Human Physiology for Nursing Students
Comprehensive Study Guide for Understanding Body Systems
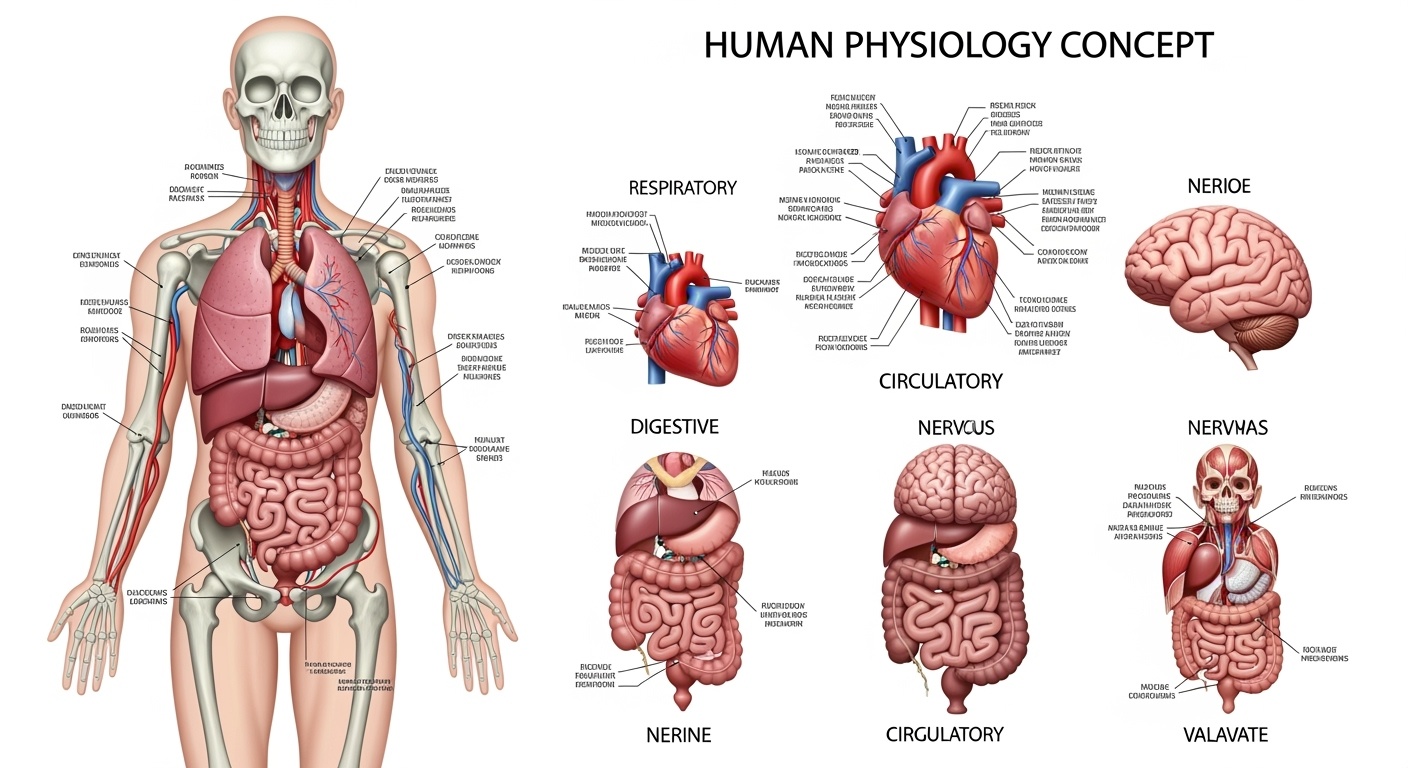
Introduction to Human Physiology
Human physiology is the scientific study of how the human body functions at cellular, tissue, organ, and system levels. For nursing students, understanding human physiology is fundamental to providing excellent patient care, as it forms the foundation for comprehending pathophysiology, pharmacology, and clinical decision-making.
The human body consists of interconnected systems that work harmoniously to maintain homeostasis. Each system has specific functions while contributing to overall body wellness. As future nurses, mastering these concepts will enable you to assess patients effectively, understand disease processes, and implement appropriate interventions.
