🫀 HEPATITIS: Complete Nursing Guide
Comprehensive Study Notes for Nursing Students
📚 Table of Contents
🔬 Definition & Overview
Hepatitis is defined as inflammation of the liver tissue, characterized by hepatocyte injury and inflammatory cell infiltration. This condition can range from mild, self-limiting illness to severe, life-threatening liver failure. The term hepatitis encompasses various etiologies, with viral infections being the most common cause worldwide.
💡 Key Points to Remember
- Hepatitis affects over 325 million people globally
- Can be acute (lasting less than 6 months) or chronic (lasting more than 6 months)
- Leading cause of liver cirrhosis and hepatocellular carcinoma
- Preventable through vaccination and lifestyle modifications
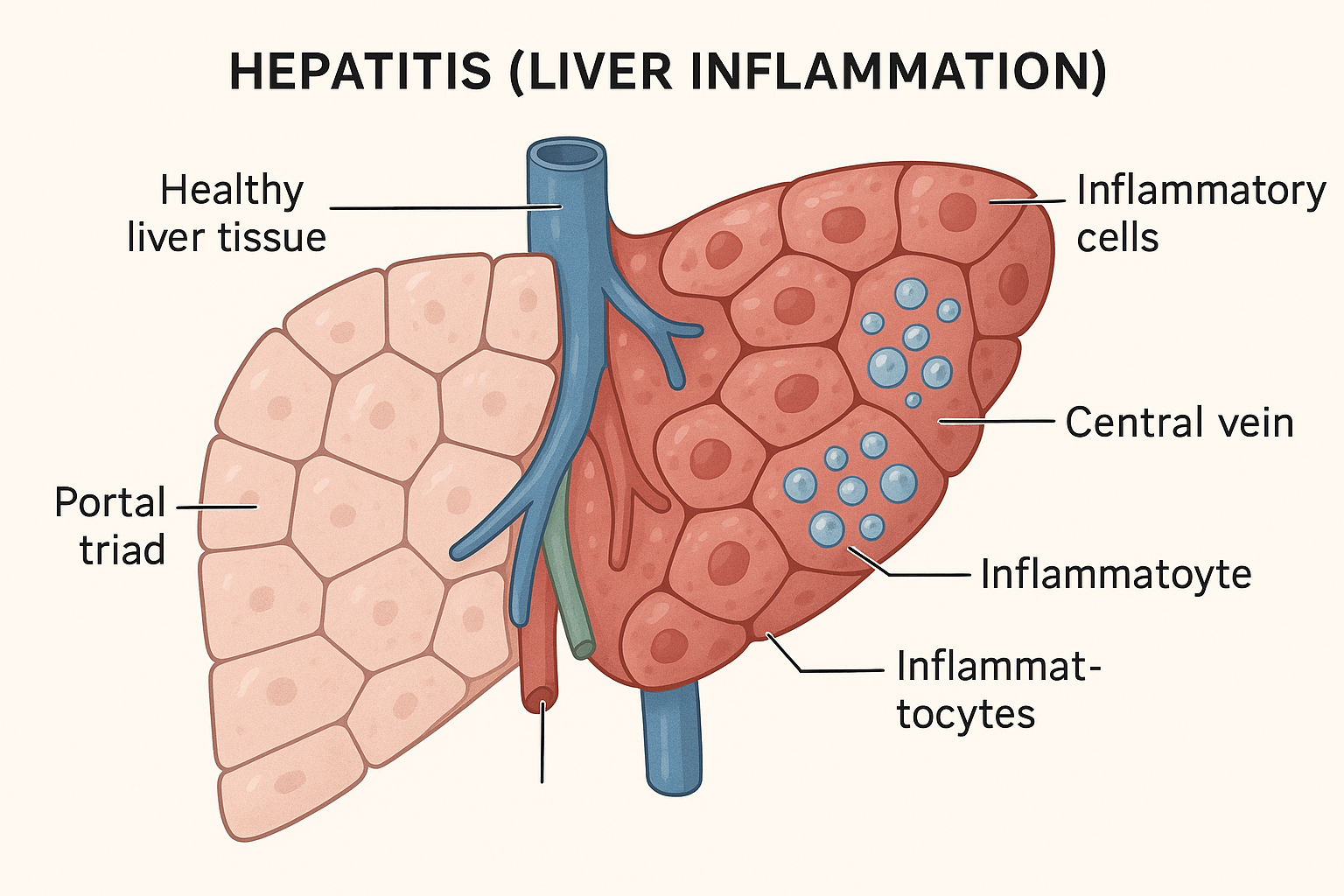
Figure 1: Hepatitis – Liver inflammation showing affected hepatocytes and inflammatory response
🧬 Pathophysiology
The pathophysiology of hepatitis involves complex immune-mediated responses that lead to hepatocyte damage and liver dysfunction. Understanding these mechanisms is crucial for effective nursing care and patient management.
