Hypovolemia: Comprehensive Nursing Notes
Essential Knowledge for Nursing Students
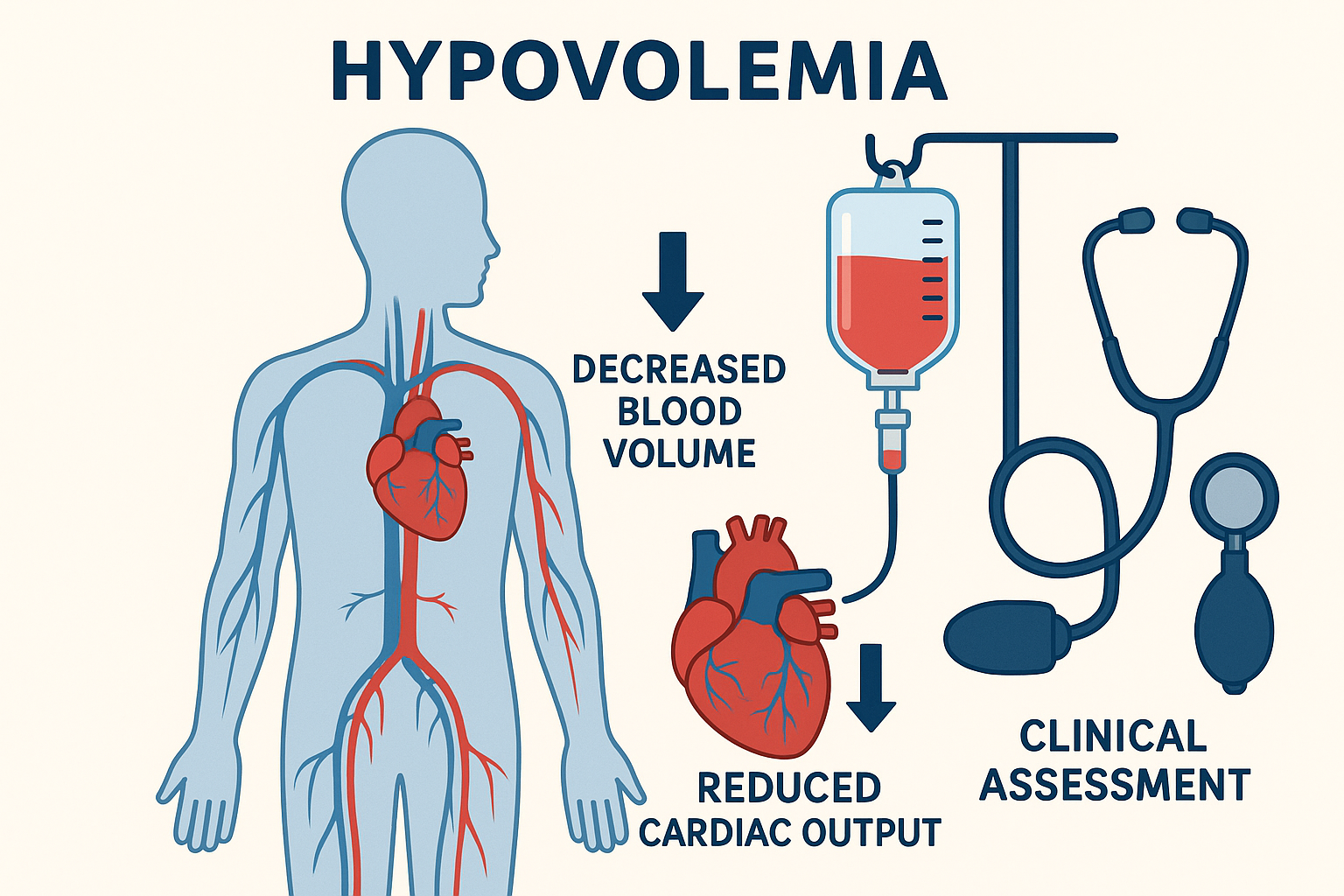
Figure 1: Hypovolemia – Decreased blood volume affecting cardiac output and tissue perfusion
Table of Contents
Definition & Overview
Hypovolemia is a condition characterized by decreased blood volume or extracellular fluid volume that leads to inadequate tissue perfusion and cellular hypoxia. When severe, it progresses to hypovolemic shock, a life-threatening emergency requiring immediate intervention.
