Hyperemesis Gravidarum
Comprehensive Nursing Notes
Table of Contents
Introduction
Hyperemesis gravidarum (HG) is a severe form of nausea and vomiting that occurs during pregnancy. While morning sickness affects up to 80% of pregnant women, hyperemesis gravidarum is a more serious condition that affects approximately 0.3-3% of pregnancies. This condition is characterized by persistent vomiting, dehydration, weight loss of more than 5% of pre-pregnancy body weight, and electrolyte imbalances.
As nursing professionals, understanding the pathophysiology, clinical manifestations, and evidence-based interventions for hyperemesis gravidarum is crucial for providing quality care to affected patients. This condition can significantly impact the pregnant woman’s quality of life and potentially lead to serious complications if not managed appropriately.
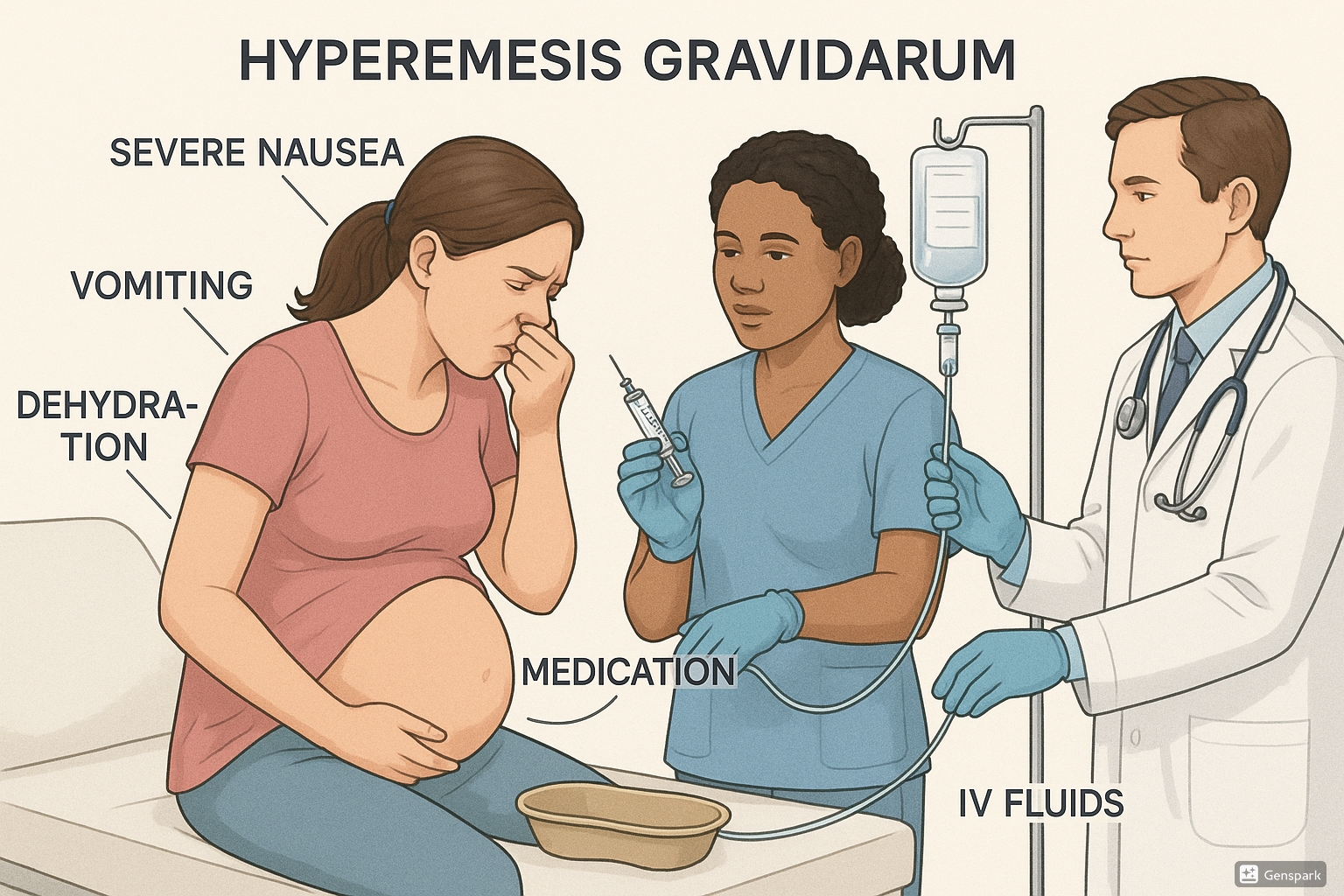
Illustration of hyperemesis gravidarum showing symptoms and treatment approaches
Pathophysiology
The exact cause of hyperemesis gravidarum remains unclear, but several physiological mechanisms have been proposed. Understanding these mechanisms is vital for developing effective nursing interventions.
