India’s Healthcare Delivery System & Nursing Services
Comprehensive Guide for Nursing Students
Welcome to this comprehensive guide on India’s healthcare delivery system and nursing services! This resource is designed to help nursing students understand the complex healthcare framework in India, the evolution of nursing education, and the current trends and challenges facing the nursing profession.
Throughout this guide, you’ll find visual aids, mnemonics, flowcharts, and other memory tools to help you retain this important information. Let’s dive in!
Learning Objectives
- Understand the structure and components of India’s current healthcare delivery system
- Trace the planning and development of nursing services and education at global and national levels
- Identify recent trends and issues in nursing service and management
- Analyze the challenges and opportunities in the nursing profession in India
Overview
India has a mixed healthcare delivery system with both public and private components. The healthcare infrastructure in India is organized in a three-tier system based on population norms as recommended in the landmark Bhore Committee Report of 1946.
Three-Tier Structure of India’s Public Healthcare System

Source: ResearchGate, Three-tier rural Healthcare system in India
Mnemonic: “PST” for India’s Healthcare Tiers
- Primary Care: Sub-centers & Primary Health Centers (First contact point)
- Secondary Care: Community Health Centers (Specialist care)
- Tertiary Care: District/Specialized Hospitals (Advanced medical care)
Primary Level
1. Sub-centers (SCs)
- Population coverage: 5000 people (plain areas) or 3000 people (hilly/difficult/tribal areas)
- Staff: At least one Auxiliary Nurse Midwife (ANM)/female health worker and one male health worker
- Under NRHM: Provision for one additional ANM on contract basis
- Services: Maternal and child health, family welfare, nutrition, immunization, diarrhea control, and communicable disease control programs
2. Primary Health Centers (PHCs)
- Population coverage: 30,000 people (plain areas) or 20,000 people (hilly/difficult/tribal areas)
- Staff: Medical officer supported by 14 paramedical and other staff
- Under NRHM: Two additional staff nurses on contract basis
- Capacity: 4-6 beds for in-patients
- Acts as referral unit for 5-6 SCs
- Services: Health promotion and curative services
Secondary Level
Community Health Centers (CHCs)
- Population coverage: 120,000 people (plain areas) or 80,000 people (hilly/difficult/tribal areas)
- Staff: Four medical specialists (surgeon, physician, gynecologist/obstetrician, pediatrician) supported by 21 paramedical and other staff
- Capacity: 30 beds with operating theater, X-ray, labor room, and laboratory facilities
- Serves as referral center for PHCs within the block
- Provides facilities for obstetric care and specialist consultations
Tertiary Level
District Hospitals and Specialized Care Centers
- Highest level of public healthcare
- Provides specialized healthcare services
- Advanced diagnostic and treatment facilities
- Teaching hospitals and medical college hospitals
First Referral Units (FRUs)
An existing facility (district hospital, sub-divisional hospital, CHC) can be declared a fully operational FRU only if it meets specific criteria:
Three Critical Determinants of a FRU:
- Emergency obstetric care including surgical interventions such as caesarean sections
- Care for small and sick newborns
- Blood storage facility on a 24-hour basis
National Rural Health Mission (NRHM)
Launched in 2005, NRHM was a watershed moment for India’s health sector, aiming to provide effective healthcare to the rural population with a special focus on 18 states having weak public health indicators and/or weak infrastructure.
Key Achievements of NRHM (2005-2013)
- Human resources: 931,239 Accredited Social Health Activists (ASHAs), 27,421 doctors, 4,078 specialists, 40,119 staff nurses, 72,984 ANMs
- Management: 618 District Program Managers and 633 District Accounts Managers deployed
- Infrastructure: More than 30,000 ambulances deployed nationwide
- Community participation: 499,210 Village level Health Sanitation and Nutrition Committees created
- Finances: Total investment of 21 billion USD by the central government (2005-2015)
- Education: Graduate medical capacity increased by 54% and post-graduate medical seats by 74% (2009-2013)
Recent Initiatives and Developments
1. Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A) Approach
Launched in 2013, this approach recognized that newborn health and survival is inextricably linked to women’s health across all life stages.