Clinical Pearl
Hypovolemia is the most common cause of shock in trauma patients and represents a true medical emergency where “time is tissue.” Early recognition and prompt treatment are crucial for patient survival.
Key Characteristics:
- • Decreased intravascular volume
- • Reduced venous return
- • Decreased cardiac output
- • Inadequate tissue perfusion
- • Cellular hypoxia
Critical Thresholds:
- • Class I: <15% blood volume loss
- • Class II: 15-30% blood volume loss
- • Class III: 30-40% blood volume loss
- • Class IV: >40% blood volume loss
Pathophysiology
Compensatory Mechanisms
The body responds to hypovolemia through several compensatory mechanisms designed to maintain perfusion to vital organs:
Pathophysiological Cascade
Cardiovascular Response
- • Increased heart rate
- • Increased contractility
- • Vasoconstriction
- • Redistribution of blood flow
Neurological Response
- • Sympathetic activation
- • Catecholamine release
- • Baroreceptor stimulation
- • Altered mental status
Renal Response
- • RAAS activation
- • ADH release
- • Sodium retention
- • Oliguria
Mnemonic: “SHOCK”
- Sympathetic activation
- Hypotension develops
- Oliguria occurs
- Compensation fails
- Kidneys shut down
Causes & Risk Factors
Hemorrhagic Causes
- Trauma: Motor vehicle accidents, falls, penetrating injuries
- Surgical: Intraoperative and postoperative bleeding
- Gastrointestinal: Peptic ulcers, varices, diverticulosis
- Obstetric: Postpartum hemorrhage, ectopic pregnancy
- Vascular: Ruptured aneurysms, arterial dissection
- Coagulopathy: Anticoagulant therapy, DIC
Non-Hemorrhagic Causes
- Gastrointestinal: Severe diarrhea, vomiting, fistulas
- Renal: Diuretic use, osmotic diuresis, nephropathy
- Cutaneous: Burns, excessive sweating, wounds
- Third-spacing: Pancreatitis, bowel obstruction
- Endocrine: Diabetes insipidus, adrenal insufficiency
- Environmental: Heat exposure, inadequate intake
Mnemonic: “BLEEDING”
- Blood loss (hemorrhage)
- Loss through GI tract
- Excessive diuresis
- Evaporative losses
- Diarrhea/vomiting
- Inadequate intake
- Nephropathy (salt-wasting)
- Glandular disorders
Clinical Manifestations
Early vs. Late Signs
Clinical presentation varies based on the severity and rate of volume loss. Early recognition is crucial for preventing progression to irreversible shock.
Early Signs (Compensated)
- • Tachycardia (>100 bpm)
- • Normal blood pressure
- • Mild anxiety or restlessness
- • Thirst
- • Fatigue
- • Decreased urine output
- • Cool, pale skin
- • Prolonged capillary refill (>2 seconds)
Late Signs (Decompensated)
- • Hypotension (SBP <90 mmHg)
- • Severe tachycardia (>120 bpm)
- • Altered mental status
- • Oliguria (<0.5 mL/kg/hr)
- • Cold, clammy skin
- • Weak, thready pulse
- • Rapid, shallow breathing
- • Mottled skin
Stages of Hypovolemic Shock
Mnemonic: “FAST PULSE”
- Fatigue and weakness
- Altered mental status
- Skin cool and clammy
- Tachycardia
- Pulse weak and thready
- Urine output decreased
- Low blood pressure
- Shortness of breath
- Eyes sunken, dry mucous membranes
Assessment & Diagnosis
Physical Assessment
- Vital Signs: HR, BP, RR, temperature, O2 sat
- Orthostatic Changes: Drop in BP >20 mmHg systolic
- Skin Assessment: Color, temperature, moisture, turgor
- Capillary Refill: >2 seconds indicates poor perfusion
- Mucous Membranes: Dry, sticky indicates dehydration
- Jugular Venous Distention: Absent in hypovolemia
- Mental Status: Confusion, agitation, lethargy
- Urine Output: <0.5 mL/kg/hr indicates oliguria
Laboratory Studies
- CBC: Hematocrit, hemoglobin levels
- Basic Metabolic Panel: Na+, K+, Cl-, CO2, BUN, creatinine
- Arterial Blood Gas: pH, lactate levels