Hormonal Factors
- Human Chorionic Gonadotropin (hCG): Elevated levels of hCG, which peak during the first trimester when hyperemesis gravidarum is most common, are associated with increased nausea and vomiting.
- Estrogen: High estrogen levels can slow gastric emptying and may contribute to nausea and vomiting.
- Growth and Differentiation Factor 15 (GDF15): Recent research suggests GDF15 produced by the placenta may be the most likely cause of hyperemesis gravidarum.
- Progesterone: Increased progesterone levels relax smooth muscle, potentially slowing gastric emptying.
Gastrointestinal Changes
- Decreased Lower Esophageal Sphincter Pressure: Makes reflux and subsequent nausea more likely.
- Delayed Gastric Emptying: Extends the time food remains in the stomach, increasing risk of nausea.
- Gastric Dysrhythmias: Abnormal electrical rhythms in the stomach contribute to nausea.
Other Proposed Mechanisms
- Thyroid Dysfunction: Transient hyperthyroidism may occur with hyperemesis gravidarum.
- Helicobacter pylori infection: May contribute to symptoms in some cases.
- Genetic Predisposition: Family history and repeat occurrences suggest genetic factors.
- Psychological Factors: While not causative, psychological stressors may exacerbate symptoms.
Important Note:
Hyperemesis gravidarum is a physiological condition with real biological causes, not a psychological disorder. Healthcare providers should avoid suggesting that symptoms are “all in the patient’s head,” which can be dismissive and harmful.
Clinical Manifestations
The clinical presentation of hyperemesis gravidarum includes a range of symptoms that distinguish it from normal morning sickness in pregnancy.
| Key Feature | Morning Sickness | Hyperemesis Gravidarum |
|---|---|---|
| Severity of Nausea | Mild to moderate | Severe, persistent, debilitating |
| Vomiting Frequency | Occasional | Multiple times daily (often >3 times/day) |
| Weight Loss | None or minimal | ≥5% of pre-pregnancy weight |
| Dehydration | Uncommon | Common |
| Electrolyte Imbalances | Rare | Common |
| Ketosis/Ketonuria | Absent | Present |
| Duration | Usually resolves by 12-14 weeks | May persist past 20 weeks or throughout pregnancy |
| Impact on Daily Life | Minimal to moderate | Severe, often prevents normal activities |
Primary Symptoms
Gastrointestinal
- Persistent, severe nausea
- Frequent vomiting (>3 times/day)
- Inability to tolerate food or fluids
- Ptyalism (excessive salivation)
- Bile-stained or bloody vomitus
Hydration Status
- Decreased skin turgor
- Dry mucous membranes
- Decreased urine output
- Dark, concentrated urine
- Extreme thirst
Secondary Symptoms and Signs
Metabolic
- Significant weight loss
- Ketonuria
- Electrolyte imbalances
- Metabolic alkalosis (from loss of HCl in vomit)
- Hypokalemia
Cardiovascular
- Orthostatic hypotension
- Tachycardia
- Weakness and fatigue
- Poor tissue perfusion
Neurological/Psychological
- Headaches
- Lethargy
- Confusion (in severe cases)
- Depression or anxiety related to chronic illness
- Insomnia
Clinical Pearls:
The persistence and severity of symptoms distinguish hyperemesis gravidarum from normal morning sickness. Patient reports of being unable to perform normal daily activities due to nausea and vomiting should raise clinical suspicion for HG, especially when accompanied by weight loss and dehydration.
