Comprehensive Guide to Hypothermia for Nursing Students
Evidence-based approaches to understanding, assessing, and managing hypothermia across all age groups
Table of Contents
Introduction to Hypothermia
Hypothermia is defined as a core body temperature below 35°C (95°F). It represents a state where the body loses heat faster than it can produce it, leading to a failure in maintaining normal body temperature. Hypothermia is a medical emergency that requires prompt recognition and intervention to prevent significant morbidity and mortality.
Key Points:
- Hypothermia occurs when core body temperature falls below 35°C (95°F)
- It results from imbalance between heat production and heat loss
- Can be accidental (environmental exposure) or therapeutic (intentionally induced)
- Presents unique challenges in different age groups, especially neonates and elderly
- Requires early recognition and appropriate interventions to prevent complications
As nursing professionals, understanding the pathophysiology, recognition, and management of hypothermia is crucial for providing evidence-based care and improving patient outcomes. This guide provides comprehensive information on hypothermia with special emphasis on vulnerable populations like neonates and elderly patients.
Pathophysiology of Hypothermia
Normal Thermoregulation
Human thermoregulation is a complex process controlled primarily by the hypothalamus, which acts as the body’s thermostat. The preoptic anterior hypothalamus contains temperature-sensitive neurons that respond to changes in blood temperature and signals from peripheral temperature receptors.
Thermoregulatory Mechanisms:
- Heat Production: Primarily through:
- Basal metabolic processes
- Voluntary muscle activity
- Involuntary muscle activity (shivering)
- Non-shivering thermogenesis (brown fat metabolism in neonates)
- Heat Conservation: Through:
- Peripheral vasoconstriction
- Behavioral responses (seeking warmth, curling up)
- Horripilation (goosebumps)
Mechanisms of Heat Loss
Understanding the mechanisms of heat loss is crucial for preventing and managing hypothermia. There are five primary mechanisms by which the body loses heat:
| Mechanism | Description | Example | Approximate Percentage |
|---|---|---|---|
| Radiation | Transfer of heat from the body surface to cooler surrounding objects without direct contact | Heat loss to cold room walls even without touching them | 40-45% |
| Conduction | Direct transfer of heat through physical contact with cooler objects | Sitting on cold surfaces, lying on cold ground | 15-20% |
| Convection | Heat loss through movement of air or water across the body surface | Wind chill effect, swimming in cold water | 20-25% |
| Evaporation | Heat loss through conversion of water to vapor | Sweating, wet clothing, respiration | 10-15% |
| Respiration | Heat loss through breathing (warming and humidifying inhaled air) | Breathing cold air, increased respiratory rate | 5-10% |
Pathophysiological Changes in Hypothermia
As core temperature decreases, various physiological processes are affected, leading to system-wide changes:
Cardiovascular Effects:
- Initial tachycardia followed by progressive bradycardia
- Peripheral vasoconstriction increases afterload
- Reduced cardiac output
- ECG changes: J waves (Osborn waves), prolonged PR, QRS, and QT intervals
- Increased risk of arrhythmias (atrial fibrillation, ventricular fibrillation)
- At temperatures below 28°C, risk of asystole increases
Respiratory Effects:
- Initial tachypnea followed by progressive bradypnea
- Decreased respiratory drive
- Bronchorrhea (increased secretions)
- Bronchospasm
- Decreased ciliary function
- Increased risk of aspiration
- Respiratory arrest below 24°C
Neurological Effects:
- Progressive decrease in cerebral blood flow (6-7% per 1°C drop)
- Initial confusion and impaired judgment
- Slurred speech
- Ataxia (incoordination)
- Progressive decrease in level of consciousness
- Loss of reflexes
- Fixed dilated pupils (not reliable indicator of brain death in hypothermia)
- Decreased cerebral oxygen consumption may provide neuroprotection
Metabolic Effects:
- Decreased basal metabolic rate (7-8% per 1°C drop)
- Initial hyperglycemia due to decreased insulin release and action
- Later hypoglycemia due to glycogen depletion
- Metabolic acidosis
- Impaired drug metabolism and clearance
- Cold diuresis leading to hypovolemia
- Electrolyte disturbances (hypokalemia, hypomagnesemia)
Hematological Effects:
- Hemoconcentration due to fluid shifts
- Increased blood viscosity
- Platelet dysfunction and sequestration
- Coagulopathy resembling DIC
- Impaired coagulation enzyme function
- Fibrinolysis
Renal Effects:
- Cold-induced diuresis (“cold diuresis”)
- Decreased renal blood flow
- Decreased glomerular filtration rate
- Impaired tubular function
- Risk of acute kidney injury during rewarming phase
Immunological Effects:
- Impaired leukocyte function and mobility
- Decreased inflammatory response
- Increased susceptibility to infection
- Impaired wound healing
Classification and Stages of Hypothermia
Hypothermia is classified based on the core body temperature. Understanding the different stages is crucial for appropriate assessment and management.
