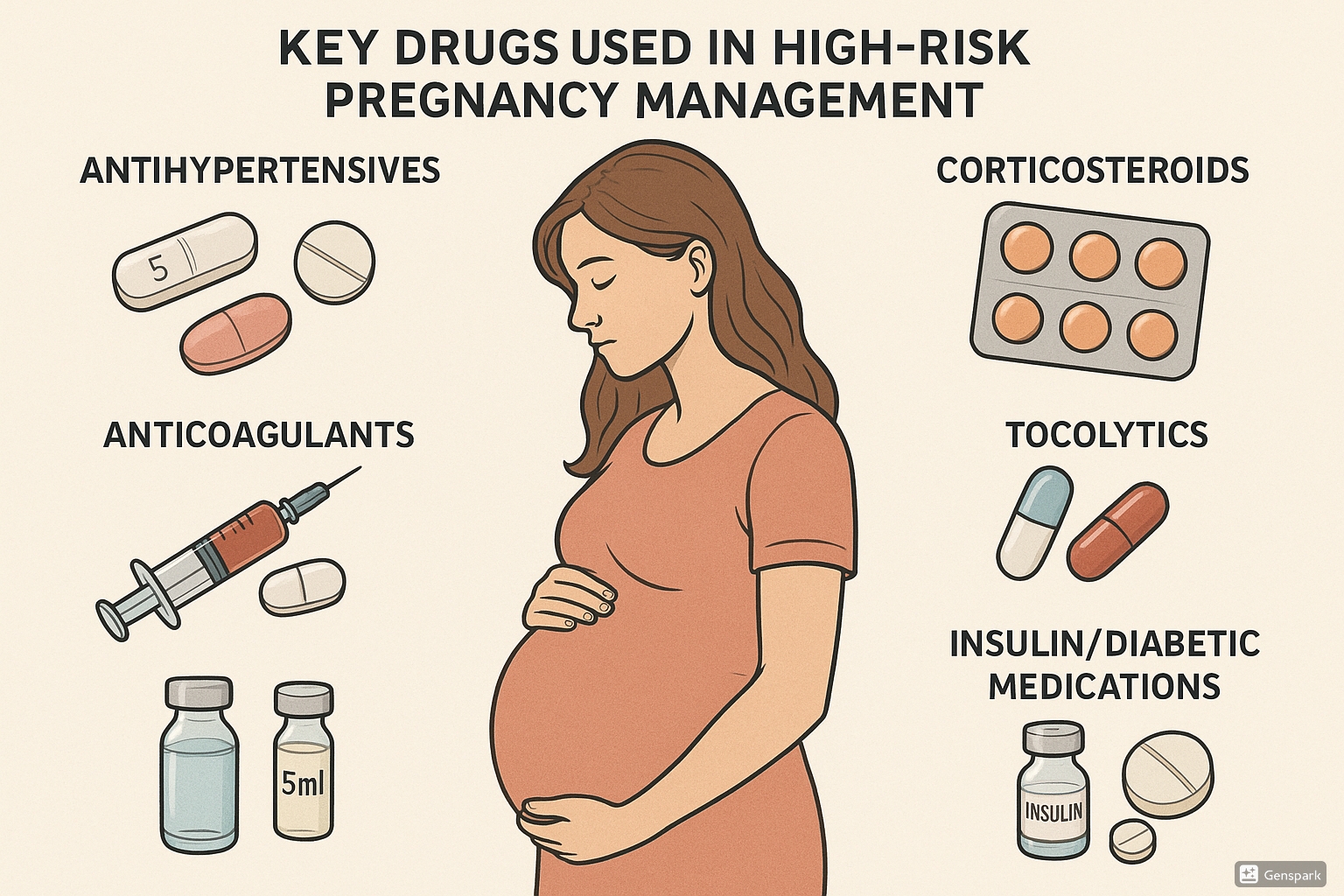
Drugs Used in Management of High-Risk Pregnancies
Comprehensive Guide for Nursing Students
Table of Contents
- Introduction to High-Risk Pregnancies
- Antihypertensive Medications
- Anticoagulants
- Corticosteroids for Fetal Lung Maturity
- Tocolytics
- Medications for Gestational Diabetes
- Progesterone for Preterm Birth Prevention
- Magnesium Sulfate
- Low-Dose Aspirin for Preeclampsia Prevention
- Thyroid Medications
- Special Considerations and Monitoring
- Best Practices in Medication Management
- References
Introduction to High-Risk Pregnancies
A high-risk pregnancy is one that threatens the health or life of the mother or her fetus. Various factors can contribute to a pregnancy being classified as high-risk, including pre-existing maternal conditions, pregnancy complications, or fetal abnormalities. Careful pharmacological management is essential to ensure optimal outcomes for both mother and baby.
High-risk pregnancy medications are specialized pharmacological agents used to manage complications that could endanger maternal and fetal health. The judicious use of these medications requires a thorough understanding of their mechanisms, benefits, risks, and appropriate monitoring protocols.
Various conditions requiring pharmacological intervention in high-risk pregnancies include:
- Hypertensive disorders (pre-eclampsia, chronic hypertension, gestational hypertension)
- Thromboembolic disorders
- Preterm labor
- Gestational diabetes
- Thyroid dysfunction
- Risk of fetal lung immaturity
This comprehensive guide explores the major drug categories used in managing high-risk pregnancies, including their mechanisms of action, dosing considerations, safety profiles, and nursing implications.
Key Principles of High-Risk Pregnancy Medication Management:
- Risk-benefit assessment is essential before initiating any medication
- Dosages often differ from non-pregnant patients
- Physiological changes of pregnancy alter drug pharmacokinetics
- Potential impacts on fetal development must always be considered
- Regular monitoring is crucial for dose adjustments
Antihypertensive Medications
Overview & Classification
Hypertensive disorders affect 5-10% of pregnancies and are a leading cause of maternal and fetal morbidity and mortality. Antihypertensive medications are used to control blood pressure and prevent complications such as stroke, placental abruption, and fetal growth restriction.
The goal of antihypertensive therapy in pregnancy is to reduce the risk of severe maternal hypertension without compromising uteroplacental perfusion or causing adverse fetal effects.
| Category | Examples | Safety in Pregnancy | Primary Use |
|---|---|---|---|
| Centrally Acting Alpha-Agonists | Methyldopa | First-line (Category B) | Chronic hypertension |
| Beta-Blockers | Labetalol | First-line (Category C) | Chronic and acute hypertension |
| Calcium Channel Blockers | Nifedipine | First-line (Category C) | Chronic and acute hypertension |
| Direct Vasodilators | Hydralazine | Second-line (Category C) | Acute severe hypertension |
| Diuretics | Hydrochlorothiazide | Use with caution (Category B) | Chronic hypertension (if already on therapy) |
| ACE Inhibitors/ARBs | Lisinopril, Losartan | Contraindicated (Category D/X) | Not used in pregnancy |
First-Line Agents
1. Methyldopa
Mechanism of Action: Centrally acting alpha-2 adrenergic agonist that reduces sympathetic outflow from the central nervous system.
