High Fever in Newborns
Comprehensive Nursing Assessment and Management
Educational Notes for Nursing Students
Table of Contents
- Introduction
- Definition and Classification
- Pathophysiology of Fever in Newborns
- Etiology and Risk Factors
- Clinical Manifestations
- Nursing Assessment
- Nursing Diagnosis
- Nursing Interventions
- Medical Management and Treatment
- Complications and Prevention
- Parental Education
- Mnemonics for Clinical Practice
- Case Study
- Global Best Practices
- References
Introduction
Fever in a newborn is a critical clinical sign that requires immediate attention and thorough assessment by healthcare professionals. Unlike older children and adults, newborns have immature immune systems and underdeveloped thermoregulatory mechanisms, making them particularly vulnerable to infections and complications associated with elevated body temperature.
For nursing professionals, understanding how to properly assess, manage, and provide care for newborns with fever is essential to prevent serious complications and ensure optimal outcomes.
This comprehensive guide will equip nursing students with the knowledge and tools necessary to effectively care for newborns presenting with fever, from initial assessment to ongoing management and parental education.
Definition and Classification
What is Fever in a Newborn?
A fever in a newborn is formally defined as a rectal or forehead (temporal) temperature of 100.4°F (38°C) or higher. This temperature threshold is crucial as it distinguishes normal temperature variation from pathological elevation requiring medical intervention.
Normal Temperature Ranges in Newborns
Normal body temperature in newborns varies slightly based on the measurement method:
| Measurement Method | Normal Range | Fever Threshold |
|---|---|---|
| Rectal (Gold Standard) | 97.9°F – 100.3°F (36.6°C – 37.9°C) | ≥ 100.4°F (38°C) |
| Axillary (Armpit) | 97.5°F – 99.3°F (36.4°C – 37.4°C) | ≥ 99.4°F (37.4°C) |
| Temporal Artery (Forehead) | 97.5°F – 100.3°F (36.4°C – 37.9°C) | ≥ 100.4°F (38°C) |
| Tympanic (Ear) | 97.7°F – 100.3°F (36.5°C – 37.9°C) | ≥ 100.4°F (38°C) |
Note: Rectal temperature measurement is considered the most accurate method for newborns but should be performed carefully by trained healthcare professionals.
Classification of Fever in Newborns
Based on severity:
- Low-grade fever: Temperature between 100.4°F (38°C) and 102.2°F (39°C)
- Moderate fever: Temperature between 102.2°F (39°C) and 104°F (40°C)
- High fever: Temperature above 104°F (40°C)
Based on onset and duration:
- Acute fever: Sudden onset, lasting less than 7 days
- Persistent fever: Lasting more than 7 days
- Recurrent fever: Episodes of fever separated by fever-free intervals of at least 24 hours
IMPORTANT: Any fever in a newborn under 28 days of age is considered a medical emergency and requires immediate evaluation, regardless of severity or duration.
Pathophysiology of Fever in Newborns
Understanding the underlying mechanisms of fever in newborns is essential for appropriate nursing assessment and interventions.
Thermoregulation in Newborns
Newborns have limited ability to regulate their body temperature due to:
- Immature hypothalamic temperature control center
- Higher body surface area to mass ratio (increased heat loss)
- Limited subcutaneous fat (reduced insulation)
- Inability to shiver effectively
- Limited ability to sweat
- Reduced metabolic responses to cold stress
Fever Generation Process
- Pathogen introduction: Infection triggers immune response
- Pyrogen release: Immune cells release endogenous pyrogens (IL-1, IL-6, TNF-α)
- Hypothalamic signaling: Pyrogens cross blood-brain barrier and stimulate prostaglandin E2 (PGE2) production
- Thermostat elevation: PGE2 increases hypothalamic temperature set point
- Physiologic response: Body initiates heat-conserving and heat-generating mechanisms
- Fever manifestation: Core temperature rises to match new set point
Clinical Insight: In newborns, the fever response may be blunted or absent even in serious infections, while in other cases, environmental factors can cause temperature elevation without infection. This makes careful assessment vital.
