Hemorrhoids, Fissures, and Fistulas
Comprehensive Nursing Guide
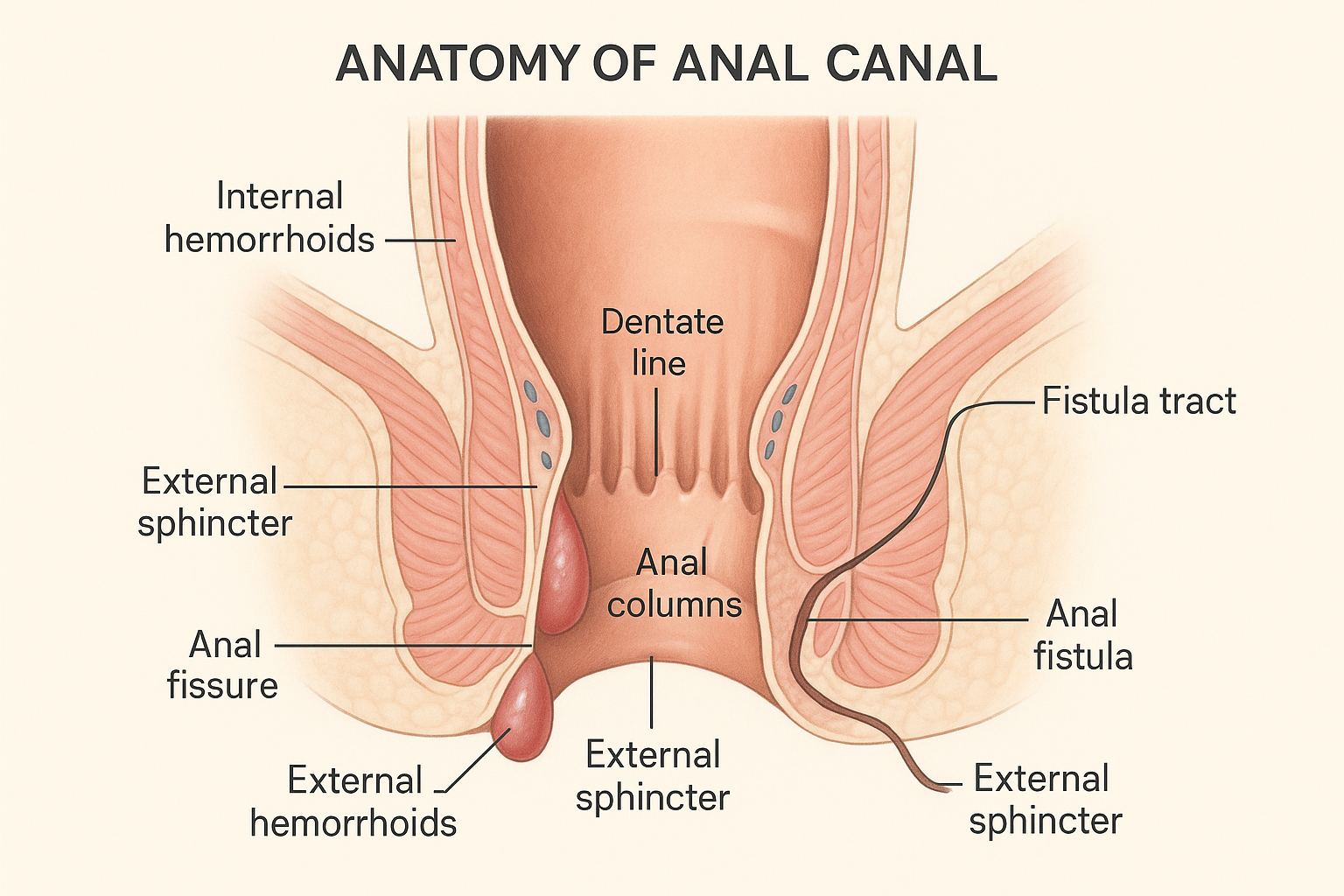
Figure 1: Anatomical cross-section showing common anorectal conditions
Introduction to Anorectal Disorders
Anorectal disorders including hemorrhoids, anal fissures, and anal fistulas represent some of the most common conditions encountered in clinical practice. These conditions significantly impact patient quality of life and require comprehensive understanding of their pathophysiology, clinical presentation, and evidence-based management strategies for optimal nursing care.