Dosage: 250-500 mg orally 2-3 times daily; maximum 3g/day
Efficacy: Moderate antihypertensive effect with excellent long-term safety data in pregnancy
Side Effects: Sedation, depression, orthostatic hypotension, hepatic dysfunction (rare)
Nursing Considerations:
- Monitor liver function tests during prolonged therapy
- Assess for excessive sedation that may interfere with activities
- Alert patient that urine may darken upon standing
2. Labetalol
Mechanism of Action: Combined alpha and beta-adrenergic receptor blocker with greater effect on beta receptors than alpha receptors.
Dosage:
- Oral: 100-400 mg twice daily; maximum 2400 mg/day
- IV (for severe hypertension): 10-20 mg IV, then 20-80 mg every 10-30 minutes; maximum 300 mg total
Efficacy: Effectively lowers blood pressure without significantly reducing cardiac output or uterine blood flow
Side Effects: Bradycardia, bronchospasm, dizziness, scalp tingling
Nursing Considerations:
- Monitor maternal heart rate and blood pressure
- Contraindicated in patients with asthma, heart block, or heart failure
- Position patient in left lateral position for IV administration
3. Nifedipine
Mechanism of Action: Calcium channel blocker that decreases peripheral vascular resistance.
Dosage: Extended-release 30-60 mg once daily; maximum 120 mg/day
Efficacy: Rapidly effective for acute blood pressure control
Side Effects: Headache, flushing, peripheral edema, tachycardia
Nursing Considerations:
- The immediate-release (sublingual) form should be avoided due to risk of precipitous hypotension
- Should not be administered with magnesium sulfate due to potential for hypotension
- Monitor for significant hypotension
IMPORTANT:
Immediate-release nifedipine should NOT be administered sublingually in pregnant women due to the risk of precipitous hypotension, which can compromise uteroplacental perfusion.
Second-Line and Acute Treatment Agents
1. Hydralazine
Mechanism of Action: Direct vasodilator that acts primarily on arterial smooth muscle.
Dosage: 5-10 mg IV every 20-40 minutes; maximum 20 mg per dose or 30 mg total
Efficacy: Effective for acute management of severe hypertension
Side Effects: Tachycardia, headache, flushing, lupus-like syndrome with prolonged use
Nursing Considerations:
- Administer slowly over 2 minutes
- Monitor blood pressure every 5 minutes for 30 minutes after administration
- May cause reflex tachycardia; monitor maternal heart rate
2. Diuretics
Mechanism of Action: Increase sodium and water excretion, reducing plasma and extracellular fluid volume.
Usage in Pregnancy: Generally avoided as first-line therapy due to potential for reduced placental perfusion; may be continued if patient was on therapy prior to pregnancy.
Side Effects: Electrolyte disturbances, volume depletion, hyperglycemia
Nursing Considerations:
- Monitor electrolytes, especially potassium
- Assess for signs of dehydration
- May be particularly useful in women with pulmonary edema
Contraindicated Antihypertensive Medications
1. ACE Inhibitors and ARBs
ACE inhibitors (e.g., lisinopril, enalapril) and Angiotensin II Receptor Blockers (e.g., losartan, valsartan) are contraindicated throughout pregnancy.
Potential Adverse Effects:
- First trimester: Potential increased risk of congenital malformations
- Second and third trimesters: Fetal renal dysfunction, oligohydramnios, pulmonary hypoplasia, growth restriction, skull hypoplasia, and fetal or neonatal death
Women who become pregnant while taking ACE inhibitors or ARBs should be switched to alternative antihypertensive medications as soon as possible.
2. Atenolol
While other beta-blockers may be used, atenolol has been associated with fetal growth restriction and should be avoided.
MNEMONIC: “SAFE BP in Pregnancy”
S – Select medications with proven safety (Methyldopa, Labetalol)
A – Avoid ACE inhibitors and ARBs
F – Fetal wellbeing monitoring is essential
E – Establish target BP <150/100 mmHg
B – Begin with lowest effective dose
P – Prevent severe hypertension to reduce complications
Anticoagulants
Overview & Indications
Pregnant women face an increased risk of venous thromboembolism (VTE) due to physiological changes including hypercoagulability, venous stasis, and vascular damage. Anticoagulants are used for both treatment of VTE and thromboprophylaxis in high-risk pregnancies.
Key Indications for Anticoagulant Use in High-Risk Pregnancies:
- History of previous VTE
- Inherited thrombophilias (e.g., Factor V Leiden, Protein C or S deficiency)
- Antiphospholipid syndrome
- Mechanical heart valves
- Atrial fibrillation
- Immobility
- Post-cesarean thromboprophylaxis in high-risk women
The physiological changes of pregnancy affect the pharmacokinetics of anticoagulants, necessitating dose adjustments and careful monitoring throughout pregnancy.
Low Molecular Weight Heparins (LMWH)
Examples: Enoxaparin (Lovenox), Dalteparin (Fragmin)
Mechanism of Action: Enhances antithrombin activity, primarily inhibiting factor Xa and, to a lesser extent, factor IIa (thrombin).
Advantages:
- Does not cross the placenta
- Predictable dose response
- Lower risk of heparin-induced thrombocytopenia (HIT)
- Lower risk of osteoporosis with prolonged use
- Once-daily or twice-daily dosing
- Less need for monitoring compared to unfractionated heparin
Dosage:
| Indication | Enoxaparin | Dalteparin |
|---|---|---|
| Prophylaxis | 40 mg SC once daily | 5,000 units SC once daily |
| Treatment | 1 mg/kg SC twice daily or 1.5 mg/kg once daily | 100 units/kg SC twice daily or 200 units/kg once daily |
| Mechanical heart valve | 1 mg/kg SC twice daily with anti-Xa monitoring | 100 units/kg SC twice daily with anti-Xa monitoring |
Monitoring: Anti-Xa levels (4-6 hours post-dose) may be measured for therapeutic dosing or in certain situations (renal impairment, extremes of body weight, mechanical heart valves).
Side Effects: Bleeding, injection site reactions, rare HIT, osteoporosis with prolonged use
Nursing Considerations:
- Teach proper injection technique for self-administration
- Monitor platelet count periodically
- Assess for signs of bleeding
- Should be discontinued 24 hours before planned induction or cesarean section
- Cannot be reversed quickly with protamine sulfate (only partially effective)
Unfractionated Heparin (UFH)
Mechanism of Action: Binds to antithrombin, enhancing its inhibitory effects on thrombin (factor IIa) and factor Xa.