- Coagulation Studies: PT, PTT, INR
- Urinalysis: Specific gravity, sodium concentration
- Type and Crossmatch: For potential blood transfusion
- Serum Lactate: >2 mmol/L indicates tissue hypoxia
- Base Deficit: Indicates metabolic acidosis
Diagnostic Criteria
Assessment Mnemonic: “VITAL SIGNS”
- Vital signs (orthostatic changes)
- Intake and output monitoring
- Turgor and skin assessment
- Altered mental status
- Laboratory values
- Specific gravity of urine
- Inspection of mucous membranes
- General appearance
- Neurological assessment
- Symptom severity
Classifications of Shock
Hypovolemic Shock
- Mechanism: Decreased blood volume
- Preload: Decreased
- Cardiac Output: Decreased
- SVR: Increased
- PCWP: Decreased
- Example: Hemorrhage, dehydration
Cardiogenic Shock
- Mechanism: Pump failure
- Preload: Increased
- Cardiac Output: Decreased
- SVR: Increased
- PCWP: Increased
- Example: MI, heart failure
Distributive Shock
- Mechanism: Vasodilation
- Preload: Decreased
- Cardiac Output: Increased/Normal
- SVR: Decreased
- PCWP: Decreased
- Example: Sepsis, anaphylaxis
Obstructive Shock
- Mechanism: Mechanical obstruction
- Preload: Decreased
- Cardiac Output: Decreased
- SVR: Increased
- PCWP: Variable
- Example: PE, cardiac tamponade
Medical Management
Treatment Priorities
The primary goals are to restore intravascular volume, maintain tissue perfusion, and address the underlying cause. Treatment must be rapid and aggressive to prevent irreversible organ damage.
Fluid Resuscitation
- Crystalloids: Normal saline or LR 30 mL/kg bolus
- Colloids: Albumin for specific indications
- Blood Products: PRBC, FFP, platelets (1:1:1 ratio)
- Hemostatic Agents: Tranexamic acid if indicated
- Monitoring: CVP, urine output, lactate levels
Source Control
- Hemorrhage Control: Direct pressure, surgery
- Endoscopic Therapy: GI bleeding management
- Interventional Radiology: Embolization
- Surgical Intervention: Repair of vessel injury
- Antidiarrheal Agents: For GI losses
Treatment Algorithm
Treatment Mnemonic: “RESTORE”
- Recognize shock early
- Establish IV access
- Stop ongoing losses
- Transfuse blood products
- Oxygen therapy
- Replace volume aggressively
- Evaluate response
Nursing Process
Nursing Assessment
- • Comprehensive history and physical
- • Vital signs with orthostatic changes
- • Cardiovascular assessment
- • Respiratory assessment
- • Neurological assessment
- • Skin and mucous membrane assessment
- • Intake and output monitoring
- • Laboratory value interpretation
Nursing Diagnoses
- • Deficient fluid volume
- • Decreased cardiac output
- • Ineffective tissue perfusion
- • Risk for shock
- • Anxiety related to condition
- • Risk for injury
- • Imbalanced nutrition
- • Impaired skin integrity
Expected Outcomes
Nursing Priority Mnemonic: “ABCDE”
- Airway management
- Breathing support
- Circulation restoration
- Disability prevention
- Exposure and examination
Nursing Interventions
Immediate Interventions
- Airway: Ensure patent airway, consider intubation
- Breathing: Provide O2, monitor SpO2
- Circulation: Establish large bore IV access
- Fluid Resuscitation: Administer crystalloids rapidly
- Bleeding Control: Apply direct pressure
- Positioning: Trendelenburg position
- Monitoring: Continuous vital signs
Ongoing Monitoring
- Vital Signs: Every 15 minutes initially
- Urine Output: Hourly measurement
- Mental Status: Neurological checks
- Skin Assessment: Color, temperature, moisture
- Laboratory Values: CBC, chemistry, lactate
- Hemodynamic Parameters: CVP, MAP
- Fluid Balance: Strict I&O monitoring
Specific Nursing Actions
Fluid Management:
- • Administer crystalloids as ordered
- • Monitor for signs of fluid overload