Cellular Damage Mechanism
Primary Injury: Viral replication or toxic exposure causes direct hepatocyte damage
Secondary Injury: Inflammatory response activates Kupffer cells and releases cytokines
Immune Response: T-lymphocytes and natural killer cells target infected hepatocytes
Regeneration: Surviving hepatocytes proliferate to restore liver function
🧠 MNEMONIC: “LIVER”
Lymphocytes attack
Inflammation spreads
Viral replication occurs
Enzymes elevate
Regeneration follows
| Phase | Duration | Key Events | Clinical Manifestations |
|---|---|---|---|
| Incubation | 2-26 weeks | Viral replication begins | Asymptomatic |
| Prodromal | 1-2 weeks | Immune response activation | Fatigue, nausea, anorexia |
| Icteric | 2-6 weeks | Peak liver inflammation | Jaundice, dark urine, clay stools |
| Recovery | 6-12 weeks | Hepatocyte regeneration | Symptom resolution |
🦠 Types of Hepatitis
Hepatitis classification is essential for nursing students to understand transmission patterns, treatment approaches, and prevention strategies. Each type of hepatitis presents unique characteristics and nursing considerations.
Hepatitis A (HAV)
Transmission: Fecal-oral route
Duration: Acute only
Prevention: Vaccine available
Hepatitis B (HBV)
Transmission: Blood, sexual contact
Duration: Acute/Chronic
Prevention: Vaccine available
Hepatitis C (HCV)
Transmission: Bloodborne
Duration: Often chronic
Prevention: No vaccine
Hepatitis D (HDV)
Transmission: Co-infection with HBV
Duration: Acute/Chronic
Prevention: HBV vaccine
Hepatitis E (HEV)
Transmission: Fecal-oral route
Duration: Usually acute
Prevention: Sanitation measures
🧠 MNEMONIC: “A-B-C-D-E Routes”
Ass to mouth (fecal-oral)
Blood and body fluids
Contaminated needles
Depends on B
Environmental contamination
| Type | Incubation Period | Chronic Risk | Vaccine Available | Treatment |
|---|---|---|---|---|
| Hepatitis A | 15-50 days | No | Yes | Supportive care |
| Hepatitis B | 45-180 days | 5-10% adults | Yes | Antivirals, interferons |
| Hepatitis C | 14-180 days | 75-85% | No | Direct-acting antivirals |
| Hepatitis D | 21-140 days | High with HBV | HBV vaccine protects | Pegylated interferon |
| Hepatitis E | 15-60 days | Rare | Limited availability | Supportive care |
🎯 Etiology & Risk Factors
Understanding the diverse causes of hepatitis enables nurses to identify at-risk patients and implement appropriate preventive measures. Risk factors vary significantly based on the type of hepatitis and geographic location.
Viral Causes
- Hepatitis A Virus (HAV): RNA virus, highly contagious
- Hepatitis B Virus (HBV): DNA virus, blood-borne pathogen
- Hepatitis C Virus (HCV): RNA virus, major cause of chronic liver disease
- Hepatitis D Virus (HDV): Defective RNA virus requiring HBV co-infection
- Hepatitis E Virus (HEV): RNA virus, waterborne transmission
Non-Viral Causes
⚠️ Drug-Induced Hepatitis (DIH)
- Acetaminophen overdose (most common)
- Antibiotics (amoxicillin-clavulanate, isoniazid)
- Anti-seizure medications (phenytoin, valproic acid)
- Statins and NSAIDs
- Herbal supplements and alternative medicines
High-Risk Populations
| Risk Factor | Associated Type | Mechanism | Prevention Strategy |
|---|---|---|---|
| Intravenous drug use | HBV, HCV | Needle sharing | Needle exchange programs |
| Healthcare workers | HBV, HCV | Occupational exposure | Universal precautions, vaccination |
| Travel to endemic areas | HAV, HEV | Poor sanitation | Pre-travel vaccination, hygiene |
| Multiple sexual partners | HBV | Sexual transmission | Safe sex practices, vaccination |
| Blood transfusion (pre-1992) | HBV, HCV | Contaminated blood products | Screening, testing |
🎯 Signs & Symptoms
Recognizing the clinical manifestations of hepatitis is crucial for early diagnosis and intervention. Symptoms can vary greatly depending on the type of hepatitis, patient age, and immune status.