Learning Objectives
- Understand the pathophysiology and risk factors for each condition
- Recognize characteristic signs and symptoms
- Implement evidence-based nursing interventions
- Differentiate between conditions for accurate assessment
- Provide appropriate patient education and discharge planning
Table of Contents
1. Hemorrhoids
2. Anal Fissures
1. Hemorrhoids
1.1 Pathophysiology
Hemorrhoid Formation Process
Arteriovenous plexus supports continence
Straining, pregnancy, chronic constipation
Loss of supporting connective tissue
Prolapse, bleeding, thrombosis
Key Pathophysiological Concepts
- Sliding Anal Lining Theory: Disruption of supporting tissues leads to distal displacement of anal cushions
- Vascular Hypothesis: Abnormal dilation of arteriovenous communications
- Mechanical Theory: Increased intra-abdominal pressure causes venous congestion
1.2 Classification & Grading
Internal Hemorrhoids
- Grade I: Bleeding only, no prolapse
- Grade II: Prolapse with spontaneous reduction
- Grade III: Prolapse requiring manual reduction
- Grade IV: Irreducible prolapse
External Hemorrhoids
- Located below dentate line
- Covered by anoderm (stratified squamous epithelium)
- Painful when thrombosed
- May form skin tags after resolution
Memory Aid: “BPMR” for Internal Hemorrhoid Grades
- Bleeding only (Grade I)
- Prolapse with spontaneous reduction (Grade II)
- Manual reduction required (Grade III)
- Reducible no more (Grade IV)
1.3 Clinical Assessment
Subjective Assessment
- Primary Complaint: Bright red rectal bleeding
- Pain Pattern: Usually painless unless thrombosed
- Prolapse History: Timing and reducibility
- Associated Symptoms: Itching, mucus discharge
- Triggering Factors: Straining, pregnancy, heavy lifting
Objective Assessment
- Inspection: Perianal area, prolapsed tissue
- Digital Examination: Assess sphincter tone
- Anoscopy: Visualize internal hemorrhoids
- Valsalva Maneuver: Evaluate prolapse
- Thrombosis Signs: Bluish, tender external mass
Clinical Pearl: Goodsall’s Rule
External openings anterior to the transverse anal line connect to the anal canal via straight radial tracts. Posterior openings connect via curved tracts to the posterior midline.
1.4 Management Strategies
Conservative Management
- High-fiber diet (25-35g/day)
- Adequate hydration (8-10 glasses/day)
- Stool softeners (docusate sodium)
- Sitz baths (15-20 minutes, 3x daily)
- Topical analgesics/anti-inflammatories
Office Procedures
- Rubber band ligation (Grades I-III)
- Sclerotherapy
- Infrared photocoagulation
- Bipolar diathermy
- Cryotherapy
Surgical Options
- Hemorrhoidectomy (Grade IV)
- Stapled hemorrhoidopexy
- Hemorrhoidal artery ligation
- Thrombectomy (acute thrombosis)
- Emergency surgery (strangulation)
2. Anal Fissures
2.1 Pathophysiology
Ischemic Theory of Fissure Formation
Primary Factors:
- • Posterior midline receives <50% perfusion
- • High anal sphincter pressure
- • Decreased blood flow during defecation
- • Mechanical trauma from hard stool
Perpetuating Cycle:
- • Pain → Sphincter spasm
- • Spasm → Further ischemia
- • Ischemia → Delayed healing
- • Fear → Constipation → Trauma
Fissure Development Pathway
(Hard stool/diarrhea)
(Posterior midline)
(Protective mechanism)
(Ischemic environment)
(Chronic fissure)
2.2 Acute vs Chronic Fissures
Acute Fissures (<6 weeks)
- • Fresh, well-demarcated tear
- • Bright red bleeding
- • Clean wound edges
- • Minimal surrounding inflammation
- • Good healing potential
- • Responds to conservative measures
- • 80-90% heal with medical therapy
Chronic Fissures (>6 weeks)
- • Deep fissure exposing sphincter
- • Indurated, fibrotic edges
- • Sentinel pile (skin tag)
- • Hypertrophied anal papilla
- • Poor healing response
- • May require surgical intervention
- • High recurrence rate
Memory Aid: “FISSURE” Signs of Chronicity
- Fibrotic edges
- Indurated appearance
- Sentinel pile present
- Sphincter muscle visible