Advantages:
- Does not cross the placenta
- Shorter half-life (1-2 hours) than LMWH
- Can be fully reversed with protamine sulfate
- May be preferred in women with renal impairment
- May be preferred peripartum due to shorter half-life
Dosage:
| Indication | Dosage | Monitoring Target |
|---|---|---|
| Prophylaxis | 5,000-10,000 units SC every 12 hours | Not typically monitored |
| Treatment | Initial: 80 units/kg bolus, then 18 units/kg/hr continuous infusion | aPTT 1.5-2.5 × control |
| Adjusted-dose prophylaxis | Starting with 5,000-10,000 units SC every 12 hours | Mid-interval (6 hours post-dose) aPTT of 1.5-2.5 × control |
Side Effects: Bleeding, HIT (more common than with LMWH), osteoporosis with prolonged use
Nursing Considerations:
- Monitor aPTT regularly for therapeutic dosing
- Check platelet count regularly (HIT risk)
- Teach proper injection technique for self-administration
- Assess for signs of bleeding
- Can be discontinued 4-6 hours before planned delivery
Warfarin and Direct Oral Anticoagulants (DOACs)
Warfarin
Mechanism of Action: Vitamin K antagonist that inhibits the synthesis of clotting factors II, VII, IX, and X.
Safety in Pregnancy: Generally contraindicated due to teratogenicity and fetal bleeding risk, but may be considered in specific situations (e.g., mechanical heart valves) during the second and early third trimesters.
Potential Adverse Effects:
- First trimester: Warfarin embryopathy (nasal hypoplasia, stippled epiphyses)
- Any trimester: Fetal intracranial hemorrhage, stillbirth, CNS abnormalities
Warfarin should be avoided during pregnancy except in specific cases where the benefits clearly outweigh risks (such as certain mechanical heart valves where LMWH may be insufficient).
Direct Oral Anticoagulants (DOACs)
Examples: Apixaban, Rivaroxaban, Dabigatran, Edoxaban
Safety in Pregnancy: Contraindicated due to limited data on safety and evidence of placental transfer.
Recommendation: Women on DOACs who become pregnant should be switched to LMWH as soon as possible.
Peripartum Management of Anticoagulation
Careful planning is required for anticoagulant management around delivery to balance the risk of thrombosis and hemorrhage.
General Recommendations:
| Anticoagulant | Timing of Discontinuation Before Delivery | Timing of Resumption After Delivery |
|---|---|---|
| Prophylactic LMWH | 24 hours before planned delivery or induction | 12-24 hours after delivery if hemostasis is adequate |
| Therapeutic LMWH | 24-36 hours before planned delivery | 24 hours after delivery if hemostasis is adequate |
| Prophylactic UFH | 12 hours before planned delivery | 6-12 hours after delivery if hemostasis is adequate |
| Therapeutic IV UFH | 4-6 hours before planned delivery | 6-12 hours after delivery if hemostasis is adequate |
| Warfarin | Transition to LMWH/UFH at 36 weeks or earlier | Can be resumed day after delivery if good hemostasis |
Neuraxial anesthesia (epidural/spinal) is generally contraindicated within 12 hours of prophylactic LMWH and 24 hours of therapeutic LMWH doses.
MNEMONIC: “CLOTS in Pregnancy”
C – Choose LMWH as first-line (Crosses placenta? No!)
L – Look for mechanical valve (special considerations)
O – Omit dose 24h before delivery (for LMWH)
T – Teach self-injection technique
S – Screen for bleeding risks regularly
Corticosteroids for Fetal Lung Maturity
Overview & Mechanism
Antenatal corticosteroids are administered to accelerate fetal lung maturity in women at risk of preterm delivery. They significantly reduce neonatal mortality, respiratory distress syndrome (RDS), intraventricular hemorrhage, and necrotizing enterocolitis.
Mechanism of Action: Corticosteroids promote the production of surfactant proteins and enzymes necessary for surfactant synthesis, induce structural maturation of the lungs, and enhance lung compliance and gas exchange.
A single course of antenatal corticosteroids should be administered to women between 24+0 and 33+6 weeks of gestation who are at risk of preterm delivery within 7 days.
Indications:
- Preterm labor
- Preterm premature rupture of membranes
- Antepartum hemorrhage
- Hypertensive disorders requiring preterm delivery
- Fetal growth restriction requiring preterm delivery
- Other conditions necessitating preterm delivery
Types of Corticosteroids
Two corticosteroids are commonly used for antenatal lung maturation:
| Parameter | Betamethasone | Dexamethasone |
|---|---|---|
| Standard Dosing Regimen | Two doses of 12 mg IM given 24 hours apart | Four doses of 6 mg IM given every 12 hours |
| Half-Life | Longer (36-54 hours) | Shorter (16-36 hours) |
| Placental Transfer | Less metabolized by placenta | More metabolized by placenta |
| Onset of Action | 24 hours | 24 hours |
| Peak Effect | 48 hours – 7 days | 48 hours – 7 days |
| Duration of Benefit | Up to 7 days | Up to 7 days |
Comparative Efficacy: Both betamethasone and dexamethasone are effective in reducing neonatal RDS and mortality. Some studies suggest betamethasone may be slightly more effective in reducing periventricular leukomalacia and infant mortality, but both are considered appropriate choices.
Timing and Administration
Optimal Timing: Maximum benefit occurs when corticosteroids are administered at least 24 hours and less than 7 days before delivery.
Administration Considerations:
- Complete course when possible, but even incomplete courses provide benefit
- Administer deep IM injection, usually in the gluteal muscle
- Store according to manufacturer’s recommendations (some preparations require refrigeration)
Special Timing Considerations:
- 24 hours before delivery: Significant reduction in RDS begins
- 48 hours after completion: Maximum effectiveness achieved
- 7 days after administration: Benefits begin to wane
Special Scenarios
1. Repeat Courses
While a single rescue course may be considered if the initial course was administered more than 7 days previously and gestational age is <34 weeks with imminent delivery risk, routine multiple courses are not recommended due to concerns about reduced fetal growth, reduced head circumference, and potential neurodevelopmental issues.
2. Late Preterm Corticosteroids
Evidence supports considering corticosteroids for women at risk of preterm birth between 34+0 and 36+6 weeks if they have not previously received a course of antenatal corticosteroids. Betamethasone is preferred in this situation.
3. Multiple Gestations
The same dosage regimen is used for multiple gestations as for singletons. There is no need to increase the dose.
Maternal Side Effects and Contraindications
Maternal Side Effects:
- Transient hyperglycemia (especially in diabetic patients)
- Leukocytosis
- Increased susceptibility to infection
- Injection site pain
Contraindications:
- Systemic maternal infection where delivery is indicated
- Chorioamnionitis (relative contraindication)
In women with diabetes, blood glucose levels should be closely monitored for 24-48 hours after corticosteroid administration, and insulin dosages may need to be adjusted.