Etiology and Risk Factors
Common Causes of Fever in Newborns
| Category | Specific Causes |
|---|---|
| Infections |
|
| Specific Infections |
|
| Non-infectious Causes |
|
Risk Factors for Neonatal Fever and Sepsis
Maternal Risk Factors
- Maternal GBS colonization
- Chorioamnionitis
- Prolonged rupture of membranes (>18 hours)
- Premature rupture of membranes
- Maternal fever during labor (>38°C/100.4°F)
- Inadequately treated maternal UTI
- Limited or no prenatal care
- Intrapartum antibiotic prophylaxis less than 4 hours before delivery
Neonatal Risk Factors
- Prematurity (<37 weeks gestation)
- Low birth weight (<2500g)
- Male gender
- Congenital anomalies
- Invasive procedures (central lines, intubation)
- Prolonged hospitalization
- Twin or multiple birth
- Galactosemia
- Perinatal asphyxia
Important Distinction: Early-onset sepsis (within first 72 hours) is typically associated with maternal risk factors and vertical transmission, while late-onset sepsis (after 72 hours) is more commonly associated with postnatal environmental exposure and healthcare-associated infections.
Clinical Manifestations
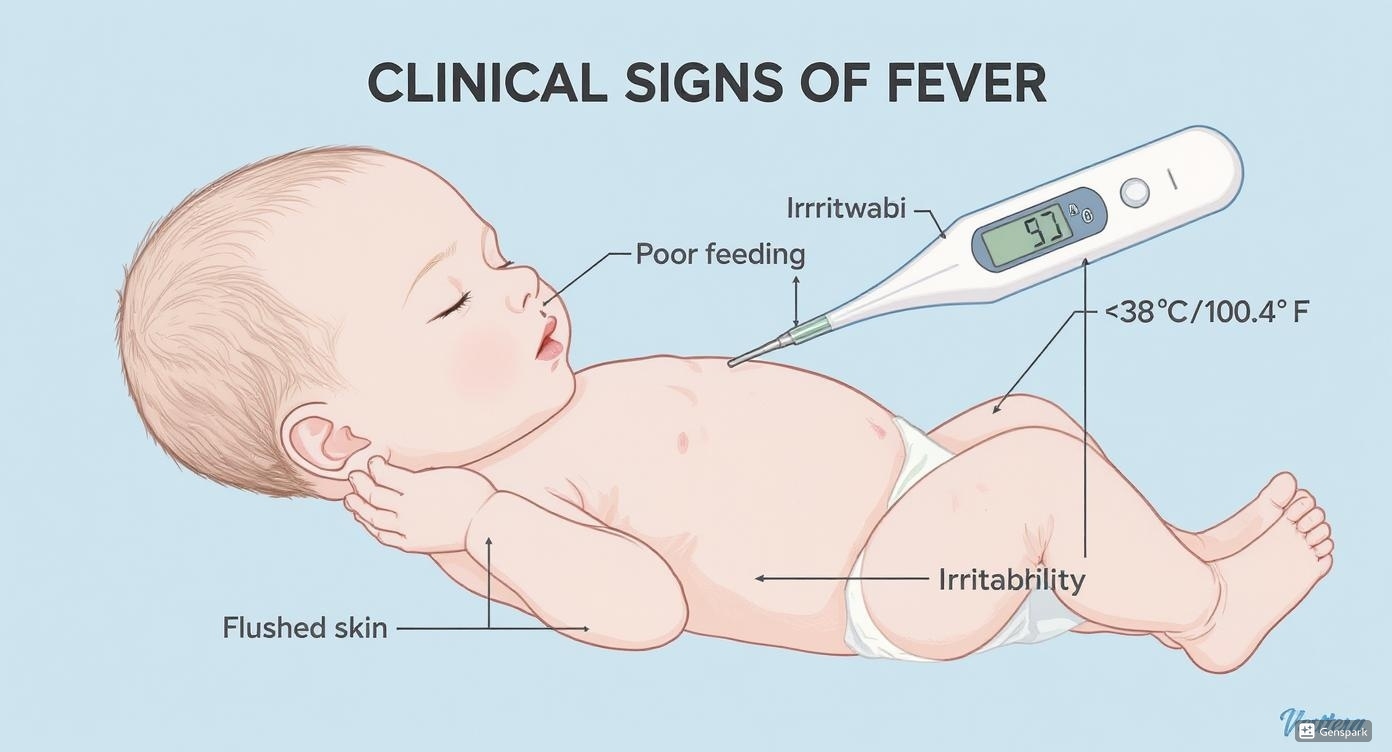
Fig 1: Clinical Signs of Fever in Newborns
Recognizing the clinical manifestations of fever in newborns is crucial, as signs can be subtle and nonspecific. Unlike older children or adults, newborns may not display typical signs of infection despite serious illness.