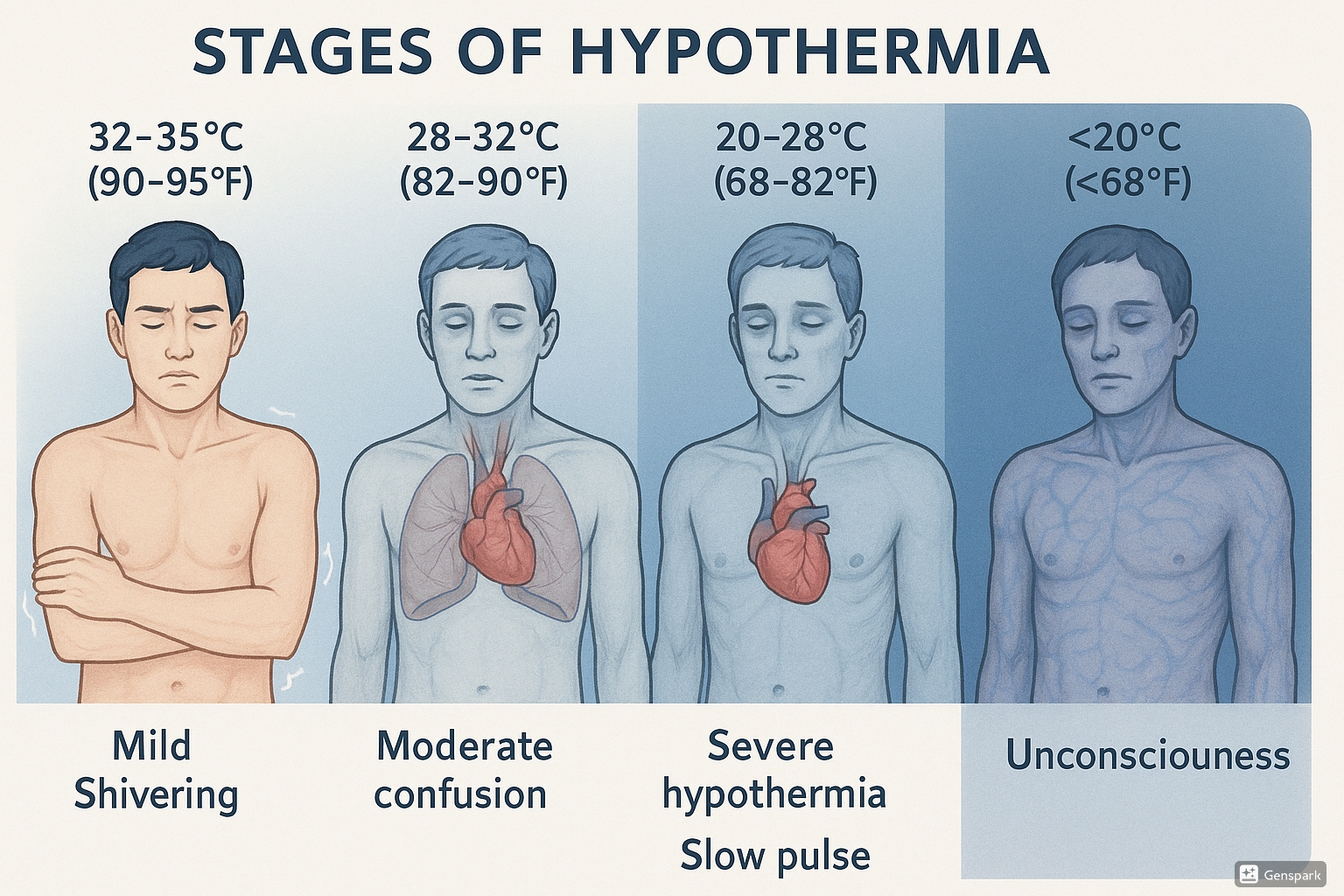
Figure 1: Stages of Hypothermia showing temperature ranges and clinical signs
| Stage | Temperature Range | Level of Consciousness | Shivering | Other Clinical Manifestations |
|---|---|---|---|---|
| Mild Hypothermia | 32-35°C (90-95°F) | Conscious, alert to confused | Present, often intense |
|
| Moderate Hypothermia | 28-32°C (82-90°F) | Decreased level of consciousness, often somnolent | Diminished or absent |
|
| Severe Hypothermia | < 28°C (< 82°F) | Unconscious | Absent |
|
| Profound Hypothermia | < 20°C (< 68°F) | Deep coma | Absent |
|
Mnemonic: “UMBLES” for Early Signs of Hypothermia
- Mumbles – Altered mental status, slurred speech
- Umbles – Poor coordination, stumbling
- Mumbles – Difficulty articulating words
- Bumbles – Poor coordination, clumsiness
- Loss of temperature control – Shivering then no shivering
- Exhaustion – Progressive fatigue
- Stupor – Decreased mental status progressing to unconsciousness
This mnemonic helps healthcare providers remember the progression of symptoms as hypothermia worsens.
Swiss Staging System for Accidental Hypothermia
An alternative classification system used particularly in wilderness and emergency medicine:
- Stage I (HT I): Clear consciousness with shivering (35-32°C)
- Stage II (HT II): Impaired consciousness without shivering (32-28°C)
- Stage III (HT III): Unconsciousness (28-24°C)
- Stage IV (HT IV): Apparent death (below 24°C)
- Stage V (HT V): Death due to irreversible hypothermia (typically below 13.7°C unless special circumstances like cold water submersion)
Risk Factors for Hypothermia
Multiple factors can increase the risk of developing hypothermia. Understanding these risk factors helps in identifying vulnerable populations and implementing preventive measures.