Diagnosis
The diagnosis of hyperemesis gravidarum is primarily clinical, based on the patient’s history and presenting symptoms, supported by laboratory findings.
Diagnostic Criteria
A diagnosis of hyperemesis gravidarum typically requires:
- Persistent nausea and vomiting during pregnancy
- Weight loss exceeding 5% of pre-pregnancy weight
- Dehydration
- Electrolyte imbalances
- Ketonuria
- Exclusion of other causes of nausea and vomiting
Assessment Tools
PUQE Score (Pregnancy-Unique Quantification of Emesis)
The PUQE score can help quantify the severity of nausea and vomiting in pregnancy:
- Mild: score ≤6
- Moderate: score 7-12
- Severe: score ≥13
The score is based on three questions about duration of nausea, frequency of vomiting, and frequency of retching over the past 24 hours.
Laboratory Studies
| Test | Expected Findings in HG | Clinical Significance |
|---|---|---|
| Urinalysis | Ketonuria, increased specific gravity | Indicates ketosis from starvation state and dehydration |
| Complete Blood Count | Increased hematocrit (concentration effect), possible leukocytosis | Reflects hemoconcentration due to fluid loss |
| Comprehensive Metabolic Panel | Electrolyte abnormalities (hypokalemia, hyponatremia, hypochloremia) | Indicates severity and guides rehydration therapy |
| Liver Function Tests | Mildly elevated transaminases | May occur in up to 50% of patients with HG |
| Thyroid Function Tests | Possible transient hyperthyroidism | May be related to thyroid stimulation by hCG |
| Amylase/Lipase | May be elevated | To rule out pancreatitis |
Additional Studies
First-Line Studies
- Urine ketones (dipstick)
- Urine specific gravity
- Serum electrolytes
- BUN/Creatinine
- Liver enzymes
As Indicated
- Abdominal ultrasound (to rule out other pathologies)
- Thyroid function tests
- H. pylori testing
- Upper endoscopy (in refractory cases)
Nursing Considerations:
When collecting laboratory specimens from patients with suspected hyperemesis gravidarum, consider the patient’s comfort. If nausea is triggered by smells or movements, minimize these triggers during blood draws. For urine collection, ensure the patient is well-supported to prevent falls if weakness or dizziness is present.
Differential Diagnosis
While hyperemesis gravidarum is a diagnosis of exclusion, several other conditions must be considered, especially when symptoms are atypical or refractory to treatment.
| Category | Conditions to Consider | Distinguishing Features |
|---|---|---|
| Gastrointestinal |
|
Often accompanied by pain, fever; may not correlate with pregnancy timing |
| Hepatobiliary |
|
More significant liver function abnormalities; HELLP and acute fatty liver typically occur later in pregnancy |
| Endocrine |
|
Additional endocrine symptoms; abnormal hormone levels beyond pregnancy expectations |
| Genitourinary |
|
Typically accompanied by flank pain, dysuria; abnormal urinalysis findings |
| Neurological |
|
Headache, visual changes, neurological symptoms predominate |
| Pregnancy-related |
|
Ultrasound findings; extremely elevated hCG levels |
Clinical Pearls:
The onset of severe symptoms after 9-10 weeks of pregnancy or the appearance of new symptoms like abdominal pain, fever, or headache should raise suspicion for alternative diagnoses beyond hyperemesis gravidarum.
Management & Treatment
The management of hyperemesis gravidarum follows a stepwise approach, beginning with conservative measures and escalating to pharmacological interventions as needed. The primary goals are to relieve symptoms, correct fluid and electrolyte imbalances, ensure adequate nutrition, and prevent complications.