Nursing Implications
Key Nursing Responsibilities:
- Verify correct timing and dosage before administration
- Educate patients about the purpose, benefits, and potential side effects
- Document timing of each dose accurately
- Monitor maternal blood glucose in women with diabetes
- Monitor for signs of infection
- Coordinate timing with other interventions (e.g., tocolytics, magnesium sulfate)
MNEMONIC: “STEROIDS for Lungs”
S – Schedule two doses of betamethasone or four of dexamethasone
T – Time critical: 24h before birth for benefits to begin
E – Effect lasts up to 7 days
R – Respiratory distress syndrome prevention is primary goal
O – Optimal gestational age: 24-34 weeks
I – Injection must be intramuscular
D – Diabetes? Monitor blood glucose closely
S – Single course is standard (repeat courses limited)
Tocolytics
Overview & Role
Tocolytics are medications used to inhibit uterine contractions and delay preterm birth. The primary goals of tocolytic therapy are to:
- Delay delivery for 48 hours to allow for corticosteroid administration for fetal lung maturity
- Allow in utero transfer to a facility with appropriate neonatal care capabilities
- Potentially prolong pregnancy to improve neonatal outcomes
Tocolytics typically delay delivery by 2-7 days but do not consistently improve long-term neonatal outcomes. Their main benefit is providing time for corticosteroid administration.
Indications for Tocolysis:
- Regular uterine contractions
- Cervical change or cervical length <25mm
- Gestational age 24-34 weeks (some protocols extend to 37 weeks)
Contraindications to Tocolysis:
- Maternal contraindications: Severe preeclampsia/eclampsia, active vaginal bleeding, cardiac disease
- Fetal contraindications: Lethal fetal anomaly, chorioamnionitis, evidence of fetal compromise, fetal demise, mature fetal lung studies
- Obstetric contraindications: Placental abruption, intrauterine infection, advanced cervical dilation (>5 cm)
Types of Tocolytics
Several classes of medications are used as tocolytics, each with a unique mechanism of action, efficacy profile, and side effect concerns:
| Class | Mechanism | Examples | Efficacy | Key Concerns |
|---|---|---|---|---|
| Calcium Channel Blockers | Block calcium influx into myometrial cells | Nifedipine | Good, first-line in many centers | Hypotension, headache |
| NSAIDs/COX Inhibitors | Inhibit prostaglandin synthesis | Indomethacin | Moderate to good | Premature closure of ductus arteriosus, oligohydramnios |
| Beta-adrenergic Agonists | Stimulate β2 receptors in myometrium | Terbutaline | Moderate | Maternal cardiac effects, pulmonary edema |
| Oxytocin Antagonists | Block oxytocin receptors | Atosiban | Moderate | Limited availability in US, cost |
| Magnesium Sulfate | Decreases intracellular calcium | Magnesium Sulfate | Limited/controversial | Toxicity concerns at higher doses |
Calcium Channel Blockers
Primary Agent: Nifedipine
Mechanism of Action: Blocks calcium influx through cell membranes, decreasing intracellular calcium concentration and reducing myometrial contractility.
Dosing Protocol:
- Loading dose: 10-20 mg orally, may repeat in 20-30 minutes if contractions persist (maximum 40 mg in first hour)
- Maintenance: 10-20 mg orally every 4-6 hours for 48-72 hours
Efficacy: Shown to be more effective than beta-mimetics with fewer side effects. Associated with decreased risk of respiratory distress syndrome, necrotizing enterocolitis, and intraventricular hemorrhage.
Side Effects:
- Maternal: Hypotension, headache, dizziness, flushing, nausea
- Fetal: Generally considered safe, minimal fetal effects
Contraindications:
- Hypersensitivity to nifedipine
- Hypotension (systolic BP <90 mmHg)
- Hepatic dysfunction
- Use caution with concurrent magnesium sulfate (risk of hypotension)
Nursing Considerations:
- Monitor blood pressure before administration and 15-30 minutes after each dose
- Observe for signs of hypotension
- Use with caution in women with diabetes (may affect glucose control)
- Do not administer sublingually due to risk of precipitous hypotension
The immediate-release (sublingual) nifedipine should NOT be used due to risk of precipitous hypotension. Only oral capsules or extended-release tablets should be used for tocolysis.
NSAIDs/COX Inhibitors
Primary Agent: Indomethacin
Mechanism of Action: Inhibits cyclooxygenase enzyme, reducing prostaglandin synthesis, which is essential for uterine contractions.
Dosing Protocol:
- Loading dose: 50-100 mg orally or rectally
- Maintenance: 25 mg orally every 4-6 hours for up to 48 hours
Efficacy: Effective short-term tocolytic with comparable efficacy to other agents.
Side Effects:
- Maternal: Nausea, heartburn, gastritis, platelet dysfunction
- Fetal: Premature constriction/closure of the ductus arteriosus, oligohydramnios, necrotizing enterocolitis, intraventricular hemorrhage
Restrictions on Use:
- Limited to pregnancies <32 weeks gestation due to risk of premature ductal closure
- Duration should not exceed 48-72 hours
- Fetal echocardiography should be considered for treatment exceeding 48 hours
Contraindications:
- Gestational age >32 weeks
- Renal or hepatic dysfunction
- Active peptic ulcer disease
- Platelet dysfunction or bleeding disorder
- Oligohydramnios
- Known ductal constriction
Nursing Considerations:
- Monitor amniotic fluid volume
- Educate patient about GI side effects and provide prophylaxis if needed
- Monitor for maternal oliguria
- Consider fetal echocardiography for prolonged therapy
Beta-adrenergic Agonists
Primary Agent: Terbutaline
Mechanism of Action: Stimulates β2-adrenergic receptors in the myometrium, leading to decreased intracellular calcium and myometrial relaxation.
Dosing Protocol:
- Acute: 0.25 mg subcutaneously every 20-30 minutes for up to 4 doses
- IV: 2.5-10 μg/min, titrated to uterine quiescence (rarely used now)
Efficacy: Effective in delaying delivery for 48 hours but with significant maternal side effects.
Side Effects:
- Maternal: Tachycardia, palpitations, tremor, headache, nausea, vomiting, hyperglycemia, hypokalemia, pulmonary edema (rare but serious)
- Fetal: Tachycardia, hyperinsulinemia, hyperglycemia
Contraindications:
- Cardiac disease
- Poorly controlled diabetes
- Hyperthyroidism
- Uncontrolled hypertension
- Use with caution in multiple gestations (increased risk of pulmonary edema)
Nursing Considerations:
- Monitor vital signs (especially pulse and respiratory rate)
- Maintain strict fluid balance
- Monitor for signs of pulmonary edema (dyspnea, tachypnea, crackles)
- Monitor electrolytes and blood glucose
- Limit fluid intake to reduce risk of pulmonary edema
The FDA has warned against the use of terbutaline for prevention of preterm labor beyond 48-72 hours due to risks of serious maternal cardiac effects and death. Maintenance therapy should be avoided.