Environmental Factors
- Cold ambient temperatures
- High wind (increases convective heat loss)
- Wet conditions (increases conductive heat loss)
- Cold water immersion (water conducts heat 25 times faster than air)
- Inadequate shelter or clothing
- High altitude (associated with colder temperatures)
Age-Related Factors
- Neonates:
- High surface area to mass ratio
- Limited subcutaneous fat
- Immature thermoregulation
- Limited ability for shivering thermogenesis
- Higher thermal conductance
- Elderly:
- Decreased basal metabolic rate
- Reduced perception of cold
- Decreased vasoconstrictor response
- Reduced shivering capacity
- Less efficient thermoregulation
Medical Conditions
- Endocrine disorders:
- Hypothyroidism
- Hypoadrenalism
- Hypopituitarism
- Diabetes mellitus (impaired vasomotor control)
- Neurological disorders:
- Stroke
- Parkinson’s disease
- Spinal cord injury
- Dementia
- Cardiovascular disorders:
- Heart failure
- Peripheral vascular disease
- Dermatological conditions:
- Extensive burns
- Erythroderma (exfoliative dermatitis)
- Psoriasis
- Other:
- Malnutrition
- Sepsis
- Shock
- Trauma
- Burns
Pharmacological and Substance-Related Factors
- Medications:
- Sedatives and hypnotics
- Antipsychotics
- Anesthetics
- Beta blockers
- Vasodilators
- Phenothiazines
- Barbiturates
- Benzodiazepines
- Opioids
- Substance use:
- Alcohol (causes vasodilation and impairs judgment)
- Recreational drugs (especially those causing altered mental status)
Social and Behavioral Factors
- Homelessness
- Inadequate heating
- Poverty
- Social isolation
- Inability to recognize cold or seek help
- Inappropriate clothing for weather conditions
- Excessive physical exertion leading to exhaustion
- Inadequate fluid and calorie intake during cold exposure
Occupational and Recreational Risk Factors
- Outdoor occupations in cold environments
- Winter sports and recreation
- Mountaineering and high-altitude activities
- Water sports in cold weather
- Military operations in cold environments
- Disaster situations with exposure to elements
High-Risk Vulnerable Populations
The following groups are particularly susceptible to hypothermia and require special attention:
- Neonates and infants
- Elderly individuals, especially those with comorbidities
- Homeless individuals
- People with mental illness or cognitive impairment
- Individuals with substance use disorders
- People with limited mobility
- Individuals with poor nutritional status
- Trauma victims
- People taking multiple medications (polypharmacy)
Assessment of Hypothermia
Accurate assessment of hypothermia is critical for proper diagnosis and management. This includes both history taking and physical examination focused on identifying risk factors, clinical manifestations, and accurate temperature measurement.
History Taking
When assessing a patient with suspected hypothermia, obtain the following information:
- Duration and circumstances of cold exposure
- Environmental conditions (temperature, wind, precipitation)
- Protective measures taken (clothing, shelter)
- Associated trauma or immersion
- Pre-existing medical conditions
- Current medications
- Alcohol or substance use
- Changes in mental status or behavior
- Symptoms experienced (shivering, confusion, weakness)
Physical Examination
Primary Assessment (ABCDE approach)
- Airway: Assess patency, protect if altered mental status
- Breathing: Rate, depth, work of breathing, oxygen saturation
- Circulation: Pulse rate, rhythm, volume; blood pressure; capillary refill; peripheral perfusion
- Disability: Level of consciousness (AVPU or GCS), pupillary responses
- Exposure: Remove wet clothing, examine for associated injuries or frostbite, but minimize exposure to prevent further heat loss
Secondary Assessment
- Vital Signs:
- Core temperature measurement (see techniques below)
- Heart rate (bradycardia is common)
- Blood pressure
- Respiratory rate
- Skin Assessment:
- Color (pale, cyanotic)
- Temperature (cold, especially extremities)
- Presence of frostbite or cold injury
- Neurological Assessment:
- Mental status
- Speech patterns
- Motor function
- Reflexes
Temperature Measurement Techniques
| Method | Accuracy | Advantages | Disadvantages | Recommended Use |
|---|---|---|---|---|
| Rectal | High |
|
|
Clinical setting, moderate to severe hypothermia |
| Esophageal | Very high |
|
|
Critical care, operating room, cardiac arrest |
| Bladder | High |
|
|
ICU setting with existing catheter |
| Tympanic | Moderate |
|
|
Initial screening, mild hypothermia |
| Axillary | Low |
|
|
Screening only, not reliable for hypothermia |
| Epitympanic (deep ear canal) | High |
|
|
Prehospital, wilderness medicine, specialized centers |
Special Considerations in Temperature Assessment
- Use thermometers capable of measuring low temperatures (conventional thermometers may not read below 34-35°C)
- Core temperature monitoring is essential for moderate to severe hypothermia
- For accurate diagnosis, confirm low readings with a second measurement or different method
- In cardiac arrest with suspected hypothermia, temperature measurement is essential before terminating resuscitation efforts
Diagnostic Studies
Laboratory Studies
- CBC: Hemoconcentration is common
- Coagulation studies: PT, PTT may be prolonged
- Electrolytes: Monitor for hypokalemia, hypocalcemia, hypomagnesemia
- Blood glucose: May be elevated initially, then decreased
- BUN/Creatinine: To assess renal function
- Arterial blood gases: Respiratory and metabolic acidosis
- Liver function tests: May show transaminitis with severe hypothermia
- Thyroid function tests: If hypothyroidism is suspected
- Toxicology screen: If substance use suspected
Imaging and Other Studies
- ECG:
- Osborn (J) waves (pathognomonic)
- Prolonged PR, QRS, QT intervals
- Atrial fibrillation or other arrhythmias
- Chest X-ray: To assess for aspiration pneumonia or pulmonary edema
- CT scan: If trauma suspected (particularly head trauma)
- Ultrasound: For cardiac evaluation, especially in severe cases
Mnemonic: “COLD” Assessment Framework
- C – Core temperature measurement (accurate, appropriate method)
- O – Observation of clinical signs and progression
- L – Laboratory and diagnostic testing
- D – Determine severity and initiate appropriate management
Clinical Manifestations of Hypothermia
The clinical presentation of hypothermia varies depending on the severity of temperature drop and affects multiple body systems. Understanding these manifestations is crucial for early recognition and appropriate intervention.