Non-Pharmacological Management
Dietary Modifications
- Small, frequent meals (every 2-3 hours)
- Dry, bland foods (crackers, toast)
- Avoidance of fatty, spicy, or triggering foods
- Cold foods (may have less aroma)
- Separate liquid and solid intake
- High-protein snacks
Lifestyle Modifications
- Rest (fatigue can worsen nausea)
- Avoidance of sensory triggers
- Fresh air/ventilation
- Acupressure wristbands
- Oral hygiene after vomiting
- Stress reduction techniques
Hydration and Nutritional Support
Oral Rehydration
- Small, frequent sips of clear fluids
- Electrolyte-containing beverages
- Ice chips or popsicles
- Avoidance of carbonated drinks
Intravenous Therapy (if needed)
- Isotonic fluids (typically normal saline)
- Electrolyte replacement as indicated
- Dextrose if ketosis present
- Thiamine supplementation (prior to glucose)
Nutritional Considerations
- Vitamin supplements (especially B6, B12, folate)
- Prenatal vitamins (may need liquid or alternate forms)
- Enteral nutrition (in severe cases)
- Total parenteral nutrition (rarely needed)
Pharmacological Management
Medications are introduced in a stepwise approach, starting with safer options and progressing as needed:
| Treatment Level | Medications | Nursing Considerations |
|---|---|---|
| First-Line |
|
Generally considered safe in pregnancy; monitor for drowsiness with doxylamine |
| Second-Line |
|
Monitor for sedation and extrapyramidal symptoms; avoid prolonged use of metoclopramide |
| Third-Line |
|
Use with caution; monitor for QT prolongation with ondansetron; limit steroid course duration |
| Additional Supportive Therapies |
|
Acid suppressants may help with reflux symptoms; thiamine prevents Wernicke’s encephalopathy |
Hospitalization Criteria
Consider hospitalization for patients with hyperemesis gravidarum when:
- Unable to maintain oral hydration
- Weight loss >5% of pre-pregnancy weight
- Electrolyte abnormalities
- Significant ketonuria
- Failure of outpatient management
Important Medication Note:
Always verify current pregnancy safety categories and recommendations before administering any medication to pregnant patients. The benefit of treating hyperemesis gravidarum must outweigh potential risks, and the lowest effective dose should be used for the shortest necessary duration.
Nursing Care & Interventions
Nursing care for patients with hyperemesis gravidarum focuses on assessment, symptom management, providing comfort measures, and preventing complications.
Nursing Assessment
Physical Assessment
- Vital signs (orthostatic changes)
- Weight (compare to pre-pregnancy)
- Skin turgor and mucous membranes
- Intake and output
- Urine ketones and specific gravity
- Signs of Mallory-Weiss tears (hematemesis)
Psychosocial Assessment
- Impact on daily functioning
- Support systems
- Emotional response to illness
- Coping strategies
- Concerns about pregnancy/fetus
- Financial and work-related concerns
Nursing Diagnoses & Care Plans
1. Deficient Fluid Volume related to excessive vomiting as evidenced by decreased urine output, dry mucous membranes, and poor skin turgor
Expected Outcomes:
- Patient will maintain adequate hydration as evidenced by normal skin turgor, moist mucous membranes, and urine output >0.5 mL/kg/hr.
- Patient will demonstrate stable vital signs without orthostatic changes.
Nursing Interventions:
- Monitor intake and output strictly; document all emesis.
- Administer IV fluids as ordered, ensuring correct rate and type.
- Assess vital signs, including orthostatic measurements, every 4 hours.
- Monitor daily weights and trends.
- Assess for signs of dehydration at each shift (skin turgor, mucous membranes, etc.).
- Encourage small amounts of oral fluids as tolerated.
- Monitor urine specific gravity and ketones.
- Position patient to prevent aspiration during vomiting episodes.
2. Imbalanced Nutrition: Less than Body Requirements related to inability to ingest or digest food as evidenced by weight loss and persistent vomiting
Expected Outcomes:
- Patient will demonstrate stabilization or improvement in weight.
