Hydrocarbons in Nursing Practice
A comprehensive study guide for nursing professionals covering clinical applications, safety protocols, and evidence-based management of hydrocarbon exposure
Table of Contents
Understanding Hydrocarbons in Healthcare
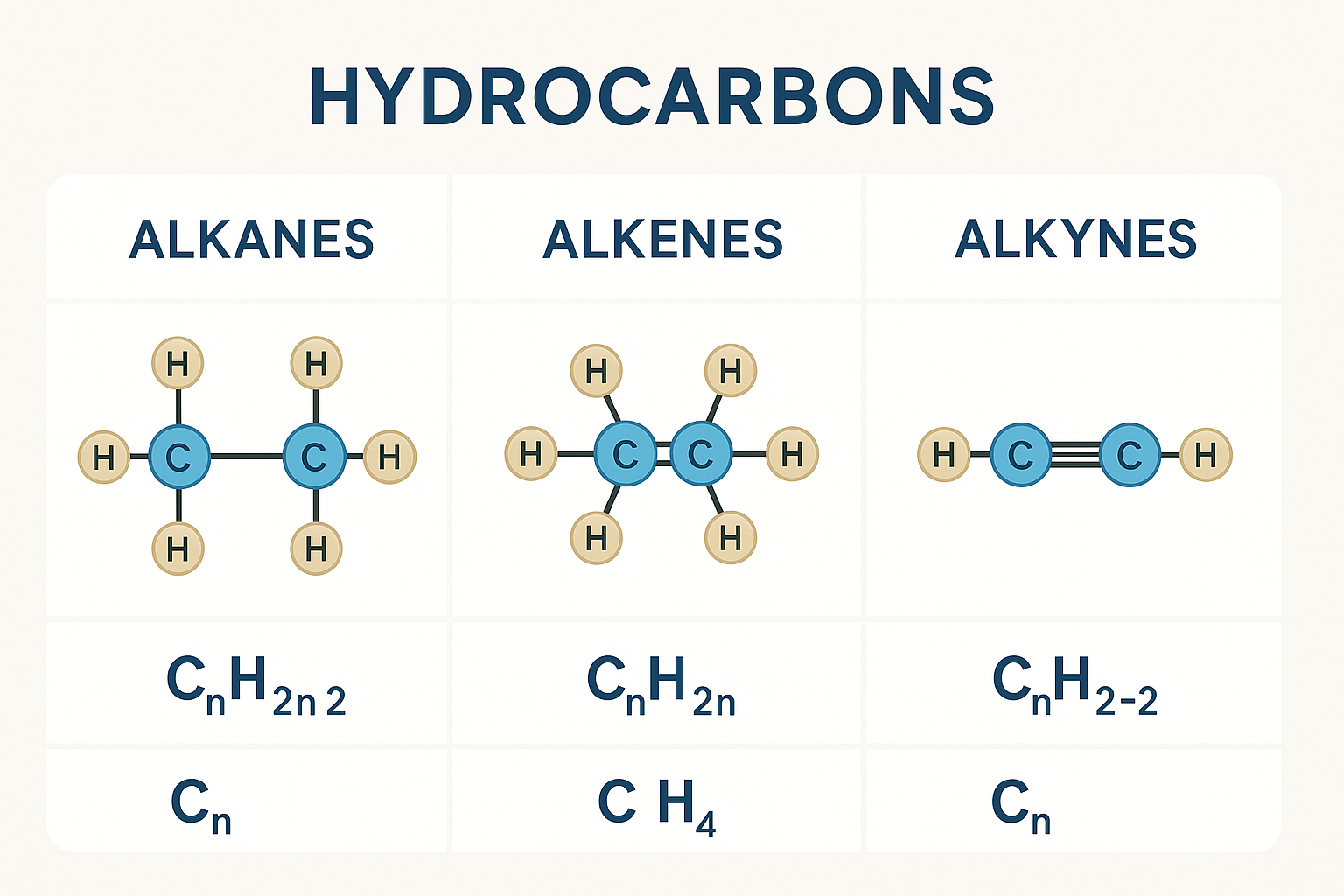
A hydrocarbon represents one of the most fundamental chemical compounds encountered in healthcare settings, consisting exclusively of hydrogen and carbon atoms. For nursing professionals, understanding hydrocarbon exposure risks, toxicity mechanisms, and clinical management protocols is essential for providing safe, evidence-based patient care.