System-Specific Manifestations
Cardiovascular System
- Mild Hypothermia:
- Tachycardia
- Increased blood pressure due to peripheral vasoconstriction
- Increased cardiac output
- Moderate Hypothermia:
- Progressive bradycardia
- Decreased cardiac output
- Atrial fibrillation (common around 30°C)
- Osborn (J) waves on ECG
- Prolonged PR, QRS, and QT intervals
- Severe Hypothermia:
- Severe bradycardia
- Hypotension
- Ventricular arrhythmias (fibrillation, asystole)
- Decreased cardiac contractility
- Decreased response to defibrillation
- Decreased response to cardiac medications
Neurological System
- Mild Hypothermia:
- Confusion, poor judgment
- Memory impairment
- Slurred speech
- Impaired coordination
- Fatigue
- Moderate Hypothermia:
- Progressive decrease in level of consciousness
- Abnormal behavior (paradoxical undressing)
- Ataxia
- Decreased reflexes
- Dilated pupils
- Severe Hypothermia:
- Unconsciousness/coma
- Absent reflexes
- Fixed, dilated pupils (not reliable for brain death diagnosis)
- EEG abnormalities
- Can mimic brain death
Respiratory System
- Mild Hypothermia:
- Tachypnea
- Increased respiratory drive
- Bronchospasm
- Moderate Hypothermia:
- Progressive decrease in respiratory rate
- Decreased respiratory effort
- Decreased cough reflex
- Increased secretions
- Severe Hypothermia:
- Severe bradypnea or apnea
- Pulmonary edema
- High risk for aspiration
- Decreased mucociliary clearance
Renal and Metabolic
- Mild Hypothermia:
- “Cold diuresis” (increased urine output)
- Initial hyperglycemia
- Moderate Hypothermia:
- Decreased glomerular filtration rate
- Decreased tubular function
- Electrolyte imbalances (especially hypokalemia)
- Severe Hypothermia:
- Metabolic acidosis
- Hypoglycemia
- Acute kidney injury
- Pancreatitis
- Severe electrolyte abnormalities
Hematological System
- Mild Hypothermia:
- Hemoconcentration
- Increased blood viscosity
- Moderate Hypothermia:
- Platelet dysfunction
- Impaired coagulation cascade
- Severe Hypothermia:
- Coagulopathy resembling DIC
- Thrombocytopenia
- Fibrinolysis
- Increased bleeding risk
Musculoskeletal System
- Mild Hypothermia:
- Shivering (involuntary muscle contractions)
- Decreased fine motor skills
- Muscle stiffness
- Moderate Hypothermia:
- Cessation of shivering
- Muscle rigidity
- Poor coordination
- Severe Hypothermia:
- Rigor mortis-like stiffness
- Rhabdomyolysis (muscle breakdown)
- Compartment syndrome risk
Unique and Paradoxical Manifestations
Paradoxical Undressing
A phenomenon observed in moderate to severe hypothermia where individuals remove clothing despite being in cold environments. This is thought to result from:
- Cold-induced paralysis of peripheral vasculature
- Return of warm blood to the extremities and trunk
- Sudden sensation of heat
- Irrational behavior due to hypothermia-induced confusion
This clinical sign has forensic importance in cases found partially clothed in cold environments.
Terminal Burrowing (Hide-and-Die Syndrome)
A pre-terminal behavior observed in severe hypothermia where individuals:
- Seek small, enclosed spaces (under beds, behind furniture)
- May appear to be hiding
- Often found in a fetal position
This phenomenon represents a primitive, potentially instinctual behavior that occurs in the late stages of hypothermia.
Clinical Pearl: The Hypothermia Triad
Remember the classic triad of hypothermia:
- Altered mental status (from confusion to coma)
- Bradycardia out of proportion to hemodynamic status
- Cold skin, especially core (trunk, head)
This triad should prompt immediate temperature assessment and management.
Management of Hypothermia
Management of hypothermia follows a systematic approach focused on preventing further heat loss, gradual rewarming based on severity, treating complications, and addressing underlying causes. The approach differs based on the severity of hypothermia and available resources.