Specific interventions include:
- Delivery of antenatal care package and tracking of high-risk pregnancies
- Skilled care at birth, emergency obstetric care, and postpartum care
- Home-based newborn care and prompt referral
- Facility-based care of the sick newborn
- Integrated management of common childhood illnesses
2. Ayushman Bharat
Launched in 2018, it consists of two major initiatives:
- Health and Wellness Centers: Upgrading SCs and PHCs to provide comprehensive primary healthcare
- Pradhan Mantri Jan Arogya Yojana (PM-JAY): World’s largest health insurance scheme, providing coverage up to ₹5 lakhs per family per year for secondary and tertiary care hospitalization
3. Digital Health Initiatives
- Ayushman Bharat Digital Mission: Creating digital health IDs for all citizens
- Telemedicine: Expansion during COVID-19 through eSanjeevani platform
- Electronic Health Records: Standardization and implementation
Current Challenges in India’s Healthcare System
Critical Challenges
- Inadequate Infrastructure: Shortage of healthcare facilities, especially in rural areas
- Workforce Shortages: Insufficient doctors, nurses, and other healthcare professionals
- Urban-Rural Divide: Concentration of healthcare facilities in urban areas
- Financial Barriers: High out-of-pocket expenditure leading to catastrophic health spending
- Quality of Care: Variation in standards of care across facilities
- Governance Issues: Weak regulatory mechanisms and accountability systems
Historical Evolution of Nursing in India
Pre-Independence Era (Before 1947)
• 1871: First School of Nursing established in Madras
• 1908: Formation of Trained Nurses Association of India (TNAI)
• 1926: Indian Nursing Council Act passed but not implemented
Post-Independence (1947-1970)
• 1947: Indian Nursing Council (INC) established
• 1950s: Bachelor of Nursing programs started
• 1959: First Master’s program in nursing at RAK College of Nursing, Delhi
• 1960s: Nursing recognized as professional service
Expansion Period (1970-2000)
• 1972: Nursing included in 5th Five Year Plan
• 1988: First PhD in Nursing at SNDT Women’s University, Mumbai
• 1992: Introduction of specialized nursing courses
• 1998: Major curriculum revisions by INC
Modern Era (2000-Present)
• 2005: NRHM launched with focus on rural health workforce
• 2013: RMNCH+A strategy with emphasis on maternal and child health
• 2017: National Health Policy emphasized specialized nursing training
• 2023: National Nursing and Midwifery Commission Act passed
Structure of Nursing Education in India
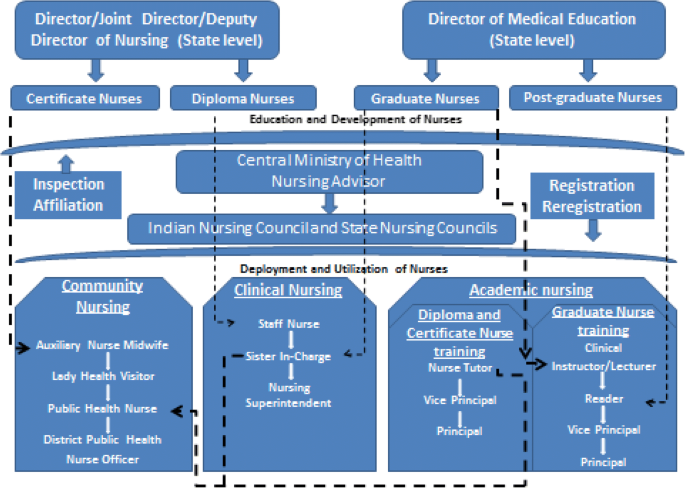
Source: International Journal for Equity in Health – BioMed Central
Current Nursing Education Structure
| Program | Duration | Eligibility | Annual Output (Approx.) |
|---|---|---|---|
| Auxiliary Nurse Midwifery (ANM) | 2 years | 10+2 in any stream | Not specified |
| General Nursing and Midwifery (GNM) | 3.5 years | 10+2 with 40% marks | 134,949 |
| B.Sc. Nursing (Basic) | 4 years | 10+2 with PCB and 45% marks | 107,814 |
| Post Basic B.Sc. Nursing | 2 years | GNM with 2 years experience | 25,485 |
| M.Sc. Nursing | 2 years | B.Sc. Nursing with 1 year experience | 13,971 |
| M.Phil./Ph.D. in Nursing | 2-5 years | M.Sc. Nursing | Limited |
Mnemonic: “CAREER” in Nursing Education Governance
- Council (Indian Nursing Council) – National regulatory body
- Approval of nursing institutions and programs
- Regulation of curriculum and standards
- Examination and certification standards
- Enrollment of qualified nurses in the register
- Reciprocity with nursing councils of other countries
Recent Developments in Nursing Curriculum
Key Reforms in Nursing Education
- Competency-Based Education: Shift from knowledge-based to competency-based curriculum
- CGPA System: Implementation of Cumulative Grade Point Average for academic evaluation
- Semester System: Division of academic year into semesters for better assessment
- Self-Directed Learning: Emphasis on providing environment for self-directed learning
- Technology Integration: Use of simulation, e-learning, and digital tools
- Specialization Options: Introduction of various specializations in nursing education
Global Scenario of Nursing Education
| Aspect | Global Trends | India’s Status |
|---|---|---|
| Minimum Educational Requirement | Bachelor’s degree increasingly becoming standard | Diploma (GNM) still widely accepted for practice |
| Advanced Practice Roles | Nurse Practitioners, Clinical Nurse Specialists recognized and autonomous | Limited recognition of advanced practice roles |
| Technology Integration | Advanced simulation labs, VR/AR, digital health records training | Growing but limited to certain institutions |