🧠 MNEMONIC: “JAUNDICED”
Jaundice (yellowing of skin/eyes)
Anorexia (loss of appetite)
Urine dark colored
Nausea and vomiting
Discomfort in RUQ
Itching (pruritus)
Clay-colored stools
Extreme fatigue
Diarrhea
Early Signs & Symptoms
Constitutional Symptoms
- Malaise and fatigue
- Low-grade fever
- Headache
- Myalgia
Gastrointestinal Symptoms
- Anorexia
- Nausea and vomiting
- Abdominal discomfort
- Diarrhea or constipation
Physical Examination
- Hepatomegaly
- Right upper quadrant tenderness
- Lymphadenopathy
- Splenomegaly (in some cases)
Specific Signs by Type
| Hepatitis Type | Distinctive Features | Onset Pattern | Severity |
|---|---|---|---|
| Hepatitis A | Sudden onset, flu-like symptoms | Acute, self-limiting | Mild to moderate |
| Hepatitis B | Gradual onset, joint pain | Insidious or acute | Variable |
| Hepatitis C | Often asymptomatic initially | Insidious | Usually mild |
| Hepatitis D | More severe than HBV alone | Acute with HBV | Severe |
| Hepatitis E | Similar to HAV, pregnancy complications | Acute | Mild, severe in pregnancy |
🚨 Red Flag Symptoms – Immediate Medical Attention Required
- Altered mental status: Confusion, disorientation (hepatic encephalopathy)
- Coagulopathy signs: Easy bruising, prolonged bleeding
- Ascites: Abdominal distension, fluid wave
- Severe jaundice: Bilirubin >10 mg/dL
- Persistent vomiting: Leading to dehydration
🔬 Diagnostic Tests
Accurate diagnosis of hepatitis requires a combination of laboratory tests, imaging studies, and clinical assessment. Understanding these diagnostic tools helps nurses interpret results and monitor patient progress effectively.
Laboratory Tests
🧪 Key Laboratory Values
| Test | Normal Range | Hepatitis Findings | Clinical Significance |
|---|---|---|---|
| ALT (Alanine Aminotransferase) | 7-40 U/L | 100-1000+ U/L | Hepatocyte damage marker |
| AST (Aspartate Aminotransferase) | 10-40 U/L | 100-1000+ U/L | Less specific than ALT |
| Total Bilirubin | 0.2-1.2 mg/dL | 2-20+ mg/dL | Liver function indicator |
| Alkaline Phosphatase | 44-147 U/L | Mildly elevated | Bile duct involvement |
| PT/INR | 11-13 sec/0.9-1.1 | Prolonged | Synthetic function |
| Albumin | 3.5-5.0 g/dL | Decreased in chronic | Protein synthesis |
Viral Markers
Hepatitis A Markers
- Anti-HAV IgM: Acute infection
- Anti-HAV IgG: Past infection or immunity
Hepatitis B Markers
- HBsAg: Active infection
- Anti-HBs: Immunity
- Anti-HBc IgM: Acute infection
- HBeAg: High infectivity
- HBV DNA: Viral load quantification
Hepatitis C Markers
- Anti-HCV: Exposure to virus
- HCV RNA: Active infection
- HCV genotype: Treatment selection
🧠 MNEMONIC: “ABC of Hepatitis Testing”
ALT/AST elevated (liver enzymes)
Bilirubin increased (jaundice marker)
Coagulation studies (PT/INR)
Imaging Studies
| Imaging Method | Purpose | Findings in Hepatitis | Nursing Considerations |
|---|---|---|---|
| Ultrasound | Initial assessment | Hepatomegaly, echogenicity changes | NPO 8-12 hours, positioning |
| CT Scan | Detailed evaluation | Liver size, density changes | Contrast allergy assessment |
| MRI | Advanced imaging | Tissue characterization | Metal screening, claustrophobia |
| Liver Biopsy | Histological diagnosis | Inflammation, fibrosis staging | Coagulation studies, consent |
👩⚕️ Nursing Assessment
Comprehensive nursing assessment of patients with hepatitis requires systematic evaluation of multiple body systems. Nurses play a critical role in early detection of complications and monitoring treatment response.