Primary Signs and Symptoms
Thermoregulatory Signs
- Elevated temperature (≥38°C/100.4°F rectal)
- Temperature instability (fluctuations)
- Hypothermia (can be a sign of severe infection)
- Warm to touch, especially trunk
- Flushed skin or mottling
Behavioral Changes
- Lethargy or decreased activity
- Irritability and inconsolable crying
- Poor feeding or feeding refusal
- Decreased responsiveness
- Altered sleep patterns
Secondary Signs by System
| Body System | Clinical Manifestations |
|---|---|
| Respiratory |
|
| Cardiovascular |
|
| Gastrointestinal |
|
| Neurological |
|
| Integumentary |
|
Critical Nursing Alert: The absence of fever does not rule out serious infection in newborns. Hypothermia can be a sign of overwhelming infection. Always assess the whole clinical picture rather than relying on temperature alone.
Nursing Assessment
A thorough nursing assessment is critical for early detection and appropriate management of fever in newborns. The assessment should be systematic and comprehensive.
Temperature Measurement Techniques
| Method | Procedure | Considerations |
|---|---|---|
| Rectal |
|
|
| Axillary |
|
|
| Temporal Artery |
|
|
| Tympanic |
|
|
Comprehensive Assessment Framework: The ABCDEF Approach
A: Airway and Breathing
- Assess respiratory rate, rhythm, and effort
- Note presence of nasal flaring, grunting, retractions
- Auscultate lung sounds for crackles or diminished breath sounds
- Check oxygen saturation
- Observe for apnea episodes
B: Blood Circulation
- Monitor heart rate and blood pressure
- Assess capillary refill time
- Check peripheral pulses
- Observe skin color and temperature
- Note signs of poor perfusion (mottling, cyanosis)
C: Core Temperature & Consciousness
- Measure temperature using appropriate method
- Assess level of consciousness, alertness
- Check primitive reflexes (Moro, sucking, rooting)
- Note responsiveness to stimulation
- Assess fontanelle (bulging, sunken)
D: Diaper & Digestion
- Note feeding patterns, interest in feeding
- Check for vomiting and characteristics
- Assess abdominal distention or tenderness
- Monitor urine output and stool patterns
- Check for signs of dehydration
E: Examination & Exposure
- Perform head-to-toe skin assessment
- Look for rashes, lesions, purpura
- Check umbilical cord site for signs of infection
- Assess cry quality and strength
- Note posture and movement
F: Family & Factors
- Collect detailed maternal history
- Note birth history and risk factors
- Ask about family illness or exposures
- Assess environmental factors (overheating, overdressing)
- Document prior antibiotic use or recent procedures
Diagnostic Studies
Nurses should be familiar with common diagnostic studies ordered for newborns with fever:
| Study | Purpose | Nursing Considerations |
|---|---|---|
| Complete Blood Count (CBC) | Assess for leukocytosis, leukopenia, thrombocytopenia, anemia | Collect before antibiotics if possible; minimize blood volume |
| Blood Culture | Identify causative organisms | Sterile collection technique; adequate volume (1-2 mL); before antibiotics |
| Urinalysis and Culture | Identify urinary tract infections | Sterile catheterization or suprapubic aspiration needed |
| Lumbar Puncture | Evaluate for meningitis | Position support; monitor vital signs; comfort measures after procedure |
| C-reactive Protein (CRP) | Non-specific inflammation marker | May be elevated 6-12 hours after onset of infection |
| Procalcitonin | Early marker of bacterial infection | More specific than CRP; rises within 2-4 hours of infection |
| Chest X-ray | Assess for pneumonia | Minimize exposure; proper positioning and immobilization |
| Viral Studies | Identify viral pathogens | May include nasal swabs, blood PCR for HSV, enterovirus |
Clinical Tip: When caring for a febrile newborn, remember that lab values may be different from older children. For example, a normal white blood cell count in a newborn is 9,000-30,000 cells/μL, and bilirubin levels are naturally higher.
Nursing Diagnosis
Based on the comprehensive assessment of a newborn with fever, several nursing diagnoses may be appropriate. These diagnoses guide the development of specific interventions and care plans.
Primary Nursing Diagnoses for Newborns with Fever
1. Hyperthermia related to infectious process as evidenced by body temperature ≥38°C (100.4°F)
This addresses the primary presenting problem of elevated body temperature and focuses interventions on temperature management.
2. Risk for Ineffective Thermoregulation related to immature regulatory mechanisms and infectious process
This diagnosis recognizes the vulnerability of newborns to temperature instability, including both hyper- and hypothermia.
3. Risk for Deficient Fluid Volume related to increased metabolic rate, decreased oral intake, and insensible losses
Addresses potential dehydration risk associated with fever, especially if the newborn is feeding poorly.