Mnemonic: “WARMER” for Hypothermia Management
- W – Warm environment (prevent further heat loss)
- A – Assess core temperature and severity
- R – Rewarming strategy selection based on severity
- M – Monitor vital signs and cardiac rhythm
- E – Evaluate and treat complications
- R – Respiratory and circulatory support as needed
Initial Management (All Patients)
- Prevent further heat loss:
- Remove from cold environment
- Remove wet clothing
- Cover with warm blankets
- Shield from wind and cold surfaces
- Warm the room/environment
- Handle gently:
- Avoid rough handling (risk of triggering arrhythmias)
- Minimize excessive movement
- Transport horizontally if possible
- Assess and monitor:
- Accurate core temperature measurement
- Cardiac monitoring
- Continuous vital sign assessment
- Check blood glucose
- Initial interventions:
- Establish IV access
- Warm IV fluids to 40-42°C (104-108°F) if available
- Administer oxygen, warmed and humidified if possible
- Check glucose and treat hypoglycemia if present
Rewarming Strategies
The approach to rewarming depends on the severity of hypothermia and available resources. There are three main categories of rewarming techniques:
Passive External Rewarming
- Best for: Mild hypothermia (32-35°C)
- Technique:
- Remove wet clothing
- Cover with dry blankets
- Warm environment (room temperature 21-24°C)
- Head covering (prevents heat loss)
- Allow body to rewarm itself through endogenous heat production
- Rate: 0.5-2°C per hour
- Advantages: Safe, low risk of complications, simple
Active External Rewarming
- Best for: Mild to moderate hypothermia (28-32°C) or mild hypothermia with comorbidities
- Techniques:
- Forced air warming blankets
- Heating pads or hot water bottles to torso only
- Radiant heat sources
- Electric blankets
- Warm water immersion (rarely used in clinical settings)
- Rate: 1-2°C per hour
- Cautions: Apply heat to torso only (not extremities) to prevent “afterdrop” phenomenon
Active Internal (Core) Rewarming
- Best for: Severe hypothermia (< 28°C) or hemodynamically unstable patients
- Techniques:
- Warmed IV fluids (40-42°C)
- Warmed, humidified oxygen (42-46°C)
- Peritoneal lavage with warm fluids
- Bladder lavage
- Pleural lavage
- Gastric lavage
- Extracorporeal blood rewarming:
- ECMO (most effective method)
- Hemodialysis
- Continuous arteriovenous/venovenous rewarming
- Rate: Up to 2-4°C per hour with extracorporeal methods
| Severity | Core Temperature | Recommended Rewarming Approach | Target Rewarming Rate | Special Considerations |
|---|---|---|---|---|
| Mild | 32-35°C (90-95°F) | Passive external rewarming; active external rewarming if comorbidities present | 0.5-2°C/hour | Monitor for arrhythmias, check glucose levels |
| Moderate | 28-32°C (82-90°F) | Active external rewarming plus minimally invasive core rewarming (warm IV fluids, warm oxygen) | 1-2°C/hour | Cardiac monitoring essential, risk of arrhythmias during rewarming |
| Severe | < 28°C (< 82°F) | Active internal (core) rewarming; consider extracorporeal methods if available, especially with cardiac instability | 1-2°C/hour; up to 4°C/hour with ECMO | High risk of rewarming shock, manage in ICU setting, consider ECMO for cardiac arrest |
| Profound | < 20°C (< 68°F) | Extracorporeal rewarming (ECMO) | As tolerated with close monitoring | “No one is dead until warm and dead” – continue resuscitation efforts until core temp > 32°C |
Cardiac Arrest in Hypothermia
Management of cardiac arrest in hypothermic patients differs from normothermic cardiac arrest protocols:
- Check pulse for up to 1 minute before starting CPR (bradycardia can be profound)
- If cardiac arrest is confirmed, begin CPR according to standard protocols
- Defibrillation modifications:
- If core temp < 30°C and VF/VT present, deliver one shock
- If unsuccessful, delay further shocks until temperature > 30°C
- Once temperature > 30°C, follow standard ACLS protocols
- Medication considerations:
- Medications may not be effective at temperatures < 30°C
- Consider withholding or increasing intervals between doses until warmer
- Drug metabolism is significantly impaired in severe hypothermia
- Risk of toxic accumulation with repeated doses
- Continue resuscitation until:
- Return of spontaneous circulation, or
- Core temperature reaches >32-35°C with continued asystole despite all measures
Critical Concepts in Hypothermia Resuscitation
“No one is dead until warm and dead”
- Hypothermia has protective effects on the brain due to decreased metabolic demand
- Successful resuscitation has been reported after prolonged cardiac arrest with hypothermia
- Longest reported survival after hypothermic cardiac arrest: 9 hours of CPR with full neurological recovery
Complications During Rewarming
Rewarming Shock
A form of vasodilatory shock that can occur during rewarming from moderate to severe hypothermia:
- Peripheral vasodilation during rewarming without adequate volume
- Increased vascular capacity
- Relative hypovolemia
- Acidosis from returning circulation to cold extremities
- Myocardial depression
Management: Fluid resuscitation, vasopressors if needed, gradual rewarming
Afterdrop Phenomenon
A continued decrease in core temperature that can occur after initiating rewarming:
- Caused by return of cold blood from the periphery to the core
- Can occur with inappropriate external rewarming (extremities before core)
- Can precipitate arrhythmias and worsen acidosis
Prevention: Rewarm the torso first, avoid aggressive extremity warming initially
Rewarming Acidosis
Metabolic acidosis that worsens during rewarming:
- Caused by returning circulation to ischemic tissues
- Washout of lactate and other acid metabolites
- Can precipitate arrhythmias
Management: Monitor pH, cautious use of bicarbonate only if severe acidosis
Other Rewarming Complications
- Arrhythmias during rewarming
- Electrolyte shifts (particularly potassium)
- Pulmonary edema
- Acute respiratory distress syndrome
- Rhabdomyolysis
- Acute kidney injury
- Coagulopathy
- Seizures
- Hypoglycemia
Medication Considerations in Hypothermia
| Medication Category | Considerations | Recommendations |
|---|---|---|
| Resuscitation Drugs (Epinephrine, Amiodarone) | Reduced effectiveness, delayed metabolism, risk of accumulation | Withhold until core temp >30°C or give at increased intervals |
| Sedatives, Analgesics | Prolonged half-life, increased sensitivity | Reduce doses by 50%, increase dosing intervals, titrate carefully |
| Neuromuscular Blockers | Prolonged effect | Avoid if possible; if necessary, use shorter-acting agents |
| Antibiotics | Altered pharmacokinetics, but may be needed for suspected infection | Administer standard doses but consider extended intervals |
| Inotropes/Vasopressors | May be needed for rewarming shock | Use standard doses, titrated to effect |
| Insulin | Reduced effectiveness in hypothermia | Monitor glucose frequently, adjust doses based on response |
Nursing Care for Hypothermic Patients
Nursing care for hypothermic patients requires a systematic approach focused on assessment, monitoring, interventions to support rewarming, prevention of complications, and patient education.