Other Tocolytics
1. Oxytocin Antagonists (Atosiban)
Mechanism: Competitively inhibits oxytocin receptors in the myometrium, preventing oxytocin-induced contractions.
Status: Approved in Europe but not available in the United States.
Advantages: Fewer cardiovascular side effects than beta-mimetics.
2. Magnesium Sulfate as Tocolytic
Mechanism: Competes with calcium at the cellular level, leading to decreased intracellular calcium and reduced myometrial contractility.
Dosing for Tocolysis:
- Loading: 4-6 g IV over 20-30 minutes
- Maintenance: 2-3 g/hour IV
Efficacy: Limited evidence supports its efficacy as a tocolytic; some studies suggest it is no more effective than placebo. Currently not recommended as a first-line tocolytic.
Side Effects: Similar to those described in magnesium sulfate section.
Combination Tocolytic Therapy
Combining tocolytics from different classes has been studied as a potential strategy to improve efficacy or reduce individual drug dosages.
Current Evidence:
- Limited data showing improved efficacy over single-agent therapy
- Increased risk of maternal adverse effects
- Generally not recommended in routine practice
Combination tocolytic therapy should only be considered in specific cases by experienced practitioners with careful monitoring due to increased risk of adverse effects.
MNEMONIC: “STOP Preterm Labor”
S – Select appropriate tocolytic based on gestational age & contraindications
T – Time tocolysis to allow corticosteroid effect (48 hours)
O – Observe closely for maternal side effects
P – Prevent recurrence by identifying and treating underlying causes
Medications for Gestational Diabetes
Overview & Approach
Gestational diabetes mellitus (GDM) affects 2-10% of pregnancies and is associated with increased risks of macrosomia, birth trauma, neonatal hypoglycemia, and maternal hypertensive disorders. Appropriate glycemic control is essential to reduce these risks.
Treatment Approach:
- First-line: Lifestyle modifications (dietary changes, physical activity)
- Second-line: Pharmacological therapy when glycemic targets not achieved with lifestyle changes
Glycemic Targets in Pregnancy:
| Time of Day | Target Blood Glucose |
|---|---|
| Fasting | ≤95 mg/dL (5.3 mmol/L) |
| 1-hour postprandial | ≤140 mg/dL (7.8 mmol/L) |
| 2-hour postprandial | ≤120 mg/dL (6.7 mmol/L) |
Pharmacologic therapy for GDM is typically initiated when target glucose levels are not achieved after 1-2 weeks of lifestyle modifications or immediately in cases of significantly elevated glucose values.
Insulin Therapy
Insulin remains the gold standard treatment for gestational diabetes when diet and exercise fail to maintain adequate glycemic control. It does not cross the placenta and has no known teratogenic effects.
Types of Insulin Used in Pregnancy:
| Insulin Type | Onset | Peak | Duration | Primary Use in GDM |
|---|---|---|---|---|
| Rapid-acting (Lispro, Aspart) | 10-15 min | 1-2 hours | 3-5 hours | Mealtime coverage |
| Short-acting (Regular) | 30-60 min | 2-4 hours | 6-8 hours | Mealtime coverage |
| Intermediate-acting (NPH) | 1-2 hours | 4-8 hours | 12-18 hours | Basal coverage |
| Long-acting (Detemir)* | 1-2 hours | Minimal | 20-24 hours | Basal coverage |
*Insulin detemir is FDA pregnancy category B; glargine has less data but is increasingly used.
Insulin Regimens:
- Starting Dosage: 0.7-1.0 units/kg/day total daily dose in divided doses
- Distribution:
- 50% as basal insulin (NPH or detemir)
- 50% as prandial insulin (rapid or short-acting)
- Adjustments: Based on blood glucose patterns, typically increased throughout pregnancy due to progressive insulin resistance
Common Regimens:
- Single injection: For fasting hyperglycemia only – bedtime intermediate-acting insulin
- Multiple daily injections: Basal-bolus regimen with NPH at bedtime and rapid-acting before meals
- Intensive therapy: Basal insulin (1-2 times daily) plus prandial insulin with each meal
Side Effects:
- Hypoglycemia (most significant risk)
- Weight gain
- Injection site reactions
Nursing Considerations:
- Educate on proper injection technique and storage
- Teach hypoglycemia recognition and management
- Emphasize importance of regular blood glucose monitoring
- Provide guidance on insulin dosage adjustments based on patterns
- Coordinate with dietary education
Oral Hypoglycemic Agents
1. Metformin
Mechanism of Action: Decreases hepatic glucose production and increases peripheral glucose uptake.
Dosage: Initial 500 mg once or twice daily, increased gradually to maximum of 2000-2500 mg daily in divided doses.
Efficacy: Multiple studies including the MiG trial (Metformin in Gestational Diabetes) have demonstrated efficacy comparable to insulin for glycemic control. Benefits include:
- Less maternal weight gain
- Lower rates of maternal hypoglycemia
- Potential reduction in gestational hypertension and preeclampsia
Limitations:
- Approximately 30-40% of women require supplemental insulin
- Crosses placenta (concentration in fetal circulation approaches maternal levels)
Side Effects: Gastrointestinal disturbances (nausea, diarrhea, bloating), vitamin B12 deficiency with long-term use
Long-term Effects: Follow-up studies of children exposed to metformin in utero suggest no adverse effects on growth, motor, or social development. Some studies show potential benefits in reducing childhood obesity.
Metformin is increasingly accepted as a safe alternative to insulin therapy in GDM, particularly for women who refuse or cannot use insulin.
2. Glyburide (Glibenclamide)
Mechanism of Action: Sulfonylurea that stimulates pancreatic insulin secretion.
Dosage: Initial 2.5 mg once or twice daily, increased as needed to maximum 20 mg daily.
Efficacy: Studies show varying degrees of efficacy compared to insulin, with some suggesting:
- Higher rates of maternal hypoglycemia compared to insulin or metformin
- Higher rates of neonatal hypoglycemia
- Greater maternal weight gain compared to metformin
- Higher rates of treatment failure than previously thought (up to 20-30%)
Placental Transfer: Initially thought to have minimal placental transfer, newer data suggest significant transfer (up to 70% of maternal concentrations).
Side Effects: Hypoglycemia, weight gain, allergic skin reactions
Recent studies suggest increased rates of neonatal hypoglycemia, macrosomia, and neonatal adiposity with glyburide compared to insulin. ACOG now recommends insulin or metformin over glyburide when medication is needed for GDM.
