATION
Provide education, coordinate with dietitians, monitor intake, and support behavior change
EVALUATION
Assess goal achievement, monitor health outcomes, and modify care plans as needed
Continuous cycle of care
Memory Aids and Quick Reference
Essential Nutrients: “Can Peter Find My Vitamins Wisely?”
Macronutrients
- Carbohydrates – Energy
- Proteins – Building blocks
- Fats – Essential fatty acids
Micronutrients
- Minerals – Structure
- Vitamins – Metabolism
Other
- Water – Life medium
Food Safety: “CLEAN, SEPARATE, COOK, CHILL”
CLEAN
Hands, surfaces, utensils
SEPARATE
Raw from cooked foods
COOK
To safe temperatures
CHILL
Refrigerate promptly
Portion Size Hand Guide
Hand Measurements
- 🤚 Palm: Protein portions (3-4 oz)
- 👊 Fist: Vegetable portions (1 cup)
- 🤏 Thumb: Fat portions (1 tbsp)
- 👌 Fingertip: Condiment portions (1 tsp)
Visual References
- 🎾 Tennis ball: Medium fruit
- 🏓 Ping pong ball: 2 tbsp nuts
- 🎲 Dice: 1 oz cheese
- 💿 CD: 1 pancake/waffle
Quick Nutritional Assessment Checklist
Red Flags
- ☐ Unintentional weight loss >10%
- ☐ Poor appetite for >3 days
- ☐ Difficulty swallowing
- ☐ Nausea/vomiting >24 hours
- ☐ Pressure ulcers present
Positive Indicators
- ☐ Stable weight maintenance
- ☐ Good appetite and intake
- ☐ Normal lab values
- ☐ Good wound healing
- ☐ Adequate energy levels
Key Takeaways for Nursing Practice
Essential Knowledge
- Food classification systems guide nutritional assessment and planning
- Understanding food origins helps identify nutritional content and quality
- Cultural and individual factors significantly impact dietary choices
- Therapeutic diets require careful monitoring and adjustment
Clinical Applications
- Integrate nutritional assessment into routine patient care
- Collaborate with dietitians for complex nutritional needs
- Provide patient education using evidence-based guidelines
- Monitor and evaluate nutritional interventions regularly