Key Learning Objectives
- Identify different types of hydrocarbon compounds and their clinical significance
- Recognize signs and symptoms of hydrocarbon toxicity
- Implement appropriate nursing interventions for hydrocarbon exposure
- Apply safety protocols to prevent hydrocarbon-related incidents
Clinical Pearl
The volatility of a hydrocarbon determines its potential for inhalation toxicity. Highly volatile compounds like gasoline pose greater respiratory risks than less volatile substances like motor oil.
Hydrocarbon Classification System
Understanding the classification of hydrocarbon compounds is crucial for nursing professionals to assess toxicity potential and implement appropriate care protocols. Each hydrocarbon category presents unique clinical challenges and requires specific management approaches.
Aliphatic Hydrocarbons
Straight or branched chain compounds without aromatic rings.
Aromatic Hydrocarbons
Ring structures with delocalized electrons.
| Hydrocarbon Type | Common Examples | Clinical Significance | Toxicity Level |
|---|---|---|---|
| Petroleum Distillates | Gasoline, Kerosene, Turpentine | High aspiration risk | High |
| Heavy Hydrocarbons | Motor oil, Tar, Asphalt | Low volatility, minimal systemic toxicity | Low |
| Aromatic Compounds | Benzene, Toluene, Xylene | CNS depression, carcinogenic potential | Moderate-High |
| Halogenated Compounds | Carbon tetrachloride, Chloroform | Hepatotoxic, nephrotoxic | High |
Clinical Significance in Nursing Practice
The clinical significance of hydrocarbon exposure extends beyond acute toxicity cases. Nurses encounter hydrocarbon-related health issues in emergency departments, occupational health settings, and community care environments.
Respiratory System
- • Chemical pneumonitis
- • Pulmonary edema
- • Respiratory depression
- • Aspiration pneumonia
Neurological System
- • CNS depression
- • Confusion and disorientation
- • Seizures
- • Peripheral neuropathy
Cardiovascular System
- • Cardiac arrhythmias
- • Myocardial sensitization
- • Hypotension
- • Sudden cardiac death
Critical Safety Alert
Never induce vomiting in patients with suspected hydrocarbon ingestion due to high aspiration risk. The low surface tension of many hydrocarbon compounds makes them extremely dangerous if aspirated into the lungs.
Toxicology and Pathophysiology
Understanding the toxicological properties of hydrocarbon compounds enables nurses to anticipate clinical presentations and implement timely interventions. The toxicity of each hydrocarbon depends on its chemical structure, volatility, and route of exposure.
Mechanisms of Toxicity
Direct Cellular Damage
Lipophilic nature of hydrocarbon compounds allows penetration of cell membranes, disrupting membrane integrity and cellular function.
Aspiration Pneumonitis
Low viscosity and surface tension facilitate deep lung penetration, causing chemical burns and inflammatory response.
CNS Depression
Interference with neurotransmitter function and membrane stability leads to altered consciousness and respiratory depression.
Temporal Progression
Mucosal irritation, burning sensation, early respiratory symptoms
CNS effects, pulmonary edema development, cardiac sensitization
Chemical pneumonitis, ARDS, multi-organ dysfunction
Secondary complications, organ failure, recovery phase
Dose-Response Relationship
The toxic effects of hydrocarbon exposure follow a predictable dose-response pattern, with severity correlating to concentration, duration, and individual susceptibility factors.
Routes of Hydrocarbon Exposure
Nurses must understand all potential routes of hydrocarbon exposure to conduct thorough assessments and implement appropriate protective measures. Each exposure route presents unique clinical challenges and requires specific nursing interventions.
Inhalation
Most common route in occupational settings
Ingestion
Accidental or intentional consumption
Dermal
Skin contact and absorption
Ocular
Eye contact and splash injuries
| Exposure Route | Common Scenarios | Clinical Manifestations | Priority Interventions |
|---|---|---|---|
| Inhalation |
• Occupational exposure • Enclosed space accidents • Intentional abuse |
• Respiratory irritation • CNS depression • Pulmonary edema |
• Remove from exposure • Oxygen therapy • Monitor respiratory status |
| Ingestion |
• Accidental ingestion • Suicide attempts • Child poisoning |
• GI irritation • Aspiration risk • Systemic toxicity |
• DO NOT induce vomiting • Supportive care • Monitor for aspiration |
| Dermal |
• Workplace spills • Cleaning activities • Fuel handling |
• Skin irritation • Contact dermatitis • Systemic absorption |
• Remove contaminated clothing • Copious irrigation • Assess for burns |
| Ocular |
• Splash injuries • Vapor exposure • Transfer from hands |
• Eye irritation • Corneal damage • Vision changes |
• Immediate irrigation • Ophthalmologic evaluation • Pain management |
Comprehensive Nursing Assessment
A systematic nursing assessment for suspected hydrocarbon exposure requires careful evaluation of multiple body systems. The assessment must be rapid yet thorough, as hydrocarbon toxicity can progress quickly from mild symptoms to life-threatening complications.