4. Risk for Infection (Sepsis) related to immature immune system and presence of infectious organisms
Recognizes the risk of progression from localized infection to systemic infection.
5. Imbalanced Nutrition: Less Than Body Requirements related to increased metabolic needs and decreased feeding
Addresses nutritional concerns due to increased caloric needs during fever and possible decreased intake.
6. Interrupted Family Processes related to crisis of infant illness and hospitalization
Recognizes the impact of the newborn’s illness on the family unit and parent-infant bonding.
7. Anxiety (Parental) related to unknown outcome of infant’s condition
Addresses the psychological impact on parents when their newborn is ill.
8. Deficient Knowledge related to lack of information about newborn fever management and warning signs
Focuses on educational needs of parents/caregivers regarding care of the infant.
Documentation Tip: When writing nursing diagnoses for newborns with fever, include all three components: problem statement, related factors (etiology), and defining characteristics (evidence). This ensures a comprehensive care approach.
Nursing Interventions
Effective nursing care for newborns with fever requires a combination of assessment, monitoring, therapeutic interventions, and family support. Below are evidence-based nursing interventions organized by priority.
Monitoring and Assessment Interventions
- Continuous monitoring of vital signs
- Monitor temperature every 1-2 hours using consistent method
- Assess heart rate, respiratory rate, and blood pressure every 2-4 hours
- Monitor oxygen saturation continuously or every 4 hours
- Document trends and report significant changes
- Fluid balance monitoring
- Maintain strict intake and output record
- Weigh diapers to estimate urine output
- Monitor for signs of dehydration (decreased urine output, dry mucous membranes, sunken fontanelle)
- Track daily weights at the same time with same scale
- Neurological assessment
- Assess level of consciousness and irritability
- Monitor fontanelle for bulging or depression
- Evaluate muscle tone and reflexes
- Report seizures or abnormal movements immediately
- Feeding assessment
- Monitor feeding interest, duration, and volume
- Assess sucking and swallowing ability
- Document episodes of vomiting or feeding intolerance
- Track nutritional intake relative to requirements
Therapeutic Interventions
Temperature Management
- Avoid overdressing or overbundling
- Maintain neutral thermal environment
- Use only lightweight clothing or blankets
- If in incubator, adjust temperature settings according to protocol
- Consider tepid sponging only if ordered and temperature is significantly elevated
- Administer antipyretics (acetaminophen) only if prescribed, noting that routine antipyretic use is not recommended for all febrile newborns
Fluid Management
- Administer IV fluids if prescribed, ensuring correct rate and solution
- Support oral feeding when appropriate
- Offer small, frequent feedings if tolerated
- Coordinate oral care with dry mucous membranes
- Monitor IV sites for signs of infiltration or phlebitis
Infection Control and Medication Administration
- Implement strict hand hygiene before and after contact
- Administer antibiotics precisely as ordered (correct dose, timing, route)
- Monitor for adverse drug reactions
- Obtain laboratory specimens as ordered
- Practice aseptic technique for all invasive procedures
- Properly dispose of contaminated materials
Comfort Measures
- Position for comfort and optimal airway maintenance
- Provide pacifier for non-nutritive sucking if acceptable
- Implement gentle handling and clustering of care
- Minimize environmental stressors (noise, bright lights)
- Provide containment holding when appropriate
- Encourage parental presence and gentle touch
Family Support and Education
- Communication with parents
- Explain all procedures and their purpose
- Provide updates on infant’s condition
- Address parental concerns and questions
- Use clear, non-medical language when possible
- Education on fever management
- Teach proper temperature measurement
- Explain warning signs requiring medical attention
- Discuss appropriate clothing and environmental temperature
- Review medication administration if prescribed
- Support for parental involvement
- Encourage parental participation in care when appropriate
- Support breastfeeding or expression of breast milk
- Promote skin-to-skin contact when medically stable
- Teach parents to recognize signs of improvement or deterioration
- Discharge planning (when appropriate)
- Provide written home care instructions
- Ensure follow-up appointments are scheduled
- Discuss infection prevention at home
- Review when to seek emergency care
Evidence-Based Practice Alert: Current guidelines do not recommend routine antipyretic use for all newborns with fever. Treatment focuses on identifying and addressing the underlying cause rather than just reducing the temperature. Antipyretics should only be used when specifically prescribed by the physician.
Medical Management and Treatment
While nursing care is fundamental for newborns with fever, medical management addresses the underlying causes. Nurses need to understand the medical approach to collaborate effectively in the care team.