- Patient will tolerate small, frequent meals without vomiting.
- Patient will maintain adequate caloric intake for pregnancy needs.
Nursing Interventions:
- Collaborate with dietitian to develop an individualized nutrition plan.
- Offer small, frequent meals of patient-preferred foods.
- Provide cold foods that may have less aroma.
- Remove food trays promptly after meals to reduce nausea triggers.
- Administer antiemetics as ordered, timing them before meals.
- Monitor laboratory values for nutritional deficiencies.
- Document food tolerance and patterns of nausea/vomiting.
- Implement nutritional supplementation as ordered (vitamins, enteral nutrition).
3. Acute Pain related to esophageal irritation and abdominal muscle strain as evidenced by verbal reports of epigastric pain and sore throat
Expected Outcomes:
- Patient will report decreased pain using a standardized pain scale.
- Patient will identify and implement non-pharmacological pain management strategies.
Nursing Interventions:
- Assess pain using a standardized scale.
- Administer analgesics as prescribed, evaluating effectiveness.
- Provide oral care after vomiting episodes.
- Apply cool compresses to the forehead or back of neck during acute nausea.
- Teach relaxation techniques for pain management.
- Position patient comfortably to minimize strain.
- Assist with frequent oral rinses to soothe irritated mucosa.
4. Risk for Impaired Skin Integrity related to malnutrition and dehydration
Expected Outcomes:
- Patient will maintain intact skin throughout hospitalization.
- Patient will demonstrate understanding of skin care measures.
Nursing Interventions:
- Assess skin integrity daily, documenting any alterations.
- Implement pressure injury prevention protocol for bed-bound patients.
- Keep skin clean and dry, especially after vomiting episodes.
- Ensure proper oral hygiene to prevent breakdown of oral mucosa.
- Apply lip balm to prevent cracking.
- Encourage mobility as tolerated to prevent pressure injuries.
5. Anxiety related to concerns about maternal and fetal health as evidenced by expressed worry and difficulty coping
Expected Outcomes:
- Patient will verbalize decreased anxiety levels.
- Patient will utilize effective coping strategies.
- Patient will express realistic understanding of condition and its management.
Nursing Interventions:
- Establish therapeutic relationship and provide emotional support.
- Validate patient’s feelings and concerns.
- Provide accurate information about hyperemesis gravidarum and its effects on pregnancy.
- Teach relaxation techniques (deep breathing, guided imagery).
- Include support person(s) in education and care planning.
- Refer to support groups or counseling as needed.
- Coordinate fetal monitoring as appropriate to reassure about fetal wellbeing.
Special Nursing Considerations
IV Therapy Management
- Administer IV fluids at prescribed rate
- Monitor IV site for infiltration or phlebitis
- Document fluid balance accurately
- Ensure thiamine administration before dextrose
- Monitor for refeeding syndrome in malnourished patients
Medication Administration
- Administer antiemetics before meals when possible
- Consider alternative routes (IV, suppository) when oral route not tolerated
- Monitor for medication side effects
- Time medication administration for maximum effectiveness
- Educate on home medication regimen if discharged
Nursing Tip:
Create a calm, low-stimulus environment for patients with hyperemesis gravidarum. Strong smells, bright lights, and noise can trigger or worsen nausea. Even routine healthcare activities like changing bed linens or emptying emesis basins can trigger symptoms, so coordinate care thoughtfully.
Patient Education
Effective patient education is crucial for managing hyperemesis gravidarum and empowering patients to participate in their care, especially since much of the management may occur at home.