Nursing Assessment
Initial and Ongoing Assessment
- Obtain accurate core temperature measurements using appropriate methods
- Perform comprehensive vital sign assessment:
- Heart rate and rhythm (anticipate bradycardia)
- Blood pressure (may be decreased)
- Respiratory rate and effort
- Oxygen saturation
- Assess level of consciousness using GCS or AVPU scale
- Evaluate skin condition:
- Color (pale, cyanotic)
- Temperature (especially core vs. peripheral)
- Presence of frostbite or other cold injury
- Monitor for shivering (presence indicates mild hypothermia, absence in cold patient suggests moderate-severe hypothermia)
- Assess for associated injuries or comorbidities
Nursing Diagnoses
Priority Nursing Diagnoses
- Hypothermia related to cold exposure or underlying conditions
- Ineffective thermoregulation related to exposure, age extremes, or altered metabolic state
- Risk for decreased cardiac output related to bradycardia and myocardial depression
- Impaired gas exchange related to decreased respiratory drive
- Altered tissue perfusion related to peripheral vasoconstriction
Additional Nursing Diagnoses
- Acute confusion related to cerebral hypoperfusion and hypothermia
- Risk for injury related to altered mental status and impaired coordination
- Imbalanced nutrition: less than body requirements related to increased metabolic demands
- Risk for infection related to immunosuppression
- Risk for impaired skin integrity related to peripheral vasoconstriction and pressure
Nursing Interventions
Immediate Interventions
- Remove wet clothing and dry the patient
- Cover with warmed blankets
- Provide warm environment (room temperature 21-24°C)
- Place insulation between patient and cold surfaces
- Apply head covering to prevent heat loss
- Handle patient gently to prevent arrhythmias
- Position properly to maintain airway
Rewarming Support
- Implement appropriate rewarming strategy based on severity
- Apply warming devices to torso first (not extremities)
- Administer warmed IV fluids (40-42°C) if ordered
- Provide warmed, humidified oxygen
- Prepare equipment for core rewarming procedures if needed
- Monitor core temperature continuously during rewarming
- Target rewarming rate of 0.5-2°C/hour based on severity
Monitoring and Management
- Continuous cardiac monitoring
- Frequent vital sign assessment (every 15-30 minutes)
- Monitor core temperature, preferably continuously
- Evaluate neurological status regularly
- Monitor fluid status and urine output
- Monitor laboratory values:
- Electrolytes
- Blood glucose
- Acid-base status
- Coagulation studies
Complications Prevention
- Implement pressure injury prevention measures:
- Frequent repositioning
- Pressure-relieving surfaces
- Skin assessment
- Monitor for signs of rewarming shock:
- Hypotension
- Tachycardia
- Decreased perfusion
- Observe for arrhythmias during rewarming
- Monitor for respiratory complications
- Maintain glycemic control
- Prevent infection through aseptic technique
Supportive Care
- Maintain adequate hydration:
- IV fluids as ordered
- Warm oral fluids if conscious and able to swallow
- Provide nutritional support:
- High-calorie diet when able to eat
- Warm, sweet beverages if appropriate
- Maintain patient dignity and privacy
- Provide emotional support to patient and family
- Reorient confused patients frequently
Nursing Evaluation
Expected Outcomes
- Core body temperature returns to normal range (36.5-37.5°C)
- Vital signs stabilize within patient’s baseline
- No evidence of arrhythmias or cardiovascular instability
- Mental status returns to baseline
- Normal or improving perfusion in extremities
- No complications from rewarming process
- Underlying causes of hypothermia identified and addressed
- Prevention strategies implemented for future episodes
Documentation
Critical Documentation Elements
- Initial core temperature and method of measurement
- Serial temperature readings during rewarming
- Rewarming method(s) used
- Response to rewarming interventions
- Vital sign trends
- Neurological status assessments
- Fluid intake and output
- Skin assessments, especially of extremities
- Complications and interventions
- Patient/family education provided
Patient and Family Education
Education Topics
- Recognition of early signs and symptoms of hypothermia
- Risk factors specific to the patient
- Preventive measures:
- Appropriate clothing in layers
- Adequate home heating
- Avoiding alcohol in cold environments
- Maintaining adequate nutrition and hydration
- When to seek medical attention
- Community resources for heating assistance if applicable
- Follow-up care requirements
Mnemonic: “ICE COLD” for Hypothermia Nursing Interventions
- I – Insulate patient from cold surfaces
- C – Cover patient with warm, dry blankets
- E – Environment warming (increase room temperature)
- C – Cardiac monitoring continuously
- O – Oxygen administration (warmed and humidified)
- L – Lab values monitoring (glucose, electrolytes)
- D – Documentation of temperature and interventions
Hypothermia in Special Populations
Hypothermia presents unique challenges in certain populations due to physiological differences, risk factors, and management considerations. This section explores considerations for elderly patients and individuals in wilderness or outdoor settings.