Initial Management Approach
The approach to managing fever in newborns depends on the infant’s age, clinical appearance, and risk factors:
| Age Group | Standard Approach |
|---|---|
| 0-28 days (Neonates) |
|
| 29-60 days |
|
| 61-90 days |
|
Antimicrobial Therapy
Empiric Antimicrobial Therapy
Initial antimicrobial therapy for febrile newborns is broad-spectrum until pathogen identification:
| Age/Condition | First-Line Therapy | Alternative Therapy |
|---|---|---|
| Early-onset sepsis (<72 hours) | Ampicillin + Gentamicin | Ampicillin + Cefotaxime |
| Late-onset sepsis (>72 hours) | Ampicillin + Cefotaxime | Vancomycin + Gentamicin |
| Suspected meningitis | Ampicillin + Cefotaxime | Ampicillin + Gentamicin + Acyclovir (if HSV suspected) |
| Hospital-acquired infection | Vancomycin + Gentamicin | Based on local antibiogram |
Key Considerations for Antimicrobial Therapy
- Dosing is weight-based and requires precise calculation
- Renal function monitoring is essential with aminoglycosides
- Duration typically 7-14 days depending on infection site and organism
- De-escalation to narrower coverage once cultures identify specific pathogen
- Therapeutic drug monitoring may be needed for certain antibiotics
Supportive Care
Fluid and Electrolyte Management
- IV fluid rate based on weight and physiologic needs
- Typically 60-100 mL/kg/day plus deficit replacement
- Regular electrolyte monitoring
- Adjustment based on clinical status
Respiratory Support
- Oxygen supplementation if needed
- Positioning for optimal breathing
- Potential need for CPAP or ventilation if respiratory failure
- Regular assessment of respiratory status
Nutritional Support
- NPO status initially for severely ill newborns
- Early enteral feeding when clinically stable
- Parenteral nutrition if prolonged NPO status
- Breast milk preferred when feeding initiated
Seizure Management
- Anticonvulsant therapy if seizures present
- Common agents: Phenobarbital, Levetiracetam
- Close neurological monitoring
- EEG monitoring in cases of suspected seizures
Monitoring Response to Treatment
Signs of Improvement
- Normalization of temperature
- Improved feeding
- Decreased irritability
- Stable vital signs
- Improved activity level
- Negative follow-up cultures
- Normalization of laboratory values
Treatment Failure Signs
- Persistent or recurrent fever despite 48 hours of antibiotics
- Worsening clinical status
- Development of new symptoms
- Persistent positive cultures
- Development of complications
Critical Alert: Any deterioration in a newborn’s clinical status should prompt immediate notification of the medical team. Signs such as decreased responsiveness, respiratory distress, poor perfusion, or abnormal movements require urgent reassessment and potential escalation of care.
Complications and Prevention
Understanding potential complications of fever in newborns and implementing preventive strategies are essential aspects of nursing care.
Potential Complications
Short-Term Complications
| Complication | Signs/Impact |
|---|---|
| Dehydration | Poor skin turgor, dry mucous membranes, sunken fontanelle, decreased urine output |
| Seizures | Abnormal movements, eye deviation, apnea, posturing |
| Septic Shock | Poor perfusion, hypotension, metabolic acidosis, altered mental status |
| Meningitis | Bulging fontanelle, irritability, lethargy, seizures |
| Respiratory Failure | Increased work of breathing, hypoxemia, need for ventilatory support |
Long-Term Complications
| Complication | Impact |
|---|---|
| Neurodevelopmental Impairment | Developmental delays, cerebral palsy, learning disabilities |
| Hearing Loss | Sensorineural hearing deficit from meningitis or ototoxic medications |
| Visual Impairment | Visual processing disorders, cortical visual impairment |
| Chronic Organ Dysfunction | Renal scarring, bronchopulmonary dysplasia, endocrine dysfunction |
| Growth Issues | Failure to thrive, growth delays |
Risk Factors for Complications
- Prematurity: Immature organ systems and immune function
- Delayed presentation: Treatment initiated after 24+ hours of symptoms
- Virulent pathogens: Certain organisms like GBS, E. coli, HSV have higher complication rates
- Meningeal involvement: Infections of the CNS
- Congenital anomalies: Structural or functional abnormalities
- Immunodeficiency: Congenital or acquired immune dysfunction
- Septic shock: Circulatory compromise significantly increases morbidity and mortality
Prevention Strategies
Prenatal and Perinatal Prevention
- Maternal GBS screening at 35-37 weeks
- Appropriate intrapartum antibiotic prophylaxis
- Treatment of maternal infections during pregnancy