Key Educational Topics
Understanding the Condition
- Explain that hyperemesis gravidarum is a medical condition, not a psychological issue
- Discuss the typical course and timeframe
- Reassure that most cases improve by 16-20 weeks (though some persist longer)
- Address concerns about fetal effects
Home Management Strategies
- Dietary modifications and meal planning
- Hydration strategies
- Avoiding identified triggers
- Rest and activity balance
- Symptom tracking methods
Dietary Education
Recommended Dietary Approaches
- Eat before feeling hungry: Empty stomach can worsen nausea
- Small, frequent meals: Every 1-2 hours rather than larger meals
- “BRATT” diet: Bananas, Rice, Applesauce, Toast, Tea (as tolerated)
- Protein-rich snacks: May help stabilize blood sugar
- Separate liquids and solids: Drink fluids between meals, not with meals
- Cold foods: Often better tolerated than hot foods (less aroma)
- Ginger products: Ginger tea, candies, or supplements
Foods/Beverages to Avoid
- Spicy, greasy, or fatty foods
- Strong-smelling foods
- Carbonated beverages
- Caffeine
- Very sweet foods
- Identified personal trigger foods
Medication Education
- Name, purpose, and dosing schedule of prescribed medications
- Proper administration techniques
- Expected effects and timeframe
- Common side effects and management
- When to take medications (often before symptoms occur)
- Importance of not skipping doses
- When to contact healthcare provider about medication concerns
Warning Signs Education
Instruct patients to seek immediate medical attention for:
- Inability to keep down any foods or fluids for 24 hours
- Signs of dehydration (extreme thirst, dark urine, dizziness)
- Weight loss continuing despite treatment
- Vomiting blood
- Fever above 100.4°F (38°C)
- Severe headache or abdominal pain
- Decreased fetal movement (if applicable by gestational age)
Coping Strategies Education
Physical Coping
- Rest in semi-reclined position after meals
- Avoid lying flat for at least 30 minutes after eating
- Fresh air and ventilation
- Acupressure techniques (P6 wrist point)
- Distraction techniques during episodes
Emotional Coping
- Mindfulness and relaxation techniques
- Connecting with support groups
- Communicating needs to family/support persons
- Journaling or tracking symptoms
- Seeking mental health support if needed
Patient Education Tip:
Provide written materials that patients can reference at home. Visual aids like food charts and symptom diaries can be especially helpful for patients with hyperemesis gravidarum. Consider the patient’s energy level when providing education—multiple short sessions may be more effective than one comprehensive session.
Complications
Untreated or inadequately managed hyperemesis gravidarum can lead to various maternal and fetal complications. Nursing professionals should be vigilant for early signs of these complications.
Maternal Complications
Nutritional/Metabolic
- Wernicke’s Encephalopathy: Due to thiamine deficiency; characterized by confusion, ataxia, and ocular abnormalities
- Vitamin Deficiencies: Especially B vitamins, vitamin K
- Malnutrition: With muscular wasting and weakness
- Refeeding Syndrome: When nutrition is reintroduced too quickly
Gastrointestinal
- Mallory-Weiss Tears: Esophageal lacerations from forceful vomiting
- Esophagitis: Inflammation of the esophagus
- Gastric Rupture: Rare but life-threatening
- Dental Erosion: From stomach acid exposure
Cardiovascular/Hematologic
- Hypovolemia: Decreased circulating volume
- Electrolyte Imbalances: Especially hypokalemia, hyponatremia
- Venous Thromboembolism: Due to dehydration and immobility
Psychological
- Depression: Common with prolonged illness
- Anxiety: About maternal and fetal health
- PTSD: May develop after severe HG experience
- Termination of Wanted Pregnancy: In extreme cases due to severe symptoms
Fetal Complications
- Low Birth Weight: Associated with maternal malnutrition
- Preterm Birth: May occur with severe HG
- Small for Gestational Age: Due to poor maternal nutrition
- Neurodevelopmental Effects: Research shows possible links to behavioral and emotional regulation issues in children
Prevention Strategies
- Early intervention and treatment at first signs of severe nausea and vomiting
- Routine thiamine supplementation when IV fluids are initiated
- Regular monitoring of electrolytes and correction of imbalances
- Nutritional support and supplementation
- Psychological support throughout pregnancy
- Close monitoring of weight and hydration status
- Early treatment of any recurrence in subsequent pregnancies
Clinical Alert:
Confusion, abnormal eye movements, or gait disturbances in a patient with hyperemesis gravidarum should raise immediate concern for Wernicke’s encephalopathy. This is a medical emergency requiring immediate thiamine administration.