Hypothermia in Elderly Patients
Unique Risk Factors in Elderly
- Physiological factors:
- Decreased basal metabolic rate
- Reduced subcutaneous fat
- Impaired vasoconstrictor response
- Decreased perception of cold
- Impaired shivering response
- Medical conditions:
- Cardiovascular disease
- Endocrine disorders (hypothyroidism, diabetes)
- Neurological conditions (stroke, Parkinson’s)
- Malnutrition
- Cognitive impairment
- Medications:
- Sedatives and hypnotics
- Antipsychotics
- Beta-blockers
- Vasodilators
- Polypharmacy
- Social factors:
- Fixed income/poverty
- Social isolation
- Inadequate housing
- Inability to manage thermostat or heating
Clinical Presentation in Elderly
- Often presents atypically:
- May lack classic shivering response
- Confusion may be the only presenting symptom
- Can mimic stroke or sepsis
- Commonly presents with:
- Altered mental status
- Lethargy
- Decreased mobility
- Falls
- Paradoxical “hot” sensation (removing clothing)
- Bradycardia out of proportion to clinical status
- Indoor hypothermia common:
- May occur even at moderate ambient temperatures (18-20°C)
- Often chronic rather than acute
- May be recurrent each winter
Management Considerations in Elderly
- Assessment:
- Consider hypothermia in any elderly with altered mental status, especially in winter
- Use accurate core temperature measurement methods
- Comprehensive evaluation for underlying causes
- Medication review
- Rewarming:
- Gentle, controlled rewarming (0.5-1°C per hour)
- Close cardiac monitoring (higher risk of arrhythmias)
- Cautious fluid administration (higher risk of fluid overload)
- Consider comorbidities during rewarming
- Supportive care:
- Nutritional support
- Careful positioning and skin care
- Early mobilization when appropriate
- Manage underlying medical conditions
Prevention Strategies for Elderly
- Individual measures:
- Maintain home temperature at minimum 20-21°C (68-70°F)
- Layer clothing, including indoors
- Warm head covering (30-40% of body heat lost through head)
- Adequate nutrition and hydration
- Regular movement/activity
- Social support:
- Regular welfare checks during cold weather
- Home energy assistance programs
- Community warming centers
- Social service referrals
- Healthcare system measures:
- Risk assessment during fall/winter months
- Medication review to minimize risk
- Patient education regarding early signs
- Telehealth temperature monitoring for high-risk individuals
Wilderness and Outdoor Hypothermia
Unique Aspects of Wilderness Hypothermia
- Environmental factors:
- Limited resources and equipment
- Delayed evacuation and definitive care
- Continued exposure to elements
- Wet conditions often present
- High altitude considerations (colder temperatures)
- Risk factors:
- Inadequate planning or equipment
- Exhaustion and dehydration
- Injuries limiting mobility
- Wet clothing (immersion or precipitation)
- Wind exposure (wind chill effect)
- Insufficient caloric intake for activity level
Swiss Staging System
Commonly used in wilderness medicine for its simplicity when equipment is limited:
- Stage 1: Conscious and shivering
- Stage 2: Impaired consciousness, not shivering
- Stage 3: Unconscious
- Stage 4: No vital signs
- Stage 5: Death from irreversible hypothermia
This system requires no equipment and allows for field assessment based on clinical presentation.
Field Management of Hypothermia
- Assessment without thermometers:
- Presence/absence of shivering
- Level of consciousness
- Ability to self-care
- Coordination and speech
- Initial management:
- Get patient out of elements (tent, snow shelter, etc.)
- Remove wet clothing
- Insulate from ground
- Add external heat sources if available
- Wrap in dry insulation (sleeping bags, emergency blankets)
- “Burrito wrap” technique (vapor barrier inside insulation)
- Heat sources in field:
- Chemical heat packs (place near major vessels: axilla, groin, neck)
- Warm water bottles (wrapped to prevent burns)
- Body-to-body warming (for mild cases)
- Heated rocks (caution to prevent burns)
- Evacuation decision-making:
- Mild hypothermia with impromptu shelter: may stabilize in field
- Moderate-severe hypothermia: evacuate if possible
- Limited resources, unable to rewarm: evacuate
- Associated trauma or illness: prioritize evacuation
Wilderness Hypothermia Prevention
Remember the mnemonic “COLD”:
- C – Keep clothing Clean (dirty clothing loses insulation value)
- O – Avoid Overheating (sweating leads to evaporative cooling)
- L – Wear clothing Loose and in Layers (trapped air provides insulation)
- D – Keep clothing Dry (wet clothing conducts heat 25x faster than air)
Additional prevention strategies:
- Proper nutrition and hydration (fuel for thermogenesis)
- Recognize early signs of hypothermia in self and others
- Adequate pre-trip planning and equipment
- Understand weather conditions and terrain
- Carry emergency shelter and heat sources
Neonatal Hypothermia
Neonatal hypothermia is a significant health concern, especially in developing countries, and is associated with increased morbidity and mortality. Newborns have unique physiological characteristics that make them particularly vulnerable to hypothermia.