- Undermined wound edges
- Recurrent symptoms >6 weeks
- Enlarged anal papilla
2.3 Clinical Assessment
Assessment Precautions
Avoid digital examination and anoscopy during acute phase due to severe pain
Diagnosis is primarily clinical based on history and gentle inspection
Classic Symptom Triad
Sharp, tearing pain during and after defecation (lasting hours)
Small amounts on toilet paper or stool surface
Involuntary muscle contraction causing more pain
Physical Examination
- • Lateral location
- • Multiple fissures
- • Unusually large or deep
- • Associated with IBD, STIs, malignancy
2.4 Management Approaches
Conservative Management (First-line)
Dietary Modifications:
- • High-fiber diet (25-35g daily)
- • Increased fluid intake
- • Stool softeners (docusate sodium)
- • Bulk-forming laxatives
Hygiene & Comfort:
- • Warm sitz baths (15-20 min, 3x daily)
- • Gentle cleansing after defecation
- • Avoid harsh soaps/wipes
- • Pat dry, don’t rub
Topical Analgesics:
- • 2% lidocaine gel
- • Topical anesthetics
- • Apply before defecation
Pharmacological Therapy
Calcium Channel Blockers:
- • Nifedipine 0.2% ointment
- • Diltiazem 2% gel
- • Apply 2-3 times daily
- • Superior to nitroglycerin
Nitroglycerin Ointment:
- • 0.2-0.4% strength
- • Vasodilator effect
- • Side effects: headache, hypotension
- • Apply in seated position
Botulinum Toxin:
- • 20-30 units injected into sphincter
- • Most effective for chronic fissures
- • Temporary sphincter paralysis
- • May require repeat injections
Surgical Management
Lateral Internal Sphincterotomy (LIS):
- • Gold standard for chronic fissures
- • 96% healing rate within 3 weeks
- • Division of internal sphincter fibers
- • Open vs closed technique
Complications:
- • Temporary incontinence (45% immediate)
- • Long-term incontinence (<10% at 5 years)
- • Bleeding (more common with open technique)
- • Keyhole deformity (rare, usually asymptomatic)
3. Anal Fistulas
3.1 Cryptoglandular Theory
Development of Anal Fistulas
Debris blocks ductal opening
Infection in intersphincteric space
Pus collection seeks drainage
External opening created
Epithelialized tract forms
Memory Aid: “FRIEND” – Causes of Fistulas
- Foreign body
- Radiation
- Infection/Inflammatory Bowel Disease
- Epithelialization
- Neoplasm
- Distal obstruction
3.2 Parks Classification System
Intersphincteric (50-80%)
- • Crosses internal sphincter only
- • Most common type
- • Simple fistulotomy usually sufficient
- • Low risk of incontinence
Transphincteric (20-40%)
- • Crosses both sphincters
- • Higher complexity
- • May require staged treatment
- • Seton placement often needed
Suprasphincteric (5%)
- • Passes above external sphincter
- • Involves puborectalis muscle
- • Complex surgical management
- • High risk procedure
Extrasphincteric (2%)
- • Bypasses sphincter complex
- • Often secondary to procedures
- • May indicate underlying pathology
- • Requires comprehensive evaluation
St. James University Hospital (SJUH) MRI Classification
Simple intersphincteric
Intersphincteric + abscess/secondary tract
Transphincteric
Transphincteric + abscess in ischiorectal fossa
Supralevator/translevator
3.3 Diagnostic Evaluation
Clinical Presentation
- Primary Symptoms:
- • Intermittent drainage
- • Perianal irritation/itching
- • Recurrent abscess episodes
- • Pain with sitting
- Drainage Character:
- • Serous, purulent, or bloody
- • May be fecal in high fistulas
- • Intermittent vs continuous
Physical Examination
- Inspection:
- • External opening identification
- • Indurated tract palpation
- • Signs of active infection
- • Goodsall’s rule application
- Digital Examination:
- • Internal opening location
- • Sphincter assessment
- • Associated pathology
Imaging Studies
- MRI Pelvis (Gold Standard):
- • Detailed tract visualization
- • Occult abscess detection
- • Sphincter relationship
- • Complex fistula mapping
- Endoanal Ultrasound:
