Hirschsprung’s Disease (Megacolon)
Comprehensive Nursing Notes
Overview
Hirschsprung’s disease (also known as congenital aganglionic megacolon) is a congenital disorder characterized by the absence of ganglion cells in the distal colon, resulting in functional intestinal obstruction.
It affects approximately 1 in 5,000 live births and is more common in males than females (4:1 ratio). About 30% of cases are associated with other congenital anomalies or genetic syndromes, particularly Down syndrome (trisomy 21).
Significance
- Leading cause of functional intestinal obstruction in neonates
- Can lead to life-threatening enterocolitis if untreated
- Requires prompt diagnosis and surgical intervention
- Long-term follow-up needed for bowel management
Quick Facts
- First described by Harald Hirschsprung in 1886
- 80% of cases diagnosed within first year of life
- Short-segment disease (affecting rectosigmoid only) occurs in 80% of cases
- Long-segment disease extends proximal to the sigmoid colon
- Total colonic aganglionosis occurs in 5-10% of cases
Pathophysiology
Etiology & Developmental Basis
Hirschsprung’s disease results from the failure of neural crest cell migration during embryonic development (typically between weeks 5-12 of gestation). This leads to the absence of ganglion cells in the submucosal (Meissner’s) and myenteric (Auerbach’s) plexuses of the intestinal wall.
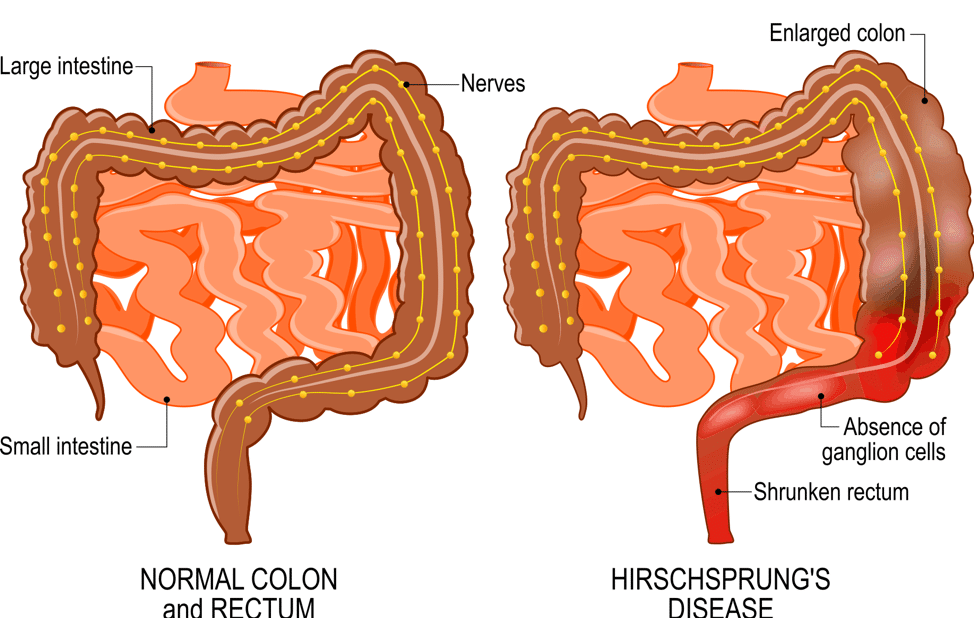
Figure 1: Pathophysiology of Hirschsprung’s Disease showing normal vs. aganglionic segment
Abnormal Findings
- Aganglionosis: Absence of ganglion cells in affected bowel segments
- Hypertrophied nerve trunks: Thickened nerve bundles in submucosa
- Increased acetylcholinesterase activity: Detectable on histochemical staining
- Transition zone: Area between normal and aganglionic bowel
- Proximal dilation: Distended colon proximal to aganglionic segment
Functional Consequences
- Loss of coordinated peristalsis: Inability to propel intestinal contents
- Persistent contraction: Tonic contraction of affected segment
- Functional obstruction: Mechanical blockage of intestinal transit
- Fecal stasis: Accumulation of stool proximal to obstruction
- Bacterial overgrowth: Risk of enterocolitis due to stasis
Genetic Factors
Several genes have been implicated in Hirschsprung’s disease, with RET proto-oncogene mutations being the most common (found in 50% of familial cases and 15-20% of sporadic cases). Other genes include GDNF, EDNRB, EDN3, and SOX10.