| Research Focus | Strong emphasis on evidence-based practice and nursing research | Emerging focus, limited resources and opportunities |
| Continuing Education | Mandatory for license renewal in many countries | Not consistently required or enforced |
| Nurse-Patient Ratio Standards | Legally mandated in many developed countries | No legally enforced standards |
International Mobility of Indian Nurses
Indian nurses are highly valued internationally, with significant migration to countries like:
- United States
- United Kingdom
- Australia
- Canada
- Gulf Countries (UAE, Saudi Arabia, Kuwait, etc.)
Impact of Nurse Migration
Positive Effects
- Remittances to home country
- Knowledge and skill transfer upon return
- International recognition of Indian nursing
- Better professional opportunities
Negative Effects
- Brain drain from Indian healthcare system
- Shortage of experienced nurses
- Loss on investment in education
- Quality of care impacts in domestic settings
Current Challenges in Nursing Profession
Nursing Workforce Challenges in India

Source: HealthLeaders Media – Top 5 Challenges in Nursing
Nursing Shortage
- India has nurse-to-population ratio of 1:670, compared to WHO standard of 1:300
- Estimated shortage of 4.3 million nurses to meet WHO norms
- Uneven distribution across urban and rural areas
- High turnover rates due to working conditions
Working Conditions
- Poor staffing ratios, especially in government hospitals
- Long working hours leading to burnout
- Lack of adequate facilities and support systems
- Safety concerns and workplace violence
- Psychological stress, especially highlighted during COVID-19
Economic Concerns
- Low pay scales compared to other professionals with similar qualifications
- Discrepancies between private and public sector compensation
- Lack of standardized minimum wages based on qualifications
- Limited financial incentives for specialization or higher education
- Economic factors driving international migration
Theory-Practice Gap
- Disconnect between nursing education and clinical practice
- Limited clinical exposure during training
- Inadequate clinical facilities for practice
- Limited simulation and skill labs
- Need for mentorship and clinical support systems
Regulatory Issues
- Weak regulatory bodies and enforcement
- Insufficient representation of nurses in policy-making
- Lack of amendment of nursing acts
- Undermined leadership positions
- Proliferation of nursing institutions without quality control
Technological Adaptation
- Need for training in new healthcare technologies
- Limited digital literacy among nursing workforce
- Inadequate infrastructure for technology integration
- Gaps in telenursing and digital health competencies
- Limited research on technology application in nursing
Emerging Trends in Nursing Services
Mnemonic: “DIGITAL” Nursing Trends
- Digital Health Records & Informatics
- Integrated Care Models
- Global Nursing Mobility
- Innovative Teaching Methodologies
- Telehealth & Remote Care
- Advanced Practice Roles
- Leadership Development
Technological Advancements in Nursing
- Telenursing: Remote patient monitoring and consultation
- Mobile Health: Use of apps for patient education and monitoring
- Simulation-Based Training: High-fidelity mannequins and virtual reality
- Electronic Health Records: Digital documentation and data management
- AI and Predictive Analytics: For patient risk assessment
- Wearable Technology: For patient monitoring and health promotion
Expansion of Nursing Research
- Evidence-Based Practice: Integration of research into care
- Clinical Trials: More nurses leading and participating
- Systematic Reviews: Critical analysis of existing literature
- Meta-analyses: Statistical combining of results from multiple studies
- Collaborative Research: Interdisciplinary and international partnerships
- Implementation Science: Translating research into practice
Faculty Development Challenges
- Qualification requirements: Many institutions struggle to recruit faculty with required qualifications
- Continuing education: Limited opportunities for faculty development and continuing education
- Research capacity: Insufficient training and resources for conducting research
- Teaching methodologies: Need for training in modern pedagogical approaches
- Technology competence: Gaps in digital literacy and technology use in teaching
- Clinical expertise: Faculty often lack recent clinical experience
Cultural Diversity in Nursing
Cultural Competence in Nursing
India’s diverse population requires nurses to develop cultural competence to provide effective care across different communities.