- Sterile techniques during delivery and cord care
- Maternal immunization (influenza, Tdap)
- Prompt treatment of chorioamnionitis
Postnatal Prevention
- Strict hand hygiene by all caregivers
- Proper umbilical cord care
- Early breastfeeding initiation
- Exclusive breastfeeding when possible
- Limited exposure to ill contacts
- Prompt evaluation of at-risk infants
- Education of parents on warning signs
Nursing Role in Prevention
- Education and Counseling
- Teach parents about proper hygiene practices
- Educate about appropriate environmental temperature
- Instruct on early recognition of fever and infection signs
- Discuss the importance of limiting exposure to sick contacts
- Infection Control
- Implement and model proper hand hygiene
- Ensure aseptic technique during procedures
- Monitor visitors for signs of illness
- Properly clean and disinfect equipment
- Support for Optimal Nutrition
- Promote and support breastfeeding
- Provide lactation support resources
- Ensure proper formula preparation if used
- Monitor growth and feeding patterns
- Advocacy and Follow-up
- Ensure appropriate discharge planning
- Facilitate follow-up appointments
- Connect families with community resources
- Advocate for appropriate screening and prevention measures
Evidence-Based Insight: Research shows that early initiation of antibiotics in febrile newborns (within 1 hour of recognition) reduces mortality rates by approximately 7.6% for each hour of delay avoided. This highlights the importance of prompt nursing recognition and response to fever in newborns.
Parental Education
Effective parental education is crucial for ensuring appropriate management of newborns with fever and preventing complications. Nurses play a vital role in providing clear, practical information to parents.
Essential Education Topics
Temperature Measurement
- Demonstrate proper technique for taking temperature
- Recommend appropriate thermometer type (rectal or temporal for newborns)
- Teach how to read and interpret temperature results
- Explain normal temperature ranges
- Advise on frequency of temperature checks when concerned
Warning Signs Requiring Medical Attention
- Any temperature ≥100.4°F (38°C) in a newborn under 3 months
- Poor feeding (missing multiple feedings)
- Significant decrease in wet diapers (fewer than 4-6 per day)
- Extreme irritability or lethargy
- Difficulty breathing or rapid breathing
- Unusual rash or skin color changes (pale, blue, or mottled)
- Bulging fontanelle
- Seizure-like activity
- Persistent vomiting
Home Care Instructions
- Appropriate clothing (light, breathable layers)
- Optimal room temperature (68-72°F/20-22°C)
- Proper positioning for comfort and airway clearance
- Feeding recommendations during illness
- Skin and diaper area care
- Medication administration if prescribed (technique, dosage, schedule)
Infection Prevention
- Hand hygiene before handling infant
- Limiting visitors, especially those with illness
- Proper cleaning of baby equipment
- Avoidance of crowded public spaces during high illness seasons
- Recognition of early signs of infection
- Importance of timely vaccinations (when age-appropriate)
Follow-up Care
- Importance of keeping scheduled appointments
- When to follow up with pediatrician after illness
- Documentation of temperatures and symptoms
- Communication with healthcare providers
- Understanding of medication completion importance
Educational Approaches and Tools
Teaching Methods
- Demonstration and return demonstration: Especially for temperature taking and medication administration
- Written materials: Clear, simple instructions with visual aids
- Video instruction: For visual learners
- Teach-back method: Ask parents to explain information in their own words
- Hands-on practice: With supervision before discharge
- Chunking information: Present in manageable segments
Addressing Barriers
- Language: Use interpreters or translated materials
- Literacy concerns: Provide pictorial instructions
- Anxiety: Allow time for questions and expression of concerns
- Cultural considerations: Respect cultural beliefs while ensuring safety
- Financial constraints: Provide information on assistance programs
- Support system: Identify key support persons who need education
Communication Technique: The FEVER Approach to Parent Education
- Facts: Provide accurate, evidence-based information
- Explain: Break down complex concepts into understandable terms
- Verify: Check understanding through teach-back method
- Encourage: Support parents’ confidence in caring for their infant
- Review: Summarize key points and provide written reinforcement