Classification Based on Extent of Aganglionosis
| Type | Description | Frequency | Clinical Significance |
|---|---|---|---|
| Short-segment | Involves rectum and distal sigmoid colon only | 80% | Better prognosis, simpler surgical approach |
| Long-segment | Extends proximal to sigmoid colon but not total colon | 15% | More complex surgery, higher complication risk |
| Total colonic | Involves entire colon, may extend into small bowel | 5% | Most challenging to manage, poorest functional outcomes |
| Total intestinal | Entire colon and significant small bowel involvement | <1% | Extremely rare, may require intestinal transplantation |
Clinical Manifestations
The clinical presentation of Hirschsprung’s disease varies depending on the extent of intestinal involvement and the age at diagnosis. Most cases are diagnosed in the neonatal period, but some may present later in infancy or childhood.
Neonatal Presentation
- Failure to pass meconium within 24-48 hours of birth (90% of normal infants pass meconium within 24 hours)
- Abdominal distention
- Bilious vomiting
- Reluctance to feed
- Signs of intestinal obstruction
- Enterocolitis (in severe cases)
Infant Presentation
- Chronic constipation
- Abdominal distention
- Failure to thrive
- Infrequent, explosive bowel movements
- Ribbon-like stools
- Intestinal obstruction episodes
- Enterocolitis (progressive, potentially fatal)
Older Child Presentation
- Chronic severe constipation
- Significant abdominal distention
- Growth delay
- Malnutrition
- Overflow fecal incontinence
- Palpable fecal mass
- History of constipation since birth
Classic Clinical Triad (Present in ~25% of cases)
Abdominal Distention
Bilious Vomiting
Failure to Pass Meconium
Hirschsprung-Associated Enterocolitis (HAEC) – Medical Emergency!
HAEC is a life-threatening complication that can occur before or after surgical treatment.
- Explosive diarrhea
- Abdominal distention
- Fever
- Lethargy
- Vomiting
- Can progress to septic shock and intestinal perforation
- Mortality rate: 30% if untreated
Diagnosis
Diagnosis of Hirschsprung’s disease involves clinical suspicion based on symptoms, followed by specialized imaging studies and ultimately confirmation by histopathologic examination.
Initial Diagnostic Approach
Clinical Evaluation
- Detailed history (delayed passage of meconium, constipation)
- Physical examination (abdominal distention, vomiting)
- Digital rectal examination (typically reveals empty rectum)
- Explosive stool release after rectal exam (characteristic)
Laboratory Studies
- CBC with differential (to evaluate for infection/inflammation)
- Electrolytes (to assess for dehydration)
- Arterial blood gases (in severe cases)
- Stool cultures (to rule out infectious causes)
Imaging Studies
Plain Abdominal X-ray
- Shows dilated loops of bowel
- Air-fluid levels
- Paucity of air in rectum
Contrast Enema
- Key diagnostic imaging study
- Shows narrowed distal segment (aganglionic)
- Dilated proximal segment (ganglionic)
- Transition zone between narrow and dilated segments
- Retention of contrast for >24 hours

Figure 2: Contrast enema showing characteristic transition zone (arrow) between the narrow aganglionic segment and dilated proximal bowel
Confirmatory Testing (Gold Standard)
Rectal Biopsy
Full-thickness or suction rectal biopsy is the definitive diagnostic test for Hirschsprung’s disease.
Histopathologic Findings
- Absence of ganglion cells in submucosal (Meissner’s) plexus
- Absence of ganglion cells in myenteric (Auerbach’s) plexus
- Hypertrophied nerve trunks
- Increased acetylcholinesterase activity (special stain)
Biopsy Types
- Suction biopsy: Less invasive, obtains submucosa only
- Full-thickness biopsy: Surgical, provides both submucosa and myenteric plexus
- Biopsies taken 2-3 cm above dentate line (to avoid physiologic hypoganglionosis)
- Multiple biopsies may be needed to identify transition zone

Figure 3: Histopathologic findings showing absence of ganglion cells and hypertrophied nerve trunks in submucosa
Additional Diagnostic Studies
Anorectal Manometry
Used in older children; shows absence of the rectoanal inhibitory reflex (RAIR).