- • Office-based procedure
- • H2O2 enhancement
- • Cost-effective alternative
Special Considerations
- Crohn’s Disease Screening:
- • Multiple/complex fistulas
- • Recurrent disease
- • Associated GI symptoms
- • Young patient age
- Examination Under Anesthesia:
- • Probe insertion
- • Methylene blue injection
- • Internal opening identification
- • Treatment planning
3.4 Surgical Management
Simple Procedures
Fistulotomy:
- • Gold standard for simple fistulas
- • 94% healing rate
- • Low risk for intersphincteric
- • Divide tract and allow healing
Fistulectomy:
- • Complete tract excision
- • Similar outcomes to fistulotomy
- • Longer healing time
- • Consider for recurrent disease
Complex Procedures
Seton Placement:
- • Loose seton for drainage
- • Cutting seton for migration
- • 98% healing for high fistulas
- • Staged approach
LIFT Procedure:
- • Ligation of Intersphincteric Fistula Tract
- • 75% healing rate
- • Excellent continence preservation
- • Suitable for transphincteric fistulas
Advanced Techniques
Advancement Flap:
- • Rectal/mucosal flap coverage
- • Good for high fistulas
- • <10% recurrence rate
- • May require trans-anal approach
Fistula Plug:
- • Biologic/synthetic materials
- • Variable success rates (13-60%)
- • Risk of sepsis
- • Higher recurrence rates
VAAFT:
- • Video-assisted technique
- • Direct visualization
- • Emerging technology
- • Reduced pain/stay
4. Comprehensive Nursing Management
4.1 Comprehensive Nursing Assessment
Primary Assessment
- Pain Assessment:
- • Use 0-10 numeric scale
- • Timing: during/after defecation
- • Character: sharp, burning, throbbing
- • Duration and triggers
- Bleeding Assessment:
- • Amount and frequency
- • Color: bright red vs dark
- • Associated with bowel movements
- • Impact on hemoglobin levels
Functional Assessment
- Bowel Pattern:
- • Frequency and consistency
- • Bristol Stool Chart scoring
- • Straining patterns
- • Incomplete evacuation sensation
- Continence Status:
- • Fecal incontinence severity
- • Gas control ability
- • Urgency episodes
- • Impact on daily activities
Psychosocial Assessment
- Quality of Life Impact:
- • Work/school attendance
- • Social activity participation
- • Sleep disturbance
- • Sexual function concerns
- Emotional Well-being:
- • Anxiety/depression screening
- • Body image concerns
- • Coping mechanisms
- • Support system availability
Risk Factor Assessment
- Contributing Factors:
- • Dietary fiber intake
- • Fluid consumption patterns
- • Physical activity level
- • Medication effects (opioids, anticholinergics)
- Comorbidities:
- • IBD, diabetes, pregnancy
- • Previous anorectal surgery
- • Chronic conditions
- • Immunosuppression status
4.2 Evidence-Based Nursing Interventions
Pain Management Interventions
Non-Pharmacological:
- • Sitz baths: 38-40°C, 15-20 minutes, 3-4x daily
- • Cold compresses for acute swelling
- • Positioning: side-lying, avoid prolonged sitting
- • Relaxation techniques during defecation
- • Donut cushions for sitting comfort
Pharmacological Support:
- • Monitor medication effectiveness
- • Assess for side effects
- • Timing of analgesics before defecation
- • Document pain scores and responses
Bowel Management Program
Dietary Interventions:
- • Fiber intake: 25-35g daily (gradual increase)
- • Fluid intake: 2-3 liters daily
- • Prune juice, psyllium, methylcellulose
- • Avoid spicy foods during acute phase
- • Regular meal timing
Toileting Routine:
- • Scheduled defecation times
- • Respond promptly to urges
- • Proper positioning on toilet
- • Avoid straining and breath-holding
Wound Care and Hygiene Management
Perineal Hygiene:
- • Gentle cleansing with warm water
- • Pat dry, avoid rubbing
- • Use soft, unscented tissue
- • Avoid harsh soaps and wipes
- • Cotton underwear, loose-fitting clothing
Post-Surgical Care:
- • Monitor wound healing progression
- • Assess for signs of infection
- • Document drainage characteristics