Parent Discharge Checklist for Newborn Fever
Before discharge, ensure parents can:
- Correctly demonstrate temperature measurement
- Identify normal temperature ranges
- Recognize signs requiring immediate medical attention
- Administer prescribed medications correctly
- Demonstrate proper handwashing technique
- Explain follow-up care plans
- Know emergency contact information
- Express understanding of prevention strategies
Mnemonics for Clinical Practice
Mnemonics can help nursing students remember important aspects of caring for newborns with fever. Here are several useful mnemonics specifically designed for this topic:
F.E.V.E.R. in Newborns
Assessment Framework for Febrile Newborns
F – Fluid status
- Assess hydration status
- Check number of wet diapers
- Evaluate mucous membranes
- Monitor fontanelle for depression
E – Examine thoroughly
- Complete head-to-toe assessment
- Check for rashes or skin changes
- Assess umbilical cord site
- Look for signs of localized infection
V – Vital signs monitoring
- Temperature (consistent method)
- Heart rate and respiratory rate
- Blood pressure if indicated
- Oxygen saturation
E – Energy and activity
- Assess level of consciousness
- Evaluate feeding behavior
- Observe muscle tone and movement
- Note irritability or lethargy
R – Risk factors evaluation
- Assess maternal history for risk factors
- Consider age-specific vulnerabilities
- Review birth history and complications
- Note exposure to illness or infections
N.E.O.N.A.T.E. with FEVER
Critical Interventions for Febrile Newborns
N – Notify provider immediately
E – Evaluate thoroughly and systematically
O – Obtain necessary specimens (blood, urine, CSF)
N – Nourish appropriately (IV or oral as indicated)
A – Administer antibiotics promptly if ordered
T – Temperature monitoring consistently
E – Educate parents thoroughly
R.I.S.K.S. for Neonatal Fever
Remember These Risk Factors for Neonatal Sepsis
R – Rupture of membranes, prolonged (>18 hours)
I – Infection, maternal (GBS, UTI, chorioamnionitis)
S – Systems immature (prematurity)
K – Knowledge deficit regarding warning signs
S – Sick contacts or sibling exposure
W.A.R.N. Parents
Teaching Parents When to Seek Care for Infant Fever
W – Warm temperature above 100.4°F (38°C)
A – Altered behavior (excessive crying, lethargy)
R – Reduced feeding (missing multiple feedings)
N – Not producing enough wet diapers (fewer than 4-6 daily)
Case Study
Case: 10-day-old Newborn with Fever
Patient Information
Patient: Baby Sofia, 10 days old, full-term vaginal delivery
Chief Complaint: Mother reports decreased feeding and irritability for past 6 hours. Home temperature was 101.2°F (38.4°C) rectally.
History: Unremarkable pregnancy. Mother GBS negative. Discharge from hospital at 48 hours of life. No known sick contacts.
Current Feeding: Exclusively breastfed, but has missed 2 feedings.
Initial Assessment
- Temperature: 101.5°F (38.6°C) rectally
- Heart Rate: 175 beats/minute
- Respiratory Rate: 68 breaths/minute
- Oxygen Saturation: 96% on room air
- Appearance: Irritable, consolable with difficulty
- Skin: Flushed, warm to touch, no rash
- Fontanelle: Soft, not bulging
- Umbilical cord site: Clean, no erythema
- Respiratory examination: Mild tachypnea, no retractions
Diagnostic Workup
- Complete Blood Count: WBC 18,000/μL with left shift
- C-reactive protein: 3.2 mg/dL (elevated)
- Blood Culture: Pending
- Urinalysis: 15-20 WBCs/HPF, positive leukocyte esterase
- Urine Culture: Pending
- Cerebrospinal Fluid: Pending (LP scheduled)
- Chest X-ray: No infiltrates, normal appearance
Working Diagnosis
Neonatal fever with suspected early sepsis, possible urinary tract infection
Management Plan
- Admit to pediatric unit
- Intravenous access for fluids and medications
- Empiric antibiotic therapy with ampicillin and gentamicin
- Continuous cardiorespiratory monitoring
- Temperature monitoring q2h
- I/O monitoring
- Support for breastfeeding or expressed breast milk
Nursing Care Plan
| Nursing Diagnosis | Interventions | Expected Outcomes |
|---|---|---|
| Hyperthermia related to infectious process |
|
Temperature returns to normal range within 48 hours |
| Risk for Deficient Fluid Volume related to fever and decreased oral intake |
|
Adequate hydration maintained as evidenced by moist mucous membranes, appropriate urine output, and stable weight |
| Anxiety (Parental) related to infant hospitalization |
|
Parents verbalize understanding of care and demonstrate decreased anxiety |
Hospital Course
Day 1-2: Sofia continued to have low-grade fever up to 100.8°F (38.2°C). IV antibiotics were administered as scheduled. Feeding improved gradually.