3. Other Oral Agents
Other classes of oral hypoglycemic agents (DPP-4 inhibitors, GLP-1 receptor agonists, SGLT2 inhibitors) have limited data on safety in pregnancy and are not recommended.
Comparative Efficacy and Clinical Decision-Making
Factors Influencing Medication Choice:
- Severity of hyperglycemia
- Patient preferences (injection vs. oral medication)
- Risk factors (obesity, previous macrosomia)
- Patient reliability/compliance
- Resource availability (ability to monitor glucose, cost)
Current Recommendations (Based on Evidence):
- First choice: Insulin (especially for more severe hyperglycemia)
- Acceptable alternative: Metformin (with patient counseling about potential need for supplemental insulin)
- Less preferred: Glyburide (due to concerns about increased adverse neonatal outcomes)
Special Considerations:
- Pre-existing conditions (e.g., PCOS may respond well to metformin)
- Obesity (metformin may have advantages due to less weight gain)
- Patient adherence issues (oral medications may improve compliance)
- Risk of hypoglycemia (metformin has lower risk than insulin or glyburide)
- Gestational age at initiation of therapy
Nursing Implications and Patient Education
Key Nursing Responsibilities:
- Teach blood glucose monitoring technique and target ranges
- Educate about medication administration (injection technique for insulin)
- Provide dietary counseling in coordination with dietitian
- Educate about symptoms and management of hypoglycemia
- Encourage appropriate physical activity
- Monitor for signs of complications
- Educate about the importance of postpartum diabetes screening
Essential Patient Education Points:
- Timing and frequency of blood glucose monitoring
- Medication dosage, schedule, and adjustment protocols
- Recognition and treatment of hypoglycemia
- Dietary principles for GDM management
- When to contact healthcare provider (persistent hyperglycemia, hypoglycemic episodes)
- Importance of keeping all prenatal appointments
- Signs and symptoms of complications that require immediate attention
MNEMONIC: “SUGAR Control”
S – Schedule regular glucose monitoring
U – Understand medication mechanism (insulin vs. oral agents)
G – Gradual dose titration based on glucose patterns
A – Avoid hypoglycemia (teach recognition and management)
R – Regular prenatal care is essential
Progesterone for Preterm Birth Prevention
Overview & Mechanism
Progesterone is a hormone essential for the maintenance of pregnancy. Its use in preventing preterm birth is based on its effects in maintaining uterine quiescence through various mechanisms.
Mechanisms of Action in Preventing Preterm Birth:
- Decreases production of prostaglandins that stimulate uterine contractions
- Inhibits the formation of gap junctions between myometrial cells
- Reduces the number of oxytocin receptors in the myometrium
- May have anti-inflammatory properties that reduce infection-associated preterm birth
- Maintains cervical integrity and decreases responsiveness to protease-induced degradation
Progesterone supplementation is primarily used in two high-risk populations: women with a history of spontaneous preterm birth and women with a sonographic short cervix in the current pregnancy.
Formulations and Routes of Administration
Two primary formulations of progesterone are used for preterm birth prevention:
| Formulation | Route | Dosage | Primary Indication |
|---|---|---|---|
| 17α-hydroxyprogesterone caproate (17-OHPC) | Intramuscular injection | 250 mg weekly | History of spontaneous preterm birth |
| Micronized progesterone | Vaginal (gel, suppository, or capsule) | 90-200 mg daily | Short cervix (≤25 mm) in current pregnancy |
Key Differences:
- 17-OHPC: Synthetic progestin, longer half-life, weekly administration, systemic effects
- Vaginal progesterone: Natural progesterone, daily administration, higher local uterine/cervical concentrations, fewer systemic effects
17α-hydroxyprogesterone caproate (17-OHPC)
Indication: Women with a singleton pregnancy and history of spontaneous preterm birth before 37 weeks in a previous pregnancy.
Dosage and Administration:
- 250 mg intramuscular injection weekly
- Initiated between 16+0 and 20+6 weeks gestation
- Continued until 36+6 weeks gestation or delivery
Evidence of Efficacy:
- Original Meis trial (2003) showed 34% reduction in recurrent preterm birth with 17-OHPC
- PROLONG trial (2019) failed to confirm benefit in a different population
- Meta-analyses suggest benefit, particularly in high-risk US populations
FDA Status: The FDA approved Makena (brand name 17-OHPC) in 2011 but recommended withdrawal in 2019 after PROLONG trial results. Currently, the medication remains available, and professional organizations continue to include it in treatment guidelines.
Side Effects:
- Injection site pain, swelling, and bruising
- Urticaria (hives) or pruritus
- Nausea
- Depression
- Glucose intolerance (rare)
Contraindications:
- Thrombophlebitis or thromboembolic disorders
- Known or suspected breast cancer or other hormone-sensitive cancer
- Undiagnosed abnormal vaginal bleeding
- Liver dysfunction or disease
- Uncontrolled hypertension
Vaginal Progesterone
Indications:
- Singleton pregnancy with short cervical length (≤25 mm) before 24 weeks gestation
- Alternative to 17-OHPC for history of spontaneous preterm birth
Formulations and Dosage:
- Vaginal gel: 90 mg daily (8% gel, Crinone)
- Vaginal suppository: 100-200 mg daily
- Vaginal capsule: 100-200 mg daily
Timing:
- Typically started after identification of short cervix (often around 20-24 weeks)
- Continued until 36+6 weeks gestation or delivery
Evidence of Efficacy:
- Multiple randomized controlled trials have demonstrated efficacy in women with short cervix
- Meta-analyses show 40-45% reduction in preterm birth in women with short cervix
- Associated with reduction in neonatal morbidity and mortality
Side Effects:
- Vaginal irritation or discharge
- Minimal systemic side effects
- Less injection site pain compared to 17-OHPC
Efficacy in Different Clinical Scenarios
| Clinical Scenario | Recommended Approach | Evidence |
|---|---|---|
| Singleton pregnancy with prior spontaneous preterm birth | 17-OHPC or vaginal progesterone | Strong evidence for 17-OHPC; increasing evidence for vaginal progesterone |
| Singleton pregnancy with short cervix (≤25 mm) | Vaginal progesterone | Strong evidence for efficacy |
| Multiple gestation | Not routinely recommended | No consistent evidence of benefit |
| Preterm premature rupture of membranes | Not recommended | Insufficient evidence |
| Arrested preterm labor | Not routinely recommended | Insufficient evidence |
| Short cervix in twin pregnancies | May consider vaginal progesterone | Limited evidence of possible benefit |
Despite initial promising results, progesterone has not been consistently shown to reduce preterm birth in multiple gestations, and routine use in this population is not currently recommended.
Current Recommendations and Controversies
Current Professional Organization Recommendations:
- ACOG (American College of Obstetricians and Gynecologists): Offers progesterone supplementation for women with singleton pregnancy and prior spontaneous preterm birth or short cervical length.