- • Dressing changes as ordered
- • Early ambulation when appropriate
4.3 Patient Education & Discharge Planning
Lifestyle Modifications
- Diet Education:
- • High-fiber food sources
- • Adequate hydration importance
- • Gradual dietary changes
- • Foods to avoid during flares
- Activity Guidelines:
- • Regular exercise benefits
- • Avoiding prolonged sitting
- • Proper lifting techniques
- • Return to work timeline
Self-Care Instructions
- Home Management:
- • Sitz bath preparation and frequency
- • Proper perineal hygiene
- • When to use topical medications
- • Signs requiring medical attention
- Medication Compliance:
- • Proper application techniques
- • Expected side effects
- • Duration of treatment
- • Drug interactions to avoid
Warning Signs
- Immediate Medical Attention:
- • Severe, uncontrolled pain
- • Heavy bleeding or clots
- • Signs of infection (fever >101°F)
- • Urinary retention
- Follow-up Scheduling:
- • Routine appointments
- • When to call healthcare provider
- • Emergency contact information
- • Specialist referral needs
5. Memory Aids & Clinical Mnemonics
“PILES” – Hemorrhoid Assessment
- Pain (usually absent unless thrombosed)
- Itching and irritation
- Lumps or prolapse
- Excessive bleeding (bright red)
- Soiling and mucus discharge
“TEAR” – Fissure Characteristics
- Tearing pain during defecation
- Exquisite tenderness
- Analgesic-resistant pain
- Rectal bleeding (small amounts)
“TRACT” – Fistula Features
- Tunnel connecting two surfaces
- Recurrent abscess episodes
- Abnormal drainage
- Chronic infection signs
- Treatment usually surgical
“NURSING” – Care Priorities
- Nutrition and fiber intake
- Understanding patient education
- Recognize complications early
- Sitz baths for comfort
- Infection prevention measures
- Non-pharmacological pain relief
- Gentle hygiene practices
Quick Reference: Time to Seek Help
Fiber Intake Guidelines
Sitz Bath Protocol
Clinical Pearls Summary
- • 90% of fissures occur in posterior midline
- • External hemorrhoids are painful only when thrombosed
- • Goodsall’s rule helps predict fistula tract direction
- • Conservative management succeeds in 80% of acute cases
- • Fiber without adequate fluids worsens constipation
Differential Diagnosis Quick Reference
| Feature | Hemorrhoids | Fissures | Fistulas |
|---|---|---|---|
| Primary Symptom | Painless bleeding, prolapse | Severe pain with defecation | Chronic drainage, recurrent abscess |
| Pain Pattern | Usually none (unless thrombosed) | Intense during/after BM | Dull, intermittent discomfort |
| Bleeding | Bright red, may be significant | Small amounts, bright red | Variable, often absent |
| Physical Finding | Enlarged vascular cushions | Linear mucosal tear | External opening with drainage |
| Treatment Approach | Conservative → procedural | Conservative → topical → surgical | Primarily surgical |
Key Takeaways for Nursing Practice
Evidence-Based Practice Points
- Conservative management is first-line for most anorectal conditions with 80% success rate
- Patient education on lifestyle modifications prevents recurrence in 70% of cases
- Early recognition and appropriate referral improve surgical outcomes significantly
- Holistic nursing care addressing physical and psychosocial needs enhances quality of life
Clinical Decision Making
- Always consider underlying conditions (IBD, malignancy) in atypical presentations
- Pain assessment guides treatment urgency and intervention selection
- Multidisciplinary approach optimizes outcomes for complex cases
- Continuous monitoring and follow-up prevent complications and ensure healing
Continuing Education Recommendations
Stay current with evolving treatment modalities, attend colorectal surgery conferences, and participate in interdisciplinary case discussions. Consider specialized certification in wound, ostomy, and continence nursing (CWOCN) for advanced practice in this area.