Primary Assessment (ABCDE)
A Airway
- • Assess patency and protection
- • Monitor for laryngeal edema
- • Evaluate gag reflex
B Breathing
- • Respiratory rate and pattern
- • Oxygen saturation
- • Adventitious lung sounds
C Circulation
- • Blood pressure and pulse
- • Cardiac rhythm monitoring
- • Perfusion assessment
Secondary Assessment
Neurological Assessment
- • Glasgow Coma Scale
- • Pupil response
- • Motor function
- • Coordination testing
Gastrointestinal Assessment
- • Nausea and vomiting
- • Abdominal pain
- • Bowel sounds
- • Hydrocarbon odor on breath
Integumentary Assessment
- • Skin color and temperature
- • Evidence of contact burns
- • Moisture and turgor
- • Presence of hydrocarbon residue
Assessment Clinical Pearl
The characteristic hydrocarbon odor on the patient’s breath or clothing can provide valuable diagnostic information. However, absence of odor does not rule out exposure, as some compounds are odorless or the sense of smell may be impaired.
Red Flag Symptoms Requiring Immediate Intervention
Respiratory
- • Severe dyspnea or stridor
- • Frothy sputum production
- • Oxygen saturation <90%
Neurological
- • Altered level of consciousness
- • Seizure activity
- • Focal neurological deficits
Evidence-Based Management Protocols
Effective management of hydrocarbon exposure requires prompt recognition, appropriate decontamination, and supportive care. The primary goal is preventing further absorption while managing complications. Unlike many poisonings, hydrocarbon exposure management focuses heavily on supportive care rather than specific antidotes.
Immediate Interventions
Decontamination Priority
- Remove patient from contaminated environment
- Remove contaminated clothing and jewelry
- Irrigate skin with copious amounts of water
- Avoid inducing vomiting (contraindicated)
Respiratory Support
- • Administer high-flow oxygen
- • Monitor oxygen saturation continuously
- • Prepare for mechanical ventilation if needed
- • Consider bronchodilators for bronchospasm
Ongoing Management
Cardiovascular Monitoring
- • Continuous cardiac monitoring
- • Serial blood pressure measurements
- • Avoid epinephrine (sensitization risk)
- • Fluid resuscitation as needed
Neurological Support
- • Frequent neurological assessments
- • Seizure precautions
- • Benzodiazepines for agitation
- • Avoid stimulants
| Clinical Scenario | Priority Actions | Contraindications | Monitoring Parameters |
|---|---|---|---|
| Inhalation Exposure |
• Remove from source • High-flow oxygen • Bronchodilators PRN |
• Avoid positive pressure until assessed |
• Oxygen saturation • Chest X-ray • ABGs |
| Ingestion |
• Do NOT induce vomiting • Activated charcoal (limited use) • Supportive care |
• Gastric lavage • Ipecac syrup • Cathartics |
• Aspiration signs • Neurological status • GI symptoms |
| Dermal Contact |
• Remove clothing • Copious water irrigation • Mild soap if available |
• Scrubbing or abrading skin • Chemical neutralizers |
• Skin integrity • Systemic absorption signs • Local irritation |
Critical Management Contraindications
Never Perform:
- • Induced vomiting (aspiration risk)
- • Gastric lavage (unless massive ingestion)
- • Use of epinephrine (cardiac sensitization)
Use Caution With:
- • Positive pressure ventilation initially
- • Activated charcoal (limited benefit)
- • Sympathomimetic drugs
Comprehensive Safety Protocols
Prevention remains the most effective strategy for managing hydrocarbon exposure. Healthcare facilities must implement robust safety protocols to protect patients, staff, and visitors from accidental hydrocarbon exposure while maintaining therapeutic effectiveness when these compounds are medically necessary.