Primary Assessment – ABCDE Approach
🔍 Airway & Breathing
- Assess for signs of hepatic encephalopathy affecting airway protection
- Monitor respiratory status for ascites-related compromise
- Evaluate for pleural effusion (hepatic hydrothorax)
💓 Circulation
- Assess for signs of portal hypertension (spider angiomata, palmar erythema)
- Monitor for bleeding tendencies due to decreased clotting factors
- Evaluate fluid balance and signs of ascites
🧠 Disability/Neurological
- Assess mental status using Glasgow Coma Scale
- Monitor for asterixis (flapping tremor)
- Evaluate cognitive function and personality changes
Comprehensive Health History
Essential History Components
- Risk Factor Assessment: Travel history, sexual practices, drug use, occupational exposure
- Symptom Timeline: Onset, duration, progression of symptoms
- Medication History: Prescription drugs, over-the-counter medications, herbal supplements
- Family History: Liver disease, autoimmune conditions
- Social History: Alcohol consumption, smoking, living conditions
Physical Assessment by System
| Body System | Assessment Focus | Normal Findings | Hepatitis Findings |
|---|---|---|---|
| Integumentary | Skin color, integrity, lesions | Normal pigmentation, no lesions | Jaundice, pruritus, spider angiomata |
| Gastrointestinal | Abdomen inspection, palpation | Soft, non-tender abdomen | Hepatomegaly, RUQ tenderness, ascites |
| Neurological | Mental status, reflexes | Alert, oriented, normal reflexes | Confusion, asterixis, altered LOC |
| Cardiovascular | Heart rate, rhythm, perfusion | Regular rate and rhythm | Tachycardia, hyperdynamic circulation |
🧠 MNEMONIC: “HEPATIC Assessment”
History taking comprehensive
Eyes and skin for jaundice
Palpate liver and spleen
Abdomen assess for ascites
Tenderness in RUQ
Inspect for spider angiomata
Cognitive function evaluate
Pain Assessment
🎯 PQRST Pain Assessment for Hepatitis
- Provocation: What makes it better/worse?
- Quality: Sharp, dull, aching, cramping?
- Radiation: Does it spread to back/shoulder?
- Severity: Rate 0-10 pain scale
- Timing: Constant, intermittent, related to meals?
📋 Nursing Diagnoses
Nursing diagnoses for hepatitis patients focus on addressing physiological alterations, promoting healing, preventing complications, and supporting patient adaptation to illness. Priority diagnoses guide individualized care planning.
Priority Nursing Diagnoses
Primary Diagnoses
- Imbalanced Nutrition: Less than Body Requirements
- Deficient Fluid Volume
- Acute Pain
- Activity Intolerance
Secondary Diagnoses
- Risk for Infection
- Deficient Knowledge
- Anxiety
- Social Isolation
Potential Complications
- Risk for Bleeding
- Disturbed Thought Processes
- Excess Fluid Volume
- Impaired Skin Integrity
Detailed Nursing Diagnosis Framework
| Nursing Diagnosis | Related Factors | Evidence | Expected Outcomes |
|---|---|---|---|
| Imbalanced Nutrition: Less than Body Requirements | Anorexia, nausea, vomiting, malabsorption | Weight loss, decreased albumin, poor intake | Patient will maintain stable weight, adequate protein levels |
| Acute Pain | Liver inflammation, capsule distension | Patient reports RUQ pain 6/10, guarding | Pain will be controlled at acceptable level ≤3/10 |
| Activity Intolerance | Fatigue, weakness, decreased energy | Unable to perform ADLs, increased dyspnea | Patient will demonstrate improved activity tolerance |
| Risk for Infection | Immunosuppression, invasive procedures | Decreased WBC function, IV access | Patient will remain free from secondary infections |
🧠 MNEMONIC: “NANDA Hepatitis”
Nutrition imbalanced
Activity intolerance
Nausea and pain
Deficient knowledge
Anxiety and fear
Collaborative Problems
Potential Complications Requiring Medical Intervention
- PC: Hepatic Encephalopathy – Altered mental status, ammonia elevation
- PC: Bleeding – Coagulopathy, thrombocytopenia
- PC: Hepatorenal Syndrome – Progressive renal failure
- PC: Ascites – Fluid accumulation, electrolyte imbalance
- PC: Portal Hypertension – Varices, splenomegaly
🎯 Nursing Interventions
Nursing interventions for hepatitis patients encompass supportive care, symptom management, complication prevention, and health promotion. Evidence-based interventions focus on optimizing liver function and promoting recovery.