Genetic Testing
May be considered in familial cases or when associated with syndromes.
Treatment & Management
The definitive treatment for Hirschsprung’s disease is surgical intervention to remove or bypass the aganglionic segment. Management involves preoperative stabilization, surgical correction, and long-term follow-up.
Preoperative Management
- Bowel decompression: Rectal irrigation with normal saline
- Nutritional support: May require parenteral nutrition
- Fluid and electrolyte replacement
- Antibiotics: If enterocolitis is present
- Temporary colostomy: May be needed in emergency situations
Management of Enterocolitis
- Bowel rest: NPO status
- Aggressive rectal irrigations: Every 6-8 hours
- IV fluids and electrolyte replacement
- Broad-spectrum antibiotics: Coverage for anaerobes
- Monitoring for sepsis
- Emergency surgery: If perforation occurs
Surgical Approaches
Several surgical procedures may be used to treat Hirschsprung’s disease. All involve removing or bypassing the aganglionic segment and preserving sphincter function.
| Procedure | Description | Advantages | Considerations |
|---|---|---|---|
| Swenson Procedure | Resection of aganglionic segment with end-to-end anastomosis | Original procedure, proven long-term results | Risk of damage to pelvic nerves, technically challenging |
| Duhamel Procedure | Aganglionic rectum left in place, ganglionic colon pulled behind and anastomosed side-to-side | Lower risk of pelvic nerve damage | Potential for stool trapping in rectal pouch |
| Soave (Endorectal Pull-through) | Mucosa of aganglionic rectum removed, ganglionic colon pulled through muscular sleeve | Preserves rectal muscle, reduces risk to pelvic structures | Technically demanding, potential for cuff abscess |
| Transanal Endorectal Pull-through | Similar to Soave but performed entirely through the anus | No abdominal incision, shorter hospital stay | Limited to shorter segment disease |
| Laparoscopic-Assisted Pull-through | Combines minimally invasive abdominal approach with transanal technique | Minimal scarring, faster recovery | Requires specialized equipment and training |
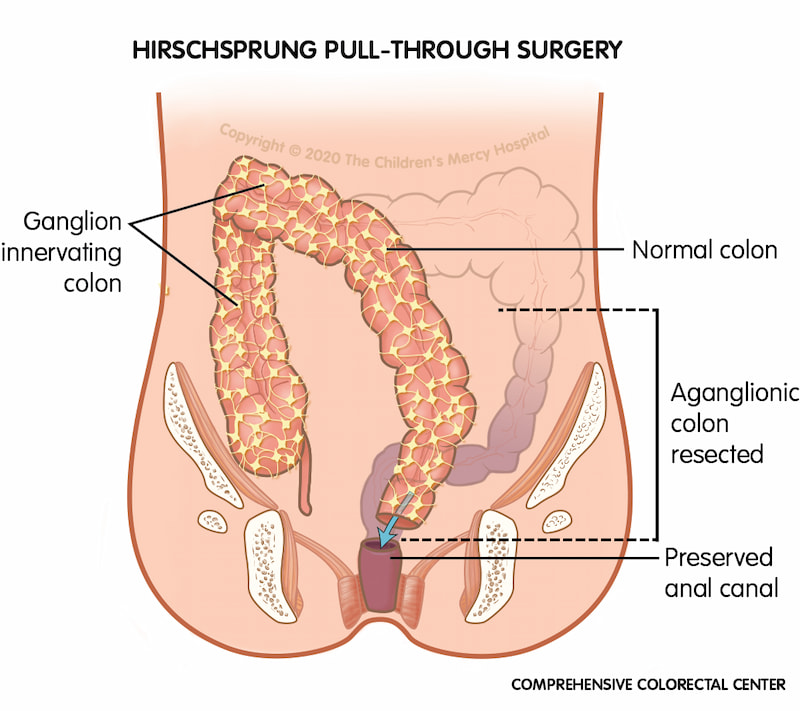
Figure 4: Illustration of pull-through procedure for Hirschsprung’s Disease
Staged vs. Primary Procedures
Staged Approach
- Initial colostomy: Temporary diversion proximal to aganglionic segment
- Definitive pull-through: Performed when infant is stable and larger
- Colostomy closure: Final stage after successful pull-through
- Often used for: Premature infants, enterocolitis, long-segment disease
Primary (Single-Stage) Approach
- Definitive repair without prior colostomy
- Increasingly common with modern techniques
- Can be performed in neonatal period
- Benefits: Single operation, avoids stoma complications
- Best for: Stable infants, short-segment disease
Long-Term Management
Constipation Management
- Dietary modifications (high fiber)
- Adequate hydration
- Laxatives or stool softeners
- Regular toilet schedule
Fecal Incontinence
- Bowel management program
- Timed enemas
- Biofeedback training
- Dietary adjustments
Monitoring
- Regular follow-up with pediatric surgeon
- Growth and nutritional assessment
- Monitoring for late complications
- Psychosocial support
Long-Term Complications
- Enterocolitis: Can occur even after surgical correction (5-35% of patients)
- Constipation: Most common long-term complication (30-50%)