- • Maintain accurate I&O records
- • Assess for pulmonary edema
- • Weight patient daily
Blood Product Administration:
- • Verify type and crossmatch
- • Monitor for transfusion reactions
- • Warm blood products if indicated
- • Use appropriate filters
- • Document transfusion details
Intervention Mnemonic: “MONITOR”
- Manage airway and breathing
- Obtain IV access
- Notify physician immediately
- Infuse fluids rapidly
- Trend vital signs closely
- Observe for complications
- Reassess frequently
Complications
Life-Threatening Complications
- Multiple Organ Failure: Kidney, liver, lung failure
- Acute Respiratory Distress Syndrome: Pulmonary edema
- Disseminated Intravascular Coagulation: Bleeding/clotting
- Acute Kidney Injury: Tubular necrosis
- Cardiovascular Collapse: Cardiac arrest
- Cerebral Hypoxia: Permanent brain damage
Treatment-Related Complications
- Fluid Overload: Pulmonary edema, CHF
- Electrolyte Imbalances: Hyponatremia, hyperkalemia
- Transfusion Reactions: Hemolytic, allergic
- Infection: Catheter-related bloodstream infections
- Coagulopathy: Dilutional, consumption
- Hypothermia: Massive transfusion
Prevention Strategies
Early recognition and aggressive treatment are key to preventing complications. Monitor for signs of organ dysfunction and maintain strict aseptic technique during procedures.
Complication Mnemonic: “ORGANS”
- Oliguria (kidney failure)
- Respiratory failure (ARDS)
- GI bleeding (stress ulcers)
- Acidosis (metabolic)
- Neurological deficits
- Sepsis (infection)
Nursing Implementation in Practice
Clinical Practice Application
Effective nursing care for hypovolemic patients requires rapid assessment, early intervention, and continuous monitoring. Nurses play a crucial role in recognizing early signs of hypovolemia and implementing appropriate interventions.
Assessment Skills
- Rapid Recognition: Identify early warning signs
- Comprehensive Assessment: Head-to-toe evaluation
- Trending Data: Monitor changes over time
- Critical Thinking: Analyze assessment findings
- Communication: Report changes promptly
- Documentation: Accurate record keeping
Intervention Skills
- IV Therapy: Skilled venipuncture and management
- Fluid Administration: Safe and effective delivery
- Medication Management: Accurate preparation and administration
- Monitoring Techniques: Proper use of equipment
- Patient Positioning: Appropriate positioning for shock
- Family Support: Communication and education
Quality Indicators
Nursing Care Pathway
Practice Mnemonic: “NURSES”
- Notice early warning signs
- Understand pathophysiology
- Respond rapidly
- Support patient and family
- Evaluate effectiveness
- Safety first always
Summary & Key Points
Essential Take-Away Points
Hypovolemia is a medical emergency requiring immediate recognition and intervention. Early treatment significantly improves patient outcomes and prevents life-threatening complications.
Key Concepts
- • Hypovolemia results from decreased blood volume
- • Early recognition is crucial for patient survival
- • Compensatory mechanisms initially maintain BP
- • Decompensation leads to organ failure
- • Fluid resuscitation is the primary treatment
- • Source control is essential
Nursing Priorities
- • Rapid assessment and recognition
- • Immediate stabilization measures
- • Continuous monitoring and evaluation
- • Safe administration of fluids and medications
- • Patient and family support
- • Prevention of complications
Final Mnemonic: “SAVE LIVES”
- Support circulation
- Assess continuously
- Volume replacement
- Early recognition
- Limit complications
- Intervene rapidly
- Vital signs monitoring
- Evaluate outcomes
- Safety first