Personal Protective Equipment
- Chemical-resistant gloves
- Eye protection/face shields
- Respiratory protection (NIOSH approved)
- Chemical-resistant aprons
Engineering Controls
- Adequate ventilation systems
- Emergency shower/eyewash stations
- Spill containment materials
- Fire suppression systems
Administrative Controls
- Staff training programs
- Exposure monitoring protocols
- Emergency response procedures
- Regular safety audits
Emergency Response Protocol
Immediate Response (First 5 minutes)
- Ensure personal safety – assess scene
- Remove patient from hydrocarbon source
- Call for emergency assistance
- Begin decontamination procedures
- Assess airway, breathing, circulation
Continuing Care (First hour)
- Maintain continuous monitoring
- Administer supportive care
- Document exposure details
- Contact poison control center
- Prepare for potential complications
Safety Clinical Pearl
When managing hydrocarbon exposure, the healthcare team’s safety is paramount. Never enter a contaminated area without proper PPE, and always ensure adequate ventilation before beginning patient care activities.
Memory Aids and Mnemonics
Effective mnemonics help nursing students and professionals remember critical information about hydrocarbon exposure management. These memory aids are designed to be practical and easily recalled during high-stress clinical situations.
FLAMES
Assessment Mnemonic for Hydrocarbon Exposure
NO VOMIT
Management Contraindications
SIGHT
Signs of Hydrocarbon Toxicity
- Skin irritation or burns
- Inhalation difficulties
- Gastrointestinal symptoms
- Headache and dizziness
- Tachycardia or arrhythmias
RAPID
Routes of Exposure
- Respiratory (inhalation)
- Absorption (dermal)
- Peroral (ingestion)
- Injection (rare, accidental)
- Direct contact (eyes, mucosa)
SAFE
Safety Protocol Steps
- Secure scene safety first
- Assess exposure source
- Follow decontamination protocol
- Evaluate and monitor patient
Global Best Practices and Innovations
Healthcare systems worldwide have developed innovative approaches to hydrocarbon exposure prevention and management. These evidence-based practices represent the current gold standard for hydrocarbon safety in healthcare environments.
Netherlands – Integrated Safety Model
Dutch healthcare facilities implement a comprehensive hydrocarbon safety program combining predictive analytics, real-time monitoring, and staff education.
Key Features:
- • Automated air quality monitoring systems
- • Predictive exposure modeling
- • Mandatory annual competency assessments
- • Integration with electronic health records
Singapore – Technology-Enhanced Response
Singapore’s healthcare system utilizes artificial intelligence and mobile technology to enhance hydrocarbon exposure response times and treatment accuracy.
Innovations:
- • AI-powered symptom recognition
- • Mobile decontamination units
- • Real-time toxicology consultation
- • Wearable exposure monitoring devices
Canada
Multi-disciplinary team approach
Germany
Research-driven protocols
Japan
Precision medicine approach
International Consensus Recommendations
Prevention Strategies
- Implement comprehensive staff training programs covering hydrocarbon safety
- Establish regular environmental monitoring protocols
- Maintain updated emergency response procedures
Treatment Excellence
- Standardize assessment tools across all clinical areas
- Integrate poison control consultation protocols
- Develop long-term follow-up care pathways
Conclusion and Key Takeaways
Mastery of hydrocarbon knowledge represents a critical competency for modern nursing practice. As healthcare environments become increasingly complex, nurses must maintain current knowledge of hydrocarbon safety, assessment techniques, and evidence-based management protocols to ensure optimal patient outcomes and workplace safety.
Essential Knowledge Points
- • Hydrocarbon toxicity varies significantly by compound type and exposure route
- • Prevention of vomiting is crucial to avoid aspiration pneumonia
- • Supportive care remains the cornerstone of treatment
- • Early recognition and intervention improve patient outcomes
Clinical Practice Applications
- • Implement systematic assessment protocols
- • Maintain current knowledge of safety procedures
- • Develop competency in emergency response
- • Advocate for comprehensive workplace safety measures
Final Clinical Pearl
Remember that every hydrocarbon exposure case is unique. While protocols provide essential guidance, clinical judgment, continuous assessment, and collaborative care remain fundamental to achieving positive patient outcomes.
Continuing Education
Stay current with evolving hydrocarbon research, safety protocols, and clinical guidelines through professional development activities, peer consultation, and evidence-based practice initiatives.