Nursing Application
Understanding human physiology helps nurses anticipate patient needs, recognize early signs of complications, and educate patients about their health conditions effectively.
Digestion and Absorption
The digestive system transforms food into absorbable nutrients through mechanical and chemical processes. This complex system involves multiple organs working together to break down macronutrients and absorb essential vitamins, minerals, and water.
Key Components of Digestion
| Organ | Function | Enzymes/Secretions |
|---|---|---|
| Mouth | Mechanical breakdown, initial starch digestion | Salivary amylase, mucus |
| Stomach | Protein digestion, food storage | Pepsin, HCl, intrinsic factor |
| Small Intestine | Major absorption site, complete digestion | Intestinal enzymes, bile salts |
| Large Intestine | Water absorption, waste formation | Mucus, bacterial enzymes |
Absorption Mechanisms
The small intestine, particularly the jejunum and ileum, serves as the primary absorption site. Villi and microvilli increase surface area by approximately 600 times, facilitating efficient nutrient uptake through various transport mechanisms including passive diffusion, facilitated diffusion, and active transport.
Nursing Clinical Example
When caring for patients with malabsorption disorders like Crohn’s disease, nurses must monitor for signs of nutritional deficiencies, including weight loss, anemia, and vitamin deficiencies. Understanding normal digestion helps identify when interventions like nutritional supplements or dietary modifications are needed.
Breathing and Respiration
The respiratory system facilitates gas exchange between the atmosphere and blood, ensuring adequate oxygen delivery and carbon dioxide removal. This system includes conducting airways and respiratory zones working together to maintain proper gas exchange and acid-base balance.
Mechanism of Breathing
Breathing involves two phases: inspiration (inhalation) and expiration (exhalation). During inspiration, the diaphragm contracts and moves downward while intercostal muscles expand the rib cage, creating negative pressure that draws air into the lungs. Expiration is typically passive, occurring as muscles relax and lung elasticity forces air out.
Regulation of Breathing
Neural Control
- Medulla oblongata: Primary respiratory center
- Pons: Modifies breathing pattern
- Cerebral cortex: Voluntary control
- Chemoreceptors: Detect CO2, O2, and pH levels
Chemical Control
- Increased CO2: Primary stimulus for breathing
- Decreased O2: Secondary stimulus
- pH changes: Affect respiratory rate
- Peripheral chemoreceptors: Monitor blood gases
| Respiratory Parameter | Normal Values | Clinical Significance |
|---|---|---|
| Tidal Volume (TV) | 500 mL | Air volume during normal breathing |
| Vital Capacity (VC) | 4800 mL | Maximum air volume expelled |
| Respiratory Rate | 12-20 breaths/min | Indicator of respiratory health |
Nursing Assessment Application
Nurses regularly assess respiratory function by monitoring breathing patterns, oxygen saturation, and respiratory rate. Understanding normal human physiology of breathing helps identify abnormalities like dyspnea, tachypnea, or irregular breathing patterns that may indicate underlying pathology.
Body Fluids and Circulation
The human circulatory system consists of the heart, blood vessels, and blood, working together to transport nutrients, oxygen, hormones, and waste products throughout the body. This closed-loop system maintains cellular homeostasis and supports all bodily functions.
Heart Structure and Function
The heart is a four-chambered muscular pump consisting of two atria and two ventricles. The cardiac cycle involves systematic contraction (systole) and relaxation (diastole) phases, generating pressure gradients that propel blood through pulmonary and systemic circuits.
Cardiac Conduction System
- Sinoatrial (SA) node: Natural pacemaker
- Atrioventricular (AV) node: Delays impulse
- Bundle of His: Conducts to ventricles
- Purkinje fibers: Spread impulse rapidly
Blood Circulation Pathways
- Pulmonary circulation: Heart to lungs
- Systemic circulation: Heart to body tissues
- Coronary circulation: Heart muscle perfusion
- Portal circulation: Liver and kidneys
Blood Composition and Functions
| Blood Component | Percentage | Primary Functions |
|---|---|---|
| Plasma | 55% | Transport medium, maintaining blood pressure |
| Red Blood Cells | 42% | Oxygen and carbon dioxide transport |
| White Blood Cells | 2% | Immune defense and infection fighting |
| Platelets | 1% | Blood clotting and hemostasis |
Nursing Cardiovascular Care
Nurses continuously monitor cardiovascular status through vital signs, cardiac rhythm assessment, and fluid balance evaluation. Understanding human physiology of circulation enables early detection of cardiac complications and appropriate intervention strategies for patients with cardiovascular conditions.