- SMFM (Society for Maternal-Fetal Medicine): Recommends offering 17-OHPC to women with singleton pregnancy and history of spontaneous preterm birth, and vaginal progesterone for women with singleton pregnancy and short cervical length.
Current Controversies:
- 17-OHPC efficacy: Conflicting results between Meis trial and PROLONG study
- Optimal formulation: Whether vaginal progesterone may replace 17-OHPC for prior preterm birth
- Optimal dosing: Variations in dose and formulation of vaginal progesterone
- Role in multiple gestations: Some subgroups may benefit, but evidence is inconsistent
- Starting earlier: Whether initiating therapy before 16 weeks offers additional benefits
Nursing Implications
Key Nursing Considerations:
- Patient Education:
- Explain purpose and expected benefits
- Teach proper administration technique for vaginal progesterone
- Discuss importance of adherence to weekly injection schedule for 17-OHPC
- Review potential side effects and when to contact healthcare provider
- Administration of 17-OHPC:
- Use proper technique for IM injection (Z-track method recommended)
- Rotate injection sites to minimize local reactions
- Consider use of longer needles for women with higher BMI
- Monitoring:
- Assess for signs of preterm labor at each visit
- Monitor for side effects and compliance
- Document cervical length measurements if performed
MNEMONIC: “PRETERM Prevention with Progesterone”
P – Prior preterm birth? Consider 17-OHPC injections
R – Route matters (IM for history, vaginal for short cervix)
E – Early start is key (16-20 weeks for 17-OHPC)
T – Timing of doses must be consistent
E – Evaluate cervical length to identify candidates
R – Resistance to therapy? Consider other risk factors
M – Multiple gestations don’t routinely benefit
Magnesium Sulfate
Overview & Dual Role
Magnesium sulfate is a versatile medication in high-risk pregnancy management with two primary applications: seizure prophylaxis in preeclampsia/eclampsia and fetal neuroprotection in preterm birth.
General Properties:
- Chemical entity: MgSO₄·7H₂O (heptahydrate)
- Administration route: Intravenous (preferred) or intramuscular
- Crosses placenta: Yes
- Therapeutic serum levels: 4-8 mEq/L (4.8-9.6 mg/dL)
- Half-life: 4-6 hours
- Excretion: Primarily renal
Magnesium sulfate was first used for seizure prevention in eclampsia in 1906 by Dr. J.L. Horn, making it one of the oldest medications still commonly used in obstetrics.
Mechanism of Action
1. Seizure Prophylaxis:
- CNS depressant effect
- Blocks N-methyl-D-aspartate (NMDA) receptors
- Decreases acetylcholine release at motor nerve terminals
- Vasodilation of cerebral blood vessels reduces cerebral ischemia
- May reduce cerebral edema by stabilizing endothelial cells
2. Fetal Neuroprotection:
- Blocks NMDA receptors, preventing excessive calcium influx into neurons
- Reduces inflammatory cytokine production
- Prevents excitatory amino acid-induced damage
- Stabilizes cell membranes
- Anti-apoptotic effects
- May improve cerebral blood flow
3. Other Physiological Effects:
- Mild tocolytic effect (reduces uterine contractility)
- Peripheral vasodilation (reduces blood pressure)
- Increased renal blood flow
- Reduces platelet aggregation
- Bronchodilation
Use for Seizure Prophylaxis in Preeclampsia
Indications:
- Eclampsia (treatment of seizures)
- Severe preeclampsia (prevention of eclampsia)
- Some cases of preeclampsia without severe features (controversial, varies by institution)
Dosing Regimen:
| Indication | Loading Dose | Maintenance Dose | Duration |
|---|---|---|---|
| Severe preeclampsia | 4-6 g IV over 20-30 minutes | 1-2 g/hour IV continuous infusion | 24 hours postpartum or until resolution of severe features |
| Eclampsia (after seizure) | 6 g IV over 15-20 minutes | 2 g/hour IV continuous infusion | 24 hours after last seizure |
Evidence of Efficacy:
- The Magpie Trial (2002) demonstrated that magnesium sulfate reduced the risk of eclampsia by more than 50% compared to placebo
- Superior to phenytoin, diazepam, or nimodipine for seizure prevention
- NNT (Number Needed to Treat) approximately 63-69 women with preeclampsia to prevent one case of eclampsia
- NNT approximately 36 women with severe preeclampsia
Use for Fetal Neuroprotection
Indications:
- Women at high risk for delivery before 32 weeks gestation
- Preterm labor with intact membranes
- Preterm premature rupture of membranes
- Planned preterm birth for maternal or fetal indications
Dosing Regimen:
| Loading Dose | Maintenance Dose | Duration |
|---|---|---|
| 4 g IV over 30 minutes | 1 g/hour IV continuous infusion |
|
Evidence of Efficacy:
- Meta-analyses demonstrate 30-45% reduction in cerebral palsy risk
- Most effective when given within 24 hours of birth
- Number needed to treat: approximately 63 women to prevent one case of cerebral palsy
- Benefit observed primarily for deliveries before 30-32 weeks gestation
Timing Considerations:
- Ideally administered at least 4 hours prior to anticipated birth
- Still beneficial even if delivery occurs sooner
- If imminent delivery is delayed, consider discontinuing after 24 hours
- May be repeated if preterm birth becomes imminent again after previous course
Monitoring and Side Effects
Clinical Monitoring:
- Vital signs (blood pressure, heart rate, respiratory rate)
- Urine output (maintain >30 ml/hour)
- Deep tendon reflexes (DTRs)
- Level of consciousness
- Respiratory assessment
Laboratory Monitoring:
- Serum magnesium levels (therapeutic range: 4-8 mEq/L or 4.8-9.6 mg/dL)
- Renal function (creatinine)
Signs of Magnesium Toxicity by Level:
| Serum Level (mEq/L) | Clinical Manifestations |
|---|---|
| 4-8 | Therapeutic range |
| 8-10 | Loss of patellar reflexes |
| 10-12 | Respiratory depression |
| 15-20 | Cardiac arrest, respiratory paralysis |
Common Side Effects:
- Flushing
- Nausea/vomiting
- Headache
- Lethargy or confusion
- Muscle weakness
- Diplopia (double vision)
- Slurred speech
- Sensation of warmth
- Hypotension (especially with rapid administration)
- Pulmonary edema (rare)
Treatment of Magnesium Toxicity:
- Discontinue magnesium infusion
- Administer calcium gluconate 10% solution (10 ml IV over 3-5 minutes) as antidote
- Provide respiratory support as needed
- Consider dialysis for severe toxicity
Special Considerations
Renal Impairment:
- Magnesium is primarily excreted by the kidneys
- Dose reduction required in women with renal insufficiency
- More frequent serum level monitoring recommended
- Consider starting at 0.5-1 g/hour for women with renal impairment
Concurrent Calcium Channel Blocker Use:
- Combined use can lead to exaggerated hypotension