Mnemonics & Learning Aids
Mnemonics and learning aids can help nursing students remember key aspects of hyperemesis gravidarum assessment and management.
VOMITS
Mnemonic for Hyperemesis Gravidarum Assessment:
- V – Vital signs (assess for tachycardia, hypotension)
- O – Output (measure urine output, assess for dehydration)
- M – Metabolic status (check electrolytes, ketones)
- I – Intake (monitor oral/IV fluid intake, tolerance)
- T – Triggers (identify and avoid nausea triggers)
- S – Support (assess psychological and social support)
MOTHER
Mnemonic for Hyperemesis Gravidarum Management:
- M – Medications (antiemetics, vitamins, etc.)
- O – Oral hygiene (after vomiting episodes)
- T – Thiamine supplementation (prevent Wernicke’s)
- H – Hydration (IV or oral as tolerated)
- E – Electrolyte monitoring and replacement
- R – Rest and relaxation techniques
MEALS
Mnemonic for Dietary Advice in Hyperemesis Gravidarum:
- M – Multiple small meals frequently
- E – Eliminate triggering foods
- A – Avoid strong aromas
- L – Low-fat options preferred
- S – Separate solids and liquids
FLUIDS
Mnemonic for IV Therapy Management in Hyperemesis Gravidarum:
- F – Flow rate (ensure proper administration)
- L – Labs (monitor electrolytes)
- U – Urinary output (maintain >0.5mL/kg/hr)
- I – Infiltration monitoring (check IV site)
- D – Documentation of intake/output
- S – Supplements (vitamins, especially B1 before glucose)
Key Differentials
| Condition | Morning Sickness | Hyperemesis Gravidarum |
|---|---|---|
| Nausea Duration | Intermittent | Persistent, severe |
| Vomiting | Occasional | Frequent (>3 times/day) |
| Weight | Stable or slight decrease | Loss ≥5% of pre-pregnancy weight |
| Ketones | Absent | Present |
| Electrolytes | Normal | Abnormal |
| Medical Intervention | Rarely needed | Often required |
Study Tip:
Create flashcards with the mnemonics and key differentials for quick review. Practice explaining the pathophysiology of hyperemesis gravidarum to a colleague or study partner to reinforce your understanding.
Global Best Practices
Different healthcare systems around the world have developed approaches to managing hyperemesis gravidarum. Among the most advanced are:
United Kingdom
The Royal College of Obstetricians and Gynaecologists publishes clear guidelines for management of HG including early intervention with antiemetics and standardized protocols for when to escalate care. Day units specifically for IV hydration without full hospital admission have shown success.
Australia
Development of multidisciplinary HG teams including obstetricians, nurses, nutritionists, and mental health providers. Implementation of early intervention protocols and home healthcare services for IV hydration to prevent hospital admission.
Scandinavia
Focus on early psychosocial support alongside medical management. Development of specialized clinics with expertise in hyperemesis gravidarum. Emphasis on education about nutritional strategies and use of complementary therapies alongside conventional treatments.
Summary
Hyperemesis gravidarum is a severe form of pregnancy-related nausea and vomiting that affects 0.3-3% of pregnancies. It is characterized by persistent vomiting, weight loss, dehydration, and electrolyte imbalances.
The pathophysiology likely involves hormonal factors (particularly hCG and GDF15), gastrointestinal changes, and possibly genetic predisposition. Management requires a multi-faceted approach including hydration therapy, antiemetic medications, nutritional support, and psychosocial care.
Nursing care focuses on assessment, monitoring for complications, administering prescribed therapies, providing comfort measures, and patient education. Key nursing diagnoses include deficient fluid volume, imbalanced nutrition, and anxiety.
Without adequate treatment, hyperemesis gravidarum can lead to serious complications including Wernicke’s encephalopathy, malnutrition, and psychological distress. With proper management, most patients can have successful pregnancy outcomes despite this challenging condition.