Immediate/Acute Care Interventions
🚨 Priority Interventions
- Monitor vital signs q4h: Temperature, BP, HR, RR, O2 saturation
- Assess neurological status q8h: LOC, orientation, presence of asterixis
- Monitor fluid balance: I&O, daily weights, assess for edema/ascites
- Laboratory monitoring: Liver enzymes, bilirubin, PT/INR, electrolytes
- Bleeding precautions: Soft toothbrush, electric razor, pad bed rails
Nutritional Support Interventions
🍽️ Nutritional Management
- Small frequent meals: 5-6 small meals to improve tolerance
- High-calorie, high-protein diet: 2500-3000 calories, 1.2-1.5g protein/kg
- Restrict sodium: <2g daily if ascites present
- Vitamin supplementation: B-complex, K, folate as ordered
- Avoid hepatotoxic substances: Alcohol, certain medications
- Monitor albumin levels: Indicator of synthetic function
Symptom Management
| Symptom | Nursing Interventions | Rationale | Evaluation Criteria |
|---|---|---|---|
| Nausea/Vomiting | Antiemetics, cool cloths, aromatherapy | Prevents dehydration, improves nutrition | Patient reports decreased nausea |
| Pruritus | Cool baths, calamine lotion, antihistamines | Reduces bile salt deposits in skin | Decreased scratching, skin integrity |
| Fatigue | Activity pacing, rest periods, energy conservation | Supports liver healing process | Improved activity tolerance |
| Abdominal Pain | Positioning, heat therapy, analgesics | Reduces inflammation-related discomfort | Pain level ≤3/10 |
🧠 MNEMONIC: “LIVER Care”
Laboratory monitoring frequent
Infection prevention measures
Vital signs assessment
Energy conservation techniques
Rest and nutrition support
Infection Control Measures
🦠 Isolation Precautions by Hepatitis Type
| Hepatitis Type | Precautions | Duration | Key Interventions |
|---|---|---|---|
| Hepatitis A | Contact precautions | 7 days after jaundice onset | Hand hygiene, gown/gloves |
| Hepatitis B | Standard precautions | Throughout hospitalization | Universal precautions, needle safety |
| Hepatitis C | Standard precautions | Throughout hospitalization | Blood/body fluid precautions |
Patient Safety Interventions
🛡️ Fall Prevention
- Assess fall risk using validated tools
- Ensure adequate lighting and clear pathways
- Assist with ambulation if weakness present
- Monitor for orthostatic hypotension
- Use bed alarms if appropriate
🩸 Bleeding Prevention
- Use soft-bristled toothbrush for oral care
- Apply pressure to venipuncture sites
- Avoid intramuscular injections when possible
- Monitor for signs of bleeding (epistaxis, bruising)
- Educate on injury prevention
💊 Medications
Medication management in hepatitis requires careful consideration of liver function, drug metabolism, and potential hepatotoxicity. Nurses must understand therapeutic regimens and monitor for adverse effects.
Antiviral Medications
| Medication | Indication | Mechanism | Nursing Considerations | Side Effects |
|---|---|---|---|---|
| Entecavir (Baraclude) | Chronic Hepatitis B | Nucleoside analog | Monitor renal function, take on empty stomach | Headache, dizziness, nausea |
| Tenofovir (Viread) | Chronic Hepatitis B | Nucleotide analog | Monitor bone density, renal function | Bone demineralization, nephrotoxicity |
| Sofosbuvir (Sovaldi) | Hepatitis C | NS5B polymerase inhibitor | Usually combined with other DAAs | Fatigue, headache, insomnia |
| Ledipasvir/Sofosbuvir (Harvoni) | Hepatitis C | Combination DAA | Check drug interactions, monitor HCV RNA | Fatigue, headache, nausea |
Supportive Medications
🎯 Symptom-Specific Medications
- Antiemetics: Ondansetron (Zofran), promethazine (Phenergan)
- Antihistamines: Diphenhydramine (Benadryl), hydroxyzine (Atarax) for pruritus
- Vitamins: Thiamine, folate, B-complex, vitamin K
- Lactulose: For hepatic encephalopathy prevention/treatment
- Diuretics: Spironolactone, furosemide for ascites management
⚠️ Medications to Avoid in Hepatitis
- Acetaminophen: High doses hepatotoxic (>4g/day)
- NSAIDs: Increased bleeding risk, renal toxicity
- Statins: Can worsen liver enzyme elevation
- Certain antibiotics: Isoniazid, ketoconazole
- Herbal supplements: Many have unknown hepatic effects
Direct-Acting Antivirals (DAAs) for Hepatitis C
🎯 DAA Therapy Nursing Management
- Pre-treatment assessment: HCV genotype, viral load, drug interactions
- During treatment: Monitor adherence, side effects, drug interactions
- Post-treatment: SVR testing at 12 weeks, monitor for reinfection
- Patient education: Importance of adherence, completion of full course
🧠 MNEMONIC: “MEDS for Hepatitis”
Monitor liver function regularly
Evaluate drug interactions
Dose adjustments may be needed
Side effects assessment crucial
Interferon Therapy
| Type | Indication | Administration | Nursing Monitoring |
|---|---|---|---|
| Pegylated Interferon α-2a | Chronic Hepatitis B, D | Weekly subcutaneous injection | CBC, liver function, depression screening |
| Interferon α-2b | Chronic Hepatitis B, C | 3x weekly injection | Flu-like symptoms, neutropenia, mood changes |
📚 Patient Education
Comprehensive patient education is essential for successful hepatitis management, prevention of transmission, and long-term health outcomes. Nurses play a vital role in providing culturally appropriate, evidence-based education.