- Careful blood pressure monitoring required
- Consider using alternative tocolytic if magnesium already in use
Effects on Labor and Delivery:
- May mildly decrease the strength of contractions
- May prolong labor slightly
- Does not preclude use of oxytocin augmentation if needed
Neonatal Effects:
- Transient hypotonia or lethargy may occur
- Respiratory depression (rare with therapeutic maternal levels)
- Decreased intestinal motility
- Hypocalcemia
Anesthetic Considerations:
- Potentiates neuromuscular blocking agents
- May prolong recovery from anesthesia
- Anesthesia providers should be informed about magnesium administration
Nursing Implications
Administration Guidelines:
- Verify order and dose carefully (high-alert medication)
- Use infusion pump for IV administration
- Administer loading dose over appropriate time period (not too rapidly)
- Avoid subcutaneous extravasation (tissue necrosis risk)
- Ensure antidote (calcium gluconate) is readily available
Monitoring Schedule:
| Parameter | Frequency | Target |
|---|---|---|
| Blood pressure | Every 5-15 min during loading, then every 30-60 min | Maintain SBP >90 mmHg |
| Heart rate | Every 30-60 min | 60-100 bpm |
| Respiratory rate | Every 30-60 min | >12 breaths/min |
| Oxygen saturation | Continuous in high-risk patients | >95% |
| Deep tendon reflexes | Every 1-4 hours | Present (1+ to 2+) |
| Urine output | Hourly | >30 mL/hour |
| Serum magnesium levels | 6-12 hours after initiation and dose changes | 4-8 mEq/L |
Critical Assessment Sequence (REFLECT):
- Respiratory rate (>12/min)
- Excretion of urine (>30 mL/hr)
- Fetal heart rate (reassuring pattern)
- Level of consciousness (alert, oriented)
- Evaluate deep tendon reflexes (present)
- Calcium gluconate availability
- Toxicity signs (monitor for)
Patient Education:
- Explain purpose of medication (seizure prevention or neuroprotection)
- Prepare for sensation of warmth, flushing during administration
- Describe monitoring procedures
- Instruct to report difficulty breathing, chest pain, or severe headache
- Explain importance of maintaining bed rest with assistance
MNEMONIC: “MgSO4 SAFETY”
M – Monitor vital signs regularly
g – Gluconate (calcium) available as antidote
S – Seizure prevention or neuroprotection (know the purpose)
O – Output (urine) must be >30 mL/hour
4 – 4-8 mEq/L is the therapeutic range
S – Side effects (explain to patient)
A – Absence of reflexes requires dose reduction
F – Fetal monitoring while on therapy
E – Evaluate respiratory rate frequently
T – Toxicity signs to watch for
Y – Yield to physician if complications arise
Low-Dose Aspirin for Preeclampsia Prevention
Overview & Rationale
Low-dose aspirin (LDA) is recommended for the prevention of preeclampsia in women at high risk. Preeclampsia, a multisystem disorder characterized by hypertension and proteinuria or end-organ dysfunction after 20 weeks gestation, affects 2-8% of pregnancies worldwide and is a leading cause of maternal and perinatal morbidity and mortality.
Pathophysiologic Rationale:
- Preeclampsia involves placental implantation defects and endothelial dysfunction
- Imbalance between prostacyclin (vasodilator) and thromboxane (vasoconstrictor) production
- Low-dose aspirin selectively inhibits thromboxane synthesis without significantly affecting prostacyclin
- This rebalances the prostacyclin:thromboxane ratio, improving placental perfusion
- May also have anti-inflammatory and antioxidant effects
Low-dose aspirin specifically refers to doses between 60-150 mg daily, which selectively inhibit platelet cyclooxygenase without significantly affecting vascular endothelial prostacyclin production.
Indications and Risk Assessment
High-Risk Factors (One factor sufficient for LDA recommendation):
- History of preeclampsia, especially with adverse outcomes
- Multifetal gestation
- Chronic hypertension
- Type 1 or Type 2 diabetes
- Renal disease
- Autoimmune disease (systemic lupus erythematosus, antiphospholipid syndrome)
Moderate-Risk Factors (LDA recommended with ≥2 factors):
- Nulliparity
- Obesity (BMI >30 kg/m²)
- Family history of preeclampsia (mother or sister)
- Age ≥35 years
- Sociodemographic characteristics (African American race, low socioeconomic status)
- Personal history factors (previous adverse pregnancy outcome, >10-year pregnancy interval)
Additional Indicators:
- Abnormal uterine artery Doppler studies
- Elevated first-trimester markers (PAPP-A, PlGF)
- History of placental insufficiency
Dosage and Administration
Recommended Dose:
- 81-150 mg daily (most common: 81 mg in US, 75-150 mg in Europe)
- Recent evidence suggests that 150 mg may be more effective than lower doses
Timing of Initiation:
- Optimally started between 12-16 weeks gestation
- May be initiated as early as after confirmation of pregnancy
- Still beneficial if started before 28 weeks, but efficacy decreases with later initiation
- Most recent data suggest maximum benefit when started before 16 weeks
Administration Recommendations:
- Take at bedtime (maximizes efficacy based on circadian rhythm of blood pressure)
- Take with food if GI upset occurs
- Use enteric-coated formulations to reduce GI irritation
- No need for monitoring of platelet function or aspirin levels
Duration:
- Continue until delivery
- May be discontinued at 36 weeks in some protocols to reduce theoretical bleeding risk
- No need to taper off; can be discontinued abruptly
Efficacy and Evidence
Overall Effectiveness:
- Meta-analyses show 10-30% reduction in preeclampsia risk, with greater benefit in high-risk women
- 17% reduction in preterm birth
- 14% reduction in fetal/neonatal death
- 20% reduction in fetal growth restriction
Key Studies:
- ASPRE Trial (2017): 150 mg aspirin started at 11-14 weeks reduced preterm preeclampsia by 62% in high-risk women identified by screening
- US Preventive Services Task Force Meta-analysis (2014): 17% reduction in risk of preeclampsia across all women, with greater benefit in high-risk groups
- CLASP Trial: Demonstrated safety of low-dose aspirin in pregnancy
Factors Affecting Efficacy:
| Factor | Impact on Efficacy | Evidence |
|---|---|---|
| Dosage | Higher doses (≥100 mg) appear more effective | Multiple meta-analyses |
| Timing of initiation | Starting before 16 weeks more effective | ASPRE trial, meta-analyses |
| Time of day | Bedtime administration more effective | Chronotherapy studies |
| Risk level | Greater benefit in higher-risk women | Consistent across studies |
| Adherence | Regular daily use required | Compliance studies |
| Maternal weight | May need higher doses for obesity | Emerging evidence |