Unique Pathophysiology in Neonates
Thermoregulatory Challenges in Newborns
- High surface area to mass ratio:
- Newborns have approximately 3 times the surface area per unit of body weight compared to adults
- Greater area for heat loss relative to heat-generating tissue
- Limited insulation:
- Minimal subcutaneous fat, especially in preterm infants
- Thin skin with high water content
- Limited capacity to retain heat
- Immature thermoregulation:
- Underdeveloped hypothalamic temperature control
- Limited ability to increase heat production through shivering
- Inefficient peripheral vasoconstriction
- Limited heat production:
- Rely primarily on non-shivering thermogenesis (brown adipose tissue)
- Brown fat may be insufficient in preterm or small-for-gestational-age infants
Heat Loss Mechanisms in Neonates
- Evaporation:
- Wet skin at birth causes rapid evaporative cooling
- Immature skin barrier increases transepidermal water loss
- Can lose 200 kcal/kg/min through evaporation at birth
- Radiation:
- Heat loss to cooler surrounding objects without contact
- Significant in delivery rooms with cold walls, windows
- Conduction:
- Heat transfer to cold surfaces in direct contact
- Cold scales, examination tables, cold hands of caregivers
- Convection:
- Heat loss from air currents across skin surface
- Air conditioning, drafts, movement during transport
Classification of Neonatal Hypothermia
The World Health Organization (WHO) defines and classifies neonatal hypothermia as follows:
| Classification | Temperature Range | Clinical Features | Management Approach |
|---|---|---|---|
| Normal | 36.5-37.5°C (97.7-99.5°F) | Normal activity and feeding | Routine care, prevention |
| Mild Hypothermia (Cold Stress) | 36.0-36.4°C (96.8-97.6°F) | Peripheral vasoconstriction, increased metabolic rate, mild tachypnea | Skin-to-skin contact, warm environment, delay bathing |
| Moderate Hypothermia | 32.0-35.9°C (89.6-96.6°F) | Poor feeding, lethargy, weak cry, decreased activity, cold extremities, central cyanosis | Active external warming, monitoring, feeding support |
| Severe Hypothermia | < 32.0°C (< 89.6°F) | Bradycardia, respiratory depression, poor perfusion, acidosis, coagulopathy, risk of apnea | Immediate medical attention, gradual rewarming, intensive monitoring |
Risk Factors for Neonatal Hypothermia
Infant Factors
- Prematurity:
- Less brown adipose tissue
- Thinner skin with higher water content
- More immature thermoregulation
- Higher surface area to body mass ratio
- Low birth weight (< 2500g):
- Reduced thermal insulation
- Limited glycogen stores
- Intrauterine growth restriction
- Perinatal asphyxia
- Hypoglycemia
- Central nervous system abnormalities
- Congenital anomalies (especially those affecting skin)
Environmental and Care Factors
- Delivery room factors:
- Low ambient temperature (< 25°C)
- Cold surfaces
- Drafts and air conditioning
- Delayed drying after birth
- Care practices:
- Early bathing
- Inadequate drying
- Delayed wrapping
- Delayed skin-to-skin contact
- Separation from mother
- Inadequate covering of head
- Resuscitation:
- Prolonged resuscitation
- Use of cold oxygen
- Exposure during procedures
- Transport-related:
- Unwarmed transport incubator
- Long-distance transport
- Inadequate thermal protection during transport
Maternal Factors
- Maternal hypothermia
- Maternal medications affecting thermoregulation
- Prolonged rupture of membranes
- Maternal illness (sepsis, hemorrhage)
- Emergency cesarean section
Socioeconomic Factors
- Home delivery without trained attendant
- Limited resources for warming
- Low awareness of hypothermia risks
- Cultural practices (early bathing, oil massage)
- Season and climate (winter months)
- Limited access to healthcare facilities
Assessment of Neonatal Hypothermia
Temperature Measurement in Neonates
- Recommended methods:
- Axillary: Most commonly used, accurate enough for clinical decision-making
- Rectal: More accurate for core temperature but risks of perforation
- Skin probe: Continuous monitoring in incubators/warmers
- Timing:
- Immediately after birth
- Upon admission to nursery or NICU
- Every 1-2 hours until stable, then every 3-4 hours
- Before, during, and after transport
- Observation for clinical signs:
- Acrocyanosis (bluish extremities)
- Cold trunk or extremities to touch
- Poor feeding or sucking
- Lethargy or irritability
- Respiratory distress
- Weak cry
Complications of Neonatal Hypothermia
Immediate Complications
- Metabolic:
- Hypoglycemia (increased glucose consumption)
- Metabolic acidosis
- Hypoxia (increased oxygen consumption)
- Respiratory:
- Increased respiratory distress
- Decreased surfactant production
- Pulmonary hypertension
- Apnea episodes
- Cardiovascular:
- Peripheral vasoconstriction
- Hypotension
- Bradycardia
- Poor perfusion
Longer-term Complications
- Infectious:
- Increased susceptibility to sepsis
- Pneumonia
- Necrotizing enterocolitis
- Hematological:
- Coagulopathy
- Thrombocytopenia
- Pulmonary hemorrhage
- Intraventricular hemorrhage (in preterm)
- Growth and development:
- Poor weight gain
- Increased length of hospital stay
- Potential neurodevelopmental impact
- Mortality:
- 2-4 times increased risk of death
- Temperature < 32°C associated with >80% mortality in some settings
Management of Neonatal Hypothermia
Preventive Measures (WHO Warm Chain)
The WHO recommends ten steps to prevent hypothermia in newborns, known as the “warm chain”:
- Warm delivery room (minimum 25-28°C)
- Immediate drying after birth
- Skin-to-skin contact with mother
- Early and exclusive breastfeeding
- Delayed bathing (at least 24 hours after birth)
- Appropriate clothing/bedding
- Mother and baby together (rooming-in)
- Warm transport if required
- Warm resuscitation
- Training and awareness of healthcare workers
Treatment Based on Severity
- Mild hypothermia (36.0-36.4°C):
- Skin-to-skin contact with mother
- Cover baby’s head
- Ensure warm environment
- Early breastfeeding
- Monitor temperature every 30-60 minutes
- Moderate hypothermia (32.0-35.9°C):
- Radiant warmer or incubator
- Warm ambient temperature (26-28°C)