Human Excretory System
The excretory system maintains homeostasis by removing metabolic wastes, regulating water balance, and controlling electrolyte concentrations. The kidneys serve as the primary organs, filtering blood and producing urine while maintaining acid-base balance and blood pressure regulation.
Kidney Structure and Function
Each kidney contains approximately one million nephrons, the functional units responsible for filtration, reabsorption, and secretion. The nephron consists of the glomerulus, Bowman’s capsule, proximal tubule, loop of Henle, distal tubule, and collecting duct, each performing specific functions in urine formation.
Filtration
Blood pressure forces water and solutes through glomerular capillaries into Bowman’s capsule, forming filtrate.
Reabsorption
Essential substances like glucose, amino acids, and water are reclaimed from filtrate back into blood.
Secretion
Additional wastes and excess ions are actively transported from blood into urine.
Urine Formation Process
| Nephron Region | Process | Substances Involved |
|---|---|---|
| Glomerulus | Filtration | Water, glucose, amino acids, urea, ions |
| Proximal Tubule | Reabsorption (65%) | Glucose, amino acids, sodium, water |
| Loop of Henle | Concentration | Water and salt reabsorption |
| Collecting Duct | Final regulation | Water, sodium, potassium balance |
Nursing Renal Assessment
Nurses monitor kidney function through urinalysis, fluid intake/output measurements, and serum creatinine levels. Understanding renal human physiology helps nurses recognize signs of kidney dysfunction, manage fluid restrictions, and educate patients about maintaining kidney health.
Locomotion and Movement
The skeletal system provides structural support, protects vital organs, produces blood cells, and serves as mineral storage. Working with the muscular system, it enables movement, maintains posture, and generates heat through muscle contractions.
Skeletal System Functions
Mechanical Functions
- Support: Framework for body structure
- Protection: Shields organs from injury
- Movement: Provides attachment for muscles
- Shape: Determines body form and posture
Metabolic Functions
- Hematopoiesis: Blood cell production
- Mineral storage: Calcium and phosphorus
- Acid-base balance: pH regulation
- Energy metabolism: Fat storage in marrow
Types of Muscle Tissue
| Muscle Type | Location | Control | Function |
|---|---|---|---|
| Skeletal | Attached to bones | Voluntary | Body movement, posture |
| Cardiac | Heart wall | Involuntary | Blood circulation |
| Smooth | Organs, blood vessels | Involuntary | Organ function, peristalsis |
Nursing Mobility Assessment
Nurses assess musculoskeletal function through range of motion testing, strength evaluation, and mobility status. Understanding human physiology of movement helps nurses develop rehabilitation plans, prevent complications from immobility, and promote patient independence in activities of daily living.
Nervous System in Humans
The nervous system coordinates and controls body activities through electrical and chemical signals. It consists of the central nervous system (brain and spinal cord) and peripheral nervous system (nerves and ganglia), working together to process information, generate responses, and maintain homeostasis.
Central Nervous System
Brain Functions
- Cerebrum: Higher cognitive functions
- Cerebellum: Balance and coordination
- Brainstem: Vital functions control
- Diencephalon: Relay and integration
Spinal Cord Functions
- Signal transmission to/from brain
- Reflex arc coordination
- Motor pattern generation
- Sensory information processing
Neuron Structure and Function
Neurons are specialized cells that transmit electrical impulses throughout the nervous system. They consist of cell body, dendrites, and axons, with synapses facilitating communication between neurons through neurotransmitter release.
| Neurotransmitter | Location | Primary Function |
|---|---|---|
| Acetylcholine | Neuromuscular junctions | Muscle contraction, memory |
| Dopamine | Brain reward pathways | Movement, motivation |
| Serotonin | Brain stem, gut | Mood regulation, sleep |
Nursing Neurological Assessment
Nurses perform comprehensive neurological assessments including Glasgow Coma Scale, pupil reactions, and reflex testing. Understanding nervous system human physiology enables nurses to recognize neurological changes, monitor patient safety, and implement appropriate neuroprotective interventions.