Challenges
- Diverse languages and communication barriers
- Varied health beliefs and practices
- Different dietary customs and restrictions
- Religious practices impacting healthcare decisions
- Traditional medicine use alongside modern healthcare
Opportunities
- Learning from diverse perspectives
- Developing versatile communication skills
- Building cultural competence applicable globally
- Enhanced patient satisfaction through cultural sensitivity
- Integration of beneficial traditional practices
Future Opportunities and Solutions
Policy Level
- Strengthening nursing regulatory bodies
- Standardizing nurse-patient ratios
- Implementing qualification-based pay scales
- Developing career advancement pathways
- Including nurses in policy-making committees
- Ensuring quality control in nursing education
Institutional Level
- Creating better working environments
- Implementing mentorship programs
- Investing in continuing education
- Enhancing clinical simulation facilities
- Developing research infrastructure
- Promoting leadership development
- Supporting work-life balance initiatives
Individual Level
- Pursuing continuous professional development
- Developing specialized clinical skills
- Engaging in research activities
- Building technological competence
- Participating in professional organizations
- Advocating for the nursing profession
- Mentoring junior nurses
India’s healthcare delivery system has undergone significant transformation since independence, with the development of a three-tier structure and various national programs and initiatives. The nursing profession has evolved alongside this system, facing both challenges and opportunities in education, service, and management.
The future of nursing in India depends on addressing persistent systemic challenges such as workforce shortages, economic concerns, and regulatory issues. At the same time, embracing emerging trends in technology, research, and specialized care will help advance the profession and improve healthcare outcomes.
By strengthening nursing education, improving working conditions, enhancing career pathways, and ensuring greater representation in policy decisions, nurses can play a pivotal role in achieving India’s healthcare goals and providing quality care to its diverse population.
Key Takeaways
- India’s healthcare system operates on a three-tier structure with primary, secondary, and tertiary levels of care.
- National initiatives like NRHM and RMNCH+A have significantly impacted healthcare delivery and nursing services.
- Nursing education in India has evolved from basic training to specialized education at graduate and post-graduate levels.
- Major challenges include nursing shortages, poor working conditions, economic concerns, and regulatory issues.
- Emerging trends include technological integration, expanded research scope, and cultural competence development.
- Multi-level solutions involving policy changes, institutional improvements, and individual development are needed.
- The future of nursing in India requires balancing global standards with local healthcare needs and contexts.
- Health systems in India – PMC – PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC5144115/
- Transformation in nursing education in India: Current issues – IJMPO. https://www.ijmpo.com/html-article/14978
- State of nursing in India: Persistent systemic challenges – PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC9547647/
- India | International Health Care System Profiles. https://www.commonwealthfund.org/international-health-policy-center/countries/india
- Healthcare Industry in India – IBEF. https://www.ibef.org/industry/healthcare-india
- Nursing Services in India. https://www.tnaijournal-nji.com/admin/assets/article/pdf/10860_pdf.pdf
- Development of nursing education in India: past, present and future. https://www.ijcmph.com/index.php/ijcmph/article/download/13361/8053/64460
- Nursing Shortage in India: Are There Solutions for Policymakers? https://journals.lww.com/ijcn/fulltext/2024/07000/nursing_shortage_in_india__are_there_solutions_for.3.aspx
- Top 10 Nursing Trends for 2025 | Purdue Global. https://www.purdueglobal.edu/blog/nursing/top-10-nursing-trends/
- 7 Growing Trends in Nursing Education | University of Cincinnati. https://online.uc.edu/blog/seven-growing-trends-in-nursing-education/
© 2025 Guide for Nursing Students | India’s Healthcare Delivery System & Nursing Services
Created for educational purposes only