Core Education Topics
Disease Understanding
- What hepatitis means
- Type-specific information
- Natural course of disease
- Prognosis and recovery
Transmission Prevention
- Mode of transmission
- When infectious
- Household precautions
- Sexual safety measures
Lifestyle Modifications
- Alcohol cessation
- Dietary recommendations
- Activity limitations
- Stress management
Dietary Education
🍽️ Nutritional Guidelines for Hepatitis Patients
| Food Category | Recommended | Avoid/Limit | Reason |
|---|---|---|---|
| Proteins | Lean meats, fish, eggs, legumes | High-fat meats, processed meats | Support liver regeneration |
| Carbohydrates | Whole grains, fruits, vegetables | Simple sugars, refined products | Provide sustained energy |
| Fats | Olive oil, avocados, nuts | Fried foods, saturated fats | Reduce liver workload |
| Fluids | Water, herbal teas | Alcohol, excessive caffeine | Maintain hydration, avoid toxins |
Medication Adherence Education
💊 Enhancing Medication Compliance
- Timing importance: Take medications at same time daily
- Duration emphasis: Complete entire course even if feeling better
- Side effect management: When to call healthcare provider
- Drug interactions: Avoid certain medications and substances
- Missed dose protocols: What to do if dose forgotten
🧠 MNEMONIC: “TEACH Hepatitis”
Transmission prevention methods
Eating healthy diet importance
Alcohol abstinence crucial
Compliance with medications
Healthcare follow-up essential
Activity and Rest Guidelines
🏃♀️ Activity Recommendations
- Acute phase: Bed rest initially, gradual activity increase
- Recovery phase: Light activities as tolerated
- Exercise guidelines: Avoid strenuous activity until liver enzymes normalize
- Work restrictions: May need modified duties or time off
- Travel considerations: Avoid areas with poor sanitation
When to Seek Medical Care
🚨 Red Flag Symptoms – Call Healthcare Provider Immediately
- Worsening jaundice: Deepening yellow color
- Confusion or drowsiness: Signs of hepatic encephalopathy
- Persistent vomiting: Unable to keep fluids down
- Bleeding: Easy bruising, nosebleeds, blood in stool
- Severe abdominal pain: Increasing or different pain pattern
- Fever >101°F: May indicate complications
Family and Household Education
| Hepatitis Type | Household Precautions | Sexual Partner Guidelines | Pregnancy Considerations |
|---|---|---|---|
| Hepatitis A | Hand hygiene, separate toileting | Avoid oral-anal contact | Vaccination if planning pregnancy |
| Hepatitis B | Don’t share personal items | Vaccination, barrier protection | Antiviral therapy, infant vaccination |
| Hepatitis C | Don’t share razors, toothbrushes | Low sexual transmission risk | Screen for vertical transmission |
⚠️ Complications
Hepatitis complications range from mild to life-threatening and require prompt recognition and intervention. Understanding potential complications helps nurses provide proactive care and early detection of deteriorating conditions.
Acute Complications
🚨 Fulminant Hepatic Failure
Definition: Rapid deterioration of liver function with encephalopathy developing within 8 weeks of symptom onset in patients without pre-existing liver disease.
- Signs: Altered mental status, coagulopathy, jaundice
- Causes: Viral hepatitis, drug toxicity, autoimmune hepatitis
- Mortality: 70-90% without transplantation
- Management: ICU care, liver transplant evaluation
Chronic Complications
| Complication | Pathophysiology | Clinical Manifestations | Nursing Management |
|---|---|---|---|
| Cirrhosis | Progressive fibrosis and scarring | Portal hypertension, ascites, varices | Monitor complications, nutrition support |
| Hepatocellular Carcinoma | Malignant transformation | Weight loss, abdominal mass, pain | Screening, symptom management |
| Portal Hypertension | Increased portal vein pressure | Splenomegaly, varices, ascites | Bleeding precautions, fluid monitoring |
| Hepatic Encephalopathy | Accumulated neurotoxins | Confusion, asterixis, coma | Ammonia reduction, safety measures |
🧠 MNEMONIC: “COMPLICATIONS”
Cirrhosis development
Oncology (liver cancer)
Mental status changes
Portal hypertension
Liver failure fulminant
Icterus prolonged
Coagulopathy severe
Ascites formation
Thrombocytopenia
Infection secondary
Organ failure multiple
Nephrotoxicity risk
Splenomegaly
Hepatic Encephalopathy Stages
| Stage | Mental Status | Neurological Signs | Nursing Interventions |
|---|---|---|---|
| Grade 1 | Mild confusion, euphoria | Tremor, apraxia | Orientation assessment, safety measures |
| Grade 2 | Drowsiness, inappropriate behavior | Asterixis, dysarthria | Frequent monitoring, fall prevention |
| Grade 3 | Stupor, marked confusion | Hyperreflexia, rigidity | Continuous observation, airway protection |
| Grade 4 | Coma | Decerebrate posturing | ICU care, intubation consideration |
Bleeding Complications
🩸 Hemorrhage Risk Assessment
- Esophageal varices: Life-threatening bleeding from portal hypertension
- Coagulopathy: Decreased clotting factors, prolonged PT/INR
- Thrombocytopenia: Low platelet count from hypersplenism
- GI bleeding: Peptic ulcers, portal gastropathy
Renal Complications
🫘 Hepatorenal Syndrome
Progressive kidney dysfunction in patients with advanced liver disease without intrinsic kidney disease.