Day 3: Afebrile. Preliminary blood cultures negative. Urine culture grew >100,000 CFU/mL of E. coli. Antibiotics narrowed to cefotaxime based on sensitivities.
Day 7: Completed 7-day course of antibiotics. Feeding well, afebrile for 5 days, clinically stable.
Discharge Planning and Education
- Follow-up appointment with pediatrician in 48 hours
- Instructions on temperature monitoring
- Education on UTI prevention
- Warning signs requiring immediate return
- Support for continued breastfeeding
Case Analysis: This case demonstrates the standard approach to managing fever in a newborn under 28 days old, including complete septic workup, empiric antibiotics, and hospitalization. The case highlights the importance of prompt intervention, support for the family unit, and comprehensive discharge planning.
Global Best Practices
Different regions have developed various approaches to managing fever in newborns. Understanding these global perspectives can enrich nursing practice.
International Approaches to Neonatal Fever Management
North American Practice (AAP Guidelines)
- Full septic workup (blood, urine, CSF) for all febrile infants 0-28 days
- Hospitalization and empiric antibiotics for all febrile neonates
- Risk stratification approach for infants 29-60 days based on clinical and laboratory criteria
- Increased use of biomarkers (procalcitonin, CRP) in decision-making
- Focus on minimizing unnecessary lumbar punctures in well-appearing older infants
European Approach (NICE Guidelines)
- Traffic light system for risk assessment (red/amber/green)
- Greater emphasis on clinical appearance in management decisions
- More selective use of lumbar puncture in well-appearing infants
- Earlier transition to oral antibiotics when clinically appropriate
- Focus on reducing hospital length of stay when possible
Kangaroo Mother Care Approach (WHO)
- Emphasis on skin-to-skin contact even during illness when stable
- Integration of maternal involvement in hospital care
- Recognition of benefits of breastfeeding for immune protection
- Focus on thermal regulation through maternal contact
- Particularly valuable in resource-limited settings
Resource-Limited Setting Adaptations
- Simplified diagnostic algorithms when laboratory testing is limited
- Greater reliance on clinical assessment
- Community health worker involvement in early detection
- Focus on essential interventions when resources are scarce
- Adaptation of care processes to local capabilities
Emerging Practice Trends
Technological Innovations
- Continuous temperature monitoring systems
- Point-of-care testing for rapid diagnosis
- Telehealth monitoring for select cases after discharge
- Electronic clinical decision support systems
- Mobile applications for parent education and monitoring
Evolving Care Models
- Step-down units for febrile infants after initial stabilization
- Enhanced observation units without full hospitalization
- Early discharge protocols for select low-risk cases
- Greater family involvement in hospital care
- Multidisciplinary team approaches to complex cases
Practice Integration: While global practices vary, core principles remain consistent: rapid recognition, thorough assessment, timely intervention, and appropriate monitoring. Nurses should adapt these principles to their local guidelines while incorporating supportive care practices from various approaches.
References
- American Academy of Pediatrics. (2021). Evaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old. Pediatrics, 148(2), e2021052228. https://publications.aap.org/pediatrics/article/148/2/e2021052228/179783/Evaluation-and-Management-of-Well-Appearing
- Cleveland Clinic. (2024). Sepsis in Newborns (Neonatal Sepsis). https://my.clevelandclinic.org/health/diseases/15371-sepsis-in-newborns
- Medline Plus. (2023). When your baby or infant has a fever. https://medlineplus.gov/ency/patientinstructions/000319.htm
- National Center for Biotechnology Information. (2022). Fever in a Neonate. In: StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482196/
- National Center for Biotechnology Information. (2022). Neonatal Sepsis. In: StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK531478/
- Nationwide Children’s Hospital. (2024). Fever in a Newborn Baby. https://www.nationwidechildrens.org/conditions/health-library/fever-in-a-newborn-baby
- Nurseslabs. (2024). Fever (Pyrexia) Nursing Diagnosis & Care Plan. https://nurseslabs.com/fever-pyrexia-nursing-care-plans/
- Nursing Times. (2006). Managing infants with pyrexia. https://www.nursingtimes.net/archive/managing-infants-with-pyrexia-29-09-2006/
- Nurse.com. (2024). Fever: Nursing Diagnosis & Interventions. https://www.nurse.com/clinical-guides/fever/
- Royal Children’s Hospital Melbourne. (2024). Nursing guidelines: Temperature management. https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Temperature_management/
These educational notes are designed for nursing students as a learning resource. Always consult current hospital protocols and healthcare provider instructions when caring for patients.
© 2025 Nursing Educational Resources. Last updated: June 2025.