- Fecal incontinence: May affect quality of life significantly
- Stricture: At the anastomosis site
- Adhesive bowel obstruction
- Failure to thrive: Due to persistent feeding problems
- Functional megacolon: Due to transition zone issues
Nursing Management & Care Plan
Nursing care for patients with Hirschsprung’s disease is focused on preoperative care, postoperative management, and long-term support. The nursing process follows the framework of assessment, diagnosis, planning, implementation, and evaluation.
Key Nursing Assessments
Preoperative Assessment
- Abdominal assessment (distention, bowel sounds, visible peristalsis)
- Stool patterns and characteristics
- Nutritional status and weight
- Fluid and electrolyte balance
- Signs of enterocolitis (fever, diarrhea, lethargy)
- Vomiting (frequency, character)
- Parent-infant bonding
Postoperative Assessment
- Vital signs (monitor for infection, pain, dehydration)
- Abdominal assessment (distention, bowel sounds)
- Surgical site (signs of infection, dehiscence)
- Stoma function (if present)
- Bowel function (first passage of stool, consistency)
- Pain assessment
- Fluid and nutrition intake
- Family coping and understanding of care
Nursing Diagnoses
| Nursing Diagnosis | Related Factors | Defining Characteristics |
|---|---|---|
| Risk for Deficient Fluid Volume | Vomiting, diarrhea, inadequate oral intake, fluid losses from GI tract | Decreased urine output, dry mucous membranes, poor skin turgor, altered electrolytes |
| Impaired Skin Integrity | Surgical incision, ostomy, frequent stooling or diarrhea | Disruption of skin surface, perianal excoriation, stomal complications |
| Imbalanced Nutrition: Less Than Body Requirements | Decreased oral intake, intestinal dysfunction, increased metabolic demands | Weight loss, failure to thrive, poor wound healing, decreased appetite |
| Constipation/Diarrhea | Intestinal dysmotility, surgical alterations, enterocolitis | Change in bowel pattern, abdominal distention, explosive bowel movements |
| Risk for Infection | Surgical procedure, invasive lines, enterocolitis | Fever, redness at surgical site, purulent drainage, elevated WBC |
| Anxiety (Parental) | Chronicity of condition, invasive procedures, uncertain prognosis | Expressed concerns, questions, apprehension, increased tension |
| Deficient Knowledge | New diagnosis, complex care requirements, unfamiliarity with condition | Questions, misconceptions, improper care techniques, verbalized concern |
Nursing Interventions
Preoperative Interventions
- Maintain NPO status as ordered prior to surgery
- Administer IV fluids to maintain hydration and electrolyte balance
- Perform rectal irrigations as ordered to decompress bowel
- Monitor vital signs and abdominal assessment q4h
- Prepare parents for surgical procedure and expected outcomes
- Administer prophylactic antibiotics as ordered
- Maintain accurate I&O (input and output) record
- Provide emotional support to child and family
Postoperative Interventions
- Monitor vital signs frequently per protocol
- Assess pain and administer appropriate analgesics
- Maintain IV fluids until oral intake is adequate
- Assess surgical site/stoma for complications
- Monitor for return of bowel function (passage of flatus, stool)
- Advance diet as tolerated per protocol
- Provide stoma care if present (colostomy/ileostomy)
- Maintain surgical drains if present