- Type 1: Rapid progression, poor prognosis
- Type 2: Slower progression, better outcomes
- Treatment: Vasoconstrictors, albumin, liver transplant
- Nursing care: Fluid balance, electrolyte monitoring
🛡️ Prevention Strategies
Prevention remains the most effective approach to controlling hepatitis. Comprehensive prevention strategies include vaccination, safe practices, screening programs, and public health measures tailored to specific hepatitis types.
Vaccination Programs
💉 Hepatitis Vaccines
| Vaccine | Target Population | Schedule | Efficacy | Duration |
|---|---|---|---|---|
| Hepatitis A | Children >1 year, high-risk adults | 2 doses, 6-12 months apart | 95-100% | 20+ years |
| Hepatitis B | All infants, high-risk adults | 3 doses over 6 months | 90-95% | Lifelong |
| Hepatitis A+B | High-risk individuals | 3 doses over 6 months | 95%+ for both | Long-term |
🧠 MNEMONIC: “PREVENT Hepatitis”
Pre-exposure vaccination
Risk factor modification
Education and awareness
Viral load monitoring
Exposure prophylaxis
Needle safety practices
Transmission route blocking
Universal Precautions
🧤 Standard Infection Control
- Hand hygiene: Wash hands before and after patient contact
- Personal protective equipment: Gloves, gowns, masks as appropriate
- Safe injection practices: One needle, one syringe, one time
- Sharps safety: Never recap needles, use safety devices
- Environmental cleaning: Disinfect surfaces with appropriate agents
High-Risk Group Interventions
| Risk Group | Specific Interventions | Screening Recommendations | Follow-up Care |
|---|---|---|---|
| Healthcare Workers | HBV vaccination, post-exposure prophylaxis | Annual HBV antibody testing | Booster vaccines if indicated |
| PWID (People Who Inject Drugs) | Needle exchange, HAV/HBV vaccination | HCV testing every 6-12 months | Treatment referral, harm reduction |
| MSM (Men who have Sex with Men) | HAV/HBV vaccination, safe sex education | Annual STI/hepatitis screening | Partner notification, treatment |
| Pregnant Women | Universal HBV screening, treatment | Screen at first prenatal visit | Infant immunoprophylaxis |
Community-Based Prevention
Public Health Measures
- Water sanitation improvement
- Food safety regulations
- Blood supply screening
- Waste management systems
Education Campaigns
- Community awareness programs
- School-based education
- Healthcare provider training
- Media campaigns
Screening Programs
- Birth cohort screening (HCV)
- High-risk population testing
- Healthcare facility screening
- Contact tracing
Post-Exposure Prophylaxis
🚨 Emergency Response Protocols
- Hepatitis A exposure: HAV vaccine or immunoglobulin within 2 weeks
- Hepatitis B exposure: HBIG + vaccine series within 24 hours (preferably within 7 days)
- Hepatitis C exposure: No prophylaxis available; monitor and test
- Occupational exposure: Report immediately, follow institutional protocols
📈 Prognosis & Outcomes
The prognosis of hepatitis varies significantly based on the type of virus, patient factors, and timing of treatment initiation. Understanding prognostic factors helps nurses provide appropriate patient education and support.