Sense Organs – Eye and Ear
The sense organs enable perception of environmental stimuli, providing crucial information for survival and interaction. The eye and ear are complex structures that convert light and sound waves into neural signals, allowing vision and hearing respectively.
Eye Structure and Vision
The human eye consists of multiple layers and structures working together to focus light and convert it into electrical signals. The cornea and lens focus light onto the retina, where photoreceptors (rods and cones) detect light and color, transmitting signals through the optic nerve to the brain.
Eye Components
- Cornea: Primary light refraction
- Iris: Controls light entry
- Lens: Fine-tunes focus
- Retina: Contains photoreceptors
- Vitreous humor: Maintains eye shape
Ear Components
- Outer ear: Collects sound waves
- Middle ear: Amplifies vibrations
- Inner ear: Converts to neural signals
- Cochlea: Hearing organ
- Vestibular system: Balance control
Hearing and Balance Mechanisms
Sound waves travel through the external auditory canal, causing tympanic membrane vibration. These vibrations are amplified by ossicles in the middle ear and transmitted to the cochlea, where hair cells convert mechanical energy into electrical signals. The vestibular system maintains balance through detection of head movements and position.
| Sensory Function | Receptor Type | Location | Clinical Assessment |
|---|---|---|---|
| Vision | Photoreceptors | Retina | Visual acuity, visual fields |
| Hearing | Hair cells | Cochlea | Audiometry, Weber test |
| Balance | Vestibular hair cells | Inner ear | Romberg test, gait assessment |
Nursing Sensory Assessment
Nurses assess sensory function through vision screenings, hearing tests, and balance evaluations. Understanding sensory organ human physiology helps nurses identify sensory deficits, implement safety measures, and develop communication strategies for patients with sensory impairments.
Human Endocrine System
The endocrine system regulates body functions through hormone secretion, maintaining homeostasis and coordinating growth, metabolism, and reproduction. This system consists of glands that release hormones directly into the bloodstream, providing long-term regulation of physiological processes.
Major Endocrine Glands
| Gland | Hormones | Primary Functions |
|---|---|---|
| Pituitary | GH, ACTH, TSH, ADH | Growth, metabolism regulation |
| Thyroid | T3, T4, Calcitonin | Metabolic rate, calcium regulation |
| Adrenal | Cortisol, Aldosterone, Epinephrine | Stress response, blood pressure |
| Pancreas | Insulin, Glucagon | Blood glucose regulation |
Hormone Regulation Mechanisms
Negative Feedback
Most common mechanism where hormone levels are regulated by their own effects, maintaining homeostasis.
Positive Feedback
Less common mechanism that amplifies hormone effects, like oxytocin during childbirth.
Neural Control
Direct nervous system regulation of hormone release, particularly for stress hormones.
Understanding human physiology of the endocrine system is crucial for nurses as hormonal imbalances affect multiple body systems simultaneously. The interconnected nature of endocrine glands means that dysfunction in one gland often impacts others, requiring comprehensive assessment and management approaches.
Nursing Endocrine Care
Nurses monitor endocrine function through hormone level testing, blood glucose monitoring, and assessment of metabolic indicators. Understanding endocrine human physiology enables nurses to recognize hormone-related symptoms, manage diabetes care, and educate patients about endocrine disorders and their treatments.
Conclusion
Mastering human physiology provides the foundation for excellence in nursing practice. Each body system works in harmony to maintain life, and understanding these intricate relationships enables nurses to provide comprehensive, patient-centered care. From assessing respiratory function to managing endocrine disorders, physiological knowledge guides clinical decision-making and improves patient outcomes.
As healthcare continues to evolve, the fundamental principles of human physiology remain constant. This knowledge empowers nurses to adapt to new technologies, understand emerging treatments, and maintain the highest standards of patient care across all healthcare settings.
Continuing Education
Regular review and application of physiological concepts through clinical practice, continuing education, and professional development ensures that nurses maintain current knowledge and provide evidence-based care throughout their careers.