- Prevent pressure injuries through frequent repositioning
- Monitor for signs of enterocolitis (distention, fever, explosive diarrhea)
Stoma Care (If Present)
- Assess stoma for color, size, and viability (should be pink to red)
- Measure stoma size for appropriate appliance fitting
- Change ostomy appliance every 3-5 days or as needed
- Empty ostomy pouch when 1/3 to 1/2 full
- Protect peristomal skin with barrier products
- Teach parents stoma care techniques
- Document stoma output (amount, consistency, color)
Family Education & Discharge Planning
- Teach parents to recognize signs of complications (enterocolitis, obstruction)
- Provide written instructions for home care
- Demonstrate and have parents return-demonstrate stoma care (if applicable)
- Discuss dietary needs and bowel management strategies
- Review medication administration (stool softeners, laxatives as needed)
- Provide contact information for healthcare team
- Schedule follow-up appointments
- Refer to community resources and support groups
- Connect with home care nursing if needed
Warning Signs to Teach Parents
Instruct parents to seek immediate medical attention if any of these occur:
- Fever (>38.0°C or 100.4°F)
- Increasing abdominal distention
- Explosive or foul-smelling diarrhea
- Vomiting
- Lethargy or irritability
- Bloody stools
- Decreased urine output
- Excessive crying or signs of pain
- Refusal to eat
- Changes in stoma appearance (if present)
Expected Outcomes
Short-Term Outcomes
- Maintains adequate hydration status
- Returns to preoperative weight
- Surgical site heals without complications
- Establishes regular bowel pattern
- Parents demonstrate proper stoma care (if applicable)
- Pain is effectively managed
Long-Term Outcomes
- Achieves normal growth patterns
- Maintains bowel continence appropriate for age
- Absence of recurrent enterocolitis
- Family demonstrates competence in all aspects of care
- Successfully adapts to living with chronic condition
- Meets developmental milestones
Memory Aids & Mnemonics
H-I-R-S-C-H-S-P-R-U-N-G
Use this mnemonic to remember the key features of Hirschsprung’s disease:
NO GANGLION
Remember the clinical presentations with this mnemonic:
HAEC Warning Signs: FEVER
Remember the warning signs of Hirschsprung-Associated Enterocolitis:
Concept Map: Hirschsprung’s Disease
References & Further Reading
- National Institute of Diabetes and Digestive and Kidney Diseases. (2023). Hirschsprung Disease. https://www.niddk.nih.gov/health-information/digestive-diseases/hirschsprung-disease
- Mayo Clinic. (2024). Hirschsprung’s disease. https://www.mayoclinic.org/diseases-conditions/hirschsprungs-disease/symptoms-causes/syc-20351556
- Demarest, L. (2023). Hirschsprung disease: What the nurse needs to know. Nursing made Incredibly Easy, 21(2), 46-51.
- Kessmann, J. (2006). Hirschsprung’s disease: diagnosis and management. American Family Physician, 74(8), 1319-1322.
- Nurseslabs. (2024). Hirschsprung Disease (Aganglionic Megacolon). https://nurseslabs.com/hirschsprung-disease-aganglionic-megacolon/
- Pathology Outlines. (2022). Colon – Hirschsprung disease. https://www.pathologyoutlines.com/topic/colonhirschsprung.html
- TeachMe Paediatrics. (2019). Hirschsprung’s disease – Pathophysiology. https://teachmepaediatrics.com/surgery/abdominal/hirschsprungs-disease/
- Langer, J. C. (2020). Hirschsprung disease. Current Opinion in Pediatrics, 32(3), 391-395.