Prognosis by Hepatitis Type
| Type | Acute Recovery Rate | Chronic Development | Long-term Outcomes | Mortality Risk |
|---|---|---|---|---|
| Hepatitis A | 99% | Never | Complete recovery, lifelong immunity | <0.1% |
| Hepatitis B | 90-95% adults | 5-10% adults, 90% infants | Variable; can lead to cirrhosis, HCC | 1-2% acute |
| Hepatitis C | 15-25% | 75-85% | 20-30% develop cirrhosis over 20 years | 1-5% with cirrhosis |
| Hepatitis D | Variable | High with chronic HBV | More severe than HBV alone | 2-20% |
| Hepatitis E | 95% | Rare | Usually complete recovery | 1-3%, 15-25% pregnant women |
Prognostic Factors
🎯 Factors Affecting Prognosis
- Age at infection: Younger age generally better outcomes
- Immune status: Immunocompromised patients have worse prognosis
- Co-infections: HIV, HBV/HCV co-infection worsen outcomes
- Alcohol use: Accelerates progression to cirrhosis
- Gender: Males may have more severe disease progression
- Treatment compliance: Early treatment improves outcomes significantly
Chronic Hepatitis Progression
🧠 MNEMONIC: “STAGES of Liver Disease”
Steatosis (fatty liver)
Telangiectasia (spider angiomata)
Ascites development
Gastroesophageal varices
Encephalopathy hepatic
Severity increasing
Quality of Life Outcomes
Physical Health
- Fatigue levels
- Activity tolerance
- Pain management
- Sleep quality
Psychological Health
- Depression rates
- Anxiety levels
- Cognitive function
- Coping mechanisms
Social Functioning
- Work productivity
- Social relationships
- Stigma experiences
- Family dynamics
Survival Rates and Statistics
📊 Long-term Survival Data
- Compensated cirrhosis: 10-year survival rate 80-90%
- Decompensated cirrhosis: 5-year survival rate 50%
- Hepatocellular carcinoma: 5-year survival rate 18%
- Post-liver transplant: 5-year survival rate 75%
- HCV cure with DAAs: >95% sustained virologic response
Factors Improving Prognosis
✅ Positive Prognostic Interventions
- Early diagnosis and treatment: Prevents progression to advanced stages
- Lifestyle modifications: Alcohol cessation, weight management
- Regular monitoring: Early detection of complications
- Vaccination: Prevention of additional hepatitis infections
- Patient education: Improved adherence and self-management
🌍 Global Best Practices
International experiences in hepatitis management provide valuable insights for improving patient outcomes. These global best practices demonstrate innovative approaches to prevention, treatment, and care delivery.
World Health Organization Initiatives
🎯 WHO Global Hepatitis Strategy 2030
- Prevention goals: 90% reduction in new infections
- Treatment targets: 80% of eligible patients receive treatment
- Mortality reduction: 65% reduction in hepatitis-related deaths
- Testing objectives: 90% of infections diagnosed
Country-Specific Success Stories
| Country/Region | Innovation | Implementation | Outcomes Achieved |
|---|---|---|---|
| Australia | National HCV elimination program | Universal DAA access, point-of-care testing | 75% reduction in new infections |
| Rwanda | Integrated HBV/HIV care | Combined screening and treatment programs | 90% HBV vaccination coverage |
| Egypt | Mass HCV screening campaign | Population-wide testing and treatment | Reduced prevalence from 10% to 0.4% |
| Scotland | Prison-based testing programs | Routine testing in correctional facilities | 70% increase in diagnosis rates |
Innovation in Care Delivery Models
Telemedicine Programs
- Remote consultation services
- Mobile health applications
- Digital medication adherence
- Virtual reality education
Community-Based Care
- Peer support networks
- Community health workers
- Mobile testing units
- Pharmacy-based services
Integrated Healthcare
- One-stop service centers
- Multi-disciplinary teams
- Electronic health records
- Coordinated care pathways
Innovative Prevention Strategies
🚀 Cutting-Edge Prevention Approaches
- Micro-elimination programs: Targeting specific high-risk populations
- Birth dose vaccination: HBV vaccine within 24 hours of birth
- Harm reduction services: Needle exchange, supervised injection sites
- Pre-exposure prophylaxis: For high-risk individuals
- Social media campaigns: Targeted awareness and education
Technology Integration
💻 Digital Health Solutions
- Point-of-care testing: Rapid diagnosis in community settings
- Electronic medical records: Improved care coordination
- Mobile applications: Medication reminders, symptom tracking
- Artificial intelligence: Risk stratification, treatment optimization
- Blockchain technology: Secure health data management
🧠 MNEMONIC: “GLOBAL Success”
Government commitment strong
Leadership in healthcare
Outreach programs comprehensive
Best practices implementation
Access to treatment universal
Local adaptation essential
Policy and Healthcare System Integration
🏛️ Key Policy Recommendations
- Universal health coverage: Include hepatitis care in essential packages
- Price negotiations: Reduce DAA costs through generic competition
- Task shifting: Train non-specialists in hepatitis care
- Quality assurance: Standardize care protocols and outcomes
- Data systems: Strengthen surveillance and monitoring
Future Directions
🔮 Emerging Trends in Hepatitis Care
- Gene therapy: Potential cure for chronic hepatitis B
- Personalized medicine: Tailored treatment based on genetics
- Immunotherapy: Enhance immune response to clear infection
- Nanotechnology: Targeted drug delivery systems
- Prevention vaccines: Universal hepatitis vaccines in development
